Abstract
Hyperactive cortico-striatal circuits including the Anterior Cingulate Cortex (ACC) have been implicated to underlie obtrusive thoughts and repetitive behaviors in Obsessive-Compulsive Disorder (OCD). Larger Error-Related Negativities (ERNs) in OCD patients during simple flanker tasks have been proposed to reflect an amplified error signal in these hyperactive circuits. Such amplified error signals typically are associated with an adaptive change in response, yet in OCD these same repetitive responses persist to the point of distress and impairment. In contrast to this repetitive character of OC behavior, larger ERN amplitudes have been linked to better avoidance learning in reinforcement learning tasks. Study I thus investigated if OC symptomatology in non-patients predicted an enhanced ERN after suboptimal choices in a probabilistic learning task. Absent any behavioral differences, higher OC symptoms predicted smaller ERNs. Study II replicated this effect in an independent sample while also replicating findings of a larger ERN in a flanker task. There were no relevant behavioral differences in reinforcement learning or error monitoring as a function of symptom score. These findings implicate different, yet overlapping neural mechanisms underlying the negative deflection in the ERP following the execution of an erroneous motor response and the one following a suboptimal choice in a reinforcement learning paradigm. OC symptomatology may be dissociated in these neural systems, with hypoactivity in a system that enables learning to avoid maladaptive choices, and hyperactivity in another system that enables the same behavior to be repeated when it was assessed as not quite good enough the first time.
Keywords: OCD, Event-related potentials, Error-related negativity, ERN, reinforcement learning
Introduction
Obsessive-Compulsive Disorder (OCD) is a common psychiatric condition characterized by intrusive and recurrent unwanted thoughts, ideas or impulses (obsessions) and the urge to perform repetitive, ritualistic behavior (compulsions) to reduce anxiety or distress (DSM-IV, 1994). The lifetime prevalence is estimated to be as high as 2-3.5% (Angst et al., 2004; Kessler et al., 2005; Weissman et al., 1994) but the recognized clinical prevalence is estimated to be much lower (Fireman, Koran, Leventhal, & Jacobson, 2001). Neuroimaging studies of OCD patients have revealed greater activity at rest and after symptom provocation in the Anterior Cingulate Cortex (ACC: Adler et al., 2000; Baxter, 1999; Breiter & Rauch, 1996; Cottraux et al., 1996; Kim et al., 2003; Perani et al., 1995; Rauch et al., 1994; Swedo, Rapoport, Leonard, Lenane, & Cheslow, 1989; van den Heuvel et al., 2005) the orbito-frontal cortex (OFC: Baxter, Schwartz, Guze, Bergman, & Szuba, 1990; Swedo et al., 1989) and the striatum (van den Heuvel et al., 2005). Since the ACC, OFC and striatum are interconnected in recurrent loops, hyperactivity in this cortico-striatal circuit is thought to contribute to the pathophysiology of OCD (Remijnse et al., 2006). Given that cortico-striatal circuits are involved in action selection, goal-directed behavior, and performance monitoring (Balleine, Delgado, & Hikosaka, 2007; Ito, Stuphorn, Brown, & Schall, 2003; Nicola, 2007), hyperactivity in this system is proposed to underlie a persistent high error signal (Pitman, 1987). This hyperactive error monitoring hypothesis suggests that patients receive malfunctioning error signals after not completing their goals (e.g. hands are not quite clean enough), leading them to repeat their compulsive behaviors.
Pitman’s (1987) hypothesis of a persistent and enhanced cortico-striatal error signal in OCD was tested by Gehring, Himle and Nisenson (2000) using the Error-Related Negativity (ERN), an electrophysiological voltage potential occurring ~80ms following errors of motor commission (Falkenstein, Hohnsbein, Hoormann, & Blanke, 1991; Gehring, Coles, Meyer, & Donchin, 1990). EEG source localization and EEG-informed functional Magnetic Resonance Imaging (fMRI) have both implicated the caudal ACC as the proposed neural generator of the ERN (Debener et al., 2005; Dehaene, Posner, & Tucker, 1994; Ullsperger & von Cramon, 2004). Convergent evidence from multiple fields of neuroimaging have implicated a hyperactive error system in the ACC where OCD patients are characterized by greater hemodynamic responses in the ACC following errors (Fitzgerald et al., 2005; Maltby, Tolin, Worhunsky, O’Keefe, & Kiehl, 2005; Ursu, Stenger, Shear, Jones, & Carter, 2003) or a larger ERN (Endrass, Klawohn, Schuster, & Kathmann, 2008; Gehring et al., 2000; Hajcak, Franklin, Foa, & Simons, 2008; Johannes et al., 2001; Ruchsow et al., 2005) but see Nieuwenhuis et al. (2005a) who utilized a reinforcement learning paradigm. Two studies have also shown that greater OC symptom scores in non-patients predict a larger ERN (Hajcak & Simons, 2002; Santesso, Segalowitz, & Schmidt, 2006), indicating that this relationship may be reliably present in non-clinical populations. Although these investigations demonstrate a reliable effect of an enhanced ERN as a function of OCD or OC symptoms, an unresolved issue is the degree to which a putative hyperactive error signal affects action selection and goal-directed behavior. Differences in post-error behaviors are rarely found between OC and control groups even in the context of larger ERN amplitudes.
Conditions in which enhanced ERN amplitudes have been found in OC populations involve instructed response conflict tasks with speeded responses (Flanker task: Endrass et al., 2008, Ruchsow et al., 2005, Santesso et al., 2006; Stroop task: Gehring et al., 2000, Hajcak & Simons, 2002; Simon task: Hajcak et al., 2008; Choice reaction time task: Johannes et al., 2001). The sole task investigating reinforcement learning, however, failed to find an effects on fronto-central scalp potentials in OCD patients (Nieuwenhuis et al., 2005a). Importantly, the ERN in this reinforcement learning task was defined as the voltage deflection following a probabilistic suboptimal response, one which the participant must learn over time through the use of valenced feedback (Holroyd & Coles, 2002). In these goal directed reinforcement learning tasks, larger error signals have been associated with a greater tendency to avoid making the same action that preceded the error, sometimes termed NoGo learning (Frank, D’Lauro, & Curran, 2007; Frank, Woroch, & Curran, 2005; Holroyd & Coles, 2002). The larger ERNs in OC groups, putatively reflecting hyperactive error monitoring circuits, should thus lead to better learning among OC patients to avoid making the choices that led to the error; i.e., a NoGo bias.
Therefore, it would be predicted that a larger ERN deflection in OCD patients would predict enhanced NoGo learning; yet it is unclear if findings of an enhanced ERN would extend to uncertain environments in which adaptive responses are needed to achieve optimal performance goals. Indeed, the prediction of enhanced avoidance learning may stand in sharp contrast to the repetitive character of OC behaviors. To investigate a possible association between action monitoring and reinforcement learning as a function of OC symptomatology, this study utilized a reinforcement learning paradigm previously shown to elicit response-locked negative deflections in fronto-central scalp potentials after suboptimal choices or similar feedback-locked deflections following negative performance feedback (here termed ERN and FRN, respectively (Frank, Seeberger, & O’Reilly, 2004; Frank et al., 2005a). Due to unexpected findings from this investigation, a second study was run to replicate the findings with the probabilistic learning task, and to compare them to findings using a standard response conflict flanker task, that has robustly elicited larger ERNs in OC populations. The findings demonstrate that the relationship between medio-frontal activation and error processing in OCD is task-dependent, with hyper activity in a response conflict task, but hypo activity in reinforcement learning.
Materials and Methods
The probabilistic reinforcement learning task was the same in Study I and Study II. The flanker task was conducted only in Study II.
Participants
Participants included 61 young adults in Study I and 59 young adults in Study II. All participants gave written informed consent and the research ethics committee of the University of Arizona approved both studies. All participants had normal or corrected-to-normal vision. Participants were awarded course credit for their participation, and were informed that a $30 gift certificate was to be awarded to the person who performed the best on the probabilistic learning task (separately for each study). Each recording consisted of a single 2-hour session and the experimenters were blind to obsessive-compulsive status until data reduction was complete. Participants were not informed of the true purpose of the experiment until after completion; recruitment materials advertised that the experiment simply measured brain activity during a learning task.
Participants were recruited from pretest data given to undergraduate students in introductory psychology classes. For each Study, more than 1000 students completed the Obsessive-Compulsive Inventory -Revised (OCI-R; Foa et al., 2002). The OCI-R is composed of 18 items covering six obsessive and compulsive dimensions: washing, obsessing, hoarding, ordering, checking and neutralizing. The OCI (Foa, Kozak, Salkovskis, Coles, & Amir, 1998) was designed to be administered to both clinical and non-clinical populations and can be used as a screening test, as well as to determine symptom severity. The psychometric properties of the OCI-R are well documented for clinical and non-clinical populations (Fullana et al., 2005; Hajcak, Huppert, Simons, & Foa, 2004; Huppert et al., 2007). In group analyses the recommended clinical significant cutoff score of 21 (Foa et al., 2002) was used to discriminate between a high (>20) and a low (<21) group. To obtain a distributed sample participants over the entire range of the OCI-R scores were recruited for the studies. To ensure that the tested sample had similar symptom levels at the time of the laboratory visit as at pretest (the interval between the mass survey and the experiment varied from one to twelve weeks in both studies), and to ensure valid responses were obtained in the mass survey, the OCI-R was re-administered after electrophysiological recording. Correlations between pre-test data and post-test scores reveal that the OCI-R data from the pre-test was highly stable (Study I: r(61)=.90, p<0.001, R2=.81; Study II: r(59)=.81, p<0.001, R2=.66). Table 1 presents demographic and symptom data obtained after the electrophysiological recordings.
Table 1.
Group characteristics for the OC high and OC low group for both samples.
| Characteristics | Group low OCI-R group | high OCI-R group |
|---|---|---|
| Study I probabilistic learning task | ||
| Number of males, females | 16, 14 | 4, 6 |
| Age (years) | 19.1 (1.8; 18-28) | 18.6 (0.5; 18-19) |
| OCI-Ra | 7.3 (5.3; 1-19) | 38.6 (10.3; 22-50) |
| BDIa | 3.5 (3.8; 0-15) | 11.7 (6.6; 1-26) |
| Total Test Accuracy | .70 (.08) | .71 (.08) |
| ‘Go’ Accuracy | .68 (.14) | .72 (.11) |
| ‘NoGo’ Accuracy | .69 (.16) | .70 (.24) |
| Study II probabilistic learning task | ||
| Number of males, females | 6, 10 | 4, 10 |
| Age (years) | 19.0 (0.6; 18-20) | 19.1 (1.5; 18-22) |
| OCI-Ra | 8.5 (5.4; 0-16) | 38.9 (10.1; 22-55) |
| BDIa | 3.7 (4.8; 0-13) | 8.6 (6.6; 1-21) |
| Total Test Accuracy | .73 (.11) | .66 (.09) |
| ‘Go’ Accuracy | .73 (.17) | .76 (.17) |
| ‘NoGo’ Accuracy | .67 (.16) | .69 (.20) |
| Study II flanker task | ||
| Number of males, females | 10, 8 | 6,12 |
| Age (years) | 18.8 (0.9; 18-21) | 18.9 (1.2; 18-22) |
| OCI-Ra | 8.8 (6.6; 0-17) | 37.9 (10.0; 22-58) |
| BDIa | 4.3 (4.4; 0-13) | 8.2 (6.1; 1-21) |
Group means are reported, with standard deviation (or SD and range) in parentheses. OCI-R=Obsessive-Compulsive Inventory –Revised. BDI=Beck Depression Inventory.
Higher scores on the OCI-R and BDI are indicative of more OCD and depressive symptoms. Maximum score on the OCI-R is 72. A score of 21 is used as a cutoff, with scores of 21 or higher suggesting the presents of OCD. Maximum score on the BDI is 63.
Exclusion criterion and participants with insufficient data
Participants were excluded if they had a history of neurological disease or head trauma, or current use of psychoactive medications. Participant data was not included in the analyses if a change in OCI-R score after the experimental session compared to the assessment score resulted in a categorization out of the their original OC group (high or low). Additionally, data were not included if there were fewer than 30 EEG epochs in all conditions, or if the participants failed to learn the reinforcement learning task as defined by choosing the most rewarding stimulus (A) over the least rewarding stimulus (B) more than 50% of the time during each test phase, thus failing to perform above chance level (see Figure 1: Frank et al., 2004; Frank et al., 2005a). In Study I, two participants were excluded for substantial change in OCI-R score and thus change in OC group. Five participants did not produce enough errors or had bad EEG data and were excluded from analysis. Since the primary interest was in the performance after learning the contingencies fourteen additional participants had to be excluded from analysis for failing to reach the performance criterion (this criterion was not different between both groups: χ2 (2, N=54) = .02, p=.89), thus yielding a final sample of 40 (10 high OC and 30 low OC). In Study II, seven participants were excluded for substantial change in OCI-R score. For the learning task 11 more participants had bad EEG recordings or did not produce sufficient errors and 10 participants were excluded from analysis for failing to reach the performance criterion (again this criterion was not different between both groups: χ2 (2, N=40) = .03, p=.85). For the flanker task, 16 participants did not produce enough errors or had bad EEG. Thus the final sample included 30 (14 high and 16 low) participants for probabilistic learning ERP data, and 36 (18 high and 18 low) for ERP data from the flanker paradigm in Study II.
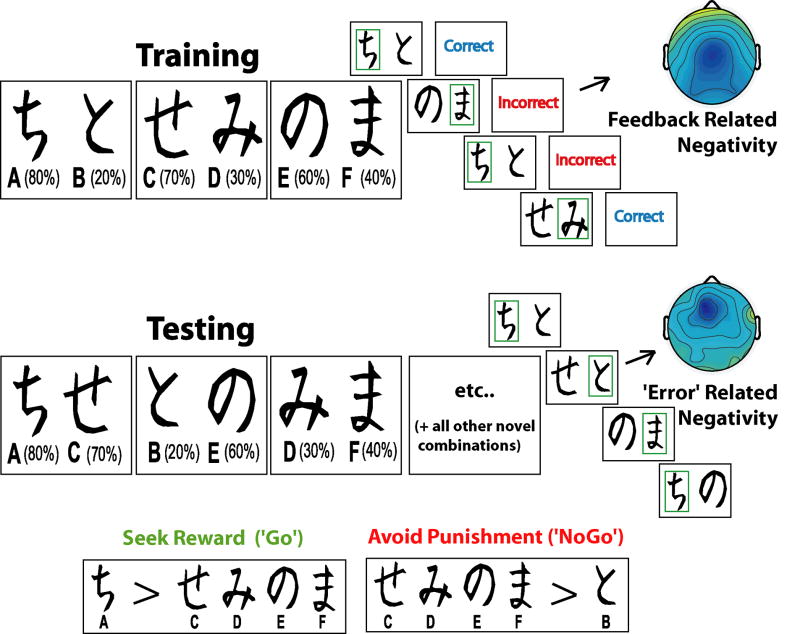
Figure 1.
Example pairs of stimuli and trial runs for training and testing sets of the probabilistic learning task. During training, each pair is presented separately. Participants have to select one of the two stimuli, slowly integrating ‘Correct’ and ‘Incorrect’ feedback (each stimulus has a unique probabilistic chance of being ‘Correct’) in order to maximize their accuracy. In the course of the testing phase, each stimulus is paired with all other stimuli and participants must choose the best one, without the aid of feedback. Note that the letter and percentage are not presented to the participant, nor are the boxes surrounding the choice. An example FRN is shown to ‘Incorrect’ feedback during Training, and an example ERN is shown to a suboptimal choice during Testing. Participants learn this task during training by a combination of seeking the most rewarding stimulus (Go learning) or avoiding the most punishing stimulus (NoGo learning), which are assessed during the testing phase.
Probabilistic Learning Task
A variant of the probabilistic selection paradigm used in Frank et al. (2005a) was presented using DMDX Software (Forster & Forster, 1999). The participants were seated 120 cm in front a CRT computer screen. The stimuli were presented in white on black background and subtended about 5° × 5° of visual angle each placed 2° apart. The task consists of a forced choice training phase consisting of up to six blocks of sixty trials each, followed by a subsequent testing phase. During the training phase the participants were presented with three stimulus pairs (termed AB, CD, EF pairs). Each stimulus was associated with a different probabilistic feedback value, as can be seen in Figure 1. All training trials began with a jittered inter-trial-interval (ITI) between 300 and 700 ms. The stimuli then appeared for a maximum of 4000 ms, and disappeared immediately after the choice was made. If the participant failed to make a choice within the 4000 ms, “No Response Detected” was presented. Following a button press, either ‘Correct’ or ‘Incorrect’ feedback was presented for 500 ms (jittered between 50 and 100 ms post response), depending on the reinforcement contingency (see Figure 1). Although this timing pattern forces an overlap in the EEG between later parts of the response epoch with early stimulus processing, immediate feedback may be necessary for adequate encoding of the action value in the basal ganglia (Frank, 2005b; Maddox, Ashby, & Bohil, 2003). Over the course of the training phase, a participant usually learns to choose A over B, C over D and E over F, solely due to adaptive responding based on the valenced feedback. The participants underwent training trials (consisting of up to six blocks of sixty stimuli each) until they reached a minimum criterion of choosing the probabilistically best stimulus in each pair (AB ≥ 65%, CD ≥ 60%, and EF ≥ 50% correct choices). If participants did not learn these criteria by the end of the sixth block, they were moved to the testing phase regardless.
The correct decision to choose one stimulus can be derived by either learning that responding to one choice is correct (Go learning), by learning that responding to the choice of the alternate stimulus is incorrect (NoGo learning), or some degree of both. To test whether the participants learned more from Go or NoGo learning, a testing phase followed the training phase. During the testing phase all possible stimuli pairs were presented eight times (120 trials total) and no feedback was provided. Thus, each pair had an optimal and suboptimal response based on what was learned during the training phase. Trials in the test phase began with an ITI of 500 ms. Stimuli were presented for a maximum of 4000 ms, and disappeared as soon as a choice was made. No feedback was provided in the testing phase. Go learning was defined as the accuracy of choosing A over C, D, E & F (i.e. seeking A), whereas NoGo learning was defined as the accuracy of choosing C, D, E & F over B (i.e. avoiding B). Since the ERN amplitude has been shown to predict NoGo, but not Go learning, this variable was of a priori interest (Frank et al., 2005a). In Study I, participants performed the task two times with different pseudo-randomly assigned character sets. Behavioral and EEG data were computed over the average of these two combined sets. In Study II, participants performed one version of the probabilistic learning task followed by the flanker task.
Flanker Task
Following the probabilistic learning task, participants in Study II performed a variant of the Eriksen flanker task (described in: Cavanagh & Allen, 2008) commonly used to elicit an ERN during motor errors of commission. The version used here utilized different letter strings for different blocks (i.e.: MMNMM; FFEFF; QQOQQ; VVUVV; IITII). Ten blocks of 40 flanker/target stimuli were presented (400 trials). In each block letter series, participants were required to identify the center letter which could be the same as the flankers (congruent e.g. MMMMM) or different (incongruent e.g. MMNMM). The letter-hand mappings were reversed between consecutive blocks of the same letter strings to increase response conflict. Each trial began with a blank screen for 100 ms, followed by a fixation cross for 700 ms. The fixation was replaced with the flanker stimuli, which were presented 135 ms before the target letter to increase conflict. The whole string was presented for another 135 ms and was followed by a fixation cross for 600 ms. Participants had 1000 ms to respond; otherwise a negative feedback (“WRONG”) was displayed for 500 ms. No other feedback was given. Instructions emphasized both speed and accuracy. Participants were given the opportunity to self-correct erroneous responses and were encouraged to do so.
Electrophysiological Data acquisition and analyses
Scalp voltage fluctuations were collected using 64 Ag/AgCl scalp electrodes arranged according to the extended international 10-20 system and recorded on NeuroScan SynAmps2 with impedances kept under 10 kΩ. Electrodes placed at the infra- and supra-orbital ridges of the left eye monitored vertical eye movements and electrodes placed on the outer canthus of the eyes recorded the horizontal electrooculogram. The EEG was recorded continuously in DC mode with a low-pass hardware filter at 100 Hz for Study I and in AC mode with bandpass filter (0.5-100 Hz) for Study II. Analog to digital conversion was done with 32-bit resolution at a sampling rate of 500 Hz. DC drifts and clippings, as well as large muscular activity, were rejected by visual inspection; the data were subsequently re-referenced to averaged mastoids, high-pass filtered at 0.5 Hz, 96 dB/oct and then low-pass filtered at 15 Hz, 96 dB/oct. To correct for the impact of blinks a regression method (Semlitsch, Anderer, Schuster, & Presslich, 1986) was applied. Response-related epochs (from 200 ms prior to 500 ms post-response) were then extracted, and response-locked averages were created separately for optimal and suboptimal choices during the test phase in the probabilistic learning task, and for correct and erroneous choices (including self-corrected errors) in the flanker task. Errors of omission (failing to respond within the time limit) were very rare and were not included in analyses. The epochs were baseline corrected with respect to the average voltage of the 100 ms pre-response window.
Following previous studies using probabilistic learning paradigms (Holroyd & Coles, 2002; Nieuwenhuis et al., 2005b), difference waveforms were created by: 1) subtracting the signal elicited on trials with optimal choices from the signal elicited on trials with suboptimal choices (dERN) in the probabilistic learning test phase; 2) subtracting the signal on correct trials from the signal on erroneous trials in the flanker task (dERN); or 3) subtracting trials with positive feedback from trials with negative feedback (dFRN) in the training phase of the probabilistic learning paradigm. For the quantification of the dERN and dFRN, trough-to-peak measurements were calculated to determine baseline-independent amplitudes of negative deflections by measuring the amplitude distance between the negative peak of the component and the preceding positive peak (Falkenstein, Hoormann, Christ, & Hohnsbein, 2000), with larger positive values reflecting larger error potentials. The time window for the response-locked ERPs (ERN, CRN, dERN) was defined from 0 to 120 ms following button press and for the preceding positivity 0 to 80 ms before this peak. For the stimulus-locked ERP (dFRN) a time window from 190 – 350 ms following feedback presentation and the preceding positive peak was defined. Thus, the difference in amplitude was used as an index of ERP amplitude as shown in Figure 2: larger positive amplitudes indicate larger negative deflections on error trials. Although some have identified potential pitfalls of using difference waves (Van Boxtel, 2004), all results show the same qualitative pattern when the error-specific ERP (ERN or FRN) was included in the analyses1. Cohen’s d were calculated for t-tests and R2 scores are reported for correlations.
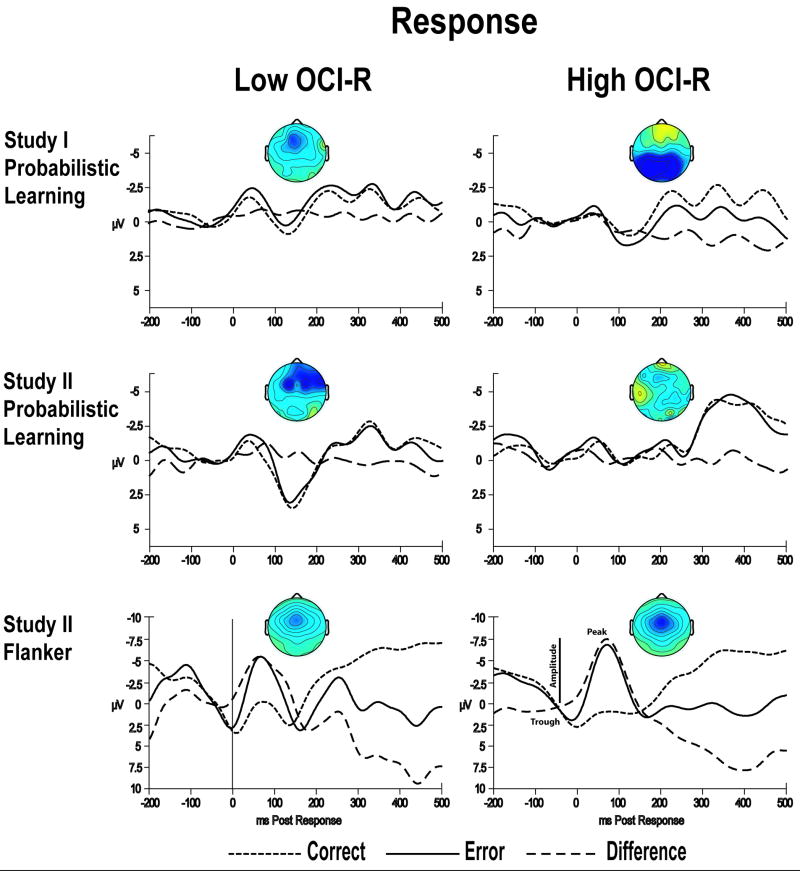
Figure 2.
Response-locked grand-average waveforms from the Cz electrode for correct and erroneous responses, and the difference wave. High and low OCI-R groups are shown separately, with ERPs from the probabilistic learning task (testing phase) in Study I and the probabilistic learning task (testing phase) and the flanker task for Study II. Scalp maps display the voltage distribution of the difference wave (from 0 – 100 ms), and are scaled from -1.5 to 1.5 μV for the probabilistic learning tasks and -10 to 10 μV for the flanker task. An example for the measurement of the dERN is detailed in the southeast ERP plot, where the larger dERN amplitudes are measured as a more positive value representing the distance between the preceding through and subsequent peak.
Results
Study I (Probabilistic Learning Task)
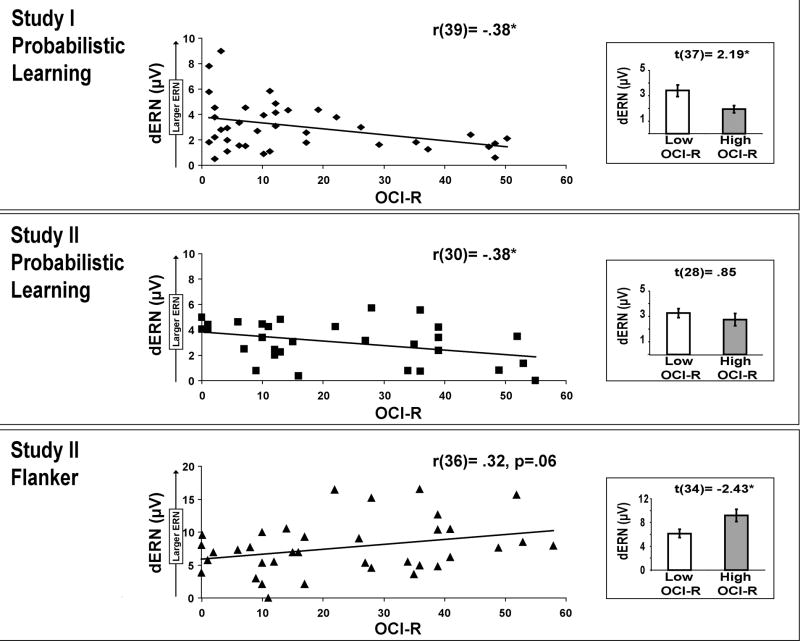
The high and low OC group showed virtually identical performance accuracy, no between group effect on Go or NoGo learning (F(1,38)=.12, p=.73) and no interaction between group and Go or NoGo learning (F(1,38)=.02, p=.88) in the testing phase2. See Table 1 for mean test phase accuracies by group. ERN amplitude (but not dERN amplitude) significantly correlated with NoGo learning (r(39)=.34, p=.04, R2=.12), with no Group * ERN interaction (F= .47). The waveforms from the central electrode site Cz are shown for response-locked ERPs in Figure 2, and for stimulus-locked ERPs in Figure 3. Figure 4 shows that the dERN amplitude systematically differed between the low and high OC group, where high OC participants had smaller dERN amplitudes (t(37)=2.19, p=.04, d=.72). Treating OC as a continuous measure, higher OCI-R scores similarly predicted lower dERN amplitudes (r(39)=- .38, p=.02, R2=.14, see Fig. 4).
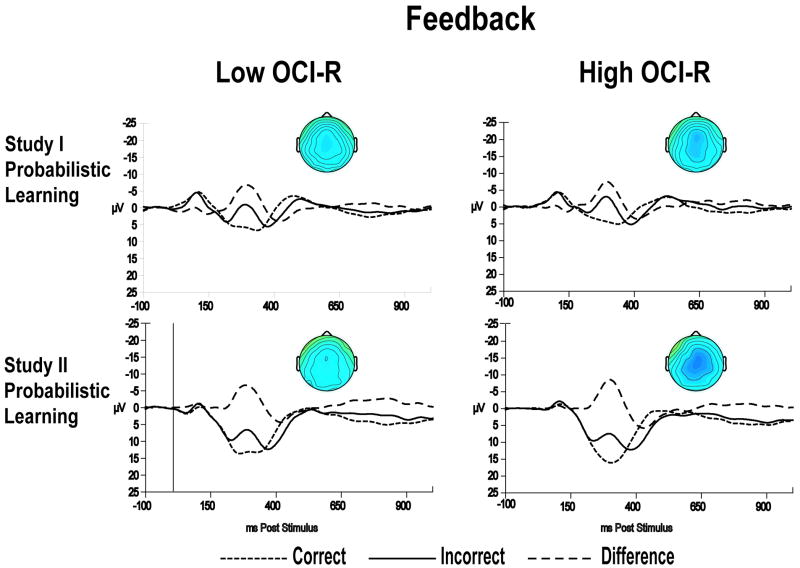
Figure 3.
Stimulus-locked grand-average waveforms from the Cz electrode for feedback (‘Correct’ or ‘Incorrect’) during the probabilistic learning task (training phase), and the difference wave. Scalp maps display the voltage distribution of the difference wave (from 250-350 ms), and are scaled from -15 to 15 μV.
Figure 4.
dERN amplitude at Cz as a function of OCI-R score for the probabilistic learning task in Study I and the probabilistic learning task and the flanker task in Study II. A smaller dERN was recorded for the high OC group during the probabilistic learning task in Study I and Study II compared to the low OC group. However a larger dERN was recorded for the high OC group during the flanker task in Study II compared to the low OC group.
To examine potential group differences in the acquisition phase of the probabilistic learning task, the dFRN component was examined. There was no difference between the low and high groups (t(38)=-.03, p=.97), nor did the dFRN amplitude significantly correlate with OCI-R scores (r(39)=-.13, p=.44). Depressive symptoms were more pronounced in the high group, as demonstrated by a significant correlation between BDI and OCI-R scores (r(40)=.69, p<.01, R2=.48). The correlation between depressive symptoms and dERN was also significant (r(39)=-.39, p=.01, R2=.15) where higher BDI scores predicted smaller dERN amplitudes.
Study II (Probabilistic Learning Task)
The first part of Study II replicated the experiment from Study I with an independent sample. No between group effect on Go or NoGo learning (F(1,28)=1.52, p=.23) and no interaction between OC group and Go or NoGo learning was found (F(1,28)=.004, p=.95). Neither ERN amplitude nor dERN amplitude significantly correlated with NoGo learning (p’s > .12), nor was there a significant Group * ERN interaction (F=3.1). Higher OCI-R scores predicted lower dERN amplitudes (r(30)=-.38, p= .04, R2=.14), replicating the main finding from Study I (although the dichotomized group difference failed to reach significance t(28)=.85, p>0.5). When the data from Study I and Study II are combined, ERN amplitude (but not dERN amplitude) correlates with NoGo learning (r(69)=.26, p=.03, R2=.07), with no significant Group * ERN interaction (F=1.2). These combined data also show that OCI-R scores negatively correlate with both ERN (r(69)=-.31, p<.01, R2=.10) and dERN (r(69)=-.36, p<.01, R2=.13) amplitudes, but does not correlate with NoGo learning (r(70)=-.06, p=.70).
Higher OCI-R scores also predicted lower dFRN amplitudes (r(30)=-.42, p=.02, R2=.18), with a significant difference between groups (low: M=12.22μV, SE=9.40; high: M=4.75 μV, SE=5.12; t(28)=2.65, p=.01, d =1.0). There was a non-significant correlation between OCI-R and BDI scores (r(30)=.33, p=.07), but the dERN was not correlated with depressive symptoms (r(30)=-.07, p=.71).
Study II (Flanker Task)
The high OCI-R group responded slightly more slowly than the low OCI-R group on correct (high OC: M=462 ms, SD=56; low OC: M=453 ms, SD=70) and erroneous trials (high OC: M=432 ms, SD=73; low OC: 419, SD=85), but there were no significant correlations between OCI-R and reaction times to correct or erroneous responses (correct response: r(29)=-.06,p=.77; incorrect response: r(29)=-.08, p=.69), and the group differences were not significant. Participants with high OCI-R scores also had slightly lower error rates (high OC: M=63.6, SD=23.5; low OC: M=72.7, SD 41.9) but correlations between OCI-R score and error rate (r(30)=.21, p=.27), post-error slowing (r(30)=-.06, p=.76), and percentage of self-corrected errors (r(29)=-.07, p=.71) were not significant. There were no between group differences regarding error rate, post-error slowing or percentage of self-corrected errors. Consistent with previous research, the high OCI-R group was characterized by larger dERN amplitudes than the low OCI-R group (t(34)=-2.43, p=.02, d =.83) as shown in Figures 2 and 4. The direct correlation between dERN and OCI-R approached statistically significance (r(36)=.32,p=.06, R2=.10). The dERN was not significantly correlated with BDI scores (r(36)=.28, p=.10).
To verify that the task dissociation in dERN amplitudes as a function of OCI-R score was not due to equivocal ERN and CRN amplitudes in the probabilistic learning task, yet different ERN and CRN amplitudes in the flanker task, separate correlations were calculated between OCI-R score and the ERN, CRN, and dERN amplitudes for each task. The correlations between OCI-R and ERN amplitudes were all in the same direction as the dERN but the relationship was not as strong. The correlations between OCI-R and CRN amplitudes were also weak and in the same direction as the dERN, except for a non-significant positive correlation between OCI-R score and the Study II CRN amplitude for the probabilistic learning task. Thus, the task dissociation in dERN amplitudes as a function of OCI-R score does not appear to be contingent on a pattern of differential variation between conditions within any of the tasks.
Discussion
Study I revealed diminished dERN amplitudes in a probabilistic learning task as a function of higher OC symptomatology, with no differences in avoidance learning. These findings were replicated in a second independent sample, which also replicated the increasingly robust findings from the literature of larger dERN amplitudes in simple motor response tasks as a function of higher OC symptoms (Endrass et al., 2008; Gehring et al., 2000; Hajcak et al., 2008; Hajcak & Simons, 2002; Johannes et al., 2001; Ruchsow et al., 2005; Santesso et al., 2006). This finding of a task-related dissociation in dERN amplitude as a function of obsessive-compulsive symptoms indicates that different, yet partially overlapping neural mechanisms may underlie the ERN following the execution of an erroneous motor response and following suboptimal choices in a probabilistic learning paradigm. Differential modulation of medial prefrontal systems may be related to obsessive-compulsive symptoms, with hypoactivity in systems promoting active avoidance, but hyperactivity in systems that perpetuate a previously maladaptive response. The former process may contribute to the inability to learn to avoid making repetitive behaviors that continually produce error signals (which would otherwise serve to extinguish such behaviors), and the latter may further exacerbate this situation by causing repeated attempts to ‘perfect’ behaviors that did not produce the desired outcome.
The lack of behavioral differences in the tasks reported here suggests that the OC-dependant modulation of underlying neural systems may not reflect hyperactive action monitoring tendencies, and also that the differential activation of these systems in OCD may not directly lead to alterations in behavior on these tasks, a finding generally consistent with the extant literature on OC populations and error monitoring (Endrass et al., 2008; Fitzgerald et al., 2005; Gehring et al., 2000; Hajcak & Simons, 2002; Johannes et al., 2001; Maltby et al., 2005; Nieuwenhuis et al., 2005; Ruchsow et al., 2005; Santesso et al., 2006; Ursu et al., 2003). A predicted correlation between ERN amplitude and avoidance (NoGo) learning was supported in this investigation (Frank et al., 2007; Frank et al., 2005a), although this correlation was non-significant with dERN amplitude. While there were slight variations in the predictive power of ERN or dERN amplitudes, combined data from Study I and Study II indicate that larger ERN amplitudes correlated positively with NoGo learning and negatively with OCI-R score, yet OCI-R score did not relate to NoGo learning.
A previous report detailed a null-result regarding ERN and FRN differences between OCD patients and a control group utilizing a probabilistic learning task (Nieuwenhuis et al., 2005a). In fact, this investigation found a non-significant negative correlation between OCD and ERN amplitude, a previous anomaly in the literature of OC populations and the ERN, but one that is in line with the findings presented here. The authors of this study speculated that trial-to-trial feedback reduces action monitoring demands in OCD, and that the response-monitoring system in OCD may only become hyperactive once stimulus-response mappings are known. These two processes, trial-to-trial feedback and undetermined stimulus-response mappings, are hallmarks of reinforcement learning. We suggest a broader perspective: that there are fundamental differences in the neural systems underlying suboptimal choices during reinforcement learning and motor errors of commission, and that OC symptoms reflect dissociation in the functioning of these systems.
A number of studies have examined hyperactive error signals as an electrophysiological correlate of performance monitoring in psychiatric populations (for a review see: Ullsperger, 2006 as well as Olvet & Hajcak 2008). Depression, pathological worry, trait anxiety and negative affect have been characterized by increased error-related signal amplitudes (Hajcak, McDonald, Simons, 2004; Chiu & Deldin, 2007; Hajcak, McDonald, & Simons, 2003; Luu, Collins, & Tucker, 2000; Tucker, Luu, Frishkoff, Quiring, & Poulsen, 2003, Paulus, Feinstein, Simmons & Stein, 2004), but see Ruchsow et al. (2006; 2004). Arguably, all internalizing psychiatric disorders mentioned above may be characterized by increased sensitivity to errors, whereas externalizing aspects of psychiatric disorders (e.g. impulsivity, substance abuse) are associated with decreased error related activity (Ridderinkhof et al., 2002; Franken, van Strien, Franzek, & van de Wetering, 2007; Easdon et al., 2005). However, there has never been a theory of why ERN amplitudes should be differently modulated by task demands as a function of psychopathological traits. This phenomenon offers a simple methodological advancement that may be applied to future investigations of how medial prefrontal systems are differentially affected by aspects of psychopathology.
Comorbidity between OCD and depression is reported to be high, with as many as one-half of OCD patients suffering from Major Depressive Disorder (Abramowitz, Storch, Keeley, & Cordell, 2007; Hong et al., 2004; Nestadt et al., 2001). Only Study I demonstrated a correlation between OCI-R and BDI and between BDI and dERN amplitude. However, given that neither of these correlations were obtained in the second sample with either the probabilistic learning paradigm or the flanker task, it seems more parsimonious to conclude that these ERN alterations are more likely to be related to OC symptomatology than comorbid depressive symptomatology in this investigation. The use of student populations for clinical analogues demands replication with OCD patients, but this methodology provides unique advantages: the psycho-pharmaceutical naivety of the studied group, homogeneity in age, and the ease of using larger sample sizes. Moreover, because a diagnostic interview was not administered, it may well be the case that some of the participants in the present studies in fact meet OCD diagnostic criteria, which would not be surprising given the early age of onset (Lensi et al., 1996; Rasmussen & Eisen, 1992; Swedo et al., 1989) and reasonably prevalent nature of OCD (Leon et al., 1995; Rasmussen & Eisen, 1992; Regier et al., 1993). Future investigations with both patient and symptomatic non-patient populations will help determine whether the observed pattern of findings replicates in more severe patient groups. If so, this present approach will be useful for identifying alterations in neural systems responsible for cognitive control and reinforcement learning.
Different neural systems have been implicated in the generation of the ERN. Outcomes that are worse than expected are characterized in the midbrain by a phasic decrease in dopaminergic tone (Hollerman & Schultz, 1998; Schultz, 2007). The reinforcement learning theory of the ERN posits that these dips in tonic dopaminergic tone cause a disinhibition of dorsal ACC neurons, generating medio-frontal negativities (Holroyd & Coles, 2002), although the reverse pattern of causation has also been suggested (Frank et al., 2005a; Pizzagalli et al., 2008). The ACC is futhermore implicated in the conflict model theory of the ERN, which posits that the degree of motor response interference causes response-related activation in the ACC (Carter et al., 1998; Yeung, Cohen, & Botvinick, 2004). However, neither of these theories predicts a situation where ERN amplitude should be dissociated in an interaction between task and individual differences, especially in the absence of behavioral effects.
Enhanced ERN amplitudes in OCD patients have been interpreted as in line with the neurobiological mismatch theory of OCD, whereby hyperactive error signals are trapped in a dysfunctional comparator which detects a mismatch between actual and intended response (Gehring et al., 2000; Pitman, 1987). However, recent findings suggest that a putative performance-monitoring dysfunction is not selective to error processing, since altered correct-response negativities are also observed (Endrass et al., 2008; Hajcak & Simons, 2002). In this investigation, the Feedback Related Negativity was either the same size (Study I) or smaller (Study II) than non-symptomatic controls, which also suggests that there are pervasive effects of OCD on ACC activity. It is apparent that the theoretical accounts of the ERN cannot fully explain the pattern of results from this study, although it is clear that individual difference investigations can offer evidence for future theoretical advancement of the neural systems underlying the ERN. Although there was no difference in the percentage of self-corrected trials between the groups, a possible difference in Flanker dERN amplitudes between OCI-R groups could have been due to self-corrected vs. uncorrected errors (Gehring et al., 1993; Ullsperger & von Cramon, 2006), but this possibility could not be investigated here due to inadequate trial counts. Since the ACC plays a necessary role in the immediate self-correction of an error (Modirrousta & Fellows, 2008), this specific dynamic of error processing remains an intriguing variable for future investigations to parse the specificity of performance monitoring in psychiatric populations.
Evidence from the fMRI literature has shown that error and conflict-related hemodynamic responses in OCD patients are different between rostral and caudal areas (Fitzgerald et al., 2005; Maltby et al., 2005; Ursu et al., 2003). The rostral part of the ACC has been related to assessing the salience of emotional and motivational information, and often shows a trade-off in activation with more dorsal areas (Bush et al., 1998). The reciprocal activation of rostral and dorsal ACC, possibly differentially altered by OCD, might explain this dissociation in medio-frontal response related ERPs. Both rostral and dorsal areas of the ACC have been implicated in the generation of the ERN and FRN (Gehring & Willoughby, 2002; Holroyd, Larsen, & Cohen, 2004; Miltner, Braun, & Coles, 1997; Nieuwenhuis, Slagter, von Geusau, Heslenfeld, & Holroyd, 2005; Ullsperger & von Cramon, 2003), perhaps due to partial phase resetting and amplitude enhancement of the frontal midline theta (Luu, Tucker, Derryberry, Reed, & Poulsen, 2003; Luu, Tucker, & Makeig, 2004; Trujillo & Allen, 2007; Cavanagh, Cohen & Allen, 2009). Given that conflict activation has been localized more dorsally and error monitoring more ventrally in medial prefrontal cortex, (Luu et al., 2003; Luu et al., 2004; Ullsperger & von Cramon, 2001), it is possible that differential activation of these separate yet partially overlapping neural systems may underlie task-specific ERN alterations as a function of OC symptomatology.
The finding that OC symptomatology was characterized by a smaller dERN in a reinforcement learning task and a larger dERN in an error commission task provides a novel foundation for future research on the role of the ACC in health and disease. OC-related alteration of the ERN may not simply be reflective of altered brain dynamics related to a ‘hyperactive action monitoring system’. Differential modulation of medial prefrontal systems may be related to obsessive-compulsive symptoms: with hypoactivity in systems promoting active avoidance, but hyperactivity in systems that perpetuate a previously maladaptive response. It is likely that there are not general behavioral impairments in action monitoring in OCD, but that OCD may be specifically characterized by a dysfunction in learning to stop making repetitive actions that produce bad outcomes. For example, it is assumed that probabilistic reversal learning is compromised in OCD patients (Kim et al., 2003; Remijnse et al., 2006; Chamberlain et al., 2008; Valerius et al., 2008), fitting with a diminished ability to avoid repetitive mistakes. Future EEG studies of OCD should investigate the role of the ERN in tasks that require avoidance of repetitive mistakes, and the possibility of differential functioning of separate, yet overlapping medial prefrontal systems involved in action monitoring.
Acknowledgments
The authors thank Antonia Kaczurkin for her assistance with data recording, all graduate students affiliated with the University of Arizona psychophysiology laboratory and Markus Ullsperger and Tilmann Klein for helpful comments on an earlier draft of this manuscript. This study benefitted from infrastructure provided by grant R01- MH066902. JFC is supported by F31MH082560.
Footnotes
- Study I: Reinforcement Learning Task
- CRN: Low M=166 (±SD 26), High M=160 (±SD 29)
- ERN (and dERN): Low M=65 (±SD 22), High M=68 (±SD 25)
- FRN (and dFRN): Low M=143 (±SD 59), High M=147 (±SD 83)
- Correct Feedback: Low M=199 (±SD 73), High M=200 (±SD 91)
- Study II: Reinforcement Learning Task
- CRN: Low M=83 (± SD 13), High M=83 (±SD 14)
- ERN (and dERN): Low M=34 (±SD 11), High M=36 (±SD 14)
- FRN (and dFRN): Low M=85 (±SD 61), High M=113 (±SD 53)
- Correct Feedback: Low M=114 (±SD 72), High M=152 (±SD 60)
- Study II: Flankers Task
- CRN: Low M=306 (±SD 53), High M=313 (± SD=47)
- ERN (and dERN): Low M=71 (±SD 43), High M=59 (±SD=22)
There were no significant group differences or correlations with the OCI-R on the measures of training phase accuracy (AB, CD, or EF pairs), or the number of blocks (both groups had a mean of 4 blocks) in any of the probabilistic learning tasks in Study I or Study II. Additionally, test phase accuracies were split based on the reinforcement value difference between stimuli into low conflict (easy choice, large distance in reinforcement value as in ‘AD’) and high conflict (difficult choice, small distance in reinforcement value as in ‘AC’) situations (Frank, Woroch & Curran, 2005a; Frank, Samanta, Moustafa & Sherman, 2007). There were no significant group differences or correlations with the OCI-R on any measures of conflict: except a single group comparison where the High OCI-R group had better high conflict test phase accuracy only in Study II, a result which appears to be driven by outliers in the Low OCI-R group. All response-related ERPs in these conditions were inversely related to OCI-R score (largely non-significantly), regardless of the level of response conflict (low or high). There was no conflict (high, low) * OCI-R interaction for ERP amplitudes (F= .21) when tested in the combined sample. These data indicate that there are no pervasive differences on any aspect of reinforcement learning in these samples, and that response-related ERP amplitudes are unchanged or reduced as a function of OCI-R score regardless of the reinforcement condition.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Theo O.J. Gründler, Max Planck Institute for Neurological Research, Cognitive Neurology Group, Cologne, Germany.
James F. Cavanagh, University of Arizona, Psychophysiology Laboratory, Tucson, USA, University of Arizona, Laboratory for Neural Computation and Cognition, Tucson, USA.
Christina M. Figueroa, University of Arizona, Psychophysiology Laboratory, Tucson, USA, University of Arizona, Laboratory for Neural Computation and Cognition, Tucson, USA
Michael J. Frank, University of Arizona, Laboratory for Neural Computation and Cognition, Tucson, USA
John J.B. Allen, University of Arizona, Psychophysiology Laboratory, Tucson, USA.
References
- Abramowitz JS, Storch EA, Keeley M, Cordell E. Obsessive-compulsive disorder with comorbid major depression: what is the role of cognitive factors? Behaviour Research and Therapy. 2007;45(10):2257–2267. doi: 10.1016/j.brat.2007.04.003. [DOI] [PubMed] [Google Scholar]
- Adler CM, McDonough-Ryan P, Sax KW, Holland SK, Arndt S, Strakowski SM. fMRI of neuronal activation with symptom provocation in unmedicated patients with obsessive compulsive disorder. Journal of Psychiatric Research. 2000;34(45):317–324. doi: 10.1016/s0022-3956(00)00022-4. [DOI] [PubMed] [Google Scholar]
- Angst J, Gamma A, Endrass J, Goodwin R, Ajdacic V, Eich D, Rössler W. Obsessive-compulsive severity spectrum in the community: prevalence, comorbidity, and course. Europeen Archives of Psychiatry and Clinical Neurosience. 2004;254(3):156–164. doi: 10.1007/s00406-004-0459-4. [DOI] [PubMed] [Google Scholar]
- Balleine BW, Delgado MR, Hikosaka O. The role of the dorsal striatum in reward and decision-making. Journal of Neuroscience. 2007;27(31):8161–8165. doi: 10.1523/JNEUROSCI.1554-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baxter LR, Jr, Schwartz JM, Guze BH, Bergman K, Szuba MP. PET imaging in obsessive compulsive disorder with and without depression. Journal of Clinical Psychiatry. 1990;51(Suppl):61–69. discussion 70. [PubMed] [Google Scholar]
- Baxter LR., Jr . Functional imaging of brain systems mediating obsessive-compulsive disorder: clinical studies. In: Charney DS, Nestler EJ, Bunney BS, editors. Neurobiology of Mental Illness. New York: Oxford University Press; 1999. pp. 534–547. [Google Scholar]
- Breiter HC, Rauch SL. Functional MRI and the study of OCD: from symptom provocation to cognitive-behavioral probes of cortico-striatal systems and the amygdala. Neuroimage. 1996;4(3 Pt 3):S127–138. doi: 10.1006/nimg.1996.0063. [DOI] [PubMed] [Google Scholar]
- Bush G, Whalen PJ, Rosen BR, Jenike MA, McInerney SC, Rauch SL. The counting Stroop: an interference task specialized for functional neuroimaging--validation study with functional MRI. Human brain mapping. 1998;6(4):270–282. doi: 10.1002/(SICI)1097-0193(1998)6:4<270::AID-HBM6>3.0.CO;2-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter CS, Braver T, Barch DM, Botvinick M, Noll D, Cohen JD. Anterior cingulate, error detection and performance monitoring: An event related fMRI study. Journal of Cognitive Neuroscience. 1998:107–107. [Google Scholar]
- Cavanagh JF, Allen JJ. Multiple aspects of the stress response under social evaluative threat: an electrophysiological investigation. Psychoneuroendocrinology. 2008;33(1):41–53. doi: 10.1016/j.psyneuen.2007.09.007. [DOI] [PubMed] [Google Scholar]
- Cavanagh JF, Cohen MX, Allen JJ. Prelude to and resolution of an error: EEG phase synchrony reveals cognitive control dynamics during action monitoring. Journal of Neuroscience. 2009;29(1):98–105. doi: 10.1523/JNEUROSCI.4137-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamberlain SR, Menzies L, Hampshire A, Suckling J, Fineberg NA, del Campo N, Aitken M, Craig K, Owen AM, Bullmore ET, Robbins TW, Sahakian BJ. Orbitofrontal dysfunction in patients with obsessive-compulsive disorder and their unaffected relatives. Science. 2008;321:421–422. doi: 10.1126/science.1154433. [DOI] [PubMed] [Google Scholar]
- Chiu PH, Deldin PJ. Neural evidence for enhanced error detection in major depressive disorder. American Journal of Psychiatry. 2007;164(4):608–616. doi: 10.1176/ajp.2007.164.4.608. [DOI] [PubMed] [Google Scholar]
- Cottraux J, Gerard D, Cinotti L, Froment JC, Deiber MP, Le Bars D, et al. A controlled positron emission tomography study of obsessive and neutral auditory stimulation in obsessive-compulsive disorder with checking rituals. Psychiatry Research. 1996;60(23):101–112. doi: 10.1016/0165-1781(96)02697-2. [DOI] [PubMed] [Google Scholar]
- Debener S, Ullsperger M, Siegel M, Fiehler K, von Cramon DY, Engel AK. Trial-by-trial coupling of concurrent electroencephalogram and functional magnetic resonance imaging identifies the dynamics of performance monitoring. Journal of Neuroscience. 2005;25(50):11730–11737. doi: 10.1523/JNEUROSCI.3286-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dehaene S, Posner MI, Tucker DM. Localization of a Neural System for Error Detection and Compensation. Psychological Science. 1994;(5):303–305. [Google Scholar]
- DSM-IV. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Easdon C, Izenberg A, Armilio L, Yu H, Alain C. Alcohol consumption impairs stimulus-and error-related processing during a Go/No-Go Task. Cognitive Brain Research. 2005;25(3):873–883. doi: 10.1016/j.cogbrainres.2005.09.009. [DOI] [PubMed] [Google Scholar]
- Endrass T, Klawohn J, Schuster F, Kathmann N. Overactive performance monitoring in obsessive-compulsive disorder: ERP evidence from correct and erroneous reactions. Neuropsychologia. 2008;46(7):1877–1887. doi: 10.1016/j.neuropsychologia.2007.12.001. [DOI] [PubMed] [Google Scholar]
- Falkenstein M, Hohnsbein J, Hoormann J, Blanke L. Effects of crossmodal divided attention on late ERP components. II. Error processing in choice reaction tasks. Electroencephalography and clinical neurophysiology. 1991;78(6):447–455. doi: 10.1016/0013-4694(91)90062-9. [DOI] [PubMed] [Google Scholar]
- Falkenstein M, Hoormann J, Christ S, Hohnsbein J. ERP components on reaction errors and their functional significance: A tutorial. Biological Psychology. 2000;51(23):87–107. doi: 10.1016/s0301-0511(99)00031-9. [DOI] [PubMed] [Google Scholar]
- Fireman B, Koran LM, Leventhal JL, Jacobson A. The prevalence of clinically recognized obsessive-compulsive disorder in a large health maintenance organization. American Journal of Psychiatry. 2001;158(11):1904–1910. doi: 10.1176/appi.ajp.158.11.1904. [DOI] [PubMed] [Google Scholar]
- Fitzgerald KD, Welsh RC, Gehring WJ, Abelson JL, Himle JA, Liberzon I, et al. Error-related hyperactivity of the anterior cingulate cortex in obsessive-compulsive disorder. Biological Psychiatry. 2005;57(3):287–294. doi: 10.1016/j.biopsych.2004.10.038. [DOI] [PubMed] [Google Scholar]
- Foa EB, Kozak MJ, Salkovskis PM, Coles ME, Amir N. The validation of a new obsessive-compulsive disorder scale: The Obsessive-Compulsive Inventory. Psychological Assessment. 1998;10(3):206–214. [Google Scholar]
- Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, et al. The Obsessive-Compulsive Inventory: development and validation of a short version. Psychological assessment. 2002;14(4):485–496. [PubMed] [Google Scholar]
- Forster J, Forster K. DMDX Display Software. Tucson: University of Arizona; 1999. [Google Scholar]
- Frank MJ, Seeberger LC, O’Reilly RC. By carrot or by stick: cognitive reinforcement learning in parkinsonism. Science. 2004;306(5703):1940–1943. doi: 10.1126/science.1102941. [DOI] [PubMed] [Google Scholar]
- Frank MJ, Woroch BS, Curran T. Error-related negativity predicts reinforcement learning and conflict biases. Neuron. 2005a;47(4):495–501. doi: 10.1016/j.neuron.2005.06.020. [DOI] [PubMed] [Google Scholar]
- Frank MJ. Dynamic dopamine modulation in the basal ganglia: a neurocomputational account of cognitive deficits in medicated and nonmedicated Parkinsonism. Journal of Cognitive Neuroscience. 2005b;17(1):51–72. doi: 10.1162/0898929052880093. [DOI] [PubMed] [Google Scholar]
- Frank MJ, D’Lauro C, Curran T. Cross-task individual differences in error processing: neural, electrophysiological, and genetic components. Cognitive, Affective & Behavioral Neuroscience. 2007;7(4):297–308. doi: 10.3758/cabn.7.4.297. [DOI] [PubMed] [Google Scholar]
- Frank MJ, Samanta J, Moustafa AA, Sherman SJ. Hold your horses: impulsivity, deep brain stimulation, and medication in parkinsonism. Science. 2007;318(5854):1309–1312. doi: 10.1126/science.1146157. [DOI] [PubMed] [Google Scholar]
- Franken JH, van Strien JW, Franzek EJ, van de Wetering BJ. Error-processing in patients with cocaine dependence. Biological Psychology. 2007;75(1):45–51. doi: 10.1016/j.biopsycho.2006.11.003. [DOI] [PubMed] [Google Scholar]
- Fullana MA, Tortella-Feliu M, Caseras X, Andion O, Torrubia R, Mataix-Cols D. Psychometric properties of the Spanish version of the Obsessive-Compulsive Inventory--revised in a non-clinical sample. Journal of anxiety disorders. 2005;19(8):893–903. doi: 10.1016/j.janxdis.2004.10.004. [DOI] [PubMed] [Google Scholar]
- Gehring WJ, Coles MGH, Meyer DE, Donchin E. The error-related negativity: an event-related brain potential accompanying errors. Psychophysiology. 1990;27:34. [Google Scholar]
- Gehring WJ, Goss B, Coles MGH, Meyer DE, Donchin E. A neural system for error-detection and compensation. Psychological Science. 1993;4(6):385–390. [Google Scholar]
- Gehring WJ, Himle J, Nisenson LG. Action-monitoring dysfunction in obsessive-compulsive disorder. Psychological Science. 2000;11(1):1–6. doi: 10.1111/1467-9280.00206. [DOI] [PubMed] [Google Scholar]
- Gehring WJ, Willoughby AR. The medial frontal cortex and the rapid processing of monetary gains and losses. Science. 2002;295(5563):2279–2282. doi: 10.1126/science.1066893. [DOI] [PubMed] [Google Scholar]
- Hajcak G, Simons RF. Error-related brain activity in obsessive-compulsive undergraduates. Psychiatry Research. 2002;110(1):63–72. doi: 10.1016/s0165-1781(02)00034-3. [DOI] [PubMed] [Google Scholar]
- Hajcak G, McDonald N, Simons RF. Anxiety and error-related brain activity. Biological Psychology. 2003;64(12):77–90. doi: 10.1016/s0301-0511(03)00103-0. [DOI] [PubMed] [Google Scholar]
- Hajcak G, Huppert JD, Simons RF, Foa EB. Psychometric properties of the OCI-R in a college sample. Behavior Research and Therapy. 2004a;42(1):115–123. doi: 10.1016/j.brat.2003.08.002. [DOI] [PubMed] [Google Scholar]
- Hajcak G, McDonald N, Simons RF. Error-related psychophysiology and negative affect. Brain and Cognition. 2004b;56(2):189–197. doi: 10.1016/j.bandc.2003.11.001. [DOI] [PubMed] [Google Scholar]
- Hajcak G, Franklin ME, Foa EB, Simons RF. Increased error-related brain activity in pediatric obsessive-compulsive disorder before and after treatment. American Journal of Psychiatry. 2008;165(1):116–123. doi: 10.1176/appi.ajp.2007.07010143. [DOI] [PubMed] [Google Scholar]
- Hollerman JR, Schultz W. Dopamine neurons report an error in the temporal prediction of reward during learning. Nature Neuroscience. 1998;1(4):304–309. doi: 10.1038/1124. [DOI] [PubMed] [Google Scholar]
- Holroyd CB, Coles MG. The neural basis of human error processing: reinforcement learning, dopamine, and the error-related negativity. Psychological Review. 2002;109(4):679–709. doi: 10.1037/0033-295X.109.4.679. [DOI] [PubMed] [Google Scholar]
- Holroyd CB, Larsen JT, Cohen JD. Context dependence of the event-related brain potential associated with reward and punishment. Psychophysiology. 2004;41(2):245–253. doi: 10.1111/j.1469-8986.2004.00152.x. [DOI] [PubMed] [Google Scholar]
- Hong JP, Samuels J, Bienvenu OJ, 3rd, Cannistraro P, Grados M, Riddle MA, Liang K, Cullen B, Hoehn-Saric R, Nestadt G. Clinical correlates of recurrent major depression in obsessive-compulsive disorder. Depression and Anxiety. 2004;20(2):86–91. doi: 10.1002/da.20024. [DOI] [PubMed] [Google Scholar]
- Huppert JD, Walther MR, Hajcak G, Yadin E, Foa EB, Simpson HB, Yadin E, Foa EB, Simpson HB, Liebowitz MR. The OCI-R: validation of the subscales in a clinical sample. Journal of Anxiety Disorders. 2007;21(3):394–406. doi: 10.1016/j.janxdis.2006.05.006. [DOI] [PubMed] [Google Scholar]
- Ito S, Stuphorn V, Brown JW, Schall JD. Performance monitoring by the anterior cingulate cortex during saccade countermanding. Science. 2003;302(5642):120–122. doi: 10.1126/science.1087847. [DOI] [PubMed] [Google Scholar]
- Johannes S, Wieringa BM, Nager W, Rada D, Dengler R, Emrich HM, Münte TF, Dietrich DE. Discrepant target detection and action monitoring in obsessive-compulsive disorder. Psychiatry Research. 2001;108(2):101–110. doi: 10.1016/s0925-4927(01)00117-2. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kim CH, Chang JW, Koo MS, Kim JW, Suh HS, Park IH, Lee HS. Anterior cingulotomy for refractory obsessive-compulsive disorder. Acta Psychiatrica Scandinavica. 2003;107(4):283–290. doi: 10.1034/j.1600-0447.2003.00087.x. [DOI] [PubMed] [Google Scholar]
- Lensi P, Cassano GB, Correddu G, Ravagli S, Kunovac JL, Akiskal HS. Obsessive-compulsive disorder. Familial-developmental history, symptomatology, comorbidity and course with special reference to gender-related differences. British Journal of Psychiatry. 1996;169(1):101–107. doi: 10.1192/bjp.169.1.101. [DOI] [PubMed] [Google Scholar]
- Leon AC, Olfson M, Broadhead WE, Barrett JE, Blacklow RS, Keller MB, Higgins ES, Weissman MM. Prevalence of mental disorders in primary care. Implications for screening. Archives of Famíly Medicine. 1995;4(10):857–861. doi: 10.1001/archfami.4.10.857. [DOI] [PubMed] [Google Scholar]
- Luu P, Collins P, Tucker DM. Mood, personality, and self-monitoring: negative affect and emotionality in relation to frontal lobe mechanisms of error monitoring. Journal of experimental psychology. 2000;129(1):43–60. doi: 10.1037//0096-3445.129.1.43. [DOI] [PubMed] [Google Scholar]
- Luu P, Tucker DM, Derryberry D, Reed M, Poulsen C. Electrophysiological responses to errors and feedback in the process of action regulation. Psychological Science. 2003;14(1):47–53. doi: 10.1111/1467-9280.01417. [DOI] [PubMed] [Google Scholar]
- Luu P, Tucker DM, Makeig S. Frontal midline theta and the error-related negativity: neurophysiological mechanisms of action regulation. Clinical Neurophysiology. 2004;115(8):1821–1835. doi: 10.1016/j.clinph.2004.03.031. [DOI] [PubMed] [Google Scholar]
- Maddox WT, Ashby FG, Bohil CJ. Delayed feedback effects on rule-based and information-integration category learning. Journal of Experimental Psychology: Learning, Memory and Cognition. 2003;29(4):650–662. doi: 10.1037/0278-7393.29.4.650. [DOI] [PubMed] [Google Scholar]
- Maltby N, Tolin DF, Worhunsky P, O’Keefe TM, Kiehl KA. Dysfunctional action monitoring hyperactivates frontal-striatal circuits in obsessive-compulsive disorder: an event-related fMRI study. Neuroimage. 2005;24(2):495–503. doi: 10.1016/j.neuroimage.2004.08.041. [DOI] [PubMed] [Google Scholar]
- Miltner WHR, Braun CH, Coles MGH. Event-related brain potentials following incorrect feedback in a time-estimation task: Evidence for a “generic” neural system for error detection. Journal of Cognitive Neuroscience. 1997;9(6):788–798. doi: 10.1162/jocn.1997.9.6.788. [DOI] [PubMed] [Google Scholar]
- Modirrousta M, Fellows LK. Dorsal medial prefrontal cortex plays a necessary role in rapid error prediction in humans. Journal of Neuroscience. 2008;28(51):14000–14005. doi: 10.1523/JNEUROSCI.4450-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nestadt G, Samuels J, Riddle MA, Liang KY, Bienvenu OJ, Hoehn-Saric R, Grados M, Cullen B. The relationship between obsessive-compulsive disorder and anxiety and affective disorders: results from the Johns Hopkins OCD Family Study. Psychological Medicine. 2001;31(3):481–487. doi: 10.1017/s0033291701003579. [DOI] [PubMed] [Google Scholar]
- Nicola SM. The nucleus accumbens as part of a basal ganglia action selection circuit. Psychopharmacology (Berl) 2007;191(3):521–550. doi: 10.1007/s00213-006-0510-4. [DOI] [PubMed] [Google Scholar]
- Nieuwenhuis S, Nielen MM, Mol N, Hajcak G, Veltman DJ. Performance monitoring in obsessive-compulsive disorder. Psychiatry Research. 2005a;134(2):111–122. doi: 10.1016/j.psychres.2005.02.005. [DOI] [PubMed] [Google Scholar]
- Nieuwenhuis S, Slagter HA, von Geusau NJA, Heslenfeld DJ, Holroyd CB. Knowing good from bad: differential activation of human cortical areas by positive and negative outcomes. European Journal of Neuroscience. 2005b;21(11):3161–3168. doi: 10.1111/j.1460-9568.2005.04152.x. [DOI] [PubMed] [Google Scholar]
- Olvet DM, Hajcak G. The error-related negativity (ERN) and psychopathology: Toward an endophenotype. Clinical Psychology Review. 2008;28(8):1343–1354. doi: 10.1016/j.cpr.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulus MP, Feinstein JS, Simmons A, Stein MB. Anterior cingulate activation in high trait anxious subjects is related to altered error processing during decision making. Biological Psychiatry. 2004;55(12):1179–1187. doi: 10.1016/j.biopsych.2004.02.023. [DOI] [PubMed] [Google Scholar]
- Perani D, Colombo C, Bressi S, Bonfanti A, Grassi F, Scarone S, Bellodi L, Smeraldi E, Fazio F. [18F]FDG PET study in obsessive-compulsive disorder. A clinical/metabolic correlation study after treatment. British Journal of Psychiatry. 1995;166(2):244–250. doi: 10.1192/bjp.166.2.244. [DOI] [PubMed] [Google Scholar]
- Pitman RK. A cybernetic model of obsessive-compulsive psychopathology. Comprehensive Psychiatry. 1987;28(4):334–343. doi: 10.1016/0010-440x(87)90070-8. [DOI] [PubMed] [Google Scholar]
- Pizzagalli DA, Evins AE, Schetter EC, Frank MJ, Pajtas PE, Santesso DL, Culhane M. Single dose of a dopamine agonist impairs reinforcement learning in humans: Behavioral evidence from a laboratory-based measure of reward responsiveness. Psychopharmacology. 2008;196(2):221–232. doi: 10.1007/s00213-007-0957-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen SA, Eisen JL. The epidemiology and clinical features of obsessive compulsive disorder. Psychiatric Clinics of North America. 1992;15(4):743–758. [PubMed] [Google Scholar]
- Rauch SL, Jenike MA, Alpert NM, Baer L, Breiter HC, Savage CR, Fischman AJ. Regional cerebral blood flow measured during symptom provocation in obsessive-compulsive disorder using oxygen 15-labeled carbon dioxide and positron emission tomography. Archives of General Psychiatry. 1994;51(1):62–70. doi: 10.1001/archpsyc.1994.03950010062008. [DOI] [PubMed] [Google Scholar]
- Regier DA, Narrow WE, Rae DS, Manderscheid RW, Locke BZ, Goodwin FK. The de facto US mental and addictive disorders service system. Epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Archives of General Psychiatry. 1993;50(2):85–94. doi: 10.1001/archpsyc.1993.01820140007001. [DOI] [PubMed] [Google Scholar]
- Remijnse PL, Nielen MM, van Balkom AJ, Cath DC, van Oppen P, Uylings HB, Veltman DJ. Reduced orbitofrontal-striatal activity on a reversal learning task in obsessive-compulsive disorder. Archives of General Psychiatry. 2006;63(11):1225–1236. doi: 10.1001/archpsyc.63.11.1225. [DOI] [PubMed] [Google Scholar]
- Ridderinkhof KR, de Vlugt Y, Bramlage A, Spaan M, Elton M, Snel J, Band GPH. Alcohol consumtion impairs detection of performance errors in mediofrontal cortex. Science. 2002;298(5601):2209–2211. doi: 10.1126/science.1076929. [DOI] [PubMed] [Google Scholar]
- Ruchsow M, Herrnberger B, Wiesend C, Gron G, Spitzer M, Kiefer M. The effect of erroneous responses on response monitoring in patients with major depressive disorder: A study with event-related potentials. Psychophysiology. 2004;41(6):833–840. doi: 10.1111/j.1469-8986.2004.00237.x. [DOI] [PubMed] [Google Scholar]
- Ruchsow M, Gron G, Reuter K, Spitzer M, Hermle L, Kiefer M. Error-related brain activity in patients with obsessive-compulsive disorder and in healthy controls. Journal of Psychophysiology. 2005;19(4):298–304. [Google Scholar]
- Ruchsow M, Herrnberger B, Beschoner P, Gron G, Spitzer M, Kiefer M. Error processing in major depressive disorder: Evidence from event-related potentials. Journal of Psychiatric Research. 2006;40(1):37–46. doi: 10.1016/j.jpsychires.2005.02.002. [DOI] [PubMed] [Google Scholar]
- Santesso DL, Segalowitz SJ, Schmidt LA. Error-related electrocortical responses are enhanced in children with obsessive-compulsive behaviors. Developmental Neuropsychology. 2006;29(3):431–445. doi: 10.1207/s15326942dn2903_3. [DOI] [PubMed] [Google Scholar]
- Schultz W. Multiple dopamine functions at different time courses. Annual Review of Neuroscience. 2007;30:259–288. doi: 10.1146/annurev.neuro.28.061604.135722. [DOI] [PubMed] [Google Scholar]
- Semlitsch HV, Anderer P, Schuster P, Presslich O. A solution for reliable and valid reduction of ocular artifacts, applied to the P300 ERP. Psychophysiology. 1986;23(6):695–703. doi: 10.1111/j.1469-8986.1986.tb00696.x. [DOI] [PubMed] [Google Scholar]
- Swedo SE, Rapoport JL, Leonard H, Lenane M, Cheslow D. Obsessive-compulsive disorder in children and adolescents. Clinical phenomenology of 70 consecutive cases. Archives of General Psychiatry. 1989;46(4):335–341. doi: 10.1001/archpsyc.1989.01810040041007. [DOI] [PubMed] [Google Scholar]
- Trujillo LT, Allen JJ. Theta EEG dynamics of the error-related negativity. Clinical Neurophysiology. 2007;118(3):645–668. doi: 10.1016/j.clinph.2006.11.009. [DOI] [PubMed] [Google Scholar]
- Tucker DM, Luu P, Frishkoff G, Quiring J, Poulsen C. Frontolimbic response to negative feedback in clinical depression. Journal of abnormal psychology. 2003;112(4):667–678. doi: 10.1037/0021-843X.112.4.667. [DOI] [PubMed] [Google Scholar]
- Ullsperger M, von Cramon DY. Subprocesses of performance monitoring: A dissociation of error processing and response competition revealed by event-related fMRI and ERPs. Neuroimage. 2001;14(6):1387–1401. doi: 10.1006/nimg.2001.0935. [DOI] [PubMed] [Google Scholar]
- Ullsperger M, von Cramon DY. Error monitoring using external feedback: Specific roles of the habenular complex, the reward system, and the cingulate motor area revealed by functional magnetic resonance imaging. Journal of Neuroscience. 2003;23(10):4308–4314. doi: 10.1523/JNEUROSCI.23-10-04308.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullsperger M, von Cramon DY. Neuroimaging of performance monitoring: Error detection and beyond. Cortex. 2004;40(45):593–604. doi: 10.1016/s0010-9452(08)70155-2. Print Electronic; Print. [DOI] [PubMed] [Google Scholar]
- Ullsperger M. Performance monitoring in neurological and psychiatric patients. International Journal of Psychophysiology. 2006;59(1):59–69. doi: 10.1016/j.ijpsycho.2005.06.010. [DOI] [PubMed] [Google Scholar]
- Ullsperger M, von Cramon DY. How does error correction differ from error signaling? An event-related potential study. Brain Research. 2006;1105(1):102–109. doi: 10.1016/j.brainres.2006.01.007. [DOI] [PubMed] [Google Scholar]
- Ursu S, Stenger VA, Shear MK, Jones MR, Carter CS. Overactive action monitoring in obsessive-compulsive disorder: evidence from functional magnetic resonance imaging. Psychological Science. 2003;14(4):347–353. doi: 10.1111/1467-9280.24411. [DOI] [PubMed] [Google Scholar]
- Valerius G, Lumpp A, Kuelz AK, Freyer T, Voderholzer U. Reversal learning as a neuropsychological indicator for the neuropathology of obsessive compulsive disorder? A behavioral study. Journal of Neuropsychiatry and Clinical Neuroscience. 2008;20:210–218. doi: 10.1176/jnp.2008.20.2.210. [DOI] [PubMed] [Google Scholar]
- Van Boxtel GJM. The use of the substraction technique in the psychophysiology of response inhibition and conflict. In: Ullsperger M, Falkenstein M, editors. Errors, Conflicts, and the Brain Current Opinions on Performance Monitoring. Leipzig: MPI of Cognitiv Neuroscience; 2004. pp. 219–225. [Google Scholar]
- van den Heuvel OA, Veltman DJ, Groenewegen HJ, Cath DC, van Balkom AJ, van Hartskamp J, Barkhof F, van Dyck R. Frontal-striatal dysfunction during planning in obsessive-compulsive disorder. Archives of General Psychiatry. 2005;62(3):301–309. doi: 10.1001/archpsyc.62.3.301. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Bland RC, Canino GJ, Greenwald S, Hwu HG, Lee CK, Newman SC, Oakley-Browne MA, Rubio-Stipec M, Wickramaratne PJ. The cross national epidemiology of obsessive compulsive disorder. The Cross National Collaborative Group. Journal of Clinical Psychiatry. 1994;55(Suppl):5–10. [PubMed] [Google Scholar]
- Yeung N, Cohen JD, Botvinick MM. The neural basis of error detection: conflict monitoring and the error-related negativity. Psychological Review. 2004;111(4):931–959. doi: 10.1037/0033-295x.111.4.939. [DOI] [PubMed] [Google Scholar]