Abstract
OBJECTIVE
Several second-generation antipsychotic (SGA) drugs have been associated with weight gain, hyperglycemia, and dyslipidemia. We evaluated whether glucose and lipid testing increased after the American Diabetes Association (ADA) consensus statement recommending metabolic monitoring for SGA-treated patients.
RESEARCH DESIGN AND METHODS
Laboratory claims for serum glucose and lipid testing were identified for an incident cohort of 18,876 adults initiating SGA drugs in a U.S. commercial health plan (2001–2006) and a control group of 56,522 adults with diabetes not receiving antipsychotics. Interrupted time-series models were used to estimate the effect of ADA recommendations on baseline and annual testing trends after adjusting for differences in age, sex, mental health diagnoses, and cardiovascular risk using propensity score matching.
RESULTS
Mean baseline testing rates for SGA-treated patients during the study period were 23% (glucose) and 8% (lipids). Among persistent users of SGA medication, annual testing rates were 38% (glucose) and 23% (lipid). Before the ADA statement, screening rates for SGA-treated patients were increasing (glucose: baseline 3.6% per year, annual 7.2% per year; lipid: baseline 1.2% per year, annual 4.8% per year; P < 0.001 for each trend). Increases were similar to background testing trends in control subjects. The ADA statement was not associated with an increase in screening rates.
CONCLUSIONS
In a commercially insured population, glucose and lipid testing for SGA-treated adults was infrequent. A gradual increase in screening rates occurred over the 6-year period, but the changes were not temporally associated with the ADA statement. More effort is needed to improve diabetes and dyslipidemia screening in these at-risk patients.
Adults with serious mental illness, commonly treated with second-generation antipsychotic (SGA) drugs, have up to two-times-greater prevalence of type 2 diabetes, dyslipidemia, hypertension, and obesity (1,2). Cardiovascular disease is the leading contributor to mortality for adults with serious mental illness (3–5), resulting in a decades less life expectancy than the general population (4). Increased risk for premature cardiovascular mortality has been attributed to lower socioeconomic status (6), physical inactivity and poor dietary choices (7), obesity (8), greater smoking and substance abuse (7), adverse medication effects (1), and underutilization of primary and secondary prevention (5). Unfortunately, diabetes and cardiovascular risk is often underrecognized (2) and undertreated (9) in patients with mental illness.
SGA medication is a leading therapeutic class based on U.S. dollar sales (Verispan; Vona). While SGA drugs were initially approved for treatment of schizophrenia, some are also approved for bipolar disorder and more recently for use in children. These agents are also used in clinical practice for treatment of other unapproved conditions, such as insomnia and anxiety. Following concerns about medication-related metabolic risks (10,11), the Food and Drug Administration (FDA) mandated class warningsdescribing increased risk for severe hyperglycemia and diabetes and required all drug manufacturers to mail “Dear Doctor” letters about the warning (12). The goal was to increase awareness of the signs and symptoms of diabetes and promote earlier detection and treatment. In February 2004, the American Diabetes Association (ADA) published a consensus statement on antipsychotic drugs and obesity and diabetes with the American Psychiatric Association, the American Association of Clinical Endocrinologists, and the North American Association for the Study of Obesity (13). The consensus statement described the metabolic risks associated with SGA drugs and recommended baseline and ongoing assessment of fasting serum glucose and lipid profiles in all patients receiving these agents.
Metabolic screening in SGA-treated patients is understudied. A recent report (14) using Medicaid data indicated that glucose and lipid testing were significantly underutilized in patients starting SGA drug therapy before the consensus statement. In the present study, we estimated 6-year trends in outpatient serum glucose and lipid testing rates using laboratory claims for individuals starting SGA drug therapy in a large, commercially insured population. We evaluated whether baseline and annual glucose and lipid testing increased after the FDA warnings and ADA consensus statement relative to background-testing trends.
RESEARCH DESIGN AND METHODS
Administrative claims data from four commercial health insurance plans in the U.S., representing ∼9 million eligible members, were analyzed. This study did not involve patient intervention or use protected health information and was therefore exempt from institutional review board review. A cohort of 18,876 adults initiating one of six widely used SGA drugs (aripiprazole, olanzapine, quetiapine, risperidone, or ziprasidone) during January 2001 through December 2006 was identified from pharmacy claims. A second control cohort of 56,522 adults with diabetes not receiving SGA medication was identified by the presence of a diabetes diagnosis in the medical claims or a prescription claim for an antihyperglycemic medication. The purpose of the control cohort was to compare glucose and lipid testing rates in SGA users with background trends for the same commercial plans and time period in a group of patients indicated for metabolic monitoring. We hypothesized that glucose and lipid testing rates in adults with diabetes would not be affected by the antipsychotic warnings and ADA consensus statement and could therefore provide a control for other temporal trends on testing rates within these commercial plans. The index date for both cohorts was the date of the first qualifying prescription or medical claim. Patients had continuous eligibility for 1 year before through 1 month after the index date for baseline testing outcomes or through 1 year after the index date for annual testing outcomes.
Assessment of glucose and lipid testing
Glucose testing was identified if a medical claim with an American Medical Association Current Procedural Terminology (CPT) code for a metabolic or general health panel (80048, 80050, and 80053) or glucose-specific serum test (82947, 82948, 82950, and 82951) was present. Lipid testing was identified if a CPT code for a lipid panel (80061) or lipid-specific serum test (82465, 84478, 83721, 83715, 83700, 83716, and 83701) was present. Baseline was operationalized as testing occurring 30 days before through 30 days after the index date. Annual monitoring was operationalized as testing occurring 31–365 days after the index date. We recognize that glucose testing rates in patients with diabetes will tend to underestimate absolute rates of glycemic monitoring, which routinely include the use of glycated hemoglobin and home testing with portable glucometers. For this reason, we only compare temporal trends in serum testing rates.
Patient characteristics
Disparities in diabetes care have been associated with mental disorders (9). Mental health disorders were identified using ICD-9 diagnosis codes ascertained from medical claims in the 12 months before the index date and classified into eight categories using Clinical Classifications Software (CCS) coding developed by the Agency for Health Care Research and Quality (15) (affective disorders, alcohol and substance abuse, anxiety and personality disorders, preadult disorders, senility, schizophrenia, other psychoses, and other mental conditions).
Dyslipidemia, hypertension, and heart disease are risk factors for type 2 diabetes and should trigger more frequent screening. To adjust for differences in cardiovascular risk between SGA users and diabetic control subjects, individuals with preexisting dyslipidemia, hypertension, and heart disease were identified using medical and pharmacy claims for 365 days before the index date. Dyslipidemia was defined as a dyslipidemia diagnosis or prescription for a cholesterol-lowering drug. Hypertension was defined as a hypertension diagnosis or prescription for an antihypertensive drug. Heart disease was defined as a diagnosis for acute myocardial infarction, coronary atherosclerosis, pulmonary heart disease, or other heart diseases using CCS classification. Age (at the index date) and sex are also associated with the likelihood of diabetes screening and were analyzed. Race/ethnicity was unavailable for analysis.
Analytic strategy
A quasiexperimental design was used to evaluate quarterly trends in baseline and annual glucose testing rates for patients initiating SGA drug therapy before versus after publication of the ADA consensus statement (first quarter 2004) using segmented time-series regression corrected for first-order autocorrelation (16). To control for differences in baseline patient characteristics when comparing temporal trends between SGA users and diabetic control subjects, a nearest neighbor 1:1 matched cohort of case and control subjects was created for each quarter using propensity score matching on patient age, sex, number of mental health disorders, and presence of preexisting cardiovascular risk (dyslipidemia, hypertension, or heart disease) (17). This resulted in a propensity-matched cohort of SGA-treated patients and control subjects (n = 8,759 pairs). The analysis of annual testing rates was performed in persistent users of SGA medication, who theoretically would be at greater risk for developing long-term metabolic side effects than patients receiving time-limited therapy. Persistent SGA users had a maximum gap in therapy ≤30 days during the initial 365 days of therapy (18). Using the same propensity-matching methods, a cohort of persistent SGA-treated patients and matched control subjects was identified (n = 2,218 pairs). Frequency of metabolic testing among SGA users starting therapy in 2005, the most recent year after the ADA statement with sufficient follow-up to report both baseline and annual rates, was compared in patients with versus without preexisting diabetes using χ2 tests. All analyses used STATA version 10 (Stata, College Station, TX).
RESULTS
Table 1 summarizes patient characteristics for adults starting SGA therapy and for diabetic control subjects who did not receive antipsychotic medication. Users of SGA medication were younger than the average adult with diabetes and more likely to have a recorded mental health diagnosis, (80.7 vs. 26.5%, P < 0.0001) but were less likely to have identified dyslipidemia, hypertension, or heart disease (51.0 vs. 69.0%, P < 0.0001). Distribution of SGA drugs before versus after the consensus statement was significantly different (P < 0.001) (aripiprazole: 2 vs. 11%; olanzapine: 48 vs. 25%; quetiapine: 21 vs. 40%; risperidone: 26 vs. 21%; and ziprasidone: 3 vs. 4%).
Table 1.
Baseline patient characteristics in all patients
| SGA cohort | Diabetes control cohort | P | |
|---|---|---|---|
| Demographics | |||
| n | 18,176 | 56,522 | |
| Female (%) | 59.3 | 46.6 | <0.0001 |
| Age-groups (years) (%) | |||
| 20–29 | 13.2 | 4.7 | |
| 30–39 | 19.0 | 13.8 | |
| 40–49 | 25.2 | 24.4 | <0.0001 |
| 50–59 | 20.1 | 32.1 | |
| 60–69 | 8.1 | 17.4 | |
| 70–79 | 6.4 | 5.7 | |
| 80–88 | 7.7 | 1.6 | |
| Mental health diagnoses (past 12 months) | |||
| Any of the following (%) | 80.7 | 26.5 | <0.001 |
| Affective disorders | 49.3 | 2.5 | <0.0001 |
| Anxiety disorders | 29.2 | 2.9 | <0.0001 |
| Alcohol and substance abuse | 15.0 | 2.0 | <0.0001 |
| Senility | 10.4 | 0.4 | <0.0001 |
| Other psychoses | 9.4 | 0.1 | <0.0001 |
| Preadult disorders | 4.1 | 0.1 | <0.0001 |
| Schizophrenia | 3.4 | <0.1 | <0.0001 |
| Other mental conditions | 51.4 | 23.0 | <0.0001 |
| Cardiovascular risk (past 12 months) (%) | |||
| Any of the following | 51.0 | 69.0 | <0.0001 |
| Hypertension | 39.9 | 55.1 | <0.0001 |
| Dyslipidemia | 26.8 | 45.7 | <0.0001 |
| Heart disease | 4.7 | 3.6 | 0.02 |
Data are percentages. χ2 tests were conducted to test for differences in patient characteristics between SGA users and adults with diabetes not receiving antipsychotic medication.
Mean baseline testing rates for SGA-treated patients during the study period were 23% (glucose) and 8% (lipids). Trends in baseline testing for all SGA-treated patients are presented in Fig. 1. Baseline testing rates were increasing for glucose (0.9% per quarter) and lipid testing (0.4% per quarter) before the consensus statement. There was not a significant increase, or “step change,” in baseline glucose testing during the quarter in which the consensus statement was published (P = 0.80). The positive growth observed in baseline glucose testing rates before the consensus statement was attenuated after the statement, as evidenced by a negative change in the slope, or “trend change,” of −0.8% per quarter (P < 0.01). For baseline lipid testing, there was a small positive step change during the quarter the consensus statement was published (1.5%, P = 02); however, the positive growth in baseline lipid testing was also attenuated after the statement as evidenced by a negative trend change after the statement (−0.5% per quarter, P < 0.001).
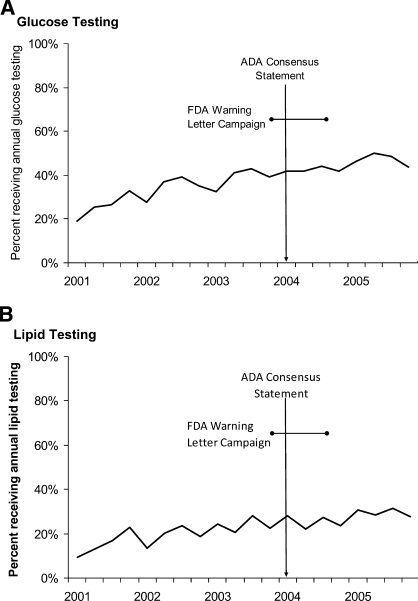
Figure 1.
Trends in baseline serum glucose (A) and lipids (B) laboratory testing in SGA-treated adults. n = 18,876 adults initiating SGA drug therapy.
Baseline testing trends for SGA-treated patients were similar to background testing trends in matched subjects with diabetes. Before the consensus statement, baseline glucose testing was increasing at similar rates in SGA patients (0.8% per quarter [95% CI 0.4–1.3]) similar to those in matched patients with diabetes (1.2% per quarter [0.6–1.8]) before. Baseline lipid testing rates were also increasing before the statement, although at a slightly slower rate for SGA patients (0.5% per quarter [0.4–0.7]) compared with patients with diabetes (1.1% per quarter [0.8 – 1.4]). After the statement, baseline testing trends were no different between SGA-treated patients and matched adults with diabetes (glucose, P = 0.68; lipids, P = 0.35), as measured by trends in the ratio of testing rates.
Among persistent users of SGA medication, mean annual testing rates during the study period were 38% (glucose) and 23% (lipids). Trends in annual metabolic testing for SGA-treated patients are presented in Fig. 2. Rates of annual glucose testing were increasing before the consensus statement (1.8% per quarter). There was no step change or increase in testing rates during the quarter the statement was published (P = 0.68), and testing trends did not change as a result of the statement (P = 0.32). Annual lipid testing rates were also increasing before the consensus statement at a rate of 1.2% per quarter. As with annual glucose testing, there was no step change in annual lipid testing rates (P = 0.32), and lipid testing trends did not change as a result of the statement (P = 0.64).
Figure 2.
Trends in annual serum glucose and lipids laboratory testing in persistent users of SGA drug therapy. n = 3,140 adults initiating SGA drug therapy who were therapy persistent for 1 year.
Annual testing trends among SGA patients were consistent with background testing trends in matched subjects with diabetes. Before the statement, annual glucose testing was increasing at similar rates for both SGA patients (1.8% per quarter [95% CI 1.3–2.2]) and patients with diabetes (1.2% per quarter [1.0–1.5]). Prestatement trends were also similar for annual lipid testing in SGA patients (1.2% per quarter [0.8–1.5]), compared with patients with diabetes (1.1% per quarter [0.9–1.3]). After the statement, annual testing trends were no different between SGA-treated patients and adults with diabetes (glucose, P = 0.92; lipids, P = 0.26) as measured by trends in the ratio of testing rates.
Table 2 summarizes the frequency of baseline and annual serum glucose and lipid testing among adults initiating SGA drug therapy in 2005. Baseline glucose testing occurred in 25% of SGA-utilizing patients and baseline lipid testing occurred in 9% of patients. Approximately 10% of patients had identified diabetes. Overall, baseline testing was higher if preexisting diabetes was identified (glucose: 36 vs. 24%, P < 0.001; lipids: 16 vs. 8%, P < 0.001). Among SGA patients with therapy persistent for 1 year, annual glucose testing occurred in 49% of patients and annual lipid testing in 31% of patients. Annual rates of testing among persistent SGA users were not significantly different between adults with and without identified diabetes. Baseline and annual testing rates were not significantly different in men versus women (data not shown).
Table 2.
Frequency of glucose and lipid testing among patients initiating SGA drug therapy in 2005
| Metabolic laboratory assessment | All patients | Frequency of testing among adults initiating SGA drug therapy |
||
|---|---|---|---|---|
| Preexisting diabetes | ||||
| Yes | No | P | ||
| Serum glucose | ||||
| All patients initiating therapy (n) | 3,351 | 324 | 3,027 | |
| Baseline test (%) | 25 | 36 | 24 | <0.001 |
| 1-year persistent users (n) | 623 | 63 | 560 | |
| Baseline test (%) | 28 | 38 | 27 | 0.07 |
| Annual test (%) | 49 | 55 | 48 | 0.32 |
| Serum lipids | ||||
| All patients initiating therapy (n} | 3,351 | 324 | 3,027 | |
| Baseline test (%) | 9 | 16 | 8 | <0.001 |
| 1-year persistent users (n) | 623 | 63 | 560 | |
| Baseline test (%) | 10 | 19 | 9 | 0.02 |
| Annual test (%) | 31 | 31 | 31 | 0.97 |
χ2 tests were conducted to test for the association between testing rates and baseline diabetes status in all patients initiating SGA and persistent users.
CONCLUSIONS
This population-based study examined the impact of the ADA consensus statement on baseline and annual testing of serum glucose and lipids for SGA-treated adults within a commercially insured population. We found that baseline and annual glucose and lipid testing rates for SGA-treated patients increased between 2001 and 2006. However, the rising trends in testing appear to be attributable to increases observed in background testing trends rather than a specific response to the ADA consensus recommendations. Importantly, metabolic testing remained suboptimal for SGA users. By the end of 2005, 75% of SGA users received no baseline glucose testing and 90% received no baseline lipids assessment. Annual rates of testing were more favorable; nonetheless, half of the SGA-treated adults received no glucose testing and two-thirds no lipid testing in the year following drug initiation.
This study identified metabolic testing based on laboratory claims from multiple outpatient settings within the commercial health plan. However, it was not possible to confirm whether tests were ordered by, or were available to, clinicians responsible for SGA treatment decision making. It is almost certain that some proportion of testing was performed for purposes other than the recommended evaluation of SGA effects on glucose or lipid levels. Therefore, the absolute rates of glucose and lipid testing we observed for SGA-treated patients are likely overestimates of actual metabolic monitoring related to SGA treatment.
Although this retrospective study was not able to look into the reasons why laboratory screening did not increase after the ADA consensus statement, we might speculate on some possible explanations. On one hand, the results are not surprising because typically half of physicians follow any given clinical guideline (19). Adoption of other monitoring recommendations following drug warnings has also been poor (20). Many causes of low adherence to evidence-based treatment recommendations have been studied, including low awareness, lack of medical consensus, low self-efficacy to enact change, and failure to overcome the inertia of previous practice (21). Another explanation offered is that physicians treat guidelines more as options as opposed to true standards and professional organizations, such as the ADA and American Psychiatric Association, cannot enforce adherence (19).
On the other hand, the low rates of serum testing observed in this study population are surprising given high awareness among psychiatrists of the metabolic risks associated with SGA medication and strong agreement on the need to screen and monitor patients (22,23). After the consensus statement, 60–80% of psychiatrists reported monitoring glucose and lipid levels at regular intervals (22,23). It could be that surveyed psychiatrists were not representative of all SGA prescribers. Alternatively, poor patient follow-through between the physician ordering the lab and the patient getting blood drawn may be occurring. More research is needed to determine why the gap exists between reported monitoring behavior and observed serum testing before improvements can be made in diabetes and dyslipidemia screening and ongoing monitoring for these at-risk patients.
The ADA consensus statement (13) and subsequent published research (1) have acknowledged that not all antipsychotics have the same metabolic riskprofile; for example, olanzapine, in particular, has been cited as having a high risk for weight gain, metabolic disturbances, and dyslipidemia (1,13). As an alternative to greater vigilance in metabolic monitoring, some physicians may have started avoiding drugs with greater metabolic risk. The finding that olanzapine's share of new starts dropped from 48 to 25% after the statement is consistent with this hypothesis. Nevertheless, the FDA class warnings (14) and the ADA consensus statement (15) call for metabolic monitoring in all patients regardless of which SGA medication they are receiving.
The results of this research are subject to limitations. Because we relied on administrative claims records, we could not evaluate the impact of the consensus statement on unbilled metabolic screening (e.g., family history of diabetes, height and body weight, or waist circumference) or testing occurring during a hospital admission. Caution should also be applied in generalizing findings to all patients initiating antipsychotic medications, for example Medicaid clients. In addition, anecdotal reports suggest some local mental health treatment centers have been successful in increasing rates of glucose and lipid testing using incentives (e.g., financial compensation to the ordering clinician) or disincentives (e.g., sharing individual clinician performance rates among a peer group).
In summary, despite psychiatrist awareness of metabolic risk and high rates of self-reported screening, we found little evidence that patients starting SGA medication typically receive serum glucose and lipid testing. Although a gradual increase in screening rates occurred over the 6-year period, publication of the ADA consensus statement on SGA drugs and diabetes risk was not associated with an increase in aboratory testing rates. Results from this study of commercially insured patients suggest a considerable gap remains between clinical practice and ADA recommendations for routine metabolic monitoring in a population at increased risk for diabetes and cardiovascular disease. More effort is needed to ensure that patients receiving SGA drugs are screened for diabetes and dyslipidemia.
Acknowledgments
This study was supported by Pfizer. E.H.M. is an employee of the University of Colorado Denver and was contracted by Pfizer for this research study. The contract supported E.M.'s time and effort to design and guide the analysis plan, to interpret the data, and to take primary responsibility for the development of the manuscript. J.W.N. is an employee of Washington University in St. Louis and was an unpaid advisor to the research team assisting in the development of the analytic plan, interpretation of the data, and review of the manuscript. S.K. is an employee of Healthcore and was a paid consultant to Pfizer in connection with the development of the manuscript. O.B. is an employee of STATinMED and received support from Pfizer in connection with the conduct of the study and development of this manuscript. J.H. and B.C. are employees of Pfizer. No other potential conflicts of interest relevant to this article were reported.
Parts of this study were presented in abstract form at the 68th Scientific Sessions of the American Diabetes Association, San Francisco, California, 6–10 June 2008; the 161st annual meeting of the American Psychiatric Association, Washington, DC, 3–8 May 2008; and the 24th International Conference on Pharmacoepidemiology and Therapeutic Risk Management, Copenhagen, Denmark, 17–20 August 2008.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1.Newcomer JW: Second-generation (atypical) antipsychotics and metabolic effects: a comprehensive literature review. CNS Drugs 2005; 19: 1– 93 [DOI] [PubMed] [Google Scholar]
- 2.McEvoy JP, Meyer JM, Goff DC, Nasrallah HA, Davis SM, Sullivan L, Meltzer HY, Hsiao J, Scott Stroup T, Lieberman JA: Prevalence of the metabolic syn-drome in patients with schizophrenia: baseline results from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia trial and com-parison with national estimates from NHANES III. Schiz Res 2005; 80: 19– 32 [DOI] [PubMed] [Google Scholar]
- 3.Goff DC, Sullivan LM, McEvoy JP, Meyer JM, Nasrallah HA, Daumit GL, Stroup TS, Davis S, Lieberman JA: A comparison of ten-year cardiac risk estimates in schizophrenia patients from the CATIE study and matched controls. Schizophrenia Res 2005; 80: 45– 53 [DOI] [PubMed] [Google Scholar]
- 4.Colton C, Manderscheid R: Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. In Prev Chronic Dis 2006 [serial online]. Available from http://www.cdc.gov/pcd/issues/2006/apr/05_0180.htm Accessed 25 June 2008 [PMC free article] [PubMed]
- 5.Newcomer JW, Hennekens CH: Severe mental illness and risk of cardiovascular disease. JAMA 2007; 298: 1794– 1796 [DOI] [PubMed] [Google Scholar]
- 6.Druss BG, Bradford WD, Rosenheck R, Radford MJ, Krumholz HM: Quality of medical care and excess mortality in older patients with mental disorders. Arch Gen Psychiatry 2001; 58: 565– 572 [DOI] [PubMed] [Google Scholar]
- 7.Goff DC CC, Evins AE, Henderson DC, Freudenreich O, Copeland PM, Bierer M, Duckworth K, Sacks FM: Medical morbidity and mortality in schizophrenia: guidelines for psychiatrists. J Clin Psychiatry 2005; 66: 183– 194 [DOI] [PubMed] [Google Scholar]
- 8.Allison DB, Fontaine KR, Heo M, Mentore JL, Cappelleri JC, Chandler LP, Weiden PJ, Cheskin LJ: The distribution of body mass index among individuals with and without schizophrenia. J Clin Psychiatry 1999; 60: 215– 220 [DOI] [PubMed] [Google Scholar]
- 9.Frayne SM, Halanych JH, Miller DR, Wang F, Lin H, Pogach L, Sharkansky EJ, Keane TM, Skinner KM, Rosen CS, Berlowitz DR: Disparities in diabetes care: impact of mental illness. Arch Intern Med 2005; 165: 2631– 2638 [DOI] [PubMed] [Google Scholar]
- 10.Haupt DW, Newcomer JW: Hyperglycemia and antipsychotic medications. J Clin Psychiatry 2001; 62: 15– 26 [PubMed] [Google Scholar]
- 11.Lean M, Pajonk F: Patients on atypical antipsychotic drugs: another high-risk group for type 2 diabetes. Diabetes Care 2003; 26: 1597– 1605 [DOI] [PubMed] [Google Scholar]
- 12.U.S. Food and Drug Administration Warning about hyperglycemia and atypical antipsychotic drugs. FDA Safety News, 2004 [article online]. Available from http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/psn/transcript.cfm?show=28#4 Accessed 14 April 2008
- 13.American Diabetes Association, American Psychiatric Association, American Association of Clinical Endocrinologists, North American Association for the Study of Obesity Consensus development conference on antipsychotic drugs and obesity and diabetes. Diabetes Care 2004; 27: 596– 601 [DOI] [PubMed] [Google Scholar]
- 14.Morrato E, Newcomer J, Allen R, Valuck R: Prevalence of baseline serum glucose and lipid testing in users of second-generation antipsychotic drugs: a retrospective, population-based study of Medicaid claims data. J Clin Psychiatry 2008; 69: 316– 322 [DOI] [PubMed] [Google Scholar]
- 15.Agency for Healthcare Research and Quality HCUP clinical classifications software (CCS) for ICD-9-CM fact sheet [article online], 2007. Available from http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccsfactsheet.jsp
- 16.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D: Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther 2002; 27: 299– 309 [DOI] [PubMed] [Google Scholar]
- 17.Baser O: Too much ado about propensity score models? Comparing methods of propensity score matching. Value Health 2006; 9: 377– 385 [DOI] [PubMed] [Google Scholar]
- 18.Sikka R, Zia F, Aubert R: Estimating medication persistency using administrative claims data. Am J Manag Care 2005; 11: 449– 457 [PubMed] [Google Scholar]
- 19.Timmermans S, Mauck A: The promises and pitfalls of evidence-based medicine. Health Aff (Millwood) 2005; 24: 18– 28 [DOI] [PubMed] [Google Scholar]
- 20.Morrato EH, Libby AM, Orton HD, deGruy FV, Brent DA, Allen RR, Valuck RJ: Frequency of provider contact after FDA advisory on risk of pediatric suicidality with SSRIs. Am J Psychiatry 2008; 165: 42– 50 [DOI] [PubMed] [Google Scholar]
- 21.Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, Rubin HR: Why don't physicians follow clinical practice guidelines? A framework for improvement JAMA 1999; 282: 1458– 1465 [DOI] [PubMed] [Google Scholar]
- 22.Ketter TA, Haupt DW: Perceptions of weight gain and bipolar pharmacotherapy: results of a 2005 survey of physicians in clinical practice. Curr Med Res Opin 2006; 22: 2345– 2353 [DOI] [PubMed] [Google Scholar]
- 23.Suppes T, McElvoy S, Hirschfeld R: Awareness of metabolic concerns and perceived impact of pharmacotherapy in patients with bipolar disorder: a survey of 500 U.S. psychiatrists. Psychopharmacol Bull 2007; 40: 22– 37 [PubMed] [Google Scholar]