Article-at-a-Glance
Background
Little is known about suicide in the hospital setting. Although suicide is a major public health concern, the literature on suicide in the medical setting is limited, and accurate data on hospital-based suicides are unavailable. Consequently, the prevalence, demographic characteristics, and risk factors for suicide in this population are unknown. The literature on completed suicides in medical or surgical wards of a general hospital was summarized to generate hypotheses for further investigation regarding in-hospital suicides.
Methods
MEDLINE, PsycINFO, IndexCat, and Scopus were queried for English-language articles on inpatient suicides in a general hospital. These data were compared with reports of suicide by psychiatric inpatients and the annual suicide statistics from the U.S. general population.
Results
Twelve articles detailing 335 suicides in the medical setting were included. Published data on hospital-based suicides are limited by selection bias, incomplete reporting, and a small number of completed suicides. Consequently, no significant setting-specific findings emerge from the existing literature. Reported cases suggest that inpatients who commit suicide in the medical setting may have a different demographic profile and employ different methods of suicide in comparison with individuals who commit suicide in psychiatric settings or the general population.
Discussion
Given the absence of systematic data collection and the highly variable nature of reported suicides, it coult not be determined if clinically relevant distinctions exist between suicides in different health care settings. Prospective and more detailed data collection are needed because a more complete characterization of suicide in medical inpatients may be useful in both prevention approaches and institutional policies with respect to hospital-based suicides.
Suicide is the eleventh leading cause of death in the United States1 and has been described as a serious public health threat by the Surgeon General.2 In 2004, more than 30,000 Americans committed suicide.3 Completed inpatient suicide, as distinct from suicidal ideation or attempts, is the second-most common sentinel event reported to The Joint Commission—exceeded only by wrong-site surgery (651 [13.1%] versus 613 [12.3%]).4 In 2006, the Joint Commission designated the assessment of suicide, for patients admitted to a health care facility for behavioral health reasons, a National Patient Safety Goal.5*
Suicide, particularly among hospitalized medically ill patients, is a rare event. Most of the published reports on inpatient suicidal behavior are derived from psychiatric hospitals and units. Although there are no accurate data with which to directly compare rates of suicide in medical versus psychiatric settings, it is likely that suicide is more common on a psychiatric inpatient unit. In addition, rates of suicide in the hospital, whether on a medical or psychiatric unit, appear to be substantially lower than community-based suicide rates.1,6,7 Nonetheless, suicides in the medical setting do occur and pose profound challenges for patients and their families, health care workers, and hospital administrators.8,9 Despite their rarity, suicides in the medical setting can have substantial effect on the hospital environment, especially for a staff that lacks specific training in the assessment and management of suicide.
Physical illness increases the risk for suicide.2,10 An increased likelihood of suicidal ideation, attempts, and completions have been reported in patients who have central nervous system (CNS) dysfunction,11,12 general medical disorders,13-16 and specific symptoms such as pain17,18 and physical limitations.19 In addition, other factors associated with suicide are also found in patients hospitalized for medical illness, such as substance abuse,20 advanced age,21,22 unemployment and other financial stressors, and feelings of hopelessness and social isolation.2,10,23 Relative rates of suicide differ on the basis of specific medical diagnoses and can change in association with treatment advances, such antiviral HIV treatment.14 Importantly, and of most concern for preventative efforts, the association between medical illness and suicide may be independent of two other well-established suicide risk factors: substance abuse and depression.24
Although suicide is a major public health concern, the literature on suicide in the medical setting is limited, and accurate data on hospital-based suicides are unavailable. Consequently, the prevalence, demographic characteristics, and risk factors for suicide in this population are unknown.
The purpose of this review, which was completed in August 2006,* was to generate hypotheses regarding medical inpatient suicide. In particular, published reports were examined for demographic or phenomenological differences between suicides committed in medical settings when compared with suicides committed in psychiatric settings or in the general population. Only completed suicides were analyzed because intent and severity of suicide attempts and gestures or the incidence of “passive suicide” could not be evaluated from literature. Relevant questions for subsequent prospective studies of in-hospital suicide are identified.
Methods
The largest data set on suicide in the United States, provided by the Centers for Disease Control and Prevention (CDC), reports annual community suicide statistics, which number in the tens of thousands. A smaller but substantial literature exists on suicides in psychiatric settings. Finally, there are comparatively few published cases of suicides committed in medical and surgical wards of the general hospital.
A comparison of these populations was intended to identify potential differences between methods and circumstances of completed suicides. Such differences, if they exist, would have implications for suicide risk-reduction strategies. The general population statistics from the CDC are the most comprehensive suicide data available. In contrast, the absolute number of hospital-based suicides that occur in any given year is very small. Therefore, the published literature on suicides in psychiatric and general hospital inpatients was queried for longer time periods to increase the size of the data set and the possibility of identifying meaningful setting-specific patterns.
General Population Data
The data on suicide in the general population were extracted from the CDC National Center for Injury Prevention and Control database for 2004,3 the most recent year for which these data are publicly available.
Psychiatric Setting Articles
MEDLINE, Scopus, and PsycINFO were queried for English-language articles reporting on suicides that occurred in a psychiatric hospital or unit using the terms “psychiatric hospital” and “inpatient suicide.” The search was limited to articles published in 1980 or later because of historical changes in both hospital care practices and pharmacologic treatments that may have affected suicide rates. Nineteen articles7,25-42 reporting 1,664 suicides in the psychiatric hospital or unit were identified.
Medical Setting Articles
MEDLINE, Scopus, IndexCat, and PsychINFO were queried for English-language journal articles or book chapters reporting suicides in patients admitted to medical or surgical services of a general hospital using the following search terms: “suicide,” “inpatient,” and “general hospital.” The reference lists from primary source articles were also searched for appropriate secondary case reports and studies of suicide. An “inpatient” was defined as a patient on the grounds of, on leave from, or absent without leave (AWOL) from a general hospital. Articles were excluded for the following reasons:
-
■
No specific cases of completed suicides were reported.
-
■
The total number of suicides was not reported.
-
■
The article reported previously published data.
-
■
Case histories had been altered (typically to protect the identity of the patient).
-
■
Information was not included to clarify whether patients had been medical or psychiatric inpatients.
Twelve case series detailing 335 suicides in the medical setting were included (Table 1, page 476). Six of the included reports had substantial population selection biases (for example, they were hospitals serving almost entirely male patients). Only eight of the medical setting reports included detail about psychiatric symptoms of the inpatients during hospitalization. Fewer than half of the studies reported marital status, employment status, or race, and only one study provided information as to the medical prognosis of patients before committing suicide.
Table 1.
Studies of General Hospital Suicides Between 1947 and 2002*
| Author | Dates | Location | N | Comments |
|---|---|---|---|---|
| Brown and Pisetsky,43 1960 | 1947-1958 | U.S. | 16 | VA hospital, almost entirely men |
| Pollack,44 1957 | 1948-1953 | U.S. | 11 | VA hospital, almost entirely men |
| Petrovsky,45 1967 | 1954-1966 | Australia | 1 | |
| Farberow et al.,46 1971 | 1959-1966 | U.S. | 173 | VA hospital, almost entirely men |
| Glickman,47 1980 | 1963-1977 | U.S. | 22 | |
| Shapiro and Waltzer,48 1980 | 1965-1979 | U.S. | 12 | |
| Pietsky and Brown,49 1979 | 1971-1975 | U.S. | 2 | VA hospital, almost entirely men |
| White et al.,50 1995 | 1980-1992 | Australia | 8 | Only suicides by jumping |
| De Leo,51 1997 | 1980-1996 | Italy | 15 | Patients over 60 years of age in general and geriatric hospitals |
| Suominen et al.,52 2002 | 1987-1988 | Finland | 26 | |
| Hung et al.,53 2000 | 1988-1997 | Taiwan | 15 | |
| Ho and Tay,54 2004 | 2000-2002 | Hong Kong | 34 | |
| Total number of reported suicides: | 335 | |||
References are listed on p. 481. U.S., United States; VA, Department of Veterans Affairs.
Statistical Analysis
Given the high degree of variability in the reported data, meta-analytic statistics could not be performed. Instead, summary descriptions as part of a qualitative analysis are presented. Method of suicide could be determined for all cases from the CDC, 671 cases in the psychiatric settings, and 304 cases in the medical setting. Data for age, sex, race, marital status, employment status, method of suicide, location of suicide, length of hospital stay, prior suicide attempt(s), medical diagnosis, prognosis, medical symptoms, and psychiatric symptoms were reported too inconsistently for aggregate analysis. Consequently, varying denominators are presented for these other variables.
Results
Demographic Characteristics
Table 2 (above) summarizes demographic characteristics of the three populations. Because of the wide range of represented countries and incomplete reporting, racial data were uninterpretable. Psychiatric patients who committed suicide tended to be younger (mean age, 41.2 years) than patients who committed suicide in medical settings (mean age, 54.3 years). Approximately one half (43/80) of the medical-setting patients were married, while slightly more than one third (128/342) of psychiatric patients were married. Whereas 60% (647/1082) of psychiatric patients were unemployed, only 10 of the 35 general medical patients for whom these data were available were unemployed.
Table 2.
Age and Gender Characteristics of Completed Suicides*
| Medical Setting | Psychiatric Setting | General Population | ||
|---|---|---|---|---|
| Excluding VA | Including VA | |||
| Period of Observation | 1954-2002 | 1947-2002 | 1980-2000 | 2003 |
| n | 133 | 335 | 1,664 | 32,439 |
| Gender Male | 107 (80.5%) | 308 (91.9%) | 1,003 (60.3%) | 25,566 (78.8%) |
| Female | 26 (19.5%) | 27 (8.1%) | 661 (39.7%) | 6,873 (21.2%) |
| Mean Age | 54.7 | 54.3 | 41.2 | |
Because of potential cofounders in the Department of Veterans Affairs (VA) populations, the studies reporting on VA hospitals were segregated.
Medical Status
Medical diagnoses are reported in Table 3 (page 477) for suicides committed in the medical setting. The most common diagnosis in the medical setting was cancer. However, the specificity of reported medical diagnoses was inconsistent, which most likely reflected both historical changes in medical diagnostics as well as greater clinical detail provided with the smaller case series. Whereas individuals with CNS deficits have historically been cited to be at higher risk for suicidal behavior11,12 in this series, only 38 of the 286 inpatients who committed suicide and had their medical diagnoses reported also had neurologic conditions.
Table 3.
Medical Diagnoses of 286 Completed Suicides in the Medical Setting
| Diagnosis* | n (%) |
|---|---|
| Neoplasms | 72 (25.2%) |
| Cardiovascular diseases | 46 (16.1%) |
| Pulmonary diseases | 44 (15.4%) |
| Neurological conditions | 38 (13.3%) |
| Gastrointestinal | 16 (5.6%) |
| Injuries | 15 (5.2%) |
| Allergies and infectious disease | 14 (4.9%) |
| Orthopedic and rheumatological | 12 (4.2%) |
| Genito-urinary | 12 (4.2%) |
| Other | 17 (5.9%) |
Cases where the principle medical diagnosis was missing or ambiguous (n = 3) or reported as suicide attempt (n = 11) were excluded from analysis.
Method, Timing, and Location of Suicide
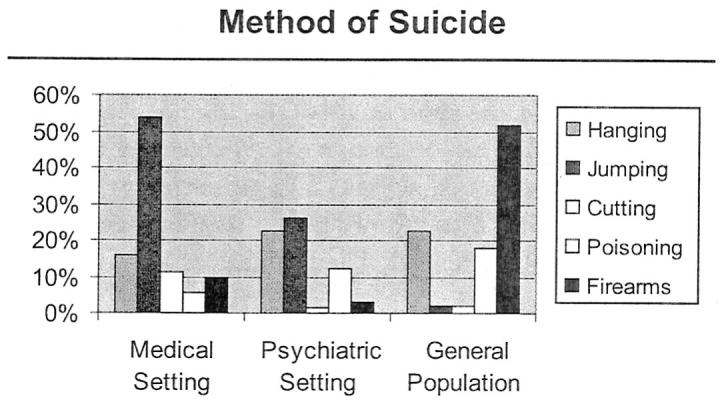
Method of suicide differed across the three populations. Table 4 (page 478) and Figure 1 (page 478) depict differences in method of suicide across these populations. Individuals in medical settings were more likely to commit suicide by jumping than in the other populations. Mean duration of medical hospitalization prior to suicide varied widely, from 2 days to several months, with an average length of stay of 31.1 days (n = 60). In contrast, the mean length of stay for inpatients in the psychiatric setting was 155 days (n = 138; outlier of 4.9 years excluded). These data do not take into consideration the substantial reductions in length of hospital stay during the past several decades in both medical and psychiatric settings.
Table 4.
Methods of Suicide*
| Hanging | Jumping | Cutting | Poisoning | Drowning | Firearms | Other | |
|---|---|---|---|---|---|---|---|
| Medical Setting |
49/304 (16.1%) |
163/304 (53.6%) |
35/304 (11.5%) |
17/304 (5.6%) |
7/304 (2.3%) |
29/304 (9.5%) |
4/304 (1.3%) |
| Psychiatric Setting |
152/671 (22.7%) |
177/671 (26.4%) |
11/671 (1.6%) |
83/671 (12.4%) |
93/671 (13.9%) |
20/671 (3.0%) |
135/671 (20.1%) |
| General Population |
7,336/32,439 (22.6%) |
676/32,439 (2.1%) |
590/32,439 (1.8%) |
5,800/32,439 (17.9%) |
365/32,439 (1.1%) |
16,750/32,439 (51.6%) |
922/32,439 (2.8%) |
Methods were categorized by International Classification of Diseases (ICD-10) and National Center for Health Statistics definitions. Methods contained in the category of “other” include suicide by transportation, fire, terrorism, unknown, and unspecified (X76, X77, X79, U03.0, U03.9, X82, X84, X75, X91, X83, Y87.0).
Figure 1. The percentages of suicides occurring by various methods for medical and psychiatric settings and the general population are shown.
Discussion
The medical literature contains limited information about factors associated with in-hospital suicides. Published studies present highly variable data about hospitalized patients who commit suicide, their underlying medical and psychiatric diagnoses, their medical prognoses, and their histories of self-harm. This literature review reveals a pressing need for more comprehensive and systematic data acquisition on in-hospital suicides.
The methodologic shortcomings of the reports reviewed here warrant specific comment. An inherent problem in the aggregation of case series is determining the validity of the findings, given the inconsistency in how variables are collected and reported. Any conclusions from the data summarized here must be tempered by the very small number of case reports on suicide in the general hospital (335 for 1947-2006) in comparison with the number of actual suicides in hospital settings (approximately 500 known inpatient suicides in the United States between January 1995 and June 2006).5 Vulnerabilities to reporting biases are another substantial concern because highly public and violent suicides, such as jumping or hanging, may be preferentially recollected, recorded, and published. In addition, the comparison groups chosen for this analysis may be skewed, given that the articles span a wide variety of countries, years, and hospital settings.
Intrinsic differences between psychiatric and medical hospital populations and environments are also likely reflected in these findings. Hospitalized psychiatric patients are typically younger and less likely to be married and have restricted access to certain methods of suicide when compared with medically ill inpatients. Differences in the location of suicide may result from the fact that many psychiatric inpatient units are locked and employ pass privileges as part of discharge planning. Furthermore, several aspects of hospital-based care have changed substantially over time and may contribute differentially to inpatient suicide. For example, the impact of hospital design and construction and length of stay are critical unanswered questions beyond the purview of this review.
An additional limitation of the reports reviewed here is the inadequate inclusion of clinical features associated with inpatient suicide. As a point of comparison, several large published case series of community-based suicides have reported the presence of depression as a major risk factor.10,55,56 In contrast, in this review of 335 patients in the medical setting who committed suicide, the presence or absence of a depressive disorder was reported in just 84 patients. Furthermore, depressive symptoms, whether or not meeting criteria for a depressive disorder, in medical inpatients who subsequently committed suicide was only reported in an additional 31 cases. The in-hospital suicide literature contains similar deficiencies with respect to documentation of a history of self-harm; only three articles noted previous suicide attempts among medical inpatients who ultimately committed suicide.
The reports reviewed here rarely included substantial detail regarding diagnostic comorbidity. For example, in those articles that reported medical diagnoses in patients who committed suicide, the designation of a neurologic disorder did not include the clinical syndrome of delirium. Although rarely reported, clinical experience suggests that delirium, as distinct from a stable neurological condition, can be an immediate contributing factor in medical/surgical inpatient suicides. Similarly, diagnoses of alcohol dependence or substance abuse were reported in only 55 out of 1,252 psychiatric inpatient suicides (4.4%), whereas substance abuse was reported in just 18 of 102 medical inpatient suicides. The large discrepancy between these data and the known comorbidity of substance abuse and suicide within the community56,57 suggests that the hospital-based suicide literature reflects either inadequate reporting of substance abuse or a different suicide phenomenology.
Despite the methodological limitations in the case series reviewed here, several observations are notable. In contrast to community-based individuals in the United States who most commonly commit suicide with a firearm and inpatients on psychiatric units whose most frequent method of suicide is hanging, inpatients on medical floors tend to commit suicide by jumping from heights. Medically ill inpatients are also more likely than psychiatric inpatients to commit suicide on hospital grounds. Medical inpatients who committed suicide appeared to be older and more likely to be married and employed than psychiatric inpatients. If replicated in subsequent, methodologically sound studies, these findings suggest the possibility of improving the environment of care and suicide assessment practices in the general hospital.
Each of the methodological limitations noted above would be substantially ameliorated by the comprehensive and systematic reporting of inpatient suicides to a central database. Hospitals, with assurance of institutional and patient confidentiality, would be asked to provide standardized reports of suicide method, timing, and clinical variables. A list of such variables is proposed in Table 5 (page 479). Robust statistical analyses could then be employed to construct distinct suicide risk profiles for hospitalized patients. If the demographic and clinical differences between inpatient suicides in medical and psychiatric settings suggested in this review are confirmed, those and other risk factors may aid in developing setting-specific prevention efforts and screening procedures. In additionally, qualitative analysis of “systems failures” implicated in in-patient suicides may lead to important improvements in hospital practices. Other promising databases for future investigation into hospital-based suicide are the National Violent Death Reporting System and the National Mortality Follow-back Survey.58,59
Table 5.
Variables for Inclusion into a Central Database on In-Hospital Suicide*
| Location and patient status |
|
| Method |
|
| Timing |
|
| Demographic characteristics |
|
| Diagnosis |
|
| Symptoms at time of suicide |
|
| Psychiatric concerns |
|
| Systems concerns |
|
VA, Department of Veterans Affairs; AWOL, absent without leave.
Several approaches to suicide prevention have been proposed, including improved physician training, suicide screening in primary care settings, means restriction, and “gatekeeper” education.60,61 Each of these areas of intervention has relevance to the prevention of suicide and the identification of important psychiatric disorders in medical settings. For example, a greater understanding of suicide risk factors in medically ill inpatients might facilitate clinician assessment of symptoms such as pain, delirium, depression, hopelessness, and “passive suicidality” in the context of severe or terminal illness. In this regard, it was interesting that in only 16% of the medical setting cases reviewed was a psychiatric consultation requested before the suicide. The Joint Commission has found that problems in “environmental safety and security” constitute the most common root cause of inpatient suicide.62 More comprehensive safety assessment of the hospital environment on medical and surgical floors might identify specific physical safeguard improvements, such as safer windows, breakaway bars in rooms, and more effective barriers in hospital atria. The gatekeepers of the hospital, such as nurses who administer intake assessments, are also likely to benefit from greater knowledge of suicide risk factors in the medically ill, and thereby improve their identification of high-risk patients requiring more thorough assessment. Further refinement of risk factors associated with in-hospital suicide would likely result in more effective screening and processes of care for patients identified as “at-risk.” Such changes in clinical assessment, practice patterns, and processes across hospital environments might lead to fewer sentinel events, increased hospital safety, and, ultimately, a larger public health benefit.
Conclusion
Systematic and methodologically sound research into the clinical characteristics and methods of suicide in patients who commit suicide in the general hospital setting is long overdue. Although these events do not commonly occur, one such event can have a devastating effect on families and institutions alike. For such low-frequency, high-impact events, collecting comprehensive clinical details about inpatient suicides is essential to create a better, safer environment of care. Such collaborative data collection across institutions has the potential to improve precision in identifying patients at risk for suicide as well as to develop more comprehensive profiles of risk factors for suicide. Improved clinical profiles of patients who commit suicide in general hospital settings can then be used in training, assessment, environmental risk management, and other institutional patient safety efforts.
Acknowledgments
This research was supported in part by the National Institute of Mental Health Intramural Research Program and the National Institutes of Health Clinical Center. The opinions expressed in the article are the views of the authors and do not necessarily reflect the views of the Department of Health and Human Services or the United States government. The authors would like to acknowledge Robert Wesley and Lisa Horowitz for their help on the manuscript as well as several patients and their families for sharing their experiences with us.
Footnotes
Goal 15: The organization identifies safety risks inherent in its [patient] population. Now renumbered as NPSG.15.01.01: The [organization] identifies [patient]s at risk for suicide. This requirement only applies to psychiatric hospitals and patients being treated for emotional or behavioral disorders in general.
As of July 2007, no new citations meeting the inclusion criteria were found.
Contributor Information
Elizabeth D. Ballard, National Institute of Mental Health (NIMH), National Institutes of Health (NIH), Bethesda, Maryland
Maryland Pao, Deputy Clinical Director, NIMH, Clinical Research Center, NIH
David Henderson, Deputy Director for Clinical Care, Clinical Center, NIH
Laura M. Lee, Special Assistant to the Deputy Director for Clinical Care, Clinical Center, NIH.
J. Michael Bostwick, Associate Professor of Psychiatry, Department of Psychiatry and Psychology, College of Medicine, Mayo Clinic, Rochester, Minnesota
Donald L. Rosenstein, Clinical Director, NIMH, Clinical Research Center, NIH
References
- 1.American Association of Suicidology [last accessed Jun. 18, 2008];Suicide in the U.S.A.: Based on Current (2004) Statistics. http://www.suicidology.org/associations/1045/files/SuicideInTheUS.pdf.
- 2.U.S. Public Health Service [last accessed Jun. 18, 2008];The Surgeon General’s Call to Action to Prevent Suicide. 1999 http://www.surgeongeneral.gov/library/calltoaction/calltoaction.pdf.
- 3.National Center for Injury Prevention and Control [last accessed Jun. 18, 2008];Welcome to WISQARS (Web-based Injury Statistics Query and Reporting System) http://www.cdc.gov/ncipc/wisqars/default.htm.
- 4.The Joint Commission [last accessed Jun. 18, 2008];Sentinel Event Statistics. http://www.jointcommission.org/SentinelEvents/Statistics/
- 5.The Joint Commission [last accessed Jun. 18, 2008];Hospital Accreditation Program: 2009 Chapter: National Patient Safety Goals. http://www.jointcommission.org/NR/rdonlyres/31666E86-E7F4-423E-9BE8-F05BD1CB0AA8/0/09_NPSG_HAP.pdf.
- 6.Keller F, Wolfersdorf M. Changes in suicide numbers in psychiatric hospitals: An analysis using log-linear time-trend models. Soc Psychiatry Psychiatr Epidemiol. 1995 Nov;30:269–273. doi: 10.1007/BF00805793. [DOI] [PubMed] [Google Scholar]
- 7.Spiessl H, Hünber-Liebermann B, Cording C. Suicidal behavior of psychiatric in-patients. Acta Psychiatr Scand. 2002 Aug;106:134–138. doi: 10.1034/j.1600-0447.2002.02270.x. [DOI] [PubMed] [Google Scholar]
- 8.Aketchi T, et al. Trauma in a nurse after patient suicide. Psychosomatics. 2003 Nov.-Dec;44:522–523. doi: 10.1176/appi.psy.44.6.522. [DOI] [PubMed] [Google Scholar]
- 9.Collins JM. Impact of patient suicide on clinicians. Journal of the American Psychiatric Nurses Association. 2003 Oct;9:159–162. [Google Scholar]
- 10.Institute of Medicine . Reducing Suicide: A National Imperative. National Academy Press; Washington, DC: 2002. [PubMed] [Google Scholar]
- 11.Jones JE, et al. Rates and risk factors for suicide, suicidal ideation and suicide attempts in chronic epilepsy. Epilepsy Behav. 2003 Oct;4:S31–S38. doi: 10.1016/j.yebeh.2003.08.019. [DOI] [PubMed] [Google Scholar]
- 12.Schoenfeld M, et al. Increased rate of suicide among patients with Huntington’s disease. J Neurol Neurosurg Psychiatry. 1984 Dec;47:1283–1287. doi: 10.1136/jnnp.47.12.1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hughes D, Kleespies P. Suicide Life Threat Behav. Vol. 31. 2001. Spring. Suicide in the medically ill; pp. 48–59. [DOI] [PubMed] [Google Scholar]
- 14.Komiti A, et al. Suicidal behaviour in people with HIV/AIDS: A review. Aust N Z J Psychiatry. 2001 Dec;35:747–757. doi: 10.1046/j.1440-1614.2001.00943.x. [DOI] [PubMed] [Google Scholar]
- 15.Björkenstam C, et al. Are cancer patients at higher suicide risk than the general population? Scand J Public Health. 2005 Jun;33:208–214. doi: 10.1080/14034940410019226. [DOI] [PubMed] [Google Scholar]
- 16.Abram HS, Moore GL, Westervelt FB. Suicidal behavior in chronic dialysis patients. Am J Psychiatry. 1971 Oct;127:1199–1204. doi: 10.1176/ajp.127.9.1199. [DOI] [PubMed] [Google Scholar]
- 17.Fishbain DA. The association of chronic pain and suicide. Semin Clin Neuropsychiatry. 1999 Jul;4:221–227. doi: 10.153/SCNP00400221. [DOI] [PubMed] [Google Scholar]
- 18.Tang NK, Crane C. Suicidality in chronic pain: A review of the prevalence, risk factors and psychological links. Psychol Med. 2006 Jan;18:1–12. doi: 10.1017/S0033291705006859. [DOI] [PubMed] [Google Scholar]
- 19.Kaplan MS, et al. Physical illness, functional limitations, and suicide risk: A population-based study. Am J Orthopsychiatry. 2007 Jan;77:56–60. doi: 10.1037/0002-9432.77.1.56. [DOI] [PubMed] [Google Scholar]
- 20.Bostwick JM, Seaman JS. Hospitalized patients and alcohol: Who is being missed? Gen Hosp Psychiatry. 2004 Jan.-Feb;26:59–62. doi: 10.1016/j.genhosppsych.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 21.Waern M, et al. Burden of illness and suicide in elderly people: Case control study. BMJ. 2002 Jun 8;324:1355. doi: 10.1136/bmj.324.7350.1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Juurlink DN, et al. Medical illness and the risk of suicide. Arch Intern Med. 2004 Jun 14;164:1179–1184. doi: 10.1001/archinte.164.11.1179. [DOI] [PubMed] [Google Scholar]
- 23.Institute of Medicine Risk Factors for Suicide: Summary of a Workshop; Washington, DC: National Academy Press. 2001. [Google Scholar]
- 24.Druss B, Pincus H. Suicidal ideation and suicide attempts in general medical illness. Arch Intern Med. 2000 May;160:1522–1526. doi: 10.1001/archinte.160.10.1522. [DOI] [PubMed] [Google Scholar]
- 25.Salmons PH. Suicide in high buildings. Br J Psychiatry. 1984 Nov;145:469–472. doi: 10.1192/bjp.145.5.469. [DOI] [PubMed] [Google Scholar]
- 26.Langley GE, Bayatti NN. Suicides in Exe Vale Hospital. Br J Psychiatry. 1984 Nov;145:463–467. doi: 10.1192/bjp.145.5.463. [DOI] [PubMed] [Google Scholar]
- 27.Goh SE, Salmons PH, Whittington RH. Hospital suicides: Are there preventable factors? Br J Psychiatry. 1989 Feb;154:247–249. doi: 10.1192/bjp.154.2.247. [DOI] [PubMed] [Google Scholar]
- 28.Morgan HG, Priest P. Suicide and other unexpected deaths among psychiatric in-patients: The Bristol confidential inquiry. Br J Psychiatry. 1991 Mar;158:368–372. doi: 10.1192/bjp.158.3.368. [DOI] [PubMed] [Google Scholar]
- 29.Hattori T, Taketani K, Osasawara Y. Suicide and suicide attempts in general hospital psychiatry: Clinical and statistical study. Psychiatry Clin Neurosci. 1995 Mar;49:43–48. doi: 10.1111/j.1440-1819.1995.tb01855.x. [DOI] [PubMed] [Google Scholar]
- 30.Roy A, Draper R. Suicide among psychiatric hospital in-patients. Psychol Med. 1995 Jan;25:199–202. doi: 10.1017/s0033291700028233. [DOI] [PubMed] [Google Scholar]
- 31.Blain PA, Donaldson LJ. The reporting of in-patient suicides: Identifying the problem. Public Health. 1995 Jul;109:293–301. doi: 10.1016/s0033-3506(95)80207-x. [DOI] [PubMed] [Google Scholar]
- 32.Shah AK, Ganesvaran T. Inpatient suicides in an Australian mental hospital. Aust N Z J Psychiatry. 1997 Apr;31:291–298. doi: 10.3109/00048679709073834. [DOI] [PubMed] [Google Scholar]
- 33.Sharma V, Persad E, Kueneman K. A closer look at inpatient suicide. J Affect Disord. 1998 Jan;47:123–129. doi: 10.1016/s0165-0327(97)00131-6. [DOI] [PubMed] [Google Scholar]
- 34.Deisenhammer EA, et al. In-patient suicide in psychiatric hospitals. Acta Psychiatr Scand. 2000 Oct;102:290–294. doi: 10.1034/j.1600-0447.2000.102004290.x. [DOI] [PubMed] [Google Scholar]
- 35.Powell J, et al. Suicide in psychiatric hospital in-patients: Risk factors and their predictive power. Br J Psychiatry. 2000 Mar;176:266–272. doi: 10.1192/bjp.176.3.266. [DOI] [PubMed] [Google Scholar]
- 36.Martin BA. The Clarke Institute experience with completed suicide: 1966 to 1997. Can J Psychiatry. 2000 Sep;45:630–638. doi: 10.1177/070674370004500705. [DOI] [PubMed] [Google Scholar]
- 37.King EA, et al. The Wessex recent in-patient suicide study, 2: Case-control study of 59 in-patient suicides. Br J Psychiatry. 2001 Jun;178:537–542. doi: 10.1192/bjp.178.6.537. [DOI] [PubMed] [Google Scholar]
- 38.Ramsay L, Gray C, White T. A review of suicide within the state hospital, Carstairs 1972-1996. Med Sci Law. 2001 Apr;41:97–101. doi: 10.1177/002580240104100202. [DOI] [PubMed] [Google Scholar]
- 39.Marušic A, et al. Comparison of psychiatric inpatient suicides with suicides completed in the surrounding community. Nord J Psychiatry. 2002;56(5):335–338. doi: 10.1080/080394802760322097. [DOI] [PubMed] [Google Scholar]
- 40.Busch KA, Fawcett J, Jacobs DG. Clinical correlates of inpatient suicide. J Clin Psychiatry. 2003 Jan;64:14–19. doi: 10.4088/jcp.v64n0105. [DOI] [PubMed] [Google Scholar]
- 41.Dong JYS, Ho TP, Kan CK. A case-control study of 92 cases of in-patient suicides. J Affect Disord. 2005 Jul;87:91–99. doi: 10.1016/j.jad.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 42.Meehan J, et al. Suicide in mental health in-patients and within 3 months of discharge. Br J Psychiatry. 2006 Feb;188:129–134. doi: 10.1192/bjp.188.2.129. [DOI] [PubMed] [Google Scholar]
- 43.Brown W, Pietsky JE. Suicidal behavior in a general hospital. Am J Med. 1960 Aug;29:307–315. [Google Scholar]
- 44.Pollack S. Suicide in a general hospital. In: Shneidman ES, Farberow NL, editors. Clues to Suicide. McGraw-Hill; New York City: 1957. pp. 152–163. [Google Scholar]
- 45.Petrovsky CC. Suicide in a general hospital. Med J Aust. 1967 Oct;2:669–672. [PubMed] [Google Scholar]
- 46.Farberow NL, et al. An eight-year survey of hospital suicides. Suicide Life Threat Behav. 1971;1(3):184–202. [Google Scholar]
- 47.Glickman LS. Psychiatric Consultation in the General Hospital. Marcel Dekker, Inc.; New York City: 1980. [Google Scholar]
- 48.Shapiro S, Waltzer H. Successful suicides and serious attempts in a general hospital over a 15-year period. Gen Hosp Psychiatry. 1980 Jun;1:118–126. doi: 10.1016/0163-8343(80)90025-0. [DOI] [PubMed] [Google Scholar]
- 49.Pietsky JE, Brown W. The general hospital patient. In: Hankoff LD, Einsidler B, editors. Suicide: Theory and Clinical Aspects. PSG Publishing; Littleton, MA: 1979. pp. 279–289. [Google Scholar]
- 50.White RT, et al. Jumping from a general hospital. Gen Hosp Psychiatry. 1995 May;17:208–215. doi: 10.1016/0163-8343(94)00092-r. [DOI] [PubMed] [Google Scholar]
- 51.De Leo D. Suicide in a general hospital: The case of the elderly. Crisis. 1997;18(1):5–6. doi: 10.1027/0227-5910.18.1.5. [DOI] [PubMed] [Google Scholar]
- 52.Suominen K, et al. General hospital suicides: A psychological autopsy study in Finland. Gen Hosp Psychiatry. 2002 Nov.-Dec;24:412–416. doi: 10.1016/s0163-8343(02)00222-0. [DOI] [PubMed] [Google Scholar]
- 53.Hung C, et al. Self-destructive acts occurring during medical general hospitalization. Gen Hosp Psychiatry. 2000 Mar.-Apr;22:115–121. doi: 10.1016/s0163-8343(00)00052-9. [DOI] [PubMed] [Google Scholar]
- 54.Ho TP, Tay MSM. Suicides in general hospitals in Hong Kong: Retrospective study. Hong Kong Med J. 2004 Oct;10:319–324. [PubMed] [Google Scholar]
- 55.Rich CL, et al. San Diego suicide study. III. Relationships between diagnoses and stressors. Arch Gen Psychiatry. 1988 Jun;45:589–592. doi: 10.1001/archpsyc.1988.01800300087012. [DOI] [PubMed] [Google Scholar]
- 56.Beautrais AL, et al. Prevalence and comorbidity of mental disorders in persons making serious suicide attempts: A case-control study. Am J Psychiatry. 1996 Aug;153:1009–1014. doi: 10.1176/ajp.153.8.1009. [DOI] [PubMed] [Google Scholar]
- 57.Borges G, Walters EE, Kessler RC. Associations of substance use, abuse, and dependence with subsequent suicidal behavior. Am J Epidemiol. 2000 Apr;151:781–789. doi: 10.1093/oxfordjournals.aje.a010278. [DOI] [PubMed] [Google Scholar]
- 58.Powell V, et al. Using NVDRS data for suicide prevention: Promising practices in seven states. Inj Prev. 2006 Dec;12(suppl 2):ii28–ii32. doi: 10.1136/ip.2006.012443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.National Vital Statistics System [last accessed Jun. 18, 2008];National Mortality Followback Survey. http://www.cdc.gov/nchs/about/major/nmfs/nmfs.htm.
- 60.Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: A review of the evidence. Am J Psychiatry. 2002 Jun;159:909–916. doi: 10.1176/appi.ajp.159.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mann JJ, et al. Suicide prevention strategies: A systematic review. JAMA. 2005 Oct 26;294:1064–1074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 62.The Joint Commission [last accessed Jul. 16, 2007];National Patient Safety Goals. http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/


