Abstract
OBJECTIVE
A low–glycemic index diet is effective as a treatment for individuals with diabetes and has been shown to improve pregnancy outcomes when used from the first trimester. A low–glycemic index diet is commonly advised as treatment for women with gestational diabetes mellitus (GDM). However, the efficacy of this advice and associated pregnancy outcomes have not been systematically examined. The purpose of this study was to determine whether prescribing a low–glycemic index diet for women with GDM could reduce the number of women requiring insulin without compromise of pregnancy outcomes.
RESEARCH DESIGN AND METHODS
All women with GDM seen over a 12-month period were considered for inclusion in the study. Women (n = 63) were randomly assigned to receive either a low–glycemic index diet or a conventional high-fiber (and higher glycemic index) diet.
RESULTS
Of the 31 women randomly assigned to a low–glycemic index diet, 9 (29%) required insulin. Of the women randomly assigned to a higher–glycemic index diet, a significantly higher proportion, 19 of 32 (59%), met the criteria to commence insulin treatment (P = 0.023). However, 9 of these 19 women were able to avoid insulin use by changing to a low–glycemic index diet. Key obstetric and fetal outcomes were not significantly different.
CONCLUSIONS
Using a low–glycemic index diet for women with GDM effectively halved the number needing to use insulin, with no compromise of obstetric or fetal outcomes.
Gestational diabetes mellitus (GDM) is defined as any degree of glucose intolerance with onset or first recognition during pregnancy (1). GDM is associated with an increase in adverse pregnancy outcomes, and the advantages of treatment on these outcomes have been identified (2). All women with GDM should have medical nutrition therapy (MNT) with the objective of achieving and maintaining blood glucose levels as close to the normal range as possible (3). MNT needs to be individualized and should be based on carbohydrate (CHO) distribution and ideally on the results of self-monitoring of blood glucose (SMBG). For the purposes of SMBG, a combination of the fasting and postprandial glucose levels is desirable.
When MNT alone is unable to keep the results of SMBG within predetermined target ranges, alternative therapies are required. Although there is some evidence that both glyburide (4) and metformin (5) can be used, the overwhelming experience has been with insulin. However, the potential use of insulin can be a source of both anxiety and of resistance to treatment change.
In normal subjects, mixed meals based on low–glycemic index foods lead to a reduction in postprandial glycemia (6). We have previously demonstrated in normal pregnant women that a diet based on low–glycemic index foods was sustainable and resulted in more favorable fetal outcomes (7). The aim of this study was to examine whether a low–glycemic index diet used as MNT for women with GDM could result in a reduced need for insulin use during pregnancy with no compromise of obstetric and fetal outcomes.
RESEARCH DESIGN AND METHODS
The study was conducted in the city of Wollongong, New South Wales, Australia, a coastal city with a population of ∼280,000 people situated about 50 miles south of Sydney. The Australasian Diabetes in Pregnancy Society (ADIPS) recommends that all pregnant women should be tested for GDM (8). Unless indicated earlier, women have a 75-g glucose tolerance test at the beginning of the third trimester with glucose samples taken after fasting and at 2 h. GDM is diagnosed if the fasting glucose is ≥5.5 mmol/l (∼100 mg/dl) and/or the 2-h glucose is ≥8.0 mmol/l (∼145 mg/dl) (9). Virtually all women with GDM are seen at the Diabetes Center by a diabetes nurse educator and a specialist dietitian. All women seen over a 12-month period (October 2007–September 2008) were considered. There are ∼3,300 deliveries each year in the area, including those in both the public and private hospitals. The prevalence of GDM is ∼7%, and there is >90% compliance with universal testing (10).
Inclusion criteria were age 18–40 years (inclusive), singleton pregnancy, no previous GDM, nonsmoker, diagnosis of GDM and seen for the first dietary visit between 28 and 32 weeks of gestation, and ability to follow the protocol requirements. Exclusion criteria included any condition or medication that could affect glucose levels and unwillingness to follow the prescribed diet.
After diagnosis of GDM and assessment by a physician (R.G.M.), all women attended the Diabetes Center. If they were potentially interested in the study, they were asked to complete a 3-day food record before the first visit with the dietitian. This record was used for the initial dietary assessment. The visit was completed between 28 and 32 weeks of gestation. Visits 2 and 3 were conducted ∼1–2 and ∼3–4 weeks, respectively, after the initial visit and included a 7-day food record that was used to calculate glycemic index. The final visit was at 35–37 weeks of gestation with a 3-day food record that was used to compare with the food record at visit 1. Thus, all women were seen at least four times for dietary assessment and if they required insulin were seen as many times as necessary for insulin adjustment.
Weight was measured to the nearest 0.1 kg on floor scales (HD-316, Wedderburn Scales; Tanita Corporation, Tokyo, Japan) with subjects dressed in light clothes and without shoes. Height was measured to the nearest 0.1 cm against a wall using a nonstretchable fiberglass measuring tape (Gulick II; Country Technology, Gays Mils, WI).
Women who met the inclusion criteria and had no exclusions were randomly assigned to receive one of two different diets using permuted blocks of unequal size with the list generated using STATA (version 7.0). Both diets were compatible with the recommended nutritional intake in pregnancy (9). The CHO intake was designed to achieve a minimum of 175 g/day with only the recommended choice of CHO foods varying. The dietary advice was individualized with specific mention of the energy and nutrient balance to achieve normal weight gain during the third trimester. The low–glycemic index diet was based on previously verified low–glycemic index food (11), including pasta, grain breads, and unprocessed breakfast cereals with a high fiber content. Women were specifically asked to avoid consuming white bread, processed commercial breakfast cereals, potatoes, and some rice varieties. Women in the conventional, higher–glycemic index diet group were advised to follow a diet with a high-fiber and low-sugar content, with no specific mention of the glycemic index. Potatoes, whole wheat bread, and specific high-fiber, moderate-to-high–glycemic index breakfast cereals were recommended. During clinic visits, the dietitian referred to the diets as the “low–glycemic index diet” or the “high-fiber/low-sugar” diet. Participants were provided with a booklet outlining the CHO choices as well as the CHO food amounts constituting one serving (based on 15-g portions). To assist with achieving stable blood glucose levels throughout the day, participants were advised to consume three small meals and two to three snacks with a specified number of servings of CHOs. Study dietitians were not blinded to dietary assignment but were aware of the need for impartiality and equivalent treatment. The physician caring for the patients was not informed of the diet allocation.
Women were provided with a home glucose meter (Accu-Check Performa; Roche) and were asked to test after fasting and 1 h after the start of each of their three major meals at least every second day. The use of insulin, unless there were exceptional circumstances, was advised if more than once a week the fasting glucose was ≥5.5 mmol/l and/or the 1-h postprandial glucose was ≥8.0 mmol/l. For women consuming the low–glycemic index diet who exceeded these values, insulin was started immediately. Women consuming the higher–glycemic index diet who exceeded these values were changed to a low–glycemic index diet, and their responses were reviewed over a week. When indicated, insulin treatment was initiated with twice-daily premixed insulin (NovoMix 30, Novo Nordisk) using a disposable pen device. The dose was adjusted regularly to achieve glycemic goals.
Food intake data for the baseline visit, visit 2, visit 3, and the final visit for each participant were entered into a customized database incorporating the Australian food composition tables and published glycemic index values using the glucose = 100 scale (FoodWorks Professional, version 4 2005; Xyris Software, Highgate Hill, QLD, Australia). When necessary, additional glycemic index data were obtained from an online database (http://www.glycemicindex.com). Overall, the dietary glycemic index was calculated as the sum of the weighted glycemic index of all CHO foods in the diet, with the weighting proportional to the contribution of each food to the total CHO intake. Because the target diets aimed for a similar carbohydrate content, glycemic load (the product of the glycemic index and the amount of CHO) was influenced only by differences in glycemic index.
Pregnancy care was the responsibility of the obstetric health care providers and was conducted in accord with standard practice. Because both diets were within the nutritional guidelines for pregnancy, the obstetric health care providers were not specifically informed of the diet allocation. Obstetric outcomes, including birth weight, fetal length and head circumference, Apgar score, and method of delivery, were obtained from the medical record. For comparison between the two groups, the fetal centile was calculated from http://www.gestation.net using Australian data. By this means the birth weight was adjusted for sex, gestational week of delivery, and maternal age, parity, height, and prepregnancy weight by recall. The ponderal index of the baby was calculated using the following formula: weight in grams divided by the cube of length in centimeters and multiplied by 100. The BMI of the mother was calculated by dividing weight at enrollment in kilograms by the square of height in meters. The Illawarra Area Health Service and University of Wollongong Human Research Committee approved the research, and participants gave written informed consent.
Statistical analysis
Independent samples t tests were used to compare the dietary components and the glycemic index, glycemic load, and CHO values of the low–glycemic index and the high–glycemic index groups at the various appointment times. Pearson χ2 tests of independence were used to compare proportions identified as needing insulin and actually starting on insulin in the low–glycemic index and high–glycemic index groups. SPSS (version 14; SPSS, Chicago, IL) was used for all statistical analyses. Unless otherwise stated, results are expressed as means ± SEM. Results were considered significant if P < 0.05.
RESULTS
This study recruited for a 12-month period starting in October 2007. Over this period 212 women with GDM were seen, of whom 63 met the criteria and agreed to participate in the study; 31 were randomly assigned to receive the low–glycemic index diet, and 32 were randomly assigned to receive the high-fiber/low-sugar diet (henceforth referred to as the high–glycemic index diet). All women except one were Caucasian. There were no significant differences in the baseline characteristics of the two groups as outlined in Table 1.
Table 1.
Baseline characteristics of the women
| Low–glycemic index group | High–glycemic index group | P value* | |
|---|---|---|---|
| n | 31 | 32 | |
| Age (years) | 30.8 ± 0.7 | 31.3 ± 0.8 | 0.68 |
| Weight at enrollment (kg) | 83.1 ± 3.2 | 86.9 ± 3.6 | 0.43 |
| BMI at enrollment (kg/m2) | 32.0 ± 1.2 | 32.8 ± 1.4 | 0.68 |
| Parity | 0.84 ± 0.17 | 0.78 ± 0.18 | 0.82 |
| Oral glucose tolerance test (mmol/l)† | |||
| Fasting glucose | 4.6 ± 0.1 | 4.7 ± 0.1 | 0.49 |
| 2-h glucose | 8.4 ± 0.2 | 8.4 ± 0.1 | 0.83 |
| Gestational age at entry to study (weeks) | 30.3 ± 0.2 | 29.9 ± 0.2 | 0.23 |
Data are means ± SEM.
*Comparison of the low–glycemic index group with the high–glycemic index group, independent samplest test.
†2-h, 75-g glucose load.
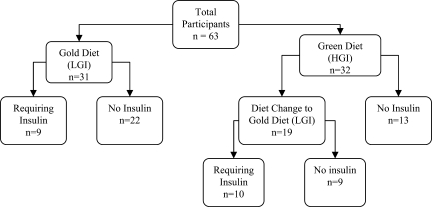
A flowchart of the number of women in each diet group and their insulin requirements is shown in Fig. 1. In summary, the number of women in the low–glycemic index group who met the criteria to start on insulin (9 of 31 [29%]) was significantly lower than 19 of 32 women (59%) as seen in the high–glycemic index diet (P = 0.023). Of the 19 women in the high–glycemic index group who met the criteria to start insulin and were then switched to the low–glycemic index diet,9 no longermet the criteria to start insulin. Thus, after dietary changes, only 10 of 32 (31%) of the women in the high–glycemic index group required insulin, and that number was not significantly different from the 9 of 31 (29%) in the original low–glycemic index group. Insulin was initiated at 32.1 ± 0.4 weeks for women in the low–glycemic index group and at 32.3 ± 0.5 weeks for women in the high–glycemic index group (P = 0.83). Thetotal daily dose of insulin at term was 24 ± 2.2 units.
Figure 1.
Flowchart of the number of women in each diet group and the number requiring insulin. HGI, higher–glycemic index diet; LGI, low–glycemic index diet.
The reported dietary intakes assessed by a 3-day food record at baseline and at the final visit of the study are shown in Table 2. There were no significant differences between the two groups at baseline with respect to energy and most nutrients except for a higher percentage of energy from protein in the women randomly assigned to the high–glycemic index group (P < 0.009). Between the baseline and final visits there was a significant reduction in total energy consumed in both groups due mainly to a reduction in the CHO intake. There were no significant differences in the extent of this reduction between the two groups. The amount of protein consumed as a percentage of energy intake increased significantly for both groups over the course of the study. The percentage of energy intake for monounsaturated fats, polyunsaturated fats, and saturated fats was not significantly different between the groups and did not change during the study (data not shown).
Table 2.
Reported dietary intake assessed by 3-day food record at baseline and the final visit
| Low–glycemic index group | High–glycemic index group, no insulin | High–glycemic index to low–glycemic index group | P value* | P value† | |
|---|---|---|---|---|---|
| n | 31 | 13 (final 12) | 19 (final 18) | ||
| Energy (cal) | |||||
| Baseline visit | 1,994 ± 72 | 1,932 ± 146 | 1,914 ± 88 | 0.50 | 0.91 |
| Final visit | 1,713 ± 66 | 1,664 ± 79 | 1,651 ± 73 | 0.63 | 0.91 |
| Change (P value‡) | −281 ± 79 (0.001) | −251 ± 140 (0.10) | −262 ± 119 (0.042) | ||
| Protein (% energy) | |||||
| Baseline visit | 18.4 ± 0.6 | 20.9 ± 1.3 | 21.7 ± 1.2 | 0.009 | 0.64 |
| Final visit | 23.9 ± 0.7 | 23.5 ± 0.8 | 24.4 ± 0.7 | 0.51 | 0.41 |
| Change (P value‡) | +5.5 ± 0.9 (<0.001) | +2.2 ± 1.1 (0.070) | +2.7 ± 1.2 (0.041) | ||
| Carbohydrate (% energy) | |||||
| Baseline visit | 45.0 ± 1.0 | 42.2 ± 1.1 | 45.1 ± 2.0 | 0.50 | 0.28 |
| Final visit | 36.7 ± 1.1 | 37.8 ± 1.1 | 35.1 ± 1.5 | 0.80 | 0.21 |
| Change (P value†) | −8.3 ± 1.1 (<0.001) | −4.3 ± 1.3 (0.006) | −10.4 ± 2.5 (<0.001) | ||
| Fat (% energy) | |||||
| Baseline visit | 31.7 ± 0.8 | 32.5 ± 1.3 | 31.7 ± 1.7 | 0.81 | 0.74 |
| Final visit | 33.4 ± 1.1 | 34.0 ± 1.2 | 34.5 ± 1.8 | 0.57 | 0.79 |
| Change (P value‡) | +1.7 ± 1.0 (0.11) | +1.6 ± 1.7 (0.36) | +3.0 ± 2.2 (0.19) | ||
| Fiber (g) | |||||
| Baseline visit | 25.4 ± 1.3 | 23.1 ± 1.2 | 24.0 ± 1.5 | 0.30 | 0.66 |
| Final visit | 25.6 ± 1.3 | 22.9 ± 1.1 | 22.3 ± 1.6 | 0.13 | 0.77 |
| Change (P value‡) | +0.3 ± 1.4 (0.86) | +0.3 ± 1.5 (0.84) | −1.9 ± 1.7 (0.28) |
Data are means ± SEM.
*Comparison of low–glycemic index group with high–glycemic index group (high–glycemic index groups combined).
†Comparing those who changed to a low–glycemic index diet with those continuing to consume a high–glycemic index diet.
‡Comparisons from baseline to final visit (§for those with baseline and final visits only).
The glycemic index for all visits is shown in Table 3. The glycemic index at baseline was similar in both groups. The women randomly assigned to the low–glycemic index diet achieved and maintained a significantly lower glycemic index at all stages. The women randomly assigned to the high–glycemic index diet, who did not meet the criteria to start insulin and, hence, had no diet changes, had no significant change in glycemic index during the course of the study. The women randomly assigned to the high–glycemic index diet, who met the criteria to start insulin and were changed to a low–glycemic index diet (usually at or shortly after visit 2), achieved a significant reduction in glycemic index by visit 3 and had a glycemic index value similar to that of the original low–glycemic index group by the final visit.
Table 3.
Glycemic index at all visits
| Low–glycemic index group | High–glycemic index group |
P value* | P value† | ||
|---|---|---|---|---|---|
| Did not meet criteria for insulin use | Met criteria for insulin use and changed to low–glycemic index diet | ||||
| n | 31 | 13 | 19 | ||
| Baseline visit | 57.3 ± 0.9 | 57.9 ± 1.5 | 57.4 ± 1.2 | 0.83 | 0.79 |
| Visit 2 | 49.2 ± 0.9‡ | 56.9 ± 1.1 | 57.9 ± 1.0 | <0.001 | 0.53 |
| Visit 3 | 48.7 ± 0.9‡ | 58.2 ± 0.7§ | 52.2 ± 1.4‖ | <0.001 | <0.001 |
| Final visit | 48.0 ± 0.9 | 56.0 ± 1.1§ | 49.6 ± 1.1‖ | 0.018 | <0.001 |
| Change: baseline to final visit (P value) | −8.4 ± 1.0 (<0.001) | −1.5 ± 1.6 (0.38) | −7.9 ± 1.1 (<0.001) | ||
Data are means ± SEM.
*Comparison of low–glycemic index with high–glycemic index groups (combined).
†Comparing those who changed to a low–glycemic index diet with those continuing to consume a high–glycemic index diet.
‡n = 30.
§n = 12.
‖n = 18.
There were no significant differences between the women in either group with respect to weight gain from baseline to delivery, induction of labor, method of delivery, or gestational age at delivery (data not shown). For women in the low–glycemic index group, the birth centile (46.3 ± 5.0) and ponderal index (2.7 ± 0.05) were not significantly different from the birth centile (54.3 ± 4.8, P = 0.25) and ponderal index (2.6 ± 0.04, P = 0.12) for women in the high–glycemic index diet group. Three women in both groups had a large-for-gestational-age baby (≥90th centile), and two women in the low–glycemic index group had a small-for-gestational-age baby (≤10th centile). Overall, there were no significant differences in obstetric and fetal outcomes between the two groups.
The obstetric and fetal outcomes were further analyzed with respect to comparing women who were and were not receiving insulin for 1) women consuming a low–glycemic index diet, 2) women consuming a high–glycemic index diet, and 3) the two groups combined. There were no significant differences with respect to induction of labor, method of delivery, fetal centile, and ponderal index (data not shown).
CONCLUSIONS
Two recent reports have shown the advantages of a low–glycemic index diet for the management of individuals with type 2 diabetes (12,13). Although evidence about the usefulness of a low–glycemic index diet in pregnancy is limited (14), we have previously shown that consumption of a low–glycemic index diet from the beginning of the second trimester resulted in better fetal outcomes (7). The usual practice in our clinic has been to encourage low–glycemic index choices when offering MNT to women with GDM. However, this recommendation was based on clinical experience and had not been formally examined. We therefore decided to extend the observations about the potential benefits of a low–glycemic index diet in pregnancy to women with GDM.
It was impossible to blind women to the glycemic index concept, as it is widely known and discussed in the lay press. The study criteria excluded any woman who was unwilling to follow the prescribed diet. The standard literature about GDM that was provided to all women wasrewritten to remove reference to the glycemic index of food. During recruitment and the consent process, it was carefully explained to all women that the best diet for the treatment of GDM was not known and that finding the best diet was the purpose of the study.
Women randomly assigned to receive a low–glycemic index diet were able to lower the glycemic index of their diet rapidly and maintain this lower level for the duration of pregnancy. Women who were consuming a higher–glycemic index diet and, because they met the criteria to start insulin, were advised to change to a low–glycemic index diet also achieved this lower level rapidly and were able to maintain it for the duration of the pregnancy. The final glycemic index in both groups consuming a low–glycemic index diet was not significantly different. Fiber intake, which sometimes has been a confounding variable in determining the potential advantages of a low–glycemic index diet, was similar in both groups. Both groups of women self-restricted their energy intake (and weight gain) by reducing the amount of CHOs consumed.
Women randomly assigned to initially consume a low–glycemic index diet had a significantly lower rate of insulin use. All women consuming the higher glycemic index diet who met the criteria to start insulin were changed to a low–glycemic index diet, and about half no longer met the criteria to start insulin and thus were able to avoid its use.
Insulin use for the women with higher glycemic levels resulted in fetal centile and ponderal indexes that were not significantly different from those in the diet-treated groups. In contrast to our previous study in normal women, the low–glycemic index diet for women with GDM did not result in a significantly lower fetal centile or ponderal index. It is very probable that this result was related to the shorter duration of the diet for women with GDM compared with women starting the diet during the first trimester. However, demonstration of a difference was not the primary aim of the study, and it was not powered for this purpose. Although a trend was apparent, it is possible that a longer duration of a low–glycemic index diet may be required.
In summary, a low–glycemic index diet for women with GDM is safe, well tolerated, and sustainable. A low–glycemic index diet significantly reduces the need for the use of insulin without compromise of obstetric or fetal outcomes.
Acknowledgments
This study was funded by internal revenue from the Illawarra Diabetes Service and the University of Sydney.
J.B.M. is a coauthor of The New Glucose Revolution book series (Hodder and Stoughton, London; Marlowe and Co, New York; and Hodder Headline, Sydney and elsewhere); President of the GI Foundation, a nonprofit glycemic index–based food endorsement program in Australia; and Director of the University of Sydney glycemic index testing service.
No potential conflicts of interest relevant to this article were reported.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1.Metzger BE, Coustan DR: (Eds). Proceedings of the Fourth International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes Care 1998; 21( Suppl. 2): B1– B167 [PubMed] [Google Scholar]
- 2.Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS: Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med 2005; 352: 2477– 2486 [DOI] [PubMed] [Google Scholar]
- 3.American Diabetes Association Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes Care 2008; 31( Suppl. 1): S61– S78 [DOI] [PubMed] [Google Scholar]
- 4.Langer L, Conway DL, Berkus MD, Xenakis EM-J, Gonzales O: A comparison of glyburide and insulin in women with gestational diabetes mellitus. N Engl J Med 2000; 343: 1134– 1138 [DOI] [PubMed] [Google Scholar]
- 5.Rowan JA, Hague WM, Gao W, Battin MR, Moore MP: Metformin versus insulin for the treatment of gestational diabetes. N Engl J Med 2008; 358: 2003– 2015 [DOI] [PubMed] [Google Scholar]
- 6.Chew I, Brand J, Thorburn A, Truswell A: Application of glycemic index to mixed meals. Am J Clin Nutr 1988; 47: 53– 56 [DOI] [PubMed] [Google Scholar]
- 7.Moses RG, Luebcke M, Davis WS, Coleman KJ, Tapsell LC, Petocz P, Brand-Miller JC: The effect of a low–glycemic index diet during pregnancy on obstetric outcomes. Am J Clin Nutr 2006; 84: 807– 812 [DOI] [PubMed] [Google Scholar]
- 8.Hoffman L, Nolan C, Wilson JD, Oats JJ, Simmons D: Gestational diabetes mellitus—management guidelines: the Australasian Diabetes in Pregnancy Society. Med J Aust 1998; 169: 93– 97 [DOI] [PubMed] [Google Scholar]
- 9.Commonwealth Department of Health and Ageing; National Health and Medical Research Council Nutrient Reference Values for Australia and New Zealand: Executive Summary, 2006 Department of Health and Ageing, National Health and Medical Research Council and New Zealand Ministry of Health, Canberra, Australia [Google Scholar]
- 10.Moses RG, Webb AJ, Comber CD, Walton JG, Coleman KJ, Davis WS, McCosker CJ: Gestational diabetes: compliance with testing. Aust NZ J Obstet Gynaecol 2003; 43: 469– 470 [DOI] [PubMed] [Google Scholar]
- 11.Atkinson FS, Foster-Powell K, Brand-Miller JC: International tables of glycemic index and glycemic load values: 2008. Diabetes Care 2008; 31: 2281– 2283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wolever TMS, Mehling C, Chiasson J-L, Josse RG, Leiter LA, Maheux P, Rabasa-Lhoret R, Rodger NW, Ryan EA: Low glycaemic index diet and disposition index in type 2 diabetes (the Canadian trial of Carbohydrates in Diabetes): a randomised controlled trial. Diabetologia 2008; 51: 1607– 1615 [DOI] [PubMed] [Google Scholar]
- 13.Jenkins DJA, Kendall CWC, McKeown-Eyssen G, Josse RG, Silverberg J, Booth GL, Vidgen E, Josse AR, Ngyuen TH, Corrigan S, Banach MS, Ares S, Mitchell S, Emam A, Augustin LSA, Parker TL, Leiter LA: Effect of a low-glycemic index or a high-cereal fiber diet on type 2 diabetes: a randomised trial. JAMA 2008; 300: 2742– 2753 [DOI] [PubMed] [Google Scholar]
- 14.Dietary advice in pregnancy for preventing gestational diabetes mellitus. Cochrane Database Syst Rev 2008; 2: CD006674. [DOI] [PubMed] [Google Scholar]