Abstract
Because of the broad availability of efficacious osteoporosis therapies, conduct of placebo-controlled trials in subjects at high risk for fracture is becoming increasing difficult. Alternative trial designs include placebo-controlled trials in patients at low risk for fracture or active comparator studies, both of which would require enormous sample sizes and associated financial resources. Another more attractive alternative is to develop and validate surrogate endpoints for fracture. In this perspective, we review the concept of surrogate endpoints as it has been developed in other fields of medicine and discuss how it could be applied in clinical trials of osteoporosis. We outline a stepwise approach and possible study designs to qualify a biomarker as a surrogate endpoint in osteoporosis and review the existing data for several potential surrogate endpoints to assess their success in meeting the proposed criteria. Finally, we suggest a research agenda needed to advance the development of biomarkers as surrogate endpoints for fracture in osteoporosis trials. To ensure optimal development and best use of biomarkers to accelerate drug development, continuous dialog among the health professionals, industry, and regulators is of paramount importance.
Key words: osteoporosis, surrogate endpoint, clinical trial, fracture, biomarker
FUTURE NEEDS FOR OSTEOPOROSIS TREATMENT
Approved osteoporosis therapies reduce the risk of vertebral fractures by 40–70%, and some also reduce the risk of nonvertebral fractures by 20–35% and/or hip fracture by 40–50%.(1) Although highly efficacious, currently approved therapies do not eliminate fractures entirely. Moreover, compliance with current therapies is low, and thus optimal antifracture efficacy may not be achieved in clinical practice.(2,3) Taken together, these observations indicate that there is a need for new therapies that provide better prevention of fragility fractures, particularly with regard to nonvertebral fractures.
CHALLENGES OF NEW CLINICAL TRIALS IN OSTEOPOROSIS: THE NEED FOR SURROGATE ENDPOINTS FOR FRACTURE
Regulatory agencies currently require 2- or 3-yr trials with fracture as the primary endpoint to show the efficacy of new therapies for osteoporosis.(4,5) Accordingly, the antifracture efficacy of drugs that are currently approved for the treatment of postmenopausal osteoporosis has been established in placebo-controlled trials performed in patients with high to moderate fracture risk, based on prevalent fractures and BMD. The primary endpoint of these trials was either incident vertebral fractures, nonvertebral fractures, or hip fractures over 3 yr.
Given the broad availability of effective drugs to treat osteoporosis, initiation of new placebo-controlled trials for new osteoporosis therapies that enroll moderate to high-risk patients is viewed as unethical in many countries.(6,7) As a result, obtaining ethical committee and patient approval for these types of studies has grown increasingly challenging. Alternatives to the current paradigm for establishing antifracture efficacy of a new therapeutic agent include (1) conducting a placebo-controlled trial in subjects with low risk for fracture, a study design that is subject to criticism regarding whether the results could be extrapolated to patients at high risk for fracture, or (2) conducting a randomized trial comparing the new therapy with a currently approved drug that has shown consistent and robust antifracture efficacy, a so-called “active comparator trial,” with either a noninferiority or superiority design, in patients with moderate to high risk for fracture. In both cases, the primary endpoint would be fracture, and the required sample sizes would be very large, on the order of 6000–30,000 subjects for 3 yr,(6) compared with 2000–8000 patients for 3 yr for previous phase III trials. These numbers imply significant costs that may jeopardize the development of new therapeutic agents in osteoporosis.
Another more attractive alternative would be the development and subsequent use of biomarkers that could serve as surrogate endpoints for fracture in clinical trials. Generally, clinical trials that use surrogate endpoints can be conducted faster, cheaper, and more efficiently than those with clinical endpoints, although there are drawbacks to this approach.(8) In this perspective, we briefly review the concept of surrogate endpoints as it has been developed in other fields of medicine and discuss how this concept could be applied in clinical trials of osteoporosis.
GENERAL DEFINITION AND VALIDATION CRITERIA FOR BIOMARKERS AND SURROGATE ENDPOINTS
The ethical and statistical framework for conducting studies to determine the clinical benefits and risks of a treatment are well established. However, in the past two decades, interest in developing methodologies suitable for studying whether a biological parameter might serve as a substitute for a clinical event or outcome in studies testing the efficacy and safety of new therapies has grown markedly.
Until recently, terminology for describing the potential substitution of biological parameters as clinical endpoints was imprecise and inconsistent. In 2001, an NIH working group provided general definitions and recommended standardized terminology that are applicable across diseases and disciplines,(9) as follows:
Biological marker (biomarker): a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention
Clinical endpoint: a characteristic or variable that reflects how a patient feels or functions or how long a patient survives
Surrogate endpoint: a biomarker intended to substitute for a clinical endpoint
In some fields, biomarkers are already being used to identify subgroups of patients that respond differently to a particular therapy and to enhance early diagnosis of disease. In addition, there is a strong and growing interest in assessing whether, and under what conditions, biomarkers may be used to guide dose selection in phase II trials and/or substitute for a primary endpoint in phase III trials.(8,10,11) Indeed, biomarkers have been used as surrogate endpoints in a many areas of medicine, including assessment of viral load in AIDS, glycosylated hemoglobin A1c (HbA1c) for non–insulin-dependent diabetes, and various surrogate endpoints in cardiovascular disease.(12) In the cancer field, over one half of recent approvals by the European Medicines Agency (EMEA) have been based on the surrogate endpoint of “response rate” rather than clinical endpoints such as overall, disease-free, or progression-free survival.(13)
Although there are no rigid guidelines for validating biomarkers as surrogate endpoints, several principles for evaluating the usefulness of biomarkers have emerged.(8,14,15) Generally, if biomarkers are to be used as regulatory tools, they must meet technical requirements for accuracy and precision, be consistent with the pathophysiology of the disease (i.e., have biological plausibility), and be associated with the clinical outcome. Supportive studies include epidemiologic evidence that a biomarker is a strong risk factor for the disease under study, as well as confirmation that it is directly modified by the intervention. Moreover, the effects of treatment on the biomarker should explain a substantial proportion of, or be strongly associated with, the effects of treatment on the clinical endpoint. The extent to which a biomarker is appropriate for use as a surrogate endpoint in evaluating a new treatment depends on the degree to which the biomarker can reliably predict the clinical benefit of that therapy compared with standard treatment of care or other approved therapy.
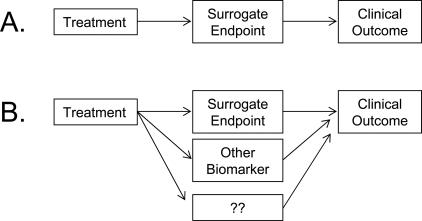
The approach to analyzing the relationship between a biomarker and clinical endpoints generally begins with a simple model characterizing the relationship between treatment, biomarker, and clinical endpoint (Fig. 1). These models characterizing the relationship between treatment, biomarker, and clinical endpoint can be used to quantify the extent to which treatment effects are mediated by the surrogate endpoint. Generally, to be a “valid” surrogate endpoint, the biomarker must be associated with, or predict a change in, the clinical outcome. The two main approaches to statistical evaluation of surrogate endpoints include analysis of single trials and analysis of multiple trials (meta-analytic approaches).
FIG. 1.
Models characterizing the relationship between treatment, biomarker (or surrogate endpoint), and clinical outcome. (A) A “perfect surrogate,” where the biomarker mediates all of the effect of the treatment on the clinical outcome. (B) The more likely situation where the biomarker mediates some, but not all, of the effect of the treatment on the clinical endpoint.
Approaches using single trials
In 1989, Prentice(16) proposed the first formal method for testing the statistical validity of a surrogate endpoint using a single trial, which relied on an “all or nothing” criteria in terms of validation. This was followed in the 1990s by the introduction of a graded criterion for validation of surrogate endpoints using single trials, termed the “proportion of treatment effect” (PTE).(17,18) The PTE reflects the proportion of treatment effect that is mediated by the surrogate endpoints and is defined as the ratio of the amount by which a treatment effect on the clinical endpoint is changed after including a surrogate endpoint in the model to the unadjusted treatment effect on the clinical endpoint. Whereas this approach is appealing, it has been criticized because of conceptual and mathematical concerns.(10,19–21)
Approaches using multiple trials
In the mid- to late 1990s, use of simultaneous analysis of multiple trials to assess the validity of surrogate endpoints was proposed.(19,22) These approaches can accommodate analyses that use both trial-level and individual-level data to determine the association between the surrogate and true endpoint.(23–25) Combining results from multiple studies through meta-analyses may provide a more robust evaluation of a potential surrogate endpoint than using results of single study.(10,21) Furthermore, meta-analyses may be particularly helpful when the available studies evaluate effects of different classes of interventions on biomarker and clinical endpoints.
Other approaches to characterizing the relationship between treatment, biomarker, and clinical endpoint include models that combine multiple biomarkers or repeated measurements of a single biomarker (i.e., “joint models”),(21,26) and most recently, information theory to create a unified framework for surrogate endpoint evaluations.(27) Whereas many methods for validation of surrogate endpoints have been proposed and are under study, presently there is lack of consensus regarding the optimal statistical approach to evaluate potential surrogate endpoints.(21,23,28) It should also be noted that, although statistical approaches are necessary to evaluate surrogate markers, these are not the only factors, because key clinical and biological observations must be considered in a comprehensive validation of a potential surrogate endpoint.(14)
DEFINITION AND VALIDATION CRITERIA FOR BIOMARKERS AND SURROGATE ENDPOINTS IN OSTEOPOROSIS
For osteoporosis, the clinical endpoint is fracture, because fractures are responsible for the morbidity and excess mortality caused by the disease. Potential biomarkers include image-based assessment of skeletal fragility, as well as circulating levels and urinary excretion of biochemical markers of bone turnover (BTMs). An ideal surrogate endpoint would be a biomarker that explains most of the antifracture efficacy of a given therapeutic agent. The optimal study to validate a surrogate endpoint for fracture would be a randomized, placebo-controlled trial with fracture outcomes in which the biomarker is measured in all subjects at baseline and during treatment (i.e., concurrent with an ongoing phase III trial).
Because most phase III trials in osteoporosis enroll thousands of subjects, depending on the particular biomarker, this approach will require extensive financial resources and relatively long duration. Moreover, this approach would “validate” the surrogate endpoint in a drug trial for which there was already a fracture endpoint, thereby negating the need for the fracture surrogate except for future drug development. Because this study is unlikely to be undertaken, below we propose an alternative, step-wise approach to investigate the potential of developing biomarkers that may substitute as surrogate endpoints for fracture in clinical trials.
At the outset it is presumed that all biomarkers under consideration, both biological and imaging-based methods, would meet established standards for accuracy, precision, and reliability. In addition, the biomarker methodology should have established quality control procedures, standardized data acquisition, and analysis, as well as methods for cross-calibration of devices at different clinical centers, as appropriate.
Step 1: show biological plausibility (i.e., relationship between biomarker and pathogenetic mechanisms leading to increase skeletal fragility)
The mechanisms underlying skeletal fragility associated with osteoporosis are multifactorial. Thus, a potential biomarker may be associated with various factors associated with skeletal fragility, including abnormalities of bone turnover, decreased bone mass, or alterations in bone micro- and macroarchitecture.(29,30) Studies establishing the biological plausibility of a biomarker in osteoporosis could include clinical observational studies, preclinical studies, and experiments using human cadaveric specimens. The biomarker could reflect aspects of the disease process and/or the severity of the disease state at a given point in time.
Step 2: show significant association between biomarker and fracture in the target population
Two different study designs could be used to show a significant association between the biomarker and fracture risk in the target population: (1) cross-sectional, case-control study or (2) a prospective longitudinal study. A typical cross-sectional study would compare values of the biomarker in postmenopausal women with one or more vertebral fractures to values in an age-matched control group of women with no prior history of fracture. However, the biomarker may be influenced by the fracture event, and moreover, case-control studies cannot control for all potential confounders. For example, BMD may decline in individuals with fracture because of reduced activity after the fracture and therefore the assessment of fracture cases versus controls will be biased in favor of low BMD being associated with fracture. Thus, longitudinal study designs are preferred.
In a longitudinal study, the biomarker is measured before the fracture occurs. The most common study designs include (1) a prospective cohort, in which the biomarker is measured in all individuals at baseline who are then followed prospectively for fracture, and (2) a nested case-control study within a prospective cohort, in which the biomarker (which was collected at baseline) is subsequently measured in all or a subset of individuals in the cohort who suffered a fracture and compared with subjects who did not suffer a fracture in the follow-up period. The prospective cohort design has been used in several large studies (i.e., Study of Osteoporotic Fractures, DUBBO, Rotterdam, OFELY, MrOS) to show that low BMD is associated with fracture.(31,32) In comparison, the nested case-control design has been used to show the association between fracture and bone turnover(33) or radiographically derived indices of bone fragility.(34) Although the prospective cohort design provides the most robust assessment of associations with fracture, it requires a large sample size (although this depends on the type of fracture to be studied), several years of follow-up, and that the biomarker be measured in all individuals. In comparison, if the biomarker was collected at baseline (although maybe not analyzed to save costs), a nested case-cohort design is more efficient because the biomarker is measured retrospectively only in a subset of individuals, and because fractures have already occurred, no additional follow-up time is needed.
In conclusion, the time frame for showing a significant association between a new biomarker and fracture risk in untreated patients can vary dramatically depending on availability of biomarker data in existing cohorts with longitudinal follow-up. If biomarker data were acquired at baseline and stored (i.e., serum or urine samples or image data), the time to establish a relationship with fracture risk through a nested case-cohort study is relatively short. In contrast, if new data acquisition in a new cohort is needed, establishing an association with fracture risk can take several years of follow-up to accumulate sufficient number of fracture cases.
Step 3: show that the biomarker changes consistently in response to therapy, preferably in a predictable and dose-dependent fashion that agrees with the known mechanism of action of the therapeutic intervention
To show that the biomarker changes in response to therapy, one could conduct a trial with a study design similar to most phase II trials—a randomized, placebo-controlled trial with multiple doses. The trial could be conducted in subjects with low or moderate risk of fracture, as long as the mechanism of action of the drug does not differ according to the severity of the disease. The study duration could vary with the responsiveness of the biomarker. For example, bone turnover markers generally respond quickly (i.e., within days or weeks) to an intervention, whereas imaging-based techniques may require a study duration of several months to more than a year. Inclusion of multiple doses and other drugs with either similar or different mechanisms of action is desirable, because the ideal biomarker will exhibit a dose–response relationship and will change in a predictable fashion with the known mechanism of action of the intervention.
Step 4: show that changes in the biomarker with treatment explain a substantial proportion of the antifracture efficacy
A few different study designs could be used to show that treatment-induced changes in the biomarker explain a substantial proportion of the antifracture efficacy of a drug. The key elements of these types of studies are that the biomarker is measured in all individuals and that fractures are included as an endpoint. Traditionally, this would be a placebo-controlled study in high-risk patients; however, as mentioned previously, these types of studies are becoming increasingly difficult because of ethical concerns associated with the wide availability of effective therapies. Thus, the alternatives are to conduct an active comparator study in subjects with high risk of fracture or a placebo-controlled trial in subjects with low- to moderate-risk of fracture.
An advantage to the active comparator trial is that there is likely to be adequate number of fractures and therefore good statistical power to show an association between changes in the biomarker and reductions in fracture risk. However, the lack of a placebo group limits these estimates because the proportion of treatment effect cannot be computed without a placebo group.(35) Conversely, a placebo-controlled trial in a population with a low to moderate risk of fracture would enroll several thousands of patients, and the analysis of the treatment effect on the biomarker would be adequately analyzed retrospectively in patients with incident fractures compared with a matched subgroup of patients without incident fractures in both treatment groups.
CRITICAL REVIEW OF SELECTED BIOMARKERS IN OSTEOPOROSIS
In this section, we attempt to evaluate how well the criteria outlined above have been met for several established techniques, such as BMD by DXA and BTMs, as well as for new potential biomarkers, including vBMD and geometry by QCT, trabecular microarchitecture measurements by MRI and high-resolution pQCT (HR-pQCT), and bone strength estimates by finite element analysis (FEA). For each biomarker, a summary is provided for each step in Tables 1 and 3, and an explanation is below. This is not meant to be an exhaustive review of the literature but rather a critical assessment of selected studies showing how these biomarkers meet criteria for qualification as surrogate endpoints for fracture. Furthermore, although there are several other techniques that seem promising for fracture risk prediction and treatment monitoring, such as quantitative ultrasound and specialized image analysis of radiographs, a comprehensive review of all possible techniques is beyond the scope of this manuscript.
Table 1.
Association Between Biomarker and Fracture Risk in Untreated Patients (Step 2)
| Study type |
Biomarker |
||||
| DXA-BMD | BTM | QCT | μ-Arch | QCT-FEA | |
| Cross-sectional | +++ | + | +++ | +++ | + |
| Longitudinal | |||||
| Nested case-cohort | +++ | ND | ND | ND | |
| Prospective | +++ | +++ | ND | ND | ND |
—, data exist, no relationship shown; +, evidence from one study, weak or moderate relationship; ++, data from more than one study, weak to moderate relationship or very strong relationship in one study; +++, data from more than one study, consistent strong association; ND, no data; BTM, bone turnover markers; μ-Arch, trabecular microarchitecture measurements by high-resolution pCT or MRI; QCT-FEA, QCT-based finite element analyses.
Table 3.
Association Between Change in Biomarker and Fracture Reduction With Treatment (Step 4)
|
Biomarker |
|||||
| DXA-BMD | BTM | QCT | μ-Arch | QCT-FEA | |
| Raloxifene | — | + | ND | ND | ND |
| Bisphosphonates | ++ | +++ | ND | ND | ND |
| Teriparatide | + | ND | ND | ND | ND |
| Strontium ranelate | ++ | ND | ND | ND | ND |
See Table 1 for definitions.
Table 2.
Change in Biomarker With Treatment (Step 3)
|
Biomarker |
|||||
| DXA-BMD | BTM | QCT | μ-Arch | QCT-FEA | |
| Raloxifene | + | ++ | + | ND | ND |
| Bisphosphonates | +++ | +++ | ++ | ND | + |
| Teriparatide | +++ | +++ | +++ | ND | + |
| Strontium ranelate | ++++ | + | ND | ND | ND |
See Table 1 for definitions.
BMD by DXA
Biological plausibility:
Bone loss caused by aging and menopause is believed to contribute to increased skeletal fragility. As such, measurements of bone mass and BMD are key elements in the pathophysiology of osteoporosis and contribution to increased fracture risk. Moreover, numerous studies using human cadaveric specimens have confirmed a strong association between BMD and strength of the proximal femur and vertebral bodies.(36–41)
Association with fracture in untreated patients:
Several large prospective studies have shown a consistent, strong relationship between low BMD and increased fracture risk in both men and women.(31,32,42,43) Although BMD at any skeletal site predicts fracture, hip BMD predicts hip fracture more strongly than BMD measurements at other sites.(31,44)
Change with therapy in a predictable, dose-dependent fashion:
The increase in BMD induced by most anti-osteoporosis agents is greater in skeletal sites enriched in trabecular bone than in those with predominant cortical bone. The increase is usually greatest at the lumbar spine, followed by the trochanter, then the total hip, and is limited at the femoral neck. Except for hormone replacement therapy (HRT) and denosumab, there is either no change or a decrease in BMD measured by DXA at the forearm. With antiresorptive agents, one half of the gain of BMD is achieved within 6–12 mo, followed by a slower increase over years. A dose-dependent increase in BMD has been shown at all skeletal sites in numerous studies with oral, transdermal, and intranasal HRTs.(45–47) Data are limited with raloxifene, which produces a small (2%) increase in BMD at the spine, hip, and total body.(48) A clear dose-dependent increase in BMD at the spine and hip has been shown with the bisphosphonates alendronate,(49–51) risedronate,(52,53) and ibandronate,(54,55) as well as with strontium ranelate.(56–58) A few studies also showed dose-dependent changes in BMD after PTH treatment.(59,60)
Explain a substantial proportion of antifracture efficacy:
Several studies have examined the association between treatment-related changes in BMD and reduction in fracture risk.(61–71) All these studies showed that the change in BMD during treatment is significantly associated with fracture risk reduction. However, the strength of that association varies with the analytical approach (i.e., meta-analysis versus single trial), fracture type (i.e., vertebral versus nonvertebral versus hip), and therapeutic agent.
For example, although one meta-analysis suggested that much of the reduction in vertebral fracture risk associated with antiresorptive therapy could be explained by increases in BMD,(62) other studies reported that <30% of the reduction in vertebral fracture risk after antiresorptive treatment was explained by the increase in BMD.(63–65) Similar variability has been reported for the association between the change in BMD and reduction in nonvertebral fracture risk after antiresorptive therapy.(66,68)
Evidence that the ability of changes in BMD to explain antifracture efficacy may depend on the treatment is provided by a recent analysis showing that, for strontium ranelate, the 3-yr change in either femoral neck or total hip BMD explains ∼75% of the observed reduction in vertebral fracture risk.(70) In comparison, changes in BMD after teriparatide treatment explain ∼30–40% of the reduction in vertebral fracture.(69)
BTMs
Biological plausibility:
The activation of bone turnover in postmenopausal women, along with the imbalance in bone remodeling favoring bone resorption over formation, is responsible for accelerated bone loss and deterioration of trabecular architecture, both of which are associated with increased skeletal fragility. BTMs have been shown to reflect the level of bone turnover as measured on iliac crest biopsies and calcium kinetics.
BTMs increase sharply after menopause and then remain stable throughout life.(72) In postmenopausal women, BTMs are negatively correlated with BMD measured by DXA regardless of the skeletal site, BTM used, and time elapsed after menopause.(72,73) Although the rate of bone loss assessed by DXA in untreated women requires rigorous quality control and a long follow-up,(74) several studies have shown that high BTM levels are significantly associated with subsequent bone loss.(75–80) In summary, there is good evidence for biological plausibility of BTMs as indices of pathophysiology of osteoporosis.
Association with fracture in untreated patients:
Increased BTM levels predict fragility fractures at all sites independently of age, BMD, and prior fractures in postmenopausal women. This association has been assessed prospectively in longitudinal cohort studies(81–89) and case-control studies.(33,90–93) The association with fracture risk is stronger for bone resorption markers than for bone formation markers and is weaker in the frail elderly in whom incident falls is the strongest predictor of fractures.(91–93)
BTMs have been suggested to improve the identification of women at high risk of fracture. Indeed, osteopenic women with high BTM levels have a risk of fracture similar to that of osteoporotic women based on BMD, whereas osteopenic women with normal BTM levels have a fracture risk that is comparable to that of postmenopausal women with normal BMD.(87)
Change with therapy in a predictable, dose-dependent fashion:
Antiresorptive drugs rapidly reduce BTMs, reflecting resorption followed by decrease of BTMs, reflecting bone formation. The onset and magnitude of the decrease depends on the route of administration (e.g., faster for intravenous than for oral bisphosphonate) and on the mechanism of action of the antiresorptive agent that influences its potency in inhibiting bone resorption (e.g., greater for denosumab and bisphosphonates than for selective estrogen receptor modulators [SERMs]). A dose-dependent decrease of BTMs has been consistently found for HRT, SERMs, bisphosphonates, and denosumab.(48,54,55,94–99)
The bone-forming agent teriparatide induces a marked increase in all BTMs, reflecting the overall increase in bone turnover seen on bone biopsies.(100) The most sensitive BTM reflecting teriparatide effects on bone is serum N-terminal propeptide of type 1 collagen (PINP), which shows an early, large, and sustained increase under treatment that correlates significantly with the subsequent increase in BMD measured by DXA and by QCT.(101–104) Strontium ranelate induces a small decrease of serum C-terminal extension peptide of type 1 collagen (CTX) and a small increase in bone alkaline phosphatase.(57)
Explain a substantial proportion of antifracture efficacy:
In retrospective nested case-control studies of phase III trials with fracture as a primary endpoint, the magnitude of the 3- to 12-mo decrease of BTMs has been shown to be significantly associated with the fracture risk reduction in five analyses of trials with raloxifene, alendronate, and risedronate.(105–109) The proportion of treatment effect (PTE) caused by the decrease in BTMs is not clearly established and varies according to the antiresorptive agent. For example, the change in bone resorption markers accounted for 50% of risedronate's effects in reducing vertebral fracture risk in the first year and approximately two thirds over 3 yr.(106) This is greater than the PTE because of the increase in BMD after therapy (∼28% for 2-yr change in BMD(65)), but the CIs of these estimates for BTMs are quite large because they were measured only in a subset of the subjects in the trial.
Interestingly, the relationship between BTM changes and fracture risk is similar for placebo and antiresorptive-treated patients, in contrast to the BMD/fracture relationship.(109,110) There are no studies relating BTM changes and fracture risk reduction with strontium ranelate or with teriparatide.
Bone morphology and vBMD by QCT
Biological plausibility:
BMD, bone size, and bone morphology are important determinants of whole bone strength.(111) Therefore, it is plausible that QCT-derived measurements of trabecular and cortical vBMD, as well as 3D characteristics of bone morphology, will reflect osteoporosis pathophysiology and disease status. In support of this, numerous studies using human cadaver specimens have shown strong relationships between QCT-derived vBMD and morphology and femoral(112–114) and vertebral strength.(39,115–120)
Association with fracture in untreated patients:
Although there are limited prospective studies,(121) numerous case-control studies have shown significant differences in QCT-derived vBMD and geometry among individuals with prior vertebral or hip fracture compared with age-matched controls with no prior history of fracture.(122–128)
Change with therapy in a predictable, dose-dependent fashion:
Treatment-induced changes in vBMD and morphology assessed by QCT vary with therapy and skeletal site.(129–135) Teriparatide treatment leads to marked gains in vertebral trabecular BMD that are greater than those observed with alendronate.(130,131,133) For example, after 18 mo, vertebral trabecular BMD increased 19% versus 3.8% in postmenopausal women treated with teriparatide or alendronate, respectively.(133) Treatment-induced changes in vBMD and morphology at the hip are generally smaller in magnitude and results are less consistent than at the spine. For example, teriparatide and alendronate had similar effects on increasing femoral neck trabecular vBMD (∼2–5%), whereas cortical vBMD increased more with alendronate than teriparatide.(133) Other studies have shown that, although cortical vBMD at the hip increases more with alendronate than PTH, cortical volume increased to a greater extent with PTH, suggesting the presence of more, but less mineralized bone after PTH compared with alendronate.(130) Raloxifene has been shown to induce small increases in vertebral BMD in comparison with placebo.(132) There are no studies showing dose-related changes of bone density/geometry induced by any anti-osteoporotic drug.
Explain a substantial proportion of antifracture efficacy:
To date, no clinical trials with fracture as an endpoint have included assessment of geometry or vBMD by QCT, and therefore, no studies have reported the proportion of treatment effect explained by a QCT-based measurement.
Trabecular microarchitecture by MRI or HR-pQCT
Biological plausibility:
Bone loss along with deterioration of trabecular and cortical bone microarchitecture are hallmarks of osteoporosis.(136–138) Trabecular bone architecture deteriorates and cortical thickness declines with increased age, because of the imbalance in bone remodeling that favors bone resorption over bone formation. Clinical studies, comparing subjects with and without fracture, have suggested that microarchitectural deterioration, as assessed by iliac biopsy, contributes to fracture risk independent of bone mass.(139–141)
Association with fracture in untreated patients:
Several case-control studies confirmed that trabecular bone microarchitecture, measured at peripheral skeletal sites either by MRI(142–146) or HR-pQCT,(128,147–149) differs between fracture cases and controls. There are no prospective studies showing an association between microarchitecture assessed by MR or HR-pQCT and fracture.
Change with therapy in a predictable, dose-dependent fashion:
One study, the QUEST trial of nasal salmon calcitonin, has shown treatment-induced changes in bone microarchitecture in postmenopausal women, as measured in vivo by high-resolution MRI.(150) Consistent with the proposed mechanism of action of this antiresorptive, there were minimal changes in the calcitonin group, but decreases in the placebo group, resulting in significant treatment-induced changes in microarchitecture when the two groups were compared. In another study, significant improvements in trabecular microarchitecture, assessed at the distal tibia by high-resolution MRI, were seen after treatment of hypogonal men with testosterone for 2 yr.(151) There are no studies showing treatment-related changes in trabecular architecture as measured by HR-pQCT. No studies have shown dose–response relationships for changes in trabecular architecture with treatment.
Explain a substantial proportion of antifracture efficacy:
To date, no clinical trials with fracture as an endpoint have included assessment of trabecular microarchitecture by in vivo methods, and therefore, no studies have reported the proportion of treatment effect explained by a change in microarchitecture.
Bone strength estimates by finite element analysis
Biological plausibility:
The finite element (FE) method was first applied to structural analysis in the 1950s,(152) and it has since been widely used in nearly every engineering and engineering-related field because it can provide the ability to estimate how an object with a complex geometrical shape (e.g., a whole bone) behaves when it is subjected to external loads. Current clinical implementation of FEA is generally based on 3D-QCT scans, where each voxel of the CT scan is converted to an element in the finite element model.(153–156) This approach should theoretically be able to represent a bone's 3D geometry and the heterogeneous distribution of BMD and material properties, subject, of course to the limitations association with the resolution of the image data, the assumptions necessary to convert QCT density data to material properties, and the choice of external loads applied to the model.(157) Laboratory studies using human cadaveric specimens have shown that predictions of whole bone strength using this approach are strongly correlated with vertebral(118–120) and femoral strength.(113,158,159) In summary, QCT-based FEA, because of its ability to reflect bone geometry and bone mass distribution in a biomechanically relevant fashion and its strong association with bone strength in vitro, is considered to have high association with skeletal fragility and disease severity and therefore meets criteria for biological plausibility.
Association with fracture in untreated patients:
Two case-control studies have shown the ability of patient-specific QCT-based FE models of the lumbar spine to discriminate postmenopausal women with vertebral fractures from age-matched controls with no fracture.(128,153) In contrast, a case-control study comparing stiffness of the proximal femur derived from QCT-based FEA in postmenopausal women with recent hip fracture to controls with no fracture showed no differences according to fracture status.(123) There are no prospective studies testing the ability of QCT-based FEA to predict fracture risk.
Change with therapy in a predictable, dose-dependent fashion:
There are no studies showing a dose-dependent relationship between treatment and FE-predicted bone strength outcomes. However, two studies have shown changes in FE-predicted bone strength after therapeutic intervention. In the first, QCT-based FE models of the lumbar spine were performed at baseline and after 6 and 18 mo of treatment with teriparatide or alendronate in postmenopausal women.(156) Both teriparatide and alendronate were associated with significant increases in vertebral bone strength parameters at 6 mo, although changes in the teriparatide group were greater than alendronate. QCT-based FEA has also been used to evaluate changes in strength parameters of proximal femur in a sideways fall configuration after bisphosphonate or teriparatide treatment.(160)
Explain a substantial proportion of antifracture efficacy:
To date, no clinical trials with fracture as an endpoint have included bone strength estimates by FEA as an outcome, and therefore, no studies have reported the proportion of treatment effect explained by a change in FE-based predictions of bone strength.
DISCUSSION
In this perspective, we argue that there is an urgent need to develop surrogate endpoints for fracture and introduce concepts related to the use of biomarkers as surrogate endpoints in osteoporosis. Whereas many concepts are universal across disease categories, there are several issues specific to the application of surrogate endpoints in osteoporosis that require further consideration.
An important question is whether any biomarker or set of biomarkers will be valid across different classes of drugs, either with the same or differing mechanisms of action. The question is whether, after validation of a biomarker based on an accepted clinical endpoint (i.e., fracture), could the biomarker be used as an endpoint for registration of a new therapy of the same or differing mechanism of action? A key consideration is whether the interaction between the potential surrogate endpoint and the mechanism of action of the drug is well understood. This is particularly important for biological markers, such as bone turnover, which decrease, increase, and are relatively unchanged after antiresorptive, teriparatide, and strontium ranelate interventions, respectively. It is possible that an imaging biomarker, such as prediction of bone strength by FEA, which integrates the material and structural effects of the treatment, may be less sensitive to the biological mechanism of action of the intervention.
It is difficult to evaluate existing data to get a sense of whether currently available biomarkers show potential to be validated across different classes of treatments. Most of the existing studies have examined the ability of BMD and/or bone turnover markers to explain fracture reduction after antiresorptive therapies, mainly oral bisphosphonates. Other antiresorptive agents, such as intravenous bisphosphonates, SERMS, and denosumab, may have similar effects, although this needs to be more thoroughly tested. Moreover, there is limited data evaluating the ability of BMD and bone turnover markers to explain the antifracture efficacy of drugs with anabolic or other mechanisms of action. Thus, it is quite plausible that, if a biomarker were validated for a given bisphosphonate, it could be accepted as a surrogate endpoint for trials of a new bisphosphonate. However, it is less likely that the same validated surrogate endpoint would be easily accepted for a trial of a new anabolic or dual-action agent, although this is not impossible depending on the nature of the biomarker.
A second important question is whether a biomarker could be valid across different fracture types or will a different biomarker be needed for vertebral, nonvertebral, and hip fractures? Because they reflect bone remodeling activity in the entire skeleton, BTMs are more likely to be able to reflect a variety of clinical endpoints than an imaging endpoint, which may have greater skeletal site specificity. Ideally, a combination of biomarkers might provide a surrogate endpoint that would be valid for all fractures.
Furthermore, because of the multifactorial nature of skeletal fragility, it may be that a set of biomarkers, rather than any individual marker, will be more strongly associated with the clinical outcome and therefore the most likely to be qualified as a surrogate endpoint for fracture. As mentioned, an imaging biomarker along with a biological marker, such as bone turnover, may allow assessment of disease severity (e.g., an imaging biomarker) along with disease activity (e.g., a bone turnover marker). Similarly, this combination, for example, of BMD change and BTM change with treatment, might provide a better prediction of the antifracture efficacy of a therapeutic agent than either biomarker alone. This possibility could be easily assessed retrospectively from existing trial data, with the caveat that bone turnover markers were generally measured only in subsets of trial subjects. Complications with this approach for new studies are the obvious expense of designing trials with multiple imaging and biological markers and the lack of fully validated statistical methods by which to evaluate the ability of a set of biomarkers to reflect the clinical endpoint.
Although there is no consensus regarding the criteria that should be achieved for statistical validation of biomarkers as surrogate endpoints, a number of approaches, using data from both single trials and multiple trials, have been developed and tested in other fields. An emerging trend for evaluation of biomarkers as surrogate endpoints is to use meta-analysis of different trials. In this case, it is imperative to include analyses of individual patient data, because analyses using only mean values from different trials can be misleading.(110) However, challenges to this approach include the need to obtain patient data that often belongs to competitors in the pharmaceutical industry, as well as the consideration as to whether biomarkers have been acquired and analyzed using a standardized approach in the different trials.
Clearly a formidable research agenda lies ahead to validate a biomarker or set of biomarkers as a surrogate endpoint for fracture in osteoporosis, including technical development and testing of biomarkers in trials, as well as advancement of the statistical methodology for their evaluation. However, as we have outlined, there are already a number of biomarkers available that are promising, although currently there are limited data to assess their true potential to serve as surrogate endpoints for fracture. To address this limitation, several ongoing phase III placebo-controlled trials of new therapeutic agents have included some of these new imaging techniques and bone turnover markers as major endpoints. These studies will provide important information about the ability of these techniques to serve as surrogate markers. As has been done in other fields,(21) simulations of trial datasets could be undertaken to probe the utility of different statistical approaches for validation of surrogate endpoints in osteoporosis trials. Additional clinical studies are needed, and sponsors of clinical trials with fractures as endpoints are encouraged to include promising surrogate endpoints as outcomes. Moreover, if meta-analyses are to be undertaken, it is imperative that guidelines for standardized image acquisition and analyses be developed so that data can be combined across trials. Finally, it is time to open discussions with regulatory authorities to present the arguments and strategy for development of surrogate endpoints for fractures in osteoporosis trials. The number of individuals suffering from osteoporosis is growing worldwide, and despite current availability of drugs that reduce fracture risk, there is still a need to develop novel therapeutics that are even more efficacious, are more convenient, and have improved safety and tolerability profiles.
CONCLUSIONS
In this perspective, we suggest there is an urgent need to develop surrogate endpoints for fracture and have outlined an approach to validate the use of biomarkers as surrogate endpoints in osteoporosis. To ensure optimal development and best use of biomarkers to accelerate drug development, continuous dialog among the health professionals, industry, and regulators is of paramount importance. Furthermore, completion of intermediate steps to validate a biomarker as a surrogate endpoint for fracture may also have the benefit of showing the biomarker's use in other clinical areas, such as improved identification of patients at highest risk for fracture and enhanced monitoring of treatment response.
ACKNOWLEDGMENTS
Although the ideas presented in this perspective represent personal opinions of the authors, the authors thank the informative discussions held during the NIH-sponsored workshop between industry and academic investigators in December 2005, which provided the inspiration for this perspective. In particular, we acknowledge Dr Gayle Lester of the National Institute of Arthritis and Musculoskeletal Diseases, who organized this meeting. The authors acknowledge funding from NIH AR053986 and INSERM U831.
Footnotes
The authors state that they have no conflicts of interest.
REFERENCES
- 1.Rosen CJ. Clinical practice. Postmenopausal osteoporosis. N Engl J Med. 2005;353:595–603. doi: 10.1056/NEJMcp043801. [DOI] [PubMed] [Google Scholar]
- 2.Caro JJ, Ishak KJ, Huybrechts KF, Raggio G, Naujoks C. The impact of compliance with osteoporosis therapy on fracture rates in actual practice. Osteoporos Int. 2004;15:1003–1008. doi: 10.1007/s00198-004-1652-z. [DOI] [PubMed] [Google Scholar]
- 3.Siris ES, Harris ST, Rosen CJ, Barr CE, Arvesen JN, Abbott TA, Silverman S. Adherence to bisphosphonate therapy and fracture rates in osteoporotic women: Relationship to vertebral and nonvertebral fractures from 2 US claims databases. Mayo Clin Proc. 2006;81:1013–1022. doi: 10.4065/81.8.1013. [DOI] [PubMed] [Google Scholar]
- 4.Committee for Medicinal Products for Human Use. London, UK: European Medicines Agency; 2006. Guideline on the Evaluation of Medicinal Products in the Treatment of Primary Osteoporosis. [Google Scholar]
- 5.Food and Drug Administration. Washington, DC, USA: Food and Drug Administration; 1994. Guidelines for Preclinical and Clinical Evaluation of Agents Used in the Prevention or Treament of Postmenopausal Osteoporosis. [Google Scholar]
- 6.Delmas PD, Calvo G, Boers M, Abadie E, Avouac B, Kahan A, Kaufman JM, Laslop A, Lekkerkerker JF, Nilsson P, Van Zwieten-Boot B, Kreutz G, Reginster JY. The use of placebo-controlled and non-inferiority trials for the evaluation of new drugs in the treatment of postmenopausal osteoporosis. Osteoporos Int. 2002;13:1–5. doi: 10.1007/s198-002-8331-3. [DOI] [PubMed] [Google Scholar]
- 7.Brody BA, Dickey N, Ellenberg SS, Heaney RP, Levine RJ, O'Brien RL, Purtilo RB, Weijer C. Is the use of placebo controls ethically permissible in clinical trials of agents intended to reduce fractures in osteoporosis. J Bone Miner Res. 2003;18:1105–1109. doi: 10.1359/jbmr.2003.18.6.1105. [DOI] [PubMed] [Google Scholar]
- 8.Berns B, Démolis P, Scheulen M. How can biomarkers become surrogate endpoints. Eur J Cancer. 2007;5:37–40. [Google Scholar]
- 9.Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: Preferred definitions and conceptual framework. Clin Pharmacol Ther. 2001;69:89–95. doi: 10.1067/mcp.2001.113989. [DOI] [PubMed] [Google Scholar]
- 10.De Gruttola VG, Clax P, DeMets DL, Downing GJ, Ellenberg SS, Friedman L, Gail MH, Prentice R, Wittes J, Zeger SL. Considerations in the evaluation of surrogate endpoints in clinical trials. summary of a National Institutes of Health workshop. Control Clin Trials. 2001;22:485–502. doi: 10.1016/s0197-2456(01)00153-2. [DOI] [PubMed] [Google Scholar]
- 11.Abadie E, Ethgen D, Avouac B, Bouvenot G, Branco J, Bruyere O, Calvo G, Devogelaer JP, Dreiser RL, Herrero-Beaumont G, Kahan A, Kreutz G, Laslop A, Lemmel EM, Nuki G, De Van Putte L, Vanhaelst L, Reginster JY. Recommendations for the use of new methods to assess the efficacy of disease-modifying drugs in the treatment of osteoarthritis. Osteoarthritis Cartilage. 2004;12:263–268. doi: 10.1016/j.joca.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 12.Temple R. Are surrogate markers adequate to assess cardiovascular disease drugs. JAMA. 1999;282:790–795. doi: 10.1001/jama.282.8.790. [DOI] [PubMed] [Google Scholar]
- 13.Palmeri S. Clincal surrogate endpoints. Eur J Cancer. 2007;5:44–45. [Google Scholar]
- 14.Alonso A, Molenberghs G, Burzykowski T, Renard D, Geys H, Shkedy Z, Tibaldi F, Abrahantes JC, Buyse M. Prentice's approach and the meta-analytic paradigm: A reflection on the role of statistics in the evaluation of surrogate endpoints. Biometrics. 2004;60:724–728. doi: 10.1111/j.0006-341X.2004.00222.x. [DOI] [PubMed] [Google Scholar]
- 15.Wagner JA, Williams SA, Webster CJ. Biomarkers and surrogate end points for fit-for-purpose development and regulatory evaluation of new drugs. Clin Pharmacol Ther. 2007;81:104–107. doi: 10.1038/sj.clpt.6100017. [DOI] [PubMed] [Google Scholar]
- 16.Prentice RL. Surrogate endpoints in clinical trials: Definition and operational criteria. Stat Med. 1989;8:431–440. doi: 10.1002/sim.4780080407. [DOI] [PubMed] [Google Scholar]
- 17.Freedman LS, Graubard BI, Schatzkin A. Statistical validation of intermediate endpoints for chronic diseases. Stat Med. 1992;11:167–178. doi: 10.1002/sim.4780110204. [DOI] [PubMed] [Google Scholar]
- 18.Lin DY, Fleming TR, De Gruttola V. Estimating the proportion of treatment effect explained by a surrogate marker. Stat Med. 1997;16:1515–1527. doi: 10.1002/(sici)1097-0258(19970715)16:13<1515::aid-sim572>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 19.Buyse M, Molenberghs G. Criteria for the validation of surrogate endpoints in randomized experiments. Biometrics. 1998;54:1014–1029. [PubMed] [Google Scholar]
- 20.Hughes MD. Evaluating surrogate endpoints. Control Clin Trials. 2002;23:703–707. doi: 10.1016/s0197-2456(02)00264-7. [DOI] [PubMed] [Google Scholar]
- 21.Lassere M, Johnson K, Hughes M, Altman D, Buyse M, Galbraith S, Wells G. Simulation studies of surrogate endpoint validation using single trial and multitrial statistical approaches. J Rheumatol. 2007;34:616–619. [PubMed] [Google Scholar]
- 22.Daniels MJ, Hughes MD. Meta-analysis for the evaluation of potential surrogate markers. Stat Med. 1997;16:1965–1982. doi: 10.1002/(sici)1097-0258(19970915)16:17<1965::aid-sim630>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 23.Gail MH, Pfeiffer R, Van Houwelingen HC, Carroll RJ. On meta-analytic assessment of surrogate outcomes. Biostatistics. 2000;1:231–246. doi: 10.1093/biostatistics/1.3.231. [DOI] [PubMed] [Google Scholar]
- 24.Buyse M, Molenberghs G, Burzykowski T, Renard D, Geys H. The validation of surrogate endpoints in meta-analyses of randomized experiments. Biostatistics. 2000;1:49–67. doi: 10.1093/biostatistics/1.1.49. [DOI] [PubMed] [Google Scholar]
- 25.Alonso A, Molenberghs G, Geys H, Buyse M, Vangeneugden T. A unifying approach for surrogate marker validation based on Prentice's criteria. Stat Med. 2006;25:205–221. doi: 10.1002/sim.2315. [DOI] [PubMed] [Google Scholar]
- 26.Xu J, Zeger SL. The evaluation of multiple surrogate endpoints. Biometrics. 2001;57:81–87. doi: 10.1111/j.0006-341x.2001.00081.x. [DOI] [PubMed] [Google Scholar]
- 27.Alonso A, Molenberghs G. Surrogate marker evaluation from an information theory perspective. Biometrics. 2007;63:180–186. doi: 10.1111/j.1541-0420.2006.00634.x. [DOI] [PubMed] [Google Scholar]
- 28.Baker SG, Kramer BS. A perfect correlate does not a surrogate make. BMC Med Res Methodol. 2003;3:16. doi: 10.1186/1471-2288-3-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bouxsein ML. Determinants of skeletal fragility. Best Pract Res Clin Rheumatol. 2005;19:897–911. doi: 10.1016/j.berh.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 30.Seeman E, Delmas PD. Bone quality–the material and structural basis of bone strength and fragility. N Engl J Med. 2006;354:2250–2261. doi: 10.1056/NEJMra053077. [DOI] [PubMed] [Google Scholar]
- 31.Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ. 1996;312:1254–1259. doi: 10.1136/bmj.312.7041.1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Johnell O, Kanis JA, Oden A, Johansson H, De Laet C, Delmas P, Eisman JA, Fujiwara S, Kroger H, Mellstrom D, Meunier PJ, Melton LJ, III, O'Neill T, Pols H, Reeve J, Silman A, Tenenhouse A. Predictive value of BMD for hip and other fractures. J Bone Miner Res. 2005;20:1185–1194. doi: 10.1359/JBMR.050304. [DOI] [PubMed] [Google Scholar]
- 33.Garnero P, Hausherr E, Chapuy MC, Marcelli C, Grandjean H, Muller C, Cormier C, Breart G, Meunier PJ, Delmas PD. Markers of bone resorption predict hip fracture in elderly women: The EPIDOS Prospective Study. J Bone Miner Res. 1996;11:1531–1538. doi: 10.1002/jbmr.5650111021. [DOI] [PubMed] [Google Scholar]
- 34.Bouxsein ML, Palermo L, Yeung C, Black DM. Digital X-ray radiogrammetry predicts hip, wrist and vertebral fracture risk in elderly women: A prospective analysis from the study of osteoporotic fractures. Osteoporos Int. 2002;13:358–365. doi: 10.1007/s001980200040. [DOI] [PubMed] [Google Scholar]
- 35.Prentice R. A case-cohort design for epidemiologic cohort studies and disease prevention trials. Biometrika. 1986;73:1–11. [Google Scholar]
- 36.Moro M, Hecker AT, Bouxsein ML, Myers ER. Failure load of thoracic vertebrae correlates with lumbar bone mineral density measured by DXA. Calcif Tissue Int. 1995;56:206–209. doi: 10.1007/BF00298611. [DOI] [PubMed] [Google Scholar]
- 37.Cheng XG, Lowet G, Boonen S, Nicholson PH, Brys P, Nijs J, Dequeker J. Assessment of the strength of proximal femur in vitro: Relationship to femoral bone mineral density and femoral geometry. Bone. 1997;20:213–218. doi: 10.1016/s8756-3282(96)00383-3. [DOI] [PubMed] [Google Scholar]
- 38.Bouxsein ML, Coan BS, Lee SC. Prediction of the strength of the elderly proximal femur by bone mineral density and quantitative ultrasound measurements of the heel and tibia. Bone. 1999;25:49–54. doi: 10.1016/s8756-3282(99)00093-9. [DOI] [PubMed] [Google Scholar]
- 39.Lochmuller EM, Burklein D, Kuhn V, Glaser C, Muller R, Gluer CC, Eckstein F. Mechanical strength of the thoracolumbar spine in the elderly: Prediction from in situ dual-energy X-ray absorptiometry, quantitative computed tomography (QCT), upper and lower limb peripheral QCT, and quantitative ultrasound. Bone. 2002;31:77–84. doi: 10.1016/s8756-3282(02)00792-5. [DOI] [PubMed] [Google Scholar]
- 40.Lochmuller EM, Muller R, Kuhn V, Lill CA, Eckstein F. Can novel clinical densitometric techniques replace or improve DXA in predicting bone strength in osteoporosis at the hip and other skeletal sites. J Bone Miner Res. 2003;18:906–912. doi: 10.1359/jbmr.2003.18.5.906. [DOI] [PubMed] [Google Scholar]
- 41.Eckstein F, Lochmuller EM, Lill CA, Kuhn V, Schneider E, Delling G, Muller R. Bone strength at clinically relevant sites displays substantial heterogeneity and is best predicted from site-specific bone densitometry. J Bone Miner Res. 2002;17:162–171. doi: 10.1359/jbmr.2002.17.1.162. [DOI] [PubMed] [Google Scholar]
- 42.Cummings SR, Cawthon PM, Ensrud KE, Cauley JA, Fink HA, Orwoll ES. BMD and risk of hip and nonvertebral fractures in older men: A prospective study and comparison with older women. J Bone Miner Res. 2006;21:1550–1556. doi: 10.1359/jbmr.060708. [DOI] [PubMed] [Google Scholar]
- 43.Kanis JA, Oden A, Johnell O, Johansson H, De Laet C, Brown J, Burckhardt P, Cooper C, Christiansen C, Cummings S, Eisman JA, Fujiwara S, Gluer C, Goltzman D, Hans D, Krieg MA, La Croix A, McCloskey E, Mellstrom D, Melton LJ, III, Pols H, Reeve J, Sanders K, Schott AM, Silman A, Torgerson D, van Staa T, Watts NB, Yoshimura N. The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int. 2007;18:1033–1046. doi: 10.1007/s00198-007-0343-y. [DOI] [PubMed] [Google Scholar]
- 44.Cummings SR, Bates D, Black DM. Clinical use of bone densitometry: Scientific review. JAMA. 2002;288:1889–1897. doi: 10.1001/jama.288.15.1889. [DOI] [PubMed] [Google Scholar]
- 45.Lindsay R. Estrogen therapy in the prevention and management of osteoporosis. Am J Obstet Gynecol. 1987;156:1347–1351. doi: 10.1016/0002-9378(87)90177-3. [DOI] [PubMed] [Google Scholar]
- 46.Ettinger B. Use of low-dosage 17 beta-estradiol for the prevention of osteoporosis. Clin Ther. 1993;15:950–962. [PubMed] [Google Scholar]
- 47.Cooper C, Stakkestad JA, Radowicki S, Hardy P, Pilate C, Dain MP, Delmas PD. Matrix delivery transdermal 17beta-estradiol for the prevention of bone loss in postmenopausal women. The International Study Group. Osteoporos Int. 1999;9:358–366. doi: 10.1007/s001980050159. [DOI] [PubMed] [Google Scholar]
- 48.Delmas PD, Bjarnason NH, Mitlak BH, Ravoux AC, Shah AS, Huster WJ, Draper M, Christiansen C. Effects of raloxifene on bone mineral density, serum cholesterol concentrations, and uterine endometrium in postmenopausal women. N Engl J Med. 1997;337:1641–1647. doi: 10.1056/NEJM199712043372301. [DOI] [PubMed] [Google Scholar]
- 49.Rossini M, Gatti D, Zamberlan N, Braga V, Dorizzi R, Adami S. Long-term effects of a treatment course with oral alendronate of postmenopausal osteoporosis. J Bone Miner Res. 1994;9:1833–1837. doi: 10.1002/jbmr.5650091121. [DOI] [PubMed] [Google Scholar]
- 50.Chesnut CH, III, McClung MR, Ensrud KE, Bell NH, Genant HK, Harris ST, Singer FR, Stock JL, Yood RA, Delmas PD, Kher U, Pryor-Tillotson S, Santora AC. Alendronate treatment of the postmenopausal osteoporotic woman: Effect of multiple dosages on bone mass and bone remodeling. Am J Med. 1995;99:144–152. doi: 10.1016/s0002-9343(99)80134-x. [DOI] [PubMed] [Google Scholar]
- 51.Liberman UA, Weiss SR, Broll J, Minne HW, Quan H, Bell NH, Rodriguez-Portales J, Downs RW, Jr, Dequeker J, Favus M. Effect of oral alendronate on bone mineral density and the incidence of fractures in postmenopausal osteoporosis. The Alendronate Phase III Osteoporosis Treatment Study Group. N Engl J Med. 1995;333:1437–1443. doi: 10.1056/NEJM199511303332201. [DOI] [PubMed] [Google Scholar]
- 52.Mortensen L, Charles P, Bekker PJ, Digennaro J, Johnston CC., Jr Risedronate increases bone mass in an early postmenopausal population: Two years of treatment plus one year of follow-up. J Clin Endocrinol Metab. 1998;83:396–402. doi: 10.1210/jcem.83.2.4586. [DOI] [PubMed] [Google Scholar]
- 53.McClung MR, Geusens P, Miller PD, Zippel H, Bensen WG, Roux C, Adami S, Fogelman I, Diamond T, Eastell R, Meunier PJ, Reginster JY. Effect of risedronate on the risk of hip fracture in elderly women. Hip Intervention Program Study Group. N Engl J Med. 2001;344:333–340. doi: 10.1056/NEJM200102013440503. [DOI] [PubMed] [Google Scholar]
- 54.Ravn P, Clemmesen B, Riis BJ, Christiansen C. The effect on bone mass and bone markers of different doses of ibandronate: A new bisphosphonate for prevention and treatment of postmenopausal osteoporosis: A 1-year, randomized, double-blind, placebo-controlled dose-finding study. Bone. 1996;19:527–533. doi: 10.1016/s8756-3282(96)00229-3. [DOI] [PubMed] [Google Scholar]
- 55.Thiebaud D, Burckhardt P, Kriegbaum H, Huss H, Mulder H, Juttmann JR, Schoter KH. Three monthly intravenous injections of ibandronate in the treatment of postmenopausal osteoporosis. Am J Med. 1997;103:298–307. doi: 10.1016/s0002-9343(97)00249-0. [DOI] [PubMed] [Google Scholar]
- 56.Meunier PJ, Slosman DO, Delmas PD, Sebert JL, Brandi ML, Albanese C, Lorenc R, Pors-Nielsen S, De Vernejoul MC, Roces A, Reginster JY. Strontium ranelate: Dose-dependent effects in established postmenopausal vertebral osteoporosis–a 2-year randomized placebo controlled trial. J Clin Endocrinol Metab. 2002;87:2060–2066. doi: 10.1210/jcem.87.5.8507. [DOI] [PubMed] [Google Scholar]
- 57.Meunier PJ, Roux C, Seeman E, Ortolani S, Badurski JE, Spector TD, Cannata J, Balogh A, Lemmel EM, Pors-Nielsen S, Rizzoli R, Genant HK, Reginster JY. The effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosis. N Engl J Med. 2004;350:459–468. doi: 10.1056/NEJMoa022436. [DOI] [PubMed] [Google Scholar]
- 58.Reginster JY, Seeman E, De Vernejoul MC, Adami S, Compston J, Phenekos C, Devogelaer JP, Curiel MD, Sawicki A, Goemaere S, Sorensen OH, Felsenberg D, Meunier PJ. Strontium ranelate reduces the risk of nonvertebral fractures in postmenopausal women with osteoporosis: Treatment of Peripheral Osteoporosis (TROPOS) study. J Clin Endocrinol Metab. 2005;90:2816–2822. doi: 10.1210/jc.2004-1774. [DOI] [PubMed] [Google Scholar]
- 59.Hodsman AB, Hanley DA, Ettinger MP, Bolognese MA, Fox J, Metcalfe AJ, Lindsay R. Efficacy and safety of human parathyroid hormone-(1-84) in increasing bone mineral density in postmenopausal osteoporosis. J Clin Endocrinol Metab. 2003;88:5212–5220. doi: 10.1210/jc.2003-030768. [DOI] [PubMed] [Google Scholar]
- 60.Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, Hodsman AB, Eriksen EF, Ish-Shalom S, Genant HK, Wang O, Mitlak BH. Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001;344:1434–1441. doi: 10.1056/NEJM200105103441904. [DOI] [PubMed] [Google Scholar]
- 61.Hochberg MC, Ross PD, Black D, Cummings SR, Genant HK, Nevitt MC, Barrett-Connor E, Musliner T, Thompson D. Larger increases in bone mineral density during alendronate therapy are associated with a lower risk of new vertebral fractures in women with postmenopausal osteoporosis. Fracture Intervention Trial Research Group. Arthritis Rheum. 1999;42:1246–1254. doi: 10.1002/1529-0131(199906)42:6<1246::AID-ANR22>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 62.Wasnich RD, Miller PD. Antifracture efficacy of antiresorptive agents are related to changes in bone density. J Clin Endocrinol Metab. 2000;85:231–236. doi: 10.1210/jcem.85.1.6267. [DOI] [PubMed] [Google Scholar]
- 63.Cummings SR, Karpf DB, Harris F, Genant HK, Ensrud K, LaCroix AZ, Black DM. Improvement in spine bone density and reduction in risk of vertebral fractures during treatment with antiresorptive drugs. Am J Med. 2002;112:281–289. doi: 10.1016/s0002-9343(01)01124-x. [DOI] [PubMed] [Google Scholar]
- 64.Sarkar S, Mitlak BH, Wong M, Stock JL, Black DM, Harper KD. Relationships between bone mineral density and incident vertebral fracture risk with raloxifene therapy. J Bone Miner Res. 2002;17:1–10. doi: 10.1359/jbmr.2002.17.1.1. [DOI] [PubMed] [Google Scholar]
- 65.Li Z, Meredith MP, Hoseyni MS. A method to assess the proportion of treatment effect explained by a surrogate endpoint. Stat Med. 2001;20:3175–3188. doi: 10.1002/sim.984. [DOI] [PubMed] [Google Scholar]
- 66.Hochberg MC, Greenspan S, Wasnich RD, Miller P, Thompson DE, Ross PD. Changes in bone density and turnover explain the reductions in incidence of nonvertebral fractures that occur during treatment with antiresorptive agents. J Clin Endocrinol Metab. 2002;87:1586–1592. doi: 10.1210/jcem.87.4.8415. [DOI] [PubMed] [Google Scholar]
- 67.Sarkar S, Reginster JY, Crans GG, Diez-Perez A, Pinette KV, Delmas PD. Relationship between changes in biochemical markers of bone turnover and BMD to predict vertebral fracture risk. J Bone Miner Res. 2004;19:394–401. doi: 10.1359/JBMR.0301243. [DOI] [PubMed] [Google Scholar]
- 68.Delmas P, Seeman E. Changes in bone mineral density explain little of the reduction in vertebral or nonvertebral fracture risk with anti-resorptive therapy. Bone. 2004;34:599–604. doi: 10.1016/j.bone.2003.12.022. [DOI] [PubMed] [Google Scholar]
- 69.Chen P, Miller PD, Delmas PD, Misurski DA, Krege JH. Change in lumbar spine BMD and vertebral fracture risk reduction in teriparatide-treated postmenopausal women with osteoporosis. J Bone Miner Res. 2006;21:1785–1790. doi: 10.1359/jbmr.060802. [DOI] [PubMed] [Google Scholar]
- 70.Bruyere O, Roux C, Detilleux J, Slosman DO, Spector TD, Fardellone P, Brixen K, Devogelaer JP, Diaz-Curiel M, Albanese C, Kaufman JM, Pors-Nielsen S, Reginster JY. Relationship between bone mineral density changes and fracture risk reduction in patients treated with strontium ranelate. J Clin Endocrinol Metab. 2007;92:3076–3081. doi: 10.1210/jc.2006-2758. [DOI] [PubMed] [Google Scholar]
- 71.Bruyere O, Roux C, Badurski J, Isaia G, de Vernejoul MC, Cannata J, Ortolani S, Slosman D, Detilleux J, Reginster JY. Relationship between change in femoral neck bone mineral density and hip fracture incidence during treatment with strontium ranelate. Curr Med Res Opin. 2007;23:3041–3045. doi: 10.1185/030079907X242818. [DOI] [PubMed] [Google Scholar]
- 72.Garnero P, Sornay-Rendu E, Chapuy MC, Delmas PD. Increased bone turnover in late postmenopausal women is a major determinant of osteoporosis. J Bone Miner Res. 1996;11:337–349. doi: 10.1002/jbmr.5650110307. [DOI] [PubMed] [Google Scholar]
- 73.Sherman SS, Tobin JD, Hollis BW, Gundberg CM, Roy TA, Plato CC. Biochemical parameters associated with low bone density in healthy men and women. J Bone Miner Res. 1992;7:1123–1130. doi: 10.1002/jbmr.5650071003. [DOI] [PubMed] [Google Scholar]
- 74.Stepan JJ. Prediction of bone loss in postmenopausal women. Osteoporos Int. 2000;11(Suppl 6):S45–S54. doi: 10.1007/s001980070005. [DOI] [PubMed] [Google Scholar]
- 75.Christiansen C, Riis BJ, Rodbro P. Prediction of rapid bone loss in postmenopausal women. Lancet. 1987;1:1105–1108. doi: 10.1016/s0140-6736(87)91671-0. [DOI] [PubMed] [Google Scholar]
- 76.Dresner-Pollak R, Parker RA, Poku M, Thompson J, Seibel MJ, Greenspan SL. Biochemical markers of bone turnover reflect femoral bone loss in elderly women. Calcif Tissue Int. 1996;59:328–333. doi: 10.1007/s002239900135. [DOI] [PubMed] [Google Scholar]
- 77.Ross PD, Knowlton W. Rapid bone loss is associated with increased levels of biochemical markers. J Bone Miner Res. 1998;13:297–302. doi: 10.1359/jbmr.1998.13.2.297. [DOI] [PubMed] [Google Scholar]
- 78.Garnero P, Sornay-Rendu E, Duboeuf F, Delmas PD. Markers of bone turnover predict postmenopausal forearm bone loss over 4 years: The OFELY study. J Bone Miner Res. 1999;14:1614–1621. doi: 10.1359/jbmr.1999.14.9.1614. [DOI] [PubMed] [Google Scholar]
- 79.Lofman O, Magnusson P, Toss G, Larsson L. Common biochemical markers of bone turnover predict future bone loss: A 5-year follow-up study. Clin Chim Acta. 2005;356:67–75. doi: 10.1016/j.cccn.2004.12.014. [DOI] [PubMed] [Google Scholar]
- 80.Lenora J, Ivaska KK, Obrant KJ, Gerdhem P. Prediction of bone loss using biochemical markers of bone turnover. Osteoporos Int. 2007;18:1297–1305. doi: 10.1007/s00198-007-0379-z. [DOI] [PubMed] [Google Scholar]
- 81.Garnero P, Sornay-Rendu E, Claustrat B, Delmas PD. Biochemical markers of bone turnover, endogenous hormones and the risk of fractures in postmenopausal women: The OFELY study. J Bone Miner Res. 2000;15:1526–1536. doi: 10.1359/jbmr.2000.15.8.1526. [DOI] [PubMed] [Google Scholar]
- 82.Ross PD, Kress BC, Parson RE, Wasnich RD, Armour KA, Mizrahi IA. Serum bone alkaline phosphatase and calcaneus bone density predict fractures: A prospective study. Osteoporos Int. 2000;11:76–82. doi: 10.1007/s001980050009. [DOI] [PubMed] [Google Scholar]
- 83.Garnero P, Cloos P, Sornay-Rendu E, Qvist P, Delmas P. Type I collagen racemization and isomerization and the irsk of fracture in postmenopausal women: The OFELY prospective study. J Bone Miner Res. 2002;17:826–833. doi: 10.1359/jbmr.2002.17.5.826. [DOI] [PubMed] [Google Scholar]
- 84.Bruyere O, Collette J, Delmas P, Rouillon A, Roux C, Seidel L, Richy F, Reginster JY. Interest of biochemical markers of bone turnover for long-term prediction of new vertebral fracture in postmenopausal osteoporotic women. Maturitas. 2003;44:259–265. doi: 10.1016/s0378-5122(03)00042-2. [DOI] [PubMed] [Google Scholar]
- 85.Melton LJ, III, Crowson CS, O'Fallon WM, Wahner HW, Riggs BL. Relative contributions of bone density, bone turnover, and clinical risk factors to long-term fracture prediction. J Bone Miner Res. 2003;18:312–318. doi: 10.1359/jbmr.2003.18.2.312. [DOI] [PubMed] [Google Scholar]
- 86.Gerdhem P, Ivaska KK, Alatalo SL, Halleen JM, Hellman J, Isaksson A, Pettersson K, Vaananen HK, Akesson K, Obrant KJ. Biochemical markers of bone metabolism and prediction of fracture in elderly women. J Bone Miner Res. 2004;19:386–393. doi: 10.1359/JBMR.0301244. [DOI] [PubMed] [Google Scholar]
- 87.Sornay-Rendu E, Munoz F, Garnero P, Duboeuf F, Delmas PD. Identification of osteopenic women at high risk of fracture: The OFELY study. J Bone Miner Res. 2005;20:1813–1819. doi: 10.1359/JBMR.050609. [DOI] [PubMed] [Google Scholar]
- 88.Meier C, Nguyen TV, Center JR, Seibel MJ, Eisman JA. Bone resorption and osteoporotic fractures in elderly men: The dubbo osteoporosis epidemiology study. J Bone Miner Res. 2005;20:579–587. doi: 10.1359/JBMR.041207. [DOI] [PubMed] [Google Scholar]
- 89.Ivaska KK, Gerdhem P, Akesson K, Obrant KJ. Bone turnover markers and prediction of fracture: Nine year follow-up study of 1040 elderly women. J Bone Miner Res. 2007;22(S1):S21. doi: 10.1359/jbmr.091006. [DOI] [PubMed] [Google Scholar]
- 90.Chapurlat RD, Garnero P, Brart G, Meunier PJ, Delmas PD. Serum type I collagen breakdown product (serum CTX) predicts hip fracture risk in elderly women: The EPIDOS study. Bone. 2000;27:283–286. doi: 10.1016/s8756-3282(00)00325-2. [DOI] [PubMed] [Google Scholar]
- 91.Chen JS, Seibel MJ, Zochling J, March L, Cameron ID, Cumming RG, Schwarz J, Simpson JM, Sambrook PN. Calcaneal ultrasound but not bone turnover predicts fractures in vitamin D deficient frail elderly at high risk of falls. Calcif Tissue Int. 2006;79:37–42. doi: 10.1007/s00223-005-0287-1. [DOI] [PubMed] [Google Scholar]
- 92.Garnero P, Dargent-Molina P, Hans D, Schott AM, Breart G, Meunier PJ, Delmas PD. Do markers of bone resorption add to bone mineral density and ultrasonographic heel measurement for the prediction of hip fracture in elderly women? The EPIDOS prospective study. Osteoporos Int. 1998;8:563–569. doi: 10.1007/s001980050100. [DOI] [PubMed] [Google Scholar]
- 93.van Daele PL, Seibel MJ, Burger H, Hofman A, Grobbee DE, van Leeuwen JP, Birkenhager JC, Pols HA. Case-control analysis of bone resorption markers, disability, and hip fracture risk: The Rotterdam study. BMJ. 1996;312:482–483. doi: 10.1136/bmj.312.7029.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Delmas PD, Pornel B, Felsenberg D, Garnero P, Hardy P, Pilate C, Dain MP. A dose-ranging trial of a matrix transdermal 17beta-estradiol for the prevention of bone loss in early postmenopausal women. International Study Group. Bone. 1999;24:517–523. doi: 10.1016/s8756-3282(99)00076-9. [DOI] [PubMed] [Google Scholar]
- 95.Prestwood KM, Kenny AM, Unson C, Kulldorff M. The effect of low dose micronized 17ss-estradiol on bone turnover, sex hormone levels, and side effects in older women: A randomized, double blind, placebo-controlled study. J Clin Endocrinol Metab. 2000;85:4462–4469. doi: 10.1210/jcem.85.12.7001. [DOI] [PubMed] [Google Scholar]
- 96.Harris ST, Gertz BJ, Genant HK, Eyre DR, Survill TT, Ventura JN, DeBrock J, Ricerca E, Chesnut CH., III The effect of short term treatment with alendronate on vertebral density and biochemical markers of bone remodeling in early postmenopausal women. J Clin Endocrinol Metab. 1993;76:1399–1406. doi: 10.1210/jcem.76.6.8501142. [DOI] [PubMed] [Google Scholar]
- 97.Christiansen C, Tanko LB, Warming L, Moelgaard A, Christgau S, Qvist P, Baumann M, Wieczorek L, Hoyle N. Dose dependent effects on bone resorption and formation of intermittently administered intravenous ibandronate. Osteoporos Int. 2003;14:609–613. doi: 10.1007/s00198-003-1409-0. [DOI] [PubMed] [Google Scholar]
- 98.McClung MR, Lewiecki EM, Cohen SB, Bolognese MA, Woodson GC, Moffett AH, Peacock M, Miller PD, Lederman SN, Chesnut CH, Lain D, Kivitz AJ, Holloway DL, Zhang C, Peterson MC, Bekker PJ. Denosumab in postmenopausal women with low bone mineral density. N Engl J Med. 2006;354:821–831. doi: 10.1056/NEJMoa044459. [DOI] [PubMed] [Google Scholar]
- 99.Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, Cosman F, Lakatos P, Leung PC, Man Z, Mautalen C, Mesenbrink P, Hu H, Caminis J, Tong K, Rosario-Jansen T, Krasnow J, Hue TF, Sellmeyer D, Eriksen EF, Cummings SR. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007;356:1809–1822. doi: 10.1056/NEJMoa067312. [DOI] [PubMed] [Google Scholar]
- 100.Lindsay R, Zhou H, Cosman F, Nieves J, Dempster DW, Hodsman AB. Effects of a one-month treatment with PTH(1-34) on bone formation on cancellous, endocortical, and periosteal surfaces of the human ilium. J Bone Miner Res. 2007;22:495–502. doi: 10.1359/jbmr.070104. [DOI] [PubMed] [Google Scholar]
- 101.Lindsay R, Nieves J, Formica C, Henneman E, Woelfert L, Shen V, Dempster D, Cosman F. Randomised controlled study of effect of parathyroid hormone on vertebral-bone mass and fracture incidence among postmenopausal women on oestrogen with osteoporosis. Lancet. 1997;350:550–555. doi: 10.1016/S0140-6736(97)02342-8. [DOI] [PubMed] [Google Scholar]
- 102.Chen P, Satterwhite JH, Licata AA, Lewiecki EM, Sipos AA, Misurski DM, Wagman RB. Early changes in biochemical markers of bone formation predict BMD response to teriparatide in postmenopausal women with osteoporosis. J Bone Miner Res. 2005;20:962–970. doi: 10.1359/JBMR.050105. [DOI] [PubMed] [Google Scholar]
- 103.Bauer DC, Garnero P, Bilezikian JP, Greenspan SL, Ensrud KE, Rosen CJ, Palermo L, Black DM. Short-term Changes in Bone Turnover Markers and Bone Mineral Density Response to Parathyroid Hormone in Postmenopausal Women with Osteoporosis. J Clin Endocrinol Metab. 2006 doi: 10.1210/jc.2005-1712. [DOI] [PubMed] [Google Scholar]
- 104.Delmas P, Watts NB, Miller P, Cahall D, Bilezikian J, Lindsay R. Bone turnover markers demonstrate greater earlier responsiveness to teriparatide following treatment with risedronate compared with alendronate: The OPTAMISE study. J Bone Miner Res. 2007;22(S1):S27. [Google Scholar]
- 105.Bjarnason NH, Sarkar S, Duong T, Mitlak B, Delmas PD, Christiansen C. Six and twelve month changes in bone turnover are related to reduction in vertebral fracture risk during 3 years of raloxifene treatment in postmenopausal osteoporosis. Osteoporos Int. 2001;12:922–930. doi: 10.1007/s001980170020. [DOI] [PubMed] [Google Scholar]
- 106.Eastell R, Barton I, Hannon R, Chines A, Garnero P, Delmas P. Relationship of early changes in bone resorption to the reduction in fracture risk with risedronate. J Bone Miner Res. 2003;18:1051–1056. doi: 10.1359/jbmr.2003.18.6.1051. [DOI] [PubMed] [Google Scholar]
- 107.Reginster JY, Sarkar S, Zegels B, Henrotin Y, Bruyere O, Agnusdei D, Collette J. Reduction in PINP, a marker of bone metabolism, with raloxifene treatment and its relationship with vertebral fracture risk. Bone. 2004;34:344–351. doi: 10.1016/j.bone.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 108.Bauer DC, Black DM, Garnero P, Hochberg M, Ott S, Orloff J, Thompson DE, Ewing SK, Delmas PD. Change in bone turnover and hip, non-spine, and vertebral fracture in alendronate-treated women: The fracture intervention trial. J Bone Miner Res. 2004;19:1250–1258. doi: 10.1359/JBMR.040512. [DOI] [PubMed] [Google Scholar]
- 109.Eastell R, Hannon RA, Garnero P, Campbell MJ, Delmas PD. Relationship of early changes in bone resorption to the reduction in fracture risk with risedronate: Review of statistical analysis. J Bone Miner Res. 2007;22:1656–1660. doi: 10.1359/jbmr.07090b. [DOI] [PubMed] [Google Scholar]
- 110.Delmas PD, Li Z, Cooper C. Relationship between changes in bone mineral density and fracture risk reduction with antiresorptive drugs: Some issues with meta-analyses. J Bone Miner Res. 2004;19:330–337. doi: 10.1359/JBMR.0301228. [DOI] [PubMed] [Google Scholar]
- 111.Bouxsein M. Biomechanics of age-related fractures. In: Marcus R, Feldman D, Nelson D, Rosen C, editors. Osteoporosis. 3rd ed. vol I. San Diego, CA, USA: Elsevier Academic Press; 2007. pp. 601–616. [Google Scholar]
- 112.Lang TF, Keyak JH, Heitz MW, Augat P, Lu Y, Mathur A, Genant HK. Volumetric quantitative computed tomography of the proximal femur: Precision and relation to bone strength. Bone. 1997;21:101–108. doi: 10.1016/s8756-3282(97)00072-0. [DOI] [PubMed] [Google Scholar]
- 113.Cody DD, Gross GJ, Hou FJ, Spencer HJ, Goldstein SA, Fyhrie DP. Femoral strength is better predicted by finite element models than QCT and DXA. J Biomech. 1999;32:1013–1020. doi: 10.1016/s0021-9290(99)00099-8. [DOI] [PubMed] [Google Scholar]
- 114.Bousson V, Le Bras A, Roqueplan F, Kang Y, Mitton D, Kolta S, Bergot C, Skalli W, Vicaut E, Kalender W, Engelke K, Laredo JD. Volumetric quantitative computed tomography of the proximal femur: Relationships linking geometric and densitometric variables to bone strength. Role for compact bone. Osteoporos Int. 2006;17:855–864. doi: 10.1007/s00198-006-0074-5. [DOI] [PubMed] [Google Scholar]
- 115.Brinckmann P, Biggeman M, Hilweg D. Prediction of the compressive strength of human lumbar vertebrae. Clin Biomech (Bristol, Avon) 1989;4:S1–S27. doi: 10.1016/0268-0033(89)90071-5. [DOI] [PubMed] [Google Scholar]
- 116.Cheng XG, Nicholson PH, Boonen S, Lowet G, Brys P, Aerssens J, Van der Perre G, Dequeker J. Prediction of vertebral strength in vitro by spinal bone densitometry and calcaneal ultrasound. J Bone Miner Res. 1997;12:1721–1728. doi: 10.1359/jbmr.1997.12.10.1721. [DOI] [PubMed] [Google Scholar]
- 117.Eckstein F, Fischbeck M, Kuhn V, Link TM, Priemel M, Lochmuller EM. Determinants and heterogeneity of mechanical competence throughout the thoracolumbar spine of elderly women and men. Bone. 2004;35:364–374. doi: 10.1016/j.bone.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 118.Crawford RP, Brouwers J, Keaveny TM. Accurate prediction of vertebral strength using voxel-based non-linear finite element models. Trans Orthop Res. 2004;29:1123. [Google Scholar]
- 119.Buckley JM, Cheng L, Loo K, Slyfield C, Xu Z. Quantitative computed tomography-based predictions of vertebral strength in anterior bending. Spine. 2007;32:1019–1027. doi: 10.1097/01.brs.0000260979.98101.9c. [DOI] [PubMed] [Google Scholar]
- 120.Buckley JM, Loo K, Motherway J. Comparison of quantitative computed tomography-based measures in predicting vertebral compressive strength. Bone. 2007;40:767–774. doi: 10.1016/j.bone.2006.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Mackey DC, Eby JG, Harris F, Taaffe DR, Cauley JA, Tylavsky FA, Harris TB, Lang TF, Cummings SR. Prediction of clinical non-spine fractures in older black and white men and women with volumetric BMD of the spine and areal BMD of the hip: The Health, Aging, and Body Composition Study*. J Bone Miner Res. 2007;22:1862–1868. doi: 10.1359/jbmr.070807. [DOI] [PubMed] [Google Scholar]
- 122.Ott SM, Kilcoyne RF, Chestnut CH. Ability of four different techniques of measuring bone mass to diagnose vertebral fractures in postmenopausal women. J Bone Miner Res. 1987;2:201–210. doi: 10.1002/jbmr.5650020306. [DOI] [PubMed] [Google Scholar]
- 123.Cody DD, Hou FJ, Divine GW, Fyhrie DP. Femoral structure and stiffness in patients with femoral neck fracture. J Orthop Res. 2000;18:443–448. doi: 10.1002/jor.1100180317. [DOI] [PubMed] [Google Scholar]
- 124.Bergot C, Laval-Jeantet AM, Hutchinson K, Dautraix I, Caulin F, Genant HK. A comparison of spinal quantitative computed tomography with dual energy X-ray absorptiometry in European women with vertebral and nonvertebral fractures. Calcif Tissue Int. 2001;68:74–82. doi: 10.1007/BF02678144. [DOI] [PubMed] [Google Scholar]
- 125.Lang TF, Guglielmi G, van Kuijk C, De Serio A, Cammisa M, Genant HK. Measurement of bone mineral density at the spine and proximal femur by volumetric quantitative computed tomography and dual-energy X-ray absorptiometry in elderly women with and without vertebral fractures. Bone. 2002;30:247–250. doi: 10.1016/s8756-3282(01)00647-0. [DOI] [PubMed] [Google Scholar]
- 126.Rehman Q, Lang T, Modin G, Lane NE. Quantitative computed tomography of the lumbar spine, not dual x-ray absorptiometry, is an independent predictor of prevalent vertebral fractures in postmenopausal women with osteopenia receiving long-term glucocorticoid and hormone-replacement therapy. Arthritis Rheum. 2002;46:1292–1297. doi: 10.1002/art.10277. [DOI] [PubMed] [Google Scholar]
- 127.Cheng X, Li J, Lu Y, Keyak J, Lang T. Proximal femoral density and geometry measurements by quantitative computed tomography: Association with hip fracture. Bone. 2007;40:169–174. doi: 10.1016/j.bone.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 128.Melton LJ, Riggs BL, Keaveny TM, Achenbach SJ, Hoffmann PF, Camp JJ, Rouleau PA, Bouxsein ML, Amin S, Atkinson EJ, Robb RA, Khosla S. Structural determinants of vertebral fracture risk. J Bone Miner Res. 2007;22:1885–1892. doi: 10.1359/jbmr.070728. [DOI] [PubMed] [Google Scholar]
- 129.Rehman Q, Lang TF, Arnaud CD, Modin GW, Lane NE. Daily treatment with parathyroid hormone is associated with an increase in vertebral cross-sectional area in postmenopausal women with glucocorticoid-induced osteoporosis. Osteoporos Int. 2003;14:77–81. doi: 10.1007/s00198-002-1312-0. [DOI] [PubMed] [Google Scholar]
- 130.Black DM, Greenspan SL, Ensrud KE, Palermo L, McGowan JA, Lang TF, Garnero P, Bouxsein ML, Bilezikian JP, Rosen CJ. The effects of parathyroid hormone and alendronate alone or in combination in postmenopausal osteoporosis. N Engl J Med. 2003;349:1207–1215. doi: 10.1056/NEJMoa031975. [DOI] [PubMed] [Google Scholar]
- 131.Finkelstein JS, Hayes A, Hunzelman JL, Wyland JJ, Lee H, Neer RM. The effects of parathyroid hormone, alendronate, or both in men with osteoporosis. N Engl J Med. 2003;349:1216–1226. doi: 10.1056/NEJMoa035725. [DOI] [PubMed] [Google Scholar]
- 132.Genant HK, Lang T, Fuerst T, Pinette KV, Zhou C, Thiebaud D, Diez-Perez A. Treatment with raloxifene for 2 years increases vertebral bone mineral density as measured by volumetric quantitative computed tomography. Bone. 2004;35:1164–1168. doi: 10.1016/j.bone.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 133.McClung MR, San Martin J, Miller PD, Civitelli R, Bandeira F, Omizo M, Donley DW, Dalsky GP, Eriksen EF. Opposite bone remodeling effects of teriparatide and alendronate in increasing bone mass. Arch Intern Med. 2005;165:1762–1768. doi: 10.1001/archinte.165.15.1762. [DOI] [PubMed] [Google Scholar]
- 134.Graeff C, Timm W, Nickelsen TN, Farrerons J, Marin F, Barker C, Gluer CC. Monitoring teriparatide-associated changes in vertebral microstructure by high-resolution CT in vivo: Results from the EUROFORS study. J Bone Miner Res. 2007;22:1426–1433. doi: 10.1359/jbmr.070603. [DOI] [PubMed] [Google Scholar]
- 135.Black DM, Bilezikian JP, Ensrud KE, Greenspan SL, Palermo L, Hue T, Lang TF, McGowan JA, Rosen CJ. One year of alendronate after one year of parathyroid hormone (1-84) for osteoporosis. N Engl J Med. 2005;353:555–565. doi: 10.1056/NEJMoa050336. [DOI] [PubMed] [Google Scholar]
- 136.Parfitt A. Age-related structural changes in trabecular and cortical bone: Cellular mechanicsms and biomechanical consequences. Calcif Tissue Int. 1984;36(Suppl):123–128. doi: 10.1007/BF02406145. [DOI] [PubMed] [Google Scholar]
- 137.Parfitt A. Trabecular bone architecture in the pathogenesis and prevention of fracture. Am J Med. 1987;82:68–72. doi: 10.1016/0002-9343(87)90274-9. [DOI] [PubMed] [Google Scholar]
- 138.Parfitt AM. Implications of architecture for the pathogenesis and prevention of vertebral fracture. Bone. 1992;13(Suppl 2):S41–S47. doi: 10.1016/8756-3282(92)90196-4. [DOI] [PubMed] [Google Scholar]
- 139.Aaron JE, Shore PA, Shore RC, Beneton M, Kanis JA. Trabecular architecture in women and men of similar bone mass with and without vertebral fracture: II. Three-dimensional histology. Bone. 2000;27:277–282. doi: 10.1016/s8756-3282(00)00328-8. [DOI] [PubMed] [Google Scholar]
- 140.Hordon LD, Raisi M, Aaron JE, Paxton SK, Beneton M, Kanis JA. Trabecular architecture in women and men of similar bone mass with and without vertebral fracture: I. Two-dimensional histology. Bone. 2000;27:271–276. doi: 10.1016/s8756-3282(00)00329-x. [DOI] [PubMed] [Google Scholar]
- 141.Legrand E, Chappard D, Pascaretti C, Duquenne M, Krebs S, Rohmer V, Basle MF, Audran M. Trabecular bone microarchitecture, bone mineral density, and vertebral fractures in male osteoporosis. J Bone Miner Res. 2000;15:13–19. doi: 10.1359/jbmr.2000.15.1.13. [DOI] [PubMed] [Google Scholar]
- 142.Majumdar S, Link TM, Augat P, Lin JC, Newitt D, Lane NE, Genant HK. Trabecular bone architecture in the distal radius using magnetic resonance imaging in subjects with fractures of the proximal femur. Magnetic Resonance Science Center and Osteoporosis and Arthritis Research Group. Osteoporos Int. 1999;10:231–239. doi: 10.1007/s001980050221. [DOI] [PubMed] [Google Scholar]
- 143.Link TM, Majumdar S, Augat P, Lin JC, Newitt D, Lu Y, Lane NE, Genant HK. In vivo high resolution MRI of the calcaneus: Differences in trabecular structure in osteoporosis patients. J Bone Miner Res. 1998;13:1175–1182. doi: 10.1359/jbmr.1998.13.7.1175. [DOI] [PubMed] [Google Scholar]
- 144.Link TM, Vieth V, Matheis J, Newitt D, Lu Y, Rummeny EJ, Majumdar S. Bone structure of the distal radius and the calcaneus vs BMD of the spine and proximal femur in the prediction of osteoporotic spine fractures. Eur Radiol. 2002;12:401–408. doi: 10.1007/s003300101127. [DOI] [PubMed] [Google Scholar]
- 145.Wehrli FW, Gomberg BR, Saha PK, Song HK, Hwang SN, Snyder PJ. Digital topological analysis of in vivo magnetic resonance microimages of trabecular bone reveals structural implications of osteoporosis. J Bone Miner Res. 2001;16:1520–1531. doi: 10.1359/jbmr.2001.16.8.1520. [DOI] [PubMed] [Google Scholar]
- 146.Wehrli FW, Hilaire L, Fernandez-Seara M, Gomberg BR, Song HK, Zemel B, Loh L, Snyder PJ. Quantitative magnetic resonance imaging in the calcaneus and femur of women with varying degrees of osteopenia and vertebral deformity status. J Bone Miner Res. 2002;17:2265–2273. doi: 10.1359/jbmr.2002.17.12.2265. [DOI] [PubMed] [Google Scholar]
- 147.Boutroy S, Bouxsein ML, Munoz F, Delmas PD. In vivo assessment of trabecular bone microarchitecture by high-resolution peripheral quantitative computed tomography. J Clin Endocrinol Metab. 2005;90:6508–6515. doi: 10.1210/jc.2005-1258. [DOI] [PubMed] [Google Scholar]
- 148.Sornay-Rendu E, Boutroy S, Munoz F, Delmas PD. Alterations of cortical and trabecular architecture are associated with fractures in postmenopausal women, partially independent of decreased BMD measured by DXA: The OFELY Study. J Bone Miner Res. 2007;22:425–433. doi: 10.1359/jbmr.061206. [DOI] [PubMed] [Google Scholar]
- 149.Melton LJ, Riggs BL, van Lenthe GH, Achenbach SJ, Muller R, Bouxsein ML, Amin S, Atkinson EJ, Khosla S. Contribution of in vivo structural measurements and load/strength ratios to the determination of forearm fracture risk in postmenopausal women. J Bone Miner Res. 2007;22:1442–1448. doi: 10.1359/jbmr.070514. [DOI] [PubMed] [Google Scholar]
- 150.Chesnut CH, III, Majumdar S, Newitt DC, Shields A, Van Pelt J, Laschansky E, Azria M, Kriegman A, Olson M, Eriksen EF, Mindeholm L. Effects of salmon calcitonin on trabecular microarchitecture as determined by magnetic resonance imaging: Results from the QUEST study. J Bone Miner Res. 2005;20:1548–1561. doi: 10.1359/JBMR.050411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Benito M, Vasilic B, Wehrli FW, Bunker B, Wald M, Gomberg B, Wright AC, Zemel B, Cucchiara A, Snyder PJ. Effect of testosterone replacement on trabecular architecture in hypogonadal men. J Bone Miner Res. 2005;20:1785–1791. doi: 10.1359/JBMR.050606. [DOI] [PubMed] [Google Scholar]
- 152.Turner M, Clough R, Martin H, Topp L. Stiffness and deflection analysis of complex structures. J Aeronautic Sci. 1956;23:805–823. [Google Scholar]
- 153.Faulkner K, Cann C, Hasedawa B. Effect of bone distribution on vertebral strength: Assessment with a patient-specific nonlinear finite element analysis. Radiology. 1991;179:669–674. doi: 10.1148/radiology.179.3.2027972. [DOI] [PubMed] [Google Scholar]
- 154.Keyak JH, Meagher JM, Skinner HB, Mote CD., Jr Automated three-dimensional finite element modelling of bone: A new method. J Biomed Eng. 1990;12:389–397. doi: 10.1016/0141-5425(90)90022-f. [DOI] [PubMed] [Google Scholar]
- 155.Keyak JH, Fourkas MG, Meagher JM, Skinner HB. Validation of an automated method of three-dimensional finite element modelling of bone. J Biomed Eng. 1993;15:505–509. doi: 10.1016/0141-5425(93)90066-8. [DOI] [PubMed] [Google Scholar]
- 156.Keaveny TM, Donley DW, Hoffmann PF, Mitlak BH, Glass EV, San Martin JA. Effects of teriparatide and alendronate on vertebral strength as assessed by finite element modeling of QCT scans in women with osteoporosis. J Bone Miner Res. 2007;22:149–157. doi: 10.1359/jbmr.061011. [DOI] [PubMed] [Google Scholar]
- 157.Morgan EF, Bouxsein ML. Use of finite element analysis to assess bone strength. BoneKEy-Osteovision. 2005;2:8–19. [Google Scholar]
- 158.Keyak JH, Rossi SA, Jones KA, Skinner HB. Prediction of femoral fracture load using automated finite element modeling. J Biomech. 1998;31:125–133. doi: 10.1016/s0021-9290(97)00123-1. [DOI] [PubMed] [Google Scholar]
- 159.Keyak JH, Kaneko TS, Tehranzadeh J, Skinner HB. Predicting proximal femoral strength using structural engineering models. Clin Orthop. 2005;437:219–228. doi: 10.1097/01.blo.0000164400.37905.22. [DOI] [PubMed] [Google Scholar]
- 160.Keaveny T, Hoffman P, Kopperdahl D, Donley D, Krohn K, Glass EV, Mitlak BH. Comparison of the effects of teriparatide and alendronate on parameters of total hip strength as assessed by finite element analysis: Results from the Forteo and Alendronate comparison trial. J Bone Miner Res. 2007;22(S1):S26. doi: 10.1359/jbmr.061011. [DOI] [PubMed] [Google Scholar]