Abstract
Context:
Nonradiographic tests to identify fractures rely on a patient's report of increased pain at the site of injury. These tests can be misleading and produce false-positive or false-negative results because of differences in pain tolerance. A painless technique using a tuning fork and stethoscope to detect fractures has undergone limited review in the athletic training literature.
Objective:
To determine if the use of a 128-Hz vibrating tuning fork and stethoscope were effective in identifying fractures.
Design:
Cross-sectional study.
Setting:
University athletic training room or local orthopaedic center when fractures were suspected.
Patients or Other Participants:
A total of 37 patients (19 males, 18 females) volunteered.
Main Outcome Measure(s):
A diminished or absent sound arising from the injured bone as compared with the uninjured bone represented a positive sign for a fracture. Radiographs interpreted by the attending orthopaedic physician provided the standard for comparison of diagnostic findings.
Results:
Sensitivity was 0.83 (10∶12), specificity was 0.80 (20∶25), positive likelihood ratio was 4.2, negative likelihood ratio was 0.21, and diagnostic accuracy was 81% (30∶37).
Conclusions:
The tuning fork and stethoscope technique was an effective screening method for a variety of fractures.
Keywords: false-negative results, false-positive results, assessment, auscultation
Key Points
In the absence of immediate radiographic evaluation, identifying fractures can be difficult.
During a field evaluation, a tuning fork and stethoscope can be useful in evaluating potential fractures. However, this method should only be used in conjunction with a thorough assessment and sound clinical judgment.
Injury evaluation is a central component of clinical practice for athletic trainers. Through interviews, observation, and the completion of special tests, the extent of many injuries can be determined and decisions made regarding referral and treatment plans. However, identifying fractures in the absence of radiographic evaluation represents a unique challenge. Percussion and squeeze tests,1–4 which elicit pain indicative of a fracture, have been recommended. Yet the findings on these tests can be affected by individual pain tolerances, leading to false-negative or false-positive results.
Research on fracture testing in the athletic training literature is limited.2 Percussion with auscultation has been presented as a means of identifying fractures.5–9 Carter9 used percussion and a stethoscope to examine possible fractures and found that the sound produced by percussion in the injured body part was reduced in “pitch and volume” when compared with the uninjured body part. Colwell and Berg7 used percussion and a stethoscope to evaluate patients for clavicle, femur, tibia, and fibula fractures, reporting a success rate of 88%. Misurya et al5 showed that a tuning fork and a pediatric stethoscope allowed fractures to be detected in 94% of patients. Other authors6–9 have noted favorable results when using auscultation for detecting fractures. In particular, Misurya et al5 and Bache and Cross6 used a stethoscope and tuning fork in diagnosing fractures of the tibia and femoral neck and shaft. Bache and Cross6 reported 87% accuracy in detecting femoral neck fractures.
My purpose was to assess the diagnostic accuracy of a tuning fork and stethoscope technique in detecting fractures in patients presented to an athletic training room and orthopaedic clinic.
METHODS
Participants
All adult patients were informed of the testing procedure before they signed a University Institutional Review Board consent form; the Board also approved the study. Each minor provided assent, and the parent or guardian gave consent. Participants (19 males, 18 females) included children, adolescents, collegiate athletes, and older, more sedentary adults (age range, 7–60 years) who were being evaluated for extremity fractures during the data collection period.
I chose to perform the tuning fork test on patients with possible fractures that were less than 7 days old. Growth factors from platelets and cells begin to form new blood vessels in the injured area within 7 to 21 days.10 After 7 days, the bony surface may have begun to heal and close (K. Donnelly, written communication, November 1996). Such healing could affect the results of the tuning fork assessment.
Instruments
Three instruments were used in this study. A 128-Hz tuning fork (Moore Medical LLC, Farmington, CT) was used along with the conical bell of a standard stethoscope (Medco Sports Medicine, Tonawonda, NY). The x-ray machine (Multix C; Siemens, Munich, Germany) was calibrated throughout the study by Physics Associates (Radford, VA). Radiologic examinations were performed and interpreted at a local orthopaedic center in southwest Virginia.
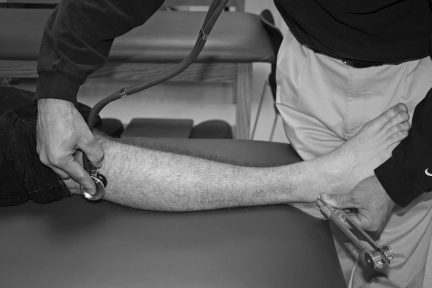
Procedures
The author administered the tuning fork test to all participants. The procedure was conducted as described by Misurya et al,6 except that the conical bell of a stethoscope was used instead of a pediatric stethoscope. The test was performed on the uninjured limb first. The tuning fork was placed on the bone distal to the suspected fracture, and the stethoscope's conical bell was placed proximal to the injury site on the same bone. I struck the tuning fork against a rubber pad and then placed the vibrating tuning fork on the bone distal to the injury site. I then listened to the sound arising from the bone via the stethoscope for approximately 6 to 8 seconds. I listened for a clear tone created by the tuning fork in the uninjured bone and compared it with the sound arising from the injured bone. For example, if the fibula was the injured bone, the vibrating tuning fork was placed on the distal tip of the lateral malleolus and the stethoscope's conical bell was placed on the fibular head (Figure). Diminished or absent sound from the injured limb as compared with the uninjured limb constituted a positive result. After the test, radiographs were taken and interpreted by the attending orthopaedic physician to confirm or rule out the presence of a fracture.
Figure. If the fibula was the injured bone, the vibrating tuning fork was placed on the distal tip of the lateral malleolus and the conical bell of a stethoscope was placed on the fibular head.
If a fracture was suspected in the phalanges of the hand, the tuning fork was placed on the tip of the phalange, and the conical bell of the stethoscope was placed at the metacarpal-phalangeal joint. The entire phalange was tested, which included the distal and proximal interphalangeal joints.
With institutional review board approval, I used an alternate method for patients with substantial swelling. The tuning fork was placed over the proximal bone, away from the swelling, and the stethoscope was placed over the swelling. Otherwise, I followed the procedure previously described.
For data analysis, I calculated sensitivity, specificity, positive and negative likelihood ratios, and diagnostic accuracy.
RESULTS
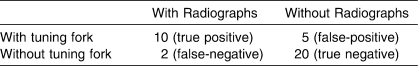
Among the 37 patients examined, radiographs confirmed the tuning fork assessment of fracture in 10; 20 true negative results were also confirmed. False-positive results occurred in 5 patients and false-negative results in 2 (Table 1). The tuning fork evaluation method was highly successful in detecting transverse fractures (n = 10) but not avulsion (n = 1) or buckle (n = 1) fractures. The 2 false-negative results occurred in patients with the avulsion and buckle fractures. (The avulsion fracture was to the 5th metatarsal; the buckle fracture was to the clavicle.)
Table 1.
Fracture Assessment Outcomes Using the Tuning Fork Test and Radiographs
Data analysis revealed sensitivity of 0.83 (10∶12), specificity of 0.80 (20∶25), positive likelihood ratio (+LR) of 4.2, negative likelihood ratio (−LR) of 0.21, and diagnostic accuracy of 81% (30∶37).
When the tuning fork assessment was modified so that the stethoscope was placed over the area of swelling, sensitivity remained at 0.83, but specificity increased to 0.92 (23∶25), with the +LR at 10.4, −LR at 0.18, and diagnostic accuracy at 89% (33∶37). Jaeschke et al11 suggested that positive examination findings on tests with a +LR exceeding 10 result in large, often conclusive shifts in the probability that the condition of interest exists. A negative examination finding on a test with a −LR of 0.1 to 0.2 provides a moderate shift in the probability that the condition is absent.
DISCUSSION
The tuning fork evaluation method was highly successful on transverse fractures (n = 10) but not as accurate on avulsion (n = 1) and buckle (n = 1) type fractures. In a transverse fracture, space created by the fracture is sufficient1,3,4 to decrease the sound the tuning fork produces and, thus, the sound is diminished as compared with the uninjured body part, resulting in a positive test.5–7 In a complete fracture, sound conduction is interrupted by the separated cortical surfaces of the bone.7 Avulsion and buckle fractures, by definition, leave the bone injured but intact and, therefore, sound is not commonly affected.1,3,4 Misurya et al5 and Bache and Cross6 explained that sound waves from the tuning fork are transmitted easily in non-transverse fractures because enough of the bone remains in contact. The only false-negative results that were identified occurred in patients with avulsion and buckle fractures.
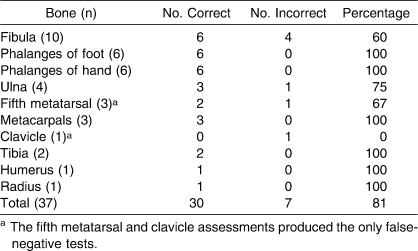
These results are in agreement with those of Misurya et al,5 Bache and Cross,6 Colwell and Berg,7 and Peltier8 in supporting the tuning fork test as a useful aid in identifying fractures. In my patients, the assessment was correct 81% of the time (30∶37), compared with the correct assessments of Misurya et al5 (94%) and Bache and Cross6 (87%). Both of the latter groups identified only the injured bone but not the fracture type. This study differed from the studies of Misurya et al5 and Bache and Cross6 because of the variety of bones examined. The earlier authors assessed fractures of the femoral neck, femoral shaft, and tibia.5–8 My results suggest that the tuning fork technique is useful across a broader range of bones than previously noted, including the extremities and the clavicle (Table 2).
Table 2.
Accuracy of the Tuning Fork Test in Fracture Assessment
The tuning fork technique appears to be an inexpensive and accurate method of evaluating possible fractures and could supplement the fracture testing techniques used by athletic trainers. In addition, it may be possible to reduce both the number of radiographs needed and the associated cost.
The Ottawa Ankle Rules (OAR) are very sensitive and, thus, effective in ruling out possible fractures of the foot and ankle.12–16 Adding tuning fork testing enhances the specificity of the OAR.12 My results also suggest that tuning fork assessment improves the specificity of fracture assessment in the absence of radiographs. In examining possible fractures of the ankle and foot, I recommend incorporating the tuning fork technique into the traditional fracture evaluation with the OAR. If multiple clinical assessment techniques are used, the likelihood of detecting a fracture while avoiding unnecessary radiographic examinations is greater. The OAR, however, apply only to ankle and foot injuries.
Previous researchers5–8 did not address the effect of swelling on the tuning fork and stethoscope method. Swelling within a tissue or a joint may alter results. When possible, the tuning fork test should be performed before swelling occurs. I placed the tuning fork distal and the stethoscope proximal to the suspected fracture. If swelling was present, the tuning fork was placed over the edema. Placing the stethoscope over the swelling (distally) and applying the tuning fork proximally allows the tuning fork to make contact with the bone and permits sounds to be transmitted along the bone. When the 3 patients with substantial swelling about the fibula were evaluated with this alternative method, there were 3 fewer false-positives (these results were not included in the data analysis). However, results of the radiographs were already known at the time of the modified examination procedure.
CONCLUSIONS
The tuning fork test is an acceptable method for identifying fractures when radiography is not immediately available. The test is easy, painless, and inexpensive to perform, and it can be administered quickly. It can be a useful tool for field evaluations. However, the tuning fork and stethoscope fracture testing method cannot and should not be used alone when a fracture is suspected. Thorough evaluation and sound clinical judgment are essential when making the decision to refer a patient for a full radiologic examination and diagnosis by a physician or to return an athlete to play.
Acknowledgments
I deeply appreciate the time and effort that Steve Ames, PhD, and other professors in the Department of Physical and Health Education put into this study. A special thank you is extended to Ms. Jackie Clouse-Snell of the Radford University Athletic Training Room and all the participants in the study. Finally thanks go to the Radford Orthopedic Center in Radford, VA, and especially Dr Ken Gray, Dr Kerry Donnelly, Ms. Karen Akers, and Mrs. Ruth Clark.
Footnotes
Michael Bryan Moore, PhD, VATL, ATC, provided conception and design; acquisition and analysis and interpretation of the data; and drafting, critical revision, and final approval of the article.
REFERENCES
- 1.Anderson M.K. Fundamentals of Sport Injury Management. 2nd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2003. pp. 55–58. [Google Scholar]
- 2.Kazemi M. Tuning fork test utilization in detection of fractures: a review of the literature. J Can Chiropract Assoc. 1999;43(2):120–124. [Google Scholar]
- 3.Prentice W.E. Arnheim's Principles of Athletic Training: A Competency-Based Approach. 12th ed. Boston, MA: McGraw Hill; 2006. p. 570. [Google Scholar]
- 4.Starkey C, Ryan J.L. Evaluation of Orthopedic and Athletic Injuries. 2nd ed. Philadelphia, PA: FA Davis; 2002. p. 183. [Google Scholar]
- 5.Misurya R.K, Khare A, Mallick A, Sural A, Vishwakarma G.K. Use of tuning fork in diagnostic auscultation of fractures. Injury. 1987;18(1):63–64. doi: 10.1016/0020-1383(87)90391-3. [DOI] [PubMed] [Google Scholar]
- 6.Bache J.B, Cross A.B. The Barford test: useful diagnostic sign in fractures of the femoral neck. Practitioner. 1984;228(1839):305–308. [PubMed] [Google Scholar]
- 7.Colwell J.C, Berg E.H. Auscultation as an important aid to the diagnosis of fractures. Surg Gynecol Obstet. 1958;106:713–714. [PubMed] [Google Scholar]
- 8.Peltier L.F. The diagnosis of fractures of the hip and femur by auscultatory percussion. Clin Orthop Rel Res. 1977;123:9–11. [PubMed] [Google Scholar]
- 9.Carter M.C. A reliable sign of fractures of the hip or pelvis. New Engl J Med. 1981;305(20):1220. doi: 10.1056/NEJM198111123052015. [DOI] [PubMed] [Google Scholar]
- 10.Mourad L. Orthopaedic Nursing. New York, NY: Delmar Publishers; 1994. pp. 19–20. [Google Scholar]
- 11.Jaeschke R, Guyatt J.H, Sackett D.L. User's guide to the medical literature, III: how to use an article about a diagnostic test? B: What are the results and will they help me in caring for my patient? The Evidence-Based Medicine Working Group. JAMA. 1994;271(9):703–707. doi: 10.1001/jama.271.9.703. [DOI] [PubMed] [Google Scholar]
- 12.Dissmann P.D, Han K.H. The tuning fork test: a useful tool for improving specificity in “Ottawa positive” patients after ankle inversion injury. Emerg Med J. 2006;23(10):788–790. doi: 10.1136/emj.2006.035519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Northrup R.L, Ragan B.G, Bell G.W. The Ottawa ankle rules and the “Buffalo” rule, part 1: overview and background. Athl Ther Today. 2005;10(1):56–59. [Google Scholar]
- 14.Northrup R.L, Ragan B.G, Bell G.W. The Ottawa ankle rules and the “Buffalo” rule, part 2: a practical application. Athl Ther Today. 2005;10(2):68–71. [Google Scholar]
- 15.Bachmann L.M, Kolb E, Koller M.T, Steurer J, ter Riet G. Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot: systemic review. BMJ. 2003;326(7386):417–423. doi: 10.1136/bmj.326.7386.417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lucchesi G.M, Jackson R.E, Peacock W.F, Cerasani C, Swor R.A. Sensitivity of the Ottawa rules. Ann Emerg Med. 1995;26(1):1–5. doi: 10.1016/s0196-0644(95)70229-6. [DOI] [PubMed] [Google Scholar]