Abstract
Objectives
The objectives of our community-wide investigation were to describe multidecade-long trends (1986-2005) in the utilization of thrombolytic therapy, percutaneous coronary interventions, and coronary artery bypass graft surgery in patients hospitalized with acute myocardial infarction (AMI).
Methods
The study sample consisted of 9422 greater Worcester (MA) residents hospitalized with confirmed AMI at all metropolitan Worcester medical centers in 11 annual periods between 1986 and 2005.
Results
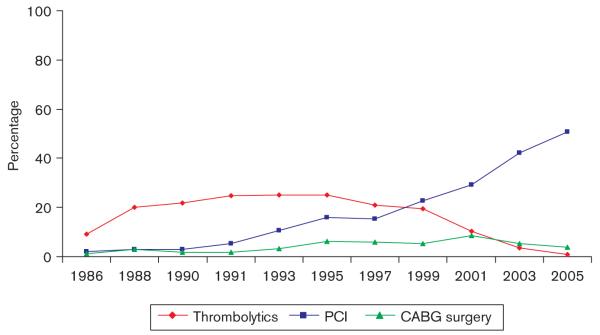
Increases in the utilization of percutaneous coronary interventions were observed between 1986 (2.0%) and 2005 (50.7%) with the most rapid increases beginning in the late 1990s. Utilization of coronary artery bypass graft surgery during hospitalization for AMI increased moderately in the 1990s, remained stable thereafter, and declined to being performed in 3.8% of hospitalized patients in 2005. The use of thrombolytic therapy increased between 1986 and 1995 (9.3-25.2%) and decreased markedly thereafter through 2005 (< 1%). Demographic and clinical characteristics of several patients were associated with the receipt of these treatment regimens.
Conclusion
The results of this study in residents of a large Central New England community suggest an increasingly invasive approach to the management of patients hospitalized with AMI.
Keywords: acute myocardial infarction, cardiovascular epidemiology, coronary reperfusion approaches
Introduction
Dramatic advances in the prevention and treatment of coronary heart disease have taken place over the past several decades. Owing to the development and increased utilization of new management approaches to the primary and secondary prevention of coronary disease, the mortality attributed to coronary disease has declined markedly in the United States over the past 35-40 years [1-3]. Beginning in the 1980s, with new insights into the pathophysiology of acute coronary disease, a paradigm shift in the management of patients with acute myocardial infarction (AMI) occurred with the increased utilization of several pharmacologic and coronary intervention reperfusion strategies.
The number of patients undergoing a percutaneous coronary intervention (PCI) in the United States has increased steadily during the past 20 years [4-8]. The utilization of coronary artery bypass graft (CABG) surgery in patients with AMI, however, has exhibited far less dramatic and consistent trends. Use of thrombolytic therapy in the management of patients hospitalized with AMI has increased since the introduction of these agents in the mid-1980s, although recent data suggest considerable declines in the use of this effective medication and concomitant increases in the use of PCI [9-11]. Few data are available, however, describing changing and contemporary, trends in the use of clot lysing therapy as well as coronary interventional procedures in patients hospitalized with AMI. These data are particularly lacking from the more generalizable perspective of a population-based investigation.
Using data from the Worcester Heart Attack Study, an ongoing population-based investigation of AMI in residents of a large New England metropolitan area [12-14], we examined the evolving application of coronary interventional procedures and the use of thrombolytic agents in this population over an approximately two-decade-long period (1986-2005). The demographic and clinical profile of patients receiving these coronary reperfusion approaches was also examined overall as well as during recent years as compared with prior years under study.
Methods
The Worcester Heart Attack Study is an ongoing investigation describing changes in the epidemiology of coronary heart disease in residents of the Worcester (MA) metropolitan area hospitalized with AMI at all greater Worcester medical centers. Details of this study have been described earlier [12-14]. In brief, the medical records of the Worcester metropolitan area show that the residents (2000 census = 478 000) hospitalized for possible AMI were individually reviewed and validated according to predefined diagnostic criteria based on clinical history, serum enzyme changes, and serial electrocardiographic findings [12-14]. Cases of perioperative-associated AMI were not included. Originally, there were 16 hospitals providing care to greater Worcester residents hospitalized with AMI. On account of hospital closures, mergers, or conversion to chronic care rehabilitation facilities, there are presently 11 greater Worcester medical centers providing care to patients with AMI. As the practice of PCI and the use of thrombolytic medications were introduced into the management of patients hospitalized with AMI during the mid-1980s, we restricted the study sample of the present report to greater Worcester residents hospitalized with AMI at medical centers of all areas in 11 annual periods between 1986 and 2005 [12-14].
Data collection
Trained study physicians and nurses abstracted sociodemographic information, medical history, and clinical data from the medical records of geographically eligible patients hospitalized with AMI at medical centers of all areas. Information was collected about patient’s age, sex, race, body mass index, insurance status, extent of prehospital delay in seeking medical care after the onset of acute coronary symptoms, comorbidities (e.g. diabetes, heart failure, hypertension, stroke), AMI order (initial vs. prior) and type (Q wave vs. non-Q wave), occurrence of clinically significant hospital complications (e.g. atrial fibrillation, heart failure, cardiogenic shock), and hospital survival status [12-14]. Nurse’s and physician’s progress notes, as well as diagnostic test results, were reviewed for information about the use of thrombolytic therapy, PCI, and CABG surgery during the index hospitalization [15].
Data analysis
For purposes of examining factors associated with the utilization of the coronary reperfusion and revascularization approaches examined, a logistic multivariable regression analysis was used. The factors included in our regression analyses were age, sex, insurance status, history of angina, diabetes, heart failure, hypertension or stroke, AMI order (initial vs. prior) and type (Q wave vs. non-Q wave AMI), clinical complications that occurred during hospitalization, and hospital survival status. Each of the variables included in our regression analyses was chosen because of their potential association with treatment for AMI. As information about the duration of prehospital delay was not collected until more recent study years, and because there was a considerable amount of missing data with regards to this variable, we did not control for this factor in our main regression analyses. We also did not control for race in our regression models, as the vast majority (94.4%) of the study population was Caucasian.
Results
Overall, the average age of greater Worcester residents hospitalized with AMI was 69.8 years, 42.7% were women, and 59.4% presented with an initial AMI. In 1986, the average age of patients hospitalized with AMI was 68.3 years increasing to 71.6 years in patients hospitalized with AMI in 2005; men comprised 59.1% of the study sample in 1986 and 53.3% in 2005.
Two-decade-long trends in the use of coronary reperfusion and revascularization strategies
Over the period under study (1986-2005), the percentage of patients receiving thrombolytic therapy during hospitalization for AMI increased between 1986 (9.3%) and 1995 (25.2%) and declined markedly thereafter. The percentage of greater Worcester residents hospitalized with AMI at all metropolitan Worcester medical centers during 2005 who were treated with thrombolytic agents was less than 1 (0.8%) (Fig. 1). In contrast, the percentage of patients receiving PCI, and those undergoing CABG surgery, increased over time, especially during the most recent years under study (Fig. 1). The utilization of PCI increased markedly between 1986 and 2005 (2.0-50.7%), rising steadily over this period. In patients undergoing PCI in 1997, 18.4% of patients received a stent as compared with 95.2% of those undergoing PCI in 2005. Use of CABG surgery increased moderately in the 1990s (1.1-6.1%), remained stable thereafter, and declined to being utilized in 3.8% of greater Worcester residents hospitalized with AMI in 2005.
Fig. 1.
Trends in the utilization of cardiac procedures and thrombolytic therapy during hospitalization for acute myocardial infarction. CABG, coronary artery bypass graft; PCI, percutaneous coronary intervention.
Characteristics of patients receiving coronary reperfusion and revascularization strategies
In examining the demographic and clinical characteristics of patients with AMI receiving thrombolytic therapy or undergoing CABG surgery or PCI, younger patients, men, and those who were overweight or obese were more likely to be treated with thrombolytic therapy or undergo these cardiac procedures than respective comparison groups (Table 1).
Table 1.
Receipt of thrombolytic therapy and cardiac procedures in patients hospitalized with AMI according to patient characteristics
| Characteristics | Thrombolytic therapy (%) | P | PCI (%) | P | CABG surgery (%) | P |
|---|---|---|---|---|---|---|
| Age (years) | ||||||
| <55 | 29.9 | <0.001 | 36.0 | <0.001 | 4.4 | <0.001 |
| 55-64 | 23.4 | 26.2 | 6.1 | |||
| 65-74 | 17.2 | 19.1 | 6.2 | |||
| ≥75 | 7.0 | 11.8 | 2.7 | |||
| Sex | ||||||
| Male | 18.8 | <0.001 | 22.9 | <0.001 | 5.3 | <0.001 |
| Female | 12.4 | 15.9 | 3.4 | |||
| Body mass index | ||||||
| <25 | 11.8 | <0.05 | 22.4 | <0.001 | 4.0 | <0.001 |
| 25-29.9 | 14.7 | 34.5 | 6.7 | |||
| ≥30 | 14.1 | 39.5 | 7.9 | |||
| Payment method | ||||||
| Private payment | 32.3 | <0.001 | 25.4 | <0.001 | 5.0 | <0.005 |
| Private insurance | 23.6 | 23.8 | 4.3 | |||
| Blue cross | 20.8 | 23.6 | 3.4 | |||
| Medicaid | 15.3 | 26.2 | 5.1 | |||
| Medicare | 11.4 | 12.2 | 3.4 | |||
| HMO | 19.1 | 29.4 | 6.5 | |||
| Prehospital delay (hours) | ||||||
| <2 | 32.5 | <0.001 | 21.7 | <0.001 | 4.2 | 0.08 |
| 2-3.9 | 25.2 | 17.0 | 5.7 | |||
| 4-5.9 | 19.2 | 18.0 | 4.0 | |||
| ≥6 | 11.6 | 14.7 | 5.7 | |||
| Medical history | ||||||
| Angina | 11.9 | <0.001 | 17.2 | <001 | 6.6 | <0.001 |
| Diabetes | 10.9 | <0.001 | 17.6 | <001 | 5.7 | <0.001 |
| Heart failure | 3.4 | <0.001 | 10.7 | <0.001 | 2.4 | <0.001 |
| Stroke | 4.9 | <0.001 | 11.8 | <0.001 | 2.6 | <0.005 |
| Hypertension | 12.9 | <0.001 | 20.3 | 0.22 | 5.1 | <0.001 |
| AMI order | ||||||
| Initial | 19.2 | <0.001 | 22.3 | <0.001 | 4.6 | 0.35 |
| Prior | 10.2 | 15.4 | 4.2 | |||
| AMI type | ||||||
| Q wave | 31.1 | <0.001 | 23.0 | <0.001 | 4.0 | 0.12 |
| Non-Q wave | 8.2 | 18.3 | 4.7 | |||
| Clinical complications | ||||||
| Heart failure | ||||||
| Present | 11.5 | <0.001 | 13.9 | <0.001 | 4.2 | 0.22 |
| Absent | 18.9 | 23.7 | 4.7 | |||
| Cardiogenic shock | ||||||
| Present | 18.8 | <0.05 | 28.8 | <0.001 | 8.1 | <0.001 |
| Absent | 15.9 | 19.3 | 4.2 | |||
| Atrial fibrillation | ||||||
| Present | 9.8 | <0.001 | 17.1 | <0.01 | 9.2 | <0.001 |
| Absent | 17.4 | 20.5 | 3.5 | |||
AMI, acute myocardial infarction; CABG, coronary artery bypass graft surgery; HMO, health maintenance organization; PCI, percutaneous coronary intervention.
Patients who were treated with thrombolytic therapy were more likely to have presented at greater Worcester hospitals within 2 h of the onset of acute coronary symptoms and more often had a Q wave infarction than patients who did not receive clot lysing medication. Patients presenting with prior angina, heart failure, diabetes, hypertension, stroke, or myocardial infarction (MI) were less likely to receive thrombolytic medication during hospitalization than respective comparison groups. Patients who paid by private means were more likely to receive thrombolytic therapy, whereas those on Medicare were the least likely to receive clot lysing medications. Patients who developed cardiogenic shock and those who did not develop heart failure or atrial fibrillation during hospitalization were more likely to be treated with thrombolytic agents.
The demographic as well as clinical characteristics of patients more (or less) likely to undergo a PCI were essentially similar to those associated with the receipt of thrombolytics, with a few exceptions. Patients who belonged to health maintenance organizations were most likely to receive a PCI among all insurance categories examined (Table 1). Middle-aged to elderly patients, those who belonged to health maintenance organizations, and those with a history of angina, diabetes, or hypertension were more likely to undergo CABG surgery during hospitalization than respective comparison groups. Patients who developed atrial fibrillation were more likely to undergo CABG surgery than those who did not develop this arrhythmia.
Beginning in 1997, we further classified patients into those with ST and non-ST segment elevation AMI. In the 2067 patients who experienced an ST segment elevation AMI between 1997 and 2005, 26.3% of these patients received thrombolytic therapy. Patients with ST segment elevation AMI were significantly more likely to undergo PCI (45.7%) or CABG surgery (6.0%) in comparison with those with a non-ST segment elevation AMI (13.4 and 4.1%, respectively) (P < 0.001).
Factors associated with receipt of different treatment modalities
We carried out a multivariable-adjusted regression analysis, both in the entire study cohort and separately in patients hospitalized during our two most recent study years of 2003 and 2005, for purposes of providing an overall and contemporary perspective, into the characteristics of patients more (or less) likely to receive thrombolytic therapy and undergo PCI or CABG surgery during hospitalization (Table 2). We did not examine factors associated with the receipt of thrombolytic therapy among patients hospitalized in our two most recent study cohorts, as very few patients with AMI were treated with thrombolytic therapy during these years.
Table 2.
Factors associated with the receipt of selected treatment modalities in patients hospitalized with AMI
| All hospitalized patients |
Patients hospitalized in 2003/2005 |
||||
|---|---|---|---|---|---|
| Characteristicsb | Thrombolytic therapy OR | PCI OR | CABG surgery OR | PCI OR | CABG surgery OR |
| Age (years) | |||||
| 55-64 | 0.89 (0.75,1.05)a | 0.75 (0.64,0.88) | 1.37 (0.99,1.88) | 0.81 (0.57,1.16) | 0.77 (0.35,1.68) |
| 65-74 | 0.69 (0.57,0.83) | 0.72 (0.60,0.85) | 1.45 (1.04,2.01) | 0.72 (0.50,1.04) | 1.85 (0.89,3.85) |
| ≥75 | 0.30 (0.25,0.37) | 0.47 (0.39,0.56) | 0.65 (0.45,0.93) | 0.36 (0.26,0.52) | 0.70 (0.31,1.55) |
| Male sex | 1.03 (0.90,1.17) | 1.09 (0.97,1.23) | 1.38 (1.11,1.71) | 1.48 (1.20,1.81) | 1.14 (0.72,1.79) |
| Body mass index | |||||
| 25-29.9 | 0.89 (0.76,1.03) | 3.94 (3.47,4.48) | 2.05 (1.62,2.59) | 1.84 (1.46,2.33) | 3.20 (1.78,5.75) |
| ≥30 | 0.72 (0.61,0.87) | 4.43 (3.85,5.09) | 2.19 (1.70,2.81) | 1.66 (1.28,2.16) | 2.75 (1.47,5.18) |
| Payment method | |||||
| Private insurance | 0.89 (0.66,1.18) | 1.13 (0.85,1.49) | 0.97 (0.55,1.71) | 1.34 (0.71,2.51) | 1.88 (0.47,7.49) |
| Blue cross | 0.76 (0.59,0.97) | 1.13 (0.89,1.43) | 0.73 (0.44,1.21) | 0.92 (0.56,1.49) | 1.28 (0.39,4.24) |
| Medicaid | 0.69 (0.48,1.01) | 1.18 (0.85,1.63) | 1.08 (0.58,2.02) | 1.02 (0.53,1.98) | 2.59 (0.65,10.27) |
| Medicare | 0.91 (0.73,1.13) | 0.70 (0.57,0.86) | 0.79 (0.54,1.17) | 0.72 (0.46,1.12) | 1.40 (0.46,4.27) |
| HMO | 0.90 (0.73,1.13) | 1.31 (1.09,1.59) | 1.31 (0.91,1.88) | 0.92 (0.60,1.41) | 1.44 (0.49,4.24) |
| Medical history | |||||
| Angina | 0.95 (0.81,1.10) | 1.0 (0.88,1.14) | 2.02 (1.63,2.49) | 1.33 (1.03,1.72) | 0.90 (0.51,1.59) |
| Diabetes | 0.78 (0.68,0.90) | 0.82 (0.72,0.92) | 1.44 (1.17,1.77) | 0.99 (0.79,1.24) | 0.94 (0.59,1.52) |
| Heart failure | 0.33 (0.26,0.43) | 0.70 (0.59,0.83) | 0.43 (0.31,0.59) | 0.64 (0.49,0.83) | 0.34 (0.17,0.66) |
| Stroke | 0.42 (0.31,0.56) | 0.75 (0.61,0.92) | 0.57 (0.39,0.85) | 0.61 (0.44,0.85) | 0.40 (0.16,1.02) |
| Hypertension | 0.89 (0.79,1.00) | 1.28 (1.14,1.44) | 1.31 (1.05,1.63) | 0.88 (0.69,1.12) | 1.43 (0.82,2.49) |
| AMI characteristics | |||||
| Initial | 1.04 (0.90,1.20) | 1.24 (1.10,1.41) | 1.17 (0.94,1.46) | 1.11 (0.89,1.39) | 0.92 (0.57,1.48) |
| Q wave | 3.79 (3.36,4.28) | 1.19 (1.06,1.34) | 0.80 (0.64,0.99) | 2.66 (2.04,3.48) | 0.80 (0.46,1.41) |
| Clinical complications | |||||
| Heart failure | 0.93 (0.81,1.06) | 0.71 (0.63,0.81) | 0.95 (0.76,1.19) | 0.59 (0.46,0.74) | 1.67 (1.02,2.72) |
| Cardiogenic shock | 1.32 (1.05,1.65) | 2.62 (2.15,3.21) | 1.97 (1.43,2.72) | 2.56 (1.61,4.08) | 1.08 (0.45,2.56) |
| Atrial fibrillation | 0.73 (0.61,0.87) | 1.06 (0.91,1.23) | 3.56 (2.86,4.42) | 0.81 (0.63,1.04) | 2.14 (1.33,3.46) |
AMI, acute myocardial infarction; CABG, coronary artery bypass graft surgery; HMO, health maintenance organization; OR, odds ratio; PCI, percutaneous coronary intervention.
95% confidence interval.
Respective referent categories: age <55, women, body mass index <25, private payment, absence of selected comorbidities, prior myocardial infarction (MI), non-Q wave MI, absence of clinical complications during hospitalization.
Older patients were significantly less likely to receive thrombolytic therapy than younger hospitalized patients during all study years (Table 2). Obese patients were significantly less likely to be treated with this therapy, patients on Blue Cross/Blue Shield insurance, as were patients with a history of diabetes, heart failure, or stroke than respective comparison groups. In contrast, patients experiencing a Q wave MI were significantly more likely to be treated with clot lysing therapy than those with a non-Q wave AMI. Patients who developed cardiogenic shock and those who did not develop atrial fibrillation during hospitalization were significantly more likely to be treated with thrombolytic therapy than respective comparison groups.
Patients of advanced age, those with Medicare insurance, and patients with a history of either diabetes, heart failure, or stroke were significantly less likely to undergo PCI during all study years than respective comparison groups. In contrast, overweight and obese patients, those belonging to health maintenance organizations, those with a history of hypertension, and patients presenting to greater Worcester hospitals with an initial Q wave MI were significantly more likely to undergo PCI during their index hospitalization. Patients who did not develop heart failure and those who developed cardiogenic shock were significantly more likely to undergo a PCI.
Patients in the age range 65-74 years, men, those who were overweight or obese, patients with a history of angina, diabetes or hypertension, and those who developed cardiogenic shock or atrial fibrillation during hospitalization were significantly more likely to undergo CABG surgery during all study years than respective comparison groups. Patients aged 75 years and above, those with a history of heart failure or stroke, and patients who developed a Q wave MI were significantly less likely to undergo coronary bypass surgery than respective comparison groups (Table 2). Relatively similar factors were associated with the likelihood of undergoing PCI or CABG surgery during hospitalization for AMI in 2003 and 2005 although the statistical significance of several of these factors was attenuated because of the small sample sizes under study.
When duration of prehospital delay was added to these regression models, because this variable was missing in a considerable percentage of the overall study sample (nearly 43%), the greater the duration of prehospital delay, the significantly less likely were patients to be treated with thrombolytic therapy, particularly those who delayed seeking medical care by 6 h or more [adjusted odds ratio (OR) = 0.57, 95% confidence interval (CI): 0.44, 0.73] compared with those who presented to area hospitals within 2 h of acute symptom onset. Although there was no significant association between duration of care seeking behavior and likelihood of undergoing CABG surgery, patients who presented to greater Worcester medical centers between 2-4 h (adjusted OR = 0.79, 95% CI: 0.70, 0.94) and 6 h or more after acute symptom onset (OR = 0.70, 95% CI: 0.58, 0.84) were significantly less likely to undergo PCI compared with patients who presented to greater Worcester hospitals within 2 h of acute symptom onset.
Changing profile of patients undergoing coronary reperfusion/revascularization over time
Contemporary, as well as changing, characteristics of patients receiving thrombolytic therapy, as well as undergoing selected coronary procedures, were examined (Table 3). Four aggregated periods were created for purposes of this analysis. These included the initial two study years (1986/1988), early to mid-1990s (1991/1993), late 1990s (1997/1999), and the two most recent years under study (2003/2005). Although the use of thrombolytic therapy increased from the mid to late 1980s to early 1990s, use of this treatment modality decreased dramatically thereafter across all patient demographic and clinical subgroups examined. Marked increases over time in the utilization of PCI were noted in elderly patients (≤ 75 years), in those with preexisting hypertension, and in persons belonging to health maintenance organizations. Similar patient characteristics were associated with an increased likelihood of undergoing CABG surgery over time.
Table 3.
Receipt of thrombolytic therapy and cardiac procedures in patients hospitalized with AMI according to demographic characteristics and time period of hospitalization
| Thrombolytic therapy |
PCI |
CABG |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristics | 1986/ 1988 (%) |
1991/ 1993 (%) |
1997/ 1999 (%) |
2003/ 2005 (%) |
P | 1986/ 1988 (%) |
1991/ 1993 (%) |
1997/ 1999 (%) |
2003/ 2005 (%) |
P | 1986/ 1988 (%) |
1991/ 1993 (%) |
1997/ 1999 (%) |
2003/ 2005 (%) |
P |
| Age (years) | |||||||||||||||
| <55 | 6.3 | 12.3 | 9.9 | 1.3 | <0.001 | 1.1 | 3.0 | 7.9 | 14.8 | <0.001 | 2.5 | 2.8 | 5.7 | 5.0 | <0.005 |
| 55-64 | 6.0 | 10.8 | 8.5 | 1.3 | 0.5 | 2.4 | 6.0 | 14.7 | 2.8 | 5.3 | 11.7 | 5.0 | |||
| 65-74 | 4.6 | 11.4 | 10.1 | 1.0 | 0.7 | 3.0 | 7.1 | 14.1 | 3.2 | 4.6 | 13.1 | 13.1 | |||
| ≥75 | 1.0 | 5.8 | 9.2 | 0.7 | 0.0 | 1.1 | 4.9 | 18.7 | 0.7 | 3.2 | 10.3 | 11.0 | |||
| Sex | |||||||||||||||
| Male | 14.4 | 26.9 | 24.4 | 2.7 | <0.005 | 1.9 | 6.0 | 17.3 | 40.3 | 0.26 | 5.7 | 11.3 | 29.3 | 20.9 | 0.69 |
| Female | 3.8 | 13.1 | 13.1 | 1.5 | 0.4 | 3.6 | 8.6 | 22.0 | 3.9 | 4.6 | 11.3 | 13.1 | |||
| Body mass index | |||||||||||||||
| <25 | 0.0 | 0.0 | 27.1 | 3.8 | <0.05 | NA | NA | 7.7 | 19.1 | <0.05 | 0.0 | 0.0 | 13.4 | 8.4 | <0.05 |
| 25-29.9 | 0.0 | 0.0 | 36.9 | 4.7 | NA | NA | 10.8 | 29.0 | 0.0 | 0.0 | 20.8 | 22.3 | |||
| ≥30 | 0.0 | 0.0 | 25.4 | 2.1 | NA | NA | 10.3 | 23.1 | 0.0 | 0.0 | 18.3 | 16.8 | |||
| Payment method | |||||||||||||||
| Private payment | 0.9 | 2.8 | 1.9 | 0.2 | <0.001 | 0.0 | 0.6 | 1.2 | 1.7 | <0.05 | 0.4 | 0.4 | 2.5 | 0.7 | 0.65 |
| Private insurance | 1.9 | 4.5 | 1.1 | 0.0 | 0.4 | 1.1 | 1.1 | 3.3 | 0.4 | 1.4 | 1.4 | 1.8 | |||
| Blue cross | 5.1 | 4.7 | 1.4 | 0.4 | 0.9 | 0.9 | 1.3 | 8.4 | 2.5 | 0.7 | 1.1 | 3.9 | |||
| Medicaid | 0.3 | 1.5 | 0.7 | 0.1 | 0.1 | 0.3 | 0.4 | 3.0 | 0.0 | 0.7 | 0.7 | 1.8 | |||
| Medicare | 3.0 | 15.4 | 13.6 | 1.1 | 0.1 | 3.9 | 8.6 | 16.8 | 1.4 | 7.5 | 18.3 | 12.2 | |||
| HMO | 5.2 | 11.2 | 13.1 | 2.4 | 0.7 | 2.7 | 9.0 | 25.8 | 2.5 | 5.4 | 11.8 | 13.3 | |||
| Prehospital delay (hours) | |||||||||||||||
| <2 | 11.2 | 24.5 | 19.6 | 2.7 | 0.42 | 2.0 | 9.4 | 19.5 | 20.3 | 0.42 | 5.5 | 8.5 | 19.5 | 9.2 | 0.96 |
| 2-3.9 | 4.6 | 11.8 | 8.2 | 1.0 | 0.7 | 3.4 | 7.8 | 10.7 | 2.4 | 7.9 | 11.6 | 6.7 | |||
| 4-5.9 | 1.3 | 2.8 | 2.4 | 0.3 | 0.4 | 2.0 | 2.7 | 4.4 | 0.6 | 1.2 | 3.7 | 0.6 | |||
| ≥6 | 0.9 | 4.8 | 4.1 | 0.0 | 0.4 | 2.6 | 7.0 | 6.8 | 2.4 | 4.3 | 12.2 | 3.7 | |||
| Medical history | |||||||||||||||
| Angina | 3.1 | 8.1 | 5.8 | 0.5 | 0.16 | 0.6 | 2.4 | 6.5 | 11.3 | <0.005 | 3.2 | 6.4 | 14.5 | 6.0 | <0.05 |
| Diabetes | 2.9 | 8.5 | 7.9 | 0.7 | 0.31 | 0.2 | 2.0 | 6.1 | 19.0 | <0.001 | 2.1 | 4.6 | 16.3 | 12.4 | 0.14 |
| Heart failure | 0.1 | 2.1 | 2.0 | 0.4 | <0.01 | 0.0 | 0.4 | 1.8 | 9.0 | <0.001 | 0.7 | 2.1 | 3.5 | 4.2 | 0.63 |
| Stroke | 0.5 | 1.3 | 1.2 | 0.1 | 0.85 | 0.4 | 0.5 | 1.4 | 4.4 | 0.94 | 0.7 | 1.1 | 3.2 | 1.8 | 0.65 |
| Hypertension | 7.4 | 19.4 | 20.3 | 2.1 | <0.005 | 1.3 | 4.3 | 15.8 | 42.8 | <0.001 | 5.0 | 9.5 | 29.7 | 27.2 | <0.001 |
| AMI order | |||||||||||||||
| Initial | 14.8 | 30.2 | 29.8 | 3.7 | 0.60 | 2.2 | 6.7 | 19.7 | 44.1 | <0.05 | 6.4 | 9.2 | 26.5 | 22.3 | 0.70 |
| Prior | 3.4 | 9.8 | 7.8 | 0.5 | 0.1 | 2.8 | 6.2 | 18.2 | 3.2 | 6.7 | 14.1 | 11.7 | |||
| MI type | |||||||||||||||
| Q wave | 13.2 | 27.7 | 26.0 | 2.0 | <0.05 | 1.6 | 5.1 | 13.8 | 18.8 | <0.001 | 3.5 | 5.7 | 15.6 | 6.4 | <0.05 |
| Non-Q wave | 5.0 | 12.3 | 11.6 | 2.2 | 0.7 | 4.4 | 12.1 | 43.5 | 6.0 | 10.3 | 25.1 | 27.6 | |||
| Clinical complications | |||||||||||||||
| Heart failure | |||||||||||||||
| Present | 8.5 | 19.0 | 13.4 | 0.9 | 0.13 | 1.6 | 6.5 | 12.9 | 31.0 | 0.89 | 1.0 | 2.7 | 4.6 | 5.2 | 0.11 |
| Absent | 18.3 | 28.7 | 23.7 | 3.2 | 3.1 | 9.1 | 22.1 | 55.6 | 2.5 | 2.4 | 6.0 | 4.3 | |||
| Cardiogenic shock | |||||||||||||||
| Present | 7.6 | 37.1 | 25.0 | 1.0 | 0.62 | 1.7 | 19.0 | 30.4 | 60.8 | <0.01 | 3.4 | 5.2 | 13.7 | 7.2 | 0.21 |
| Absent | 14.9 | 24.1 | 19.8 | 2.3 | 2.5 | 7.3 | 18.1 | 45.1 | 1.8 | 2.3 | 5.0 | 4.5 | |||
| Atrial fibrillation | |||||||||||||||
| Present | 10.6 | 15.2 | 11.5 | 1.5 | 0.26 | 2.4 | 6.4 | 17.7 | 34.5 | 0.09 | 3.2 | 6.4 | 12.2 | 7.1 | 0.89 |
| Absent | 15.1 | 26.6 | 21.6 | 2.5 | 2.5 | 8.3 | 19.2 | 49.2 | 1.6 | 1.8 | 4.5 | 4.0 | |||
AMI, acute myocardial infarction; CABG, coronary artery bypass graft surgery; HMO, health maintenance organization; MI, myocardial infarction; PCI, percutaneous coronary intervention.
Use of cardiac procedures according to patient’s age and sex
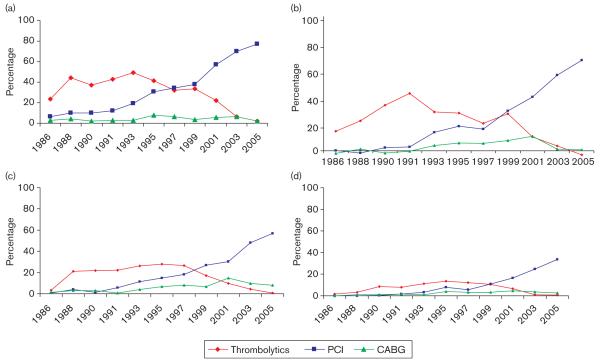
Owing to the differences in the utilization of thrombolytic therapy and interventional procedures in individuals of different ages and in men as compared with women, as well as ongoing national interest in this area, we carried out two further subgroup analyses according to patient’s age (< 55, 55-64, 65-74, ≤ 75 years) and sex (Fig. 2a-d).
Fig. 2.
(a) Trends in cardiac procedures and thrombolytic therapy in patients below 55 years of age. (b) Trends in cardiac procedures and thrombolytic therapy in patients aged 55-64 years. (c) Trends in cardiac procedures and thrombolytic therapy in patients aged 65-74 years. (d) Trends in cardiac procedures and thrombolytic therapy in patients aged 75 years and above. CABG, coronary artery bypass graft; PCI, percutaneous coronary intervention.
The use of thrombolytic agents was highest in patients below 65 years; patients in all age strata exhibited increasing trends in the use of clot lysing medications from the mid-1980s to early/mid 1990s with a marked decline in thrombolytic use from the late 1990s to 2005. The use of thrombolytic therapy declined from 9 to 10% in the four age groups examined during the mid-1990s to less than 1% across all four age strata in 2005. In contrast, patients of all ages had a slight increase in the use of PCI from the mid-1980s to the mid-1990s with a sharp increase thereafter (Fig. 2a-d). In 2005, 38.3% of patients at least 75 years of age received PCI compared with 76.8% of patients below 55 years. The use of CABG surgery remained relatively stable from the mid-1980s to the mid-1990s, but approximately doubled in use for patients aged 55 years and above in the late 1990s. The use of coronary bypass surgery declined to previously observed levels for patients aged 55-64 years, but remained stable or declined for patients 65-74 and at least 75 years old.
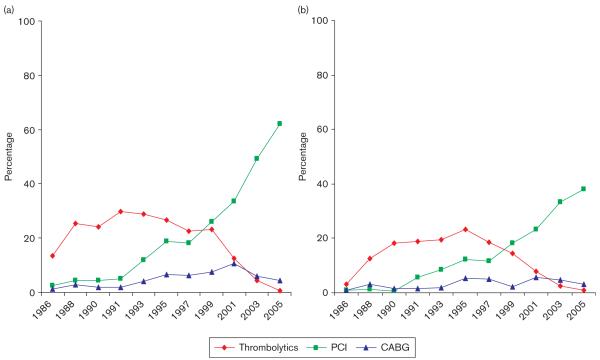
Men were between two and three times more likely to receive thrombolytic therapy than women over the entire study period (Fig. 3a and b). The use of thrombolytic agents increased in men and women from the mid-1980s to early 1990s, remained stable until the late 1990s, and then declined in both sexes through 2005. Trends in cardiac procedure use did not differ significantly between the two sexes although men had a much higher overall procedure use relative to women. The use of PCI increased over time for both men and women; however, the extent of use in men was appreciably greater than for women across all study years. In 2005, 62.0% of men and 38.0% of women underwent a PCI during their acute hospitalization. The use of CABG surgery increased for both men and women from the mid-1980s to the late 1990s; however, the use in men declined by approximately one-third from the late 1990s to 2005, with slight increases noted in women over time.
Fig. 3.
(a) Trends in cardiac procedures and thrombolytic therapy in men hospitalized with acute myocardial infarction. (b) Trends in cardiac procedures and thrombolytic therapy in women hospitalized with acute myocardial infarction. CABG, coronary artery bypass graft; PCI, percutaneous coronary intervention.
Discussion
The results of this study in the residents of a large New England metropolitan area suggest divergent trends over the past 20 years in the use of clot lysing medication and coronary reperfusion/revascularization approaches in greater Worcester residents hospitalized at all metropolitan Worcester medical centers with AMI. The use of thrombolytic therapy peaked during the mid-1990s but has declined markedly thereafter to essentially non-use in 2005. Use of PCI has become the primary coronary reperfusion treatment approach of choice in this patient population, whereas the use of CABG surgery has remained relatively stable over time, being used significantly less often during recent study years as compared with PCI. The results of this study update and extend our recently published findings to include an additional study year as well as to include data on the use of thrombolytic therapy in our study population [16].
Changing trends in the use of coronary reperfusion and revascularization procedures
Our results are in agreement with the findings from several prior studies and with our earlier publication [5,6,16]. In the National Registry of Myocardial Infarction, a decline in the use of thrombolytic therapy was observed in patients hospitalized with AMI at more than 1200 medical centers throughout the United States between 1990 and 1999 (34% to 21%); only minor increasesin the use of both PCI (7-10%) and CABG surgery (11-13%) were observed over this period [5]. In 1999, approximately one in five greater Worcester residents hospitalized with AMI were treated with thrombolytic therapy and 23 and 5% underwent PCI and CABG surgery, respectively.
In the Minnesota Heart Survey, which evaluated trends in the use of coronary reperfusion approaches in the residents of Twin Cities (MN) between the ages of 30 and 74 years hospitalized with acute coronary disease at numerous medical centers throughout the St Paul-Minneapolis metropolitan area between 1985 and 1997, the use of thrombolytic therapy increased for both men (13-28%) and women (11-27%) during this period [6]. Similar increases in the use of coronary angioplasty were observed in both sexes between the initial (one in every 20 men and women) and most recent (one in every three men and women) years under study. Increases in the use of CABG surgery were observed in men (5-10%), whereas the use of CABG surgery remained stable in women (7-8%) over this period.
Differences in practice standards between New England and other regions of the United States need to be considered in comparing our findings to national or other more regional-based investigations, upper age limit of patients included, demographic, clinical, and treatment characteristics of the respective study populations, as well as time periods under investigation. It has been previously shown that physicians practicing in New England are less likely to use thrombolytic and coronary reperfusion therapy, but effective cardiac medications more often, compared with physicians practicing in other regions of the United States [17]. These differences could be because of several factors including the fact that practitioners in New England follow evidence-based guidelines more closely when treating patients with cardiac disease, which may result in better overall care [18]. Cost considerations as well as patient treatment preferences may also vary according to geographic location.
The results of this study clearly demonstrate that PCI has become the predominant modality used for the management of patients hospitalized with AMI throughout Central Massachusetts and has probably made an important contribution to the improving hospital as well as long-term prognosis of this patient population during the past several decades [12-14,16]. Monitoring of these evolving treatment approaches remains of continued importance, particularly in the present era of quality-assurance initiatives and cost-containment efforts.
Factors associated with the use of coronary reperfusion strategies and revascularization procedures
Several demographic and clinical factors were associated with the utilization of PCI and CABG surgery in this study. Elderly patients were consistently less likely to receive any of these cardiac procedures, a finding consistent with the results of other investigations [7,8,19,20].
Although there has been a marked decline over time in the use of thrombolytic therapy for the management of patients with AMI, patients with a Q wave and/or ST segment elevation MI were significantly more likely to receive thrombolytic therapy than patients with other electrocardiographic findings. These findings are consistent with the results of numerous prior studies, which have shown the importance of rapid clot dissolution in patients with ST segment elevation MI [5,9,10]. Men were more likely to receive all procedures of interest relative to women, a finding that has been noted in several prior investigations [8,21], including our own [16]. In the National Inpatient Sample database, women underwent coronary angioplasty and stent placement at essentially similar rates with men over the period 1995 through 2001 [8]; women, however, were approximately 20% less likely to undergo coronary bypass surgery than men. Our results showed similar trends with women being less likely to receive cardiac procedures than men. In contrast, both men and women exhibited relatively similar trends in the use of the cardiac interventional procedures of interest as well as of thrombolytic therapy.
Comparatively younger patients in our study were more likely to receive treatment with thrombolytic therapy and PCI, whereas patients between the ages of 55 and 74 years were more likely to undergo CABG surgery, findings that are supported by the results from several previous studies. Investigators from the multinational Global Registry of Acute Coronary Events study found higher rates of thrombolytic therapy, PCI, and cardiac surgery use in patients aged 65-74 years who were hospitalized with an acute coronary syndrome as compared with older patients [19]. Investigators from the National Registry of Myocardial Infarction reported a declining utilization of thrombolytic therapy across all age groups, and a slight decrease in the use of CABG surgery, between 1990 and 1999 in patients hospitalized with AMI with concomitant increases in the use of PCI [5]. Findings from the Minnesota Heart Survey suggest increasing trends in PCI usage, and stable use of CABG surgery, in patients hospitalized with AMI in medical centers throughout the Minneapolis-St Paul metropolitan area between 1985 and 1995. The use of thrombolytic therapy increased during the first half of this study but declined slightly by 1995 [6].
In our study, overweight and obese individuals were significantly more likely to undergo a PCI and CABG surgery than persons of normal weight. In an analysis of a Medicare-insured, elderly patient population, overweight and obese individuals had higher rates of coronary procedure utilization compared with those of normal body weight [22].
Earlier studies have shown that patients with a Q wave MI derive significant benefit from the use of coronary reperfusion and revascularization therapies; however, the benefit of such techniques for patients with a non-Q wave MI is less definitive [3]. Recent years have seen the development of more stringent, aggressive guidelines regarding the management of patients with a non-Q wave AMI because of increasing clinical knowledge of its prognostic importance [23].
Several AMI-associated clinical features have been associated with the utilization of various cardiac procedures. In a single Veteran’s Affairs Hospital, patients with a Q wave MI were more likely to undergo a PCI, whereas those with a history of heart failure were less likely to undergo a PCI, in the early to mid-1990s [24]. Patients with diabetes were less likely to be treated with thrombolytic therapy or receive a PCI, but were more likely to undergo CABG surgery, than patients without diabetes, findings similar to the results of our study.
We can only speculate about the factors that may have contributed to the observed trends in procedure utilization in our study. Hospital reimbursement procedures, willingness to perform procedures in different at-risk groups, issues related to patient acceptability of different procedures and therapies, and generally greater adherence to evidence-based medications and therapeutic procedures may have taken place over the period under study and have led to changes in the management of patients hospitalized with AMI.
Study strengths and limitations
The strengths of this study include its population-based perspective, multiple time periods under investigation, and independent confirmation of AMI. The limitations of this observational investigation include the lack of data on physician characteristics that may be associated with treatment prescribing practices, patient preferences, and information about other situational, financial, or socio-cultural factors that may be related to the treatment decision-making process in the setting of AMI.
Conclusion
The results of our community-wide investigation show the changing utilization of different management approaches in patients hospitalized with AMI. The increasingly aggressive management of these high-risk patients with PCI, together with the demographic and clinical characteristics associated with the receipt of the coronary reperfusion approaches examined, need to be considered when planning the future role of these and other possible treatment modalities in the management of patients with AMI. There remains an ongoing need for continued monitoring of the characteristics of patients who fail to receive specific cardiac procedures and beneficial cardiac medications, as well as consideration of the financial implications of specific treatment approaches, in the context of evolving systems of healthcare delivery and cost-containment strategies.
Acknowledgements
This research was made possible by the cooperation of participating hospitals in the Worcester metropolitan area and through funding support provided by the National Institutes of Health (RO1 HL35434).
References
- 1.American Heart Association . Heart Disease and Stroke Statistics - 2008 Update. American Heart Association; Dallas, Texas: 2008. © 2008, American Heart Association. [Google Scholar]
- 2.Ryan TJ, Anderson JL, Antman EM, Braniff BA, Brooks NH, Califf RM, et al. ACC/AHA guidelines for the management of patients with acute myocardial infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction) J Am Coll Cardiol. 1996;28:1328–1428. doi: 10.1016/s0735-1097(96)00392-0. [DOI] [PubMed] [Google Scholar]
- 3.Ryan TJ, Antman EM, Brooks NH, Califf RM, Hillis LD, Hiratzka LF, et al. update: ACC/AH guidelines for the management of patients with acute myocardial infarction: executive summary and recommendations: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction) Circulation. 1999;100:1016–1030. doi: 10.1161/01.cir.100.9.1016. 1999. [DOI] [PubMed] [Google Scholar]
- 4.Heidenreich PA, McClellan M. Trends in treatment and outcomes for acute myocardial infarction: 1975-1995. Am J Med. 2001;110:165–174. doi: 10.1016/s0002-9343(00)00712-9. [DOI] [PubMed] [Google Scholar]
- 5.Rogers WJ, Canto JG, Lambrew CT, Tiefenbrunn AJ, Kinkaid B, Shoultz DA, et al. Temporal trends in the treatment of over 1.5 million patients with myocardial infarction in the US from 1990 through 1999: the National Registry of Myocardial Infarction 1, 2 and 3. J Am Coll Cardiol. 2000;36:2056–2063. doi: 10.1016/s0735-1097(00)00996-7. [DOI] [PubMed] [Google Scholar]
- 6.McGovern PG, Jacobs DR, Jr, Shahar E, Arnett DK, Folsom AR, Blackburn H, et al. Trends in acute coronary heart disease mortality, morbidity, and medical care from 1985 through 1997: the Minnesota Heart Survey. Circulation. 2001;104:19–24. doi: 10.1161/01.cir.104.1.19. [DOI] [PubMed] [Google Scholar]
- 7.Pilote L, Saynina O, Lavoie F, McClellan M. Cardiac procedure use and outcomes in elderly patients with acute myocardial infarction in the United States and Quebec, Canada, 1988-1994. Med Care. 2003;41:813–822. doi: 10.1097/00005650-200307000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Bertoni AG, Bonds DE, Lovato J, Goff DC, Brancati FL. Sex disparities in procedure use for acute myocardial infarction in the United States, 1995-2001. Am Heart J. 2004;147:1054–1060. doi: 10.1016/j.ahj.2003.11.019. [DOI] [PubMed] [Google Scholar]
- 9.Rosamond WD, Shahar E, McGovern PG, Sides TL, Luepker RV. Trends in coronary thrombolytic therapy for acute myocardial infarction (The Minnesota Heart Survey Registry, 1990-1993) Am J Cardiol. 1996;78:271–277. doi: 10.1016/s0002-9149(96)00276-7. [DOI] [PubMed] [Google Scholar]
- 10.Goldberg RJ, Spencer FA, Okolo J, Lessard D, Yarzebski J, Gore JM. Long-term trends in the use of coronary reperfusion strategies in acute myocardial infarction: a community-wide perspective. J Thromb Thrombolysis. 2007;23:163–171. doi: 10.1007/s11239-006-9029-0. [DOI] [PubMed] [Google Scholar]
- 11.Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 12.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Recent changes in attack and survival rates of acute myocardial infarction (1975-1981): the Worcester Heart Attack Study. J Am Med Assoc. 1986;255:2774–2779. [PubMed] [Google Scholar]
- 13.Goldberg RJ, Yarzebski J, Lessard D, Gore JM. A two-decades (1975-1995) long experience in the incidence, in-hospital and long-term case-fatality rates of acute myocardial infarction: a community-wide perspective. J Am Coll Cardiol. 1999;33:1533–1539. doi: 10.1016/s0735-1097(99)00040-6. [DOI] [PubMed] [Google Scholar]
- 14.Goldberg RJ, Spencer FA, Yarzebski J, Lessard D, Gore JM, Alpert JS, et al. A 25-year perspective into the changing landscape of patients hospitalized with acute myocardial infarction (the Worcester Heart Attack Study) Am J Cardiol. 2004;94:1373–1378. doi: 10.1016/j.amjcard.2004.07.142. [DOI] [PubMed] [Google Scholar]
- 15.Spencer FA, Lessard D, Yarzebski J, Gore JM, Goldberg RJ. Decade-long changes in the use of combination evidence-based medical therapy at discharge for patients surviving acute myocardial infarction. Am Heart J. 2005;150:838–844. doi: 10.1016/j.ahj.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 16.Hahn J, Lessard D, Yarzebski J, Goldberg J, Pruell S, Spencer FA, et al. A community-wide perspective into changing trends in the utilization of diagnostic and interventional procedures in patients hospitalized with acute myocardial infarction. Am Heart J. 2007;153:594–605. doi: 10.1016/j.ahj.2007.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krumholz HM, Chen J, Rathore SS, Wang Y, Radford MJ. Regional variation in the treatment and outcomes of myocardial infarction: investigating New England’s advantage. Am Heart J. 2003;146:242–249. doi: 10.1016/S0002-8703(03)00237-0. [DOI] [PubMed] [Google Scholar]
- 18.Pilote L, Califf RM, Sapp S, Miller DP, Mark DB, Weaver WD, et al. Regional variation across the United States in the management of acute myocardial infarction. N Engl J Med. 1995;333:565–572. doi: 10.1056/NEJM199508313330907. [DOI] [PubMed] [Google Scholar]
- 19.Avezum A, Makdisse M, Spencer F, Gore JM, Fox KA, Montalescot G, et al. GRACE investigators Impact of age on management and outcome of acute coronary syndrome: observations from the Global Registry of Acute Coronary Events (GRACE) Am Heart J. 2005;149:67–73. doi: 10.1016/j.ahj.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 20.De Boer MJ, Ottervanger JP, Van’t Hof AW, Hoorntje JC, Suryapranata H, Zijlstra F. Reperfusion therapy in elderly patients with acute myocardial infarction: a randomized comparison of primary angioplasty and thrombolytic therapy. J Am Coll Cardiol. 2002;39:1723–1728. doi: 10.1016/s0735-1097(02)01878-8. [DOI] [PubMed] [Google Scholar]
- 21.Vaccarino V, Rathore SS, Wenger NK, Frederick PD, Abramson JL, Barron HV, et al. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. N Engl J Med. 2005;353:671–682. doi: 10.1056/NEJMsa032214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yancy WS, Jr, Olsen MK, Curtis LH, Schulman KA, Cuffe MS, Oddone EZ. Variations in coronary procedure utilization depending on body mass index. Arch Intern Med. 2005;165:1381–1387. doi: 10.1001/archinte.165.12.1381. [DOI] [PubMed] [Google Scholar]
- 23.Yang H, Pu M, Rodriguez D, Underwood D, Griffin BP, Kalahasti V, et al. Ischemic and viable myocardium in patients with non-Q-wave or Q-wave myocardial infarction and left ventricular dysfunction: a clinical study using positron emission tomography, echocardiography, and electrocardiography. J Am Coll Cardiol. 2004;43:592–598. doi: 10.1016/j.jacc.2003.07.052. [DOI] [PubMed] [Google Scholar]
- 24.Maynard C, Sales AE. Changes in the use of coronary artery revascularization procedures in the Department of Veterans Affairs, the National Hospital Discharge Survey, and the Nationwide Inpatient Sample, 1991-1999. BMC Health Services Res. 2003;3:12–19. doi: 10.1186/1472-6963-3-12. [DOI] [PMC free article] [PubMed] [Google Scholar]