Abstract
Context:
For some time, educators have advised clinical instructors (CIs) to capture the elusive teachable moment in clinical education. However, a universal definition of a teachable moment does not exist. Without a clear understanding of this concept, CIs and athletic training students (ATSs) may have difficulty facilitating the teachable moment.
Objective:
To recognize and define a teachable moment as it relates to the athletic training clinical education setting and to identify potential barriers to creating the teachable moment.
Design:
Mixed-methods design employing grounded theory and quantitative analysis.
Setting:
Collegiate sports medicine clinic affiliated with a Commission on Accreditation of Allied Health Education Programs–accredited athletic training education program.
Patients or Other Participants:
11 CIs (6 men, 5 women) and 11 ATSs (3 men, 8 women).
Data Collection and Analysis:
Participants completed a teachable moment questionnaire to define and identify teachable moments. Follow-up semistructured interviews were conducted after data collection. A qualitative analysis was conducted on responses using open, axial, and selective coding. Member checking was conducted to establish trustworthiness. Qualitative data were quantified to descriptively report the findings.
Results:
Engaged clinical experiences were the overarching theme. Three major themes that defined a teachable moment emerged: (1) professional discourse about skills, techniques, research, and special cases; (2) authentic experience or actual hands-on experience; and (3) skill development or time for skill instruction, practice, role playing, and simulations. Participants reported 158 teachable moments (CIs = 75, ATSs = 83). Lack of time and other duties were examples of barriers hindering the teachable moment.
Conclusions:
The teachable moment occurs when a CI and an ATS actively participate and interact with each other to enhance learning and foster intellectual curiosity in the clinical education environment. An underlying barrier to the teachable moment is perceived to be the CI's day-to-day responsibilities.
Keywords: athletic training education, instructional strategies
Key Points
A teachable moment occurs when a clinical instructor and an athletic training student work together to enhance learning and foster intellectual curiosity in the clinical education environment.
Professional discourse, authentic experience, and skill development emerged as critical concepts illustrating the definition of a teachable moment and are strategies to keep athletic training students engaged in clinical experiences.
The daily responsibilities of the clinical instructor are perceived barriers to the teachable moment.
The clinical instructors and athletic training students recognized identical situations as teachable moments only 22% of the time.
Participants became increasingly aware of and actively sought out teachable moments.
The clinical education component in the preparation of medical professionals is perhaps the most critical.1 Athletic training education programs (ATEPs) across the United States rely heavily on clinical education to function as a bridge from classroom knowledge to clinical practice and to allow athletic training students (ATSs) to perform psychomotor skills under supervision.2–4 The role of the clinical instructor (CI) is crucial to the professional development of the ATS.4 The CI “should be aware of the topics that are being covered in the classroom in order to recognize ‘teachable moments’ in the clinical setting that will build on theoretical knowledge.”1
A teachable moment is a multifaceted construct that is conceptually abstract and difficult to define. Several descriptions or references to teachable moments exist. Leist and Kristofco5 described the teachable moment as a time when an individual is ready to learn and accept new information. Furthermore, the teachable moment requires the educator to respond to inquiry on the spot. Teachable moments have been described in early childhood education as a means for students and teachers to learn from each other in highly connected teaching and learning communities.6 Rea7 referenced the phenomenon of a teachable moment when teaching science. If a student brings in an unusual rock to science class, then the teacher can model curiosity by exploring and relating the student's rock to current scientific concepts.7 A “seize-the-day” approach entails responding to a student's question or relating events to a news story containing a scientific concept, thus capturing the essence of a teachable moment.8
In the medical literature, the teachable moment is described as a naturally occurring health event (eg, disease diagnosis) that may be used as a motivational tactic to encourage the patient to modify behavior (eg, smoking cessation).9 Patient education is another area of emphasis on capturing the teachable moment.10 This is described as any time during a visit to a physician that the physician or other health care provider is willing to answer questions or teach new skills to a patient (eg, use of an inhaler).10 Nursing education defines the teachable moment as the ability of the instructor to recognize the educational priorities of the student and facilitate learning into practice.11 Using systematic reviews (comprehensive summaries found in established databases) can help medical residents capture teachable moments during clinical practice. If an attending physician asks a medical resident about a specific treatment, the resident can access the most recent literature quickly to help make decisions regarding patient care.12 Furthermore, Buyck and Lang13 explained that teachable moments warrant instructional intervention to modify or reinforce a skill.
In the athletic training literature, very little information exists regarding the teachable moment. However, several references to teachable moments are made. Hutsick14 stated that one of the explicit roles of clinical education is to seize the teachable moment. She also stated that, for ATSs, authentic experiences tend to be more memorable than simulated experiences. Wagner15 developed a plan for capturing teachable moments in which athletic training CIs complete weekly modules (scenarios) to increase knowledge and retention of clinical education concepts. Geisler and Parker16 described teachable moments as part of each student's clinical education plans. These teachable moments are clinical learning opportunities that may include providing the ATS with real-world experiences, discussions about theory and praxis, opportunities for reviewing previously learned concepts, and opportunities for learning alternative approaches.16
Although the teachable moment has been described in medical,9,10,12 nursing,11 and education5–8 disciplines and is frequently referred to in athletic training, a universal definition of a teachable moment does not exist. As such, instructors or students may have difficulty recognizing a teachable moment when it occurs. Thus, the purpose of my investigation was 3-fold: (1) to describe the emergent definition of a teachable moment from the perspective of CIs and ATSs, (2) to explore whether CIs and ATSs identified similar experiences when teachable moments occurred, and (3) to identify potential barriers to creating the teachable moment.
METHODS
Participants and Setting
A convenience-sampling technique was used to recruit participants from 1 large Southern, metropolitan, Carnegie-designated very high research activity university.17–19 The study was conducted at a collegiate sports medicine facility that served as a clinical education site for undergraduate ATSs. All participants recruited for participation were affiliated with the same ATEP, which was accredited by the Commission on Accreditation of Allied Health Education Programs. The first group of participants comprised CIs from the sports medicine facility. The second group of participants consisted of ATSs currently enrolled in an ATEP. Through an e-mail sent to the CIs working in the collegiate sports medicine facility, I recruited a sample of 11 CIs (6 men, 5 women). On average, the CIs participating in this study had been certified by the Board of Certification for 2.8 years (range, 0.5–11.0 years). The CIs had an average of 1.3 years' (range, 0.5–4.0 years) experience as CIs and an average of 1 year (range, 0–3 years) of teaching experience. Seven CIs participating in this study were Approved Clinical Instructors.
After the CIs agreed to be involved in the study, I sent an e-mail to ATSs currently assigned to these CIs and requested their participation in the study. As a result, 11 ATSs (3 men, 8 women) in the undergraduate ATEP completing clinical education experiences in the sports medicine clinic agreed to participate. Most of the ATSs (n = 6) were in their second year of the professional program, so most were upper-level students. The CIs were paired with their assigned ATSs, and they completed the study for a 1-week period in either the spring or the fall of 2005.
All participants provided informed consent. This study was approved by the Institutional Review Board at the University of South Florida.
Design
I used a dominant-status concurrent design.20 Data collection was both qualitative (dominant status) and quantitative in nature. The first phase of data analysis was conducted using qualitative inquiry; the second phase was quantitative. During data collection, I used the qualitative paradigm to explore the data collected for defining and recognizing a teachable moment. My study was designed to provide initial insight into and understanding of the teachable moment. To understand the phenomena being studied, I used a grounded theory approach, which is deemed appropriate when no hypothesis is set a priori.21
In this study, I gave more emphasis (dominant status) to the qualitative paradigm because of the predominantly open-ended format of the teachable moment questionnaire (TMQ) used. Qualitative analysis (open, axial, and selective coding) was conducted before the quantitative analysis (calculation of frequencies and percentages) of the qualitative results.18 In this phase, qualitative themes are numerically represented to interpret a target phenomenon.21 The purpose for this design was complementarity, which helps the researcher illustrate and clarify the results from one method (qualitative in my study) with results from the other method (quantitative).18 This allowed me to describe the emergent themes in my study and to clearly depict the frequency in which these themes were perceived to occur.
Instrumentation
Using existing literature referencing teachable moments in medical education,11,13 I developed a TMQ that included both open-ended and closed-ended questions. The purpose of the TMQ was to ask both CIs and ATSs to define a teachable moment from their perspectives, to state how many teachable moments were perceived in a given clinical experience, and to identify any barriers that prevented a teachable moment from occurring. After the TMQ was developed, a panel of 14 experts reviewed the questionnaire. The panel consisted of a sample of athletic trainers, ATSs, and educators. One expert had considerable experience in survey development and mixed methodologies. The panels were instructed to provide feedback regarding readability, clarity, and completion time of the questionnaire. When the feedback was obtained, I made minor adjustments to the wording and prepared the TMQ for distribution to the study participants.
The TMQ was designed to guide the participants in their exploration of defining teachable moments and identifying barriers that prevent teachable moments from occurring. The first phase of the TMQ collected information on the education and professional background of the CIs and ATSs, such as teaching experience, CI experience, years certified, work setting, and length in an ATEP. During the first phase of the TMQ, participants also defined a teachable moment based on their perceptions. The second phase of the TMQ, which consisted of 7 daily logs, contained closed-ended questions, including perceived frequency of occurrence of teachable moments during daily clinical experience, duration of time spent in clinical experience, and percentage of time spent interacting with a CI or ATS during the clinical experience. The daily log also contained open-ended questions asking participants to briefly describe teachable moments that occurred during clinical experiences that day and to document whether any barriers may have prevented the ATS or CI from initiating or responding to teachable moments.
Procedures
I met with each participant before beginning the study to explain the procedures and to provide an instruction sheet outlining the research protocol. Rather than assigning pseudonyms, I assigned a code to each ATS and CI pair (eg, ATS1 was paired with CI1, ATS2 was paired with CI2). This code corresponded with the code labeled on the TMQ provided to participants. Participants completed the first phase of the TMQ before completing the daily logs. On the TMQ, the CIs and ATSs documented their experiences of perceived teachable moments while completing their clinical experience for 1 week (same week for each paired CI and ATS). After each day of clinical experience, each participant was instructed to complete the daily log provided in the TMQ. Participants were instructed not to discuss their documented teachable moments with each other during the study period. At the end of the study period, the TMQs were collected for data analysis.
Within 2 weeks of the data collection period, participants met with me for member checking of the data collected from the TMQ and for a follow-up interview. The TMQ data were reviewed, transcribed, and transferred to an Excel (2007 version; Microsoft Corp, Redmond, WA) spreadsheet. During the follow-up meeting, participants first reviewed their transcribed responses from the TMQ to ensure accuracy. Common themes from the initial analysis were discussed with the participants. Immediately after member checking, I conducted a semistructured interview. Each interview lasted approximately 30 minutes and was not recorded audiovisually. However, I typed responses into an Excel spreadsheet. The questions for the follow-up interview were reflective in nature, allowing participants to consider their initial definition of a teachable moment (Table 1). Participants could add more thoughts to their definitions. Additionally, participants were instructed to identify whether one teachable moment stood out in their minds and to describe that teachable moment. They were also instructed to identify whom they felt was more likely to initiate or respond to teachable moments, to identify whether they thought teachable moments occurred yet went unnoticed, and to reflect upon the effect of participating in this study. Participants were allowed to review their responses from the interviews to ensure that data transcriptions were accurate.
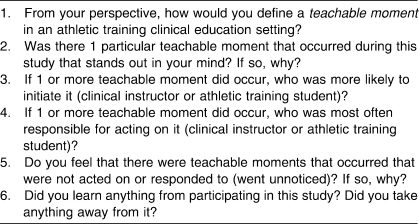
Table 1.
Semistructured Follow-Up Interview Questions
Data Analysis
After all participants completed the TMQ and follow-up interviews, qualitative analyses of all TMQ open-ended responses and the semistructured interviews were completed using a grounded theory approach. Open coding, which entails reading transcripts and categorizing elements of the data, was completed initially to define common experiences qualifying as teachable moments.18,22 Axial coding and selective coding were completed as described by Creswell.17 With axial coding, I grouped key concepts into categories.23 Selective coding was used to integrate key concepts into an overarching theme.21 Constant comparative analysis was conducted throughout the coding stages to compare the experiences of a teachable moment from an ATS's perspective with those from a CI's perspective.24 Data collection took place until theoretical saturation was achieved.17,18 The coding scheme that I identified was verified by an outside researcher who was not directly involved in the project.
Upon completion of the qualitative analysis, identified themes were quantitized, which is a method of translating qualitative data to numerical form.25 Obtaining counts of each theme identified in qualitative analysis prevented me from overweighting or underweighting the prevalence of a particular theme.18,25 Frequencies and percentages were calculated for each theme to clearly illustrate the prevalence of each theme. Representing the themes in numerical form allowed for ease of comparison between perceived recognition of teachable moments by CIs and ATSs and between perceived barriers to initiating or responding to teachable moments. Means and SDs were calculated for perceived frequency of occurrence of teachable moments during daily clinical experience, duration of time spent in clinical experience, and percentage of time spent interacting with a CI during the clinical experience.
Three techniques were used to establish trustworthiness of data collection and analysis. First, member checks were conducted with each of the participants to ensure accuracy of the data collected.26 Second, peer debriefing was completed by an outside researcher to review the coding scheme.26 This individual was a professor in the college of education who had extensive training in qualitative methods. As noted, the outside reviewer agreed with the coding scheme. Third, triangulation of data occurred through the use of multiple data sources.26 These data sources included the completed questionnaires, interviews of CIs, and interviews of ATSs. Using multiple perspectives (CI and ATS) allowed me to collect thick, rich data to provide an accurate analysis of the data.
RESULTS
Number of Perceived Teachable Moments
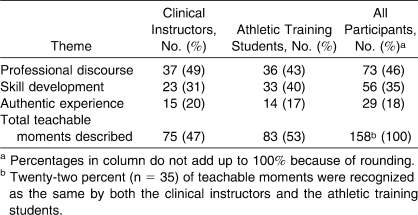
The total time of clinical experiences for all ATSs (n = 11) was 229.5 hours in a 1-week period. The average length of each clinical experience was 5 hours (range, 2.5–8.5 hours). Each student averaged 20.0 ± 2.6 hours of clinical experience during the study. The CIs and ATSs identified 158 teachable moments during this period. Collectively, CIs reported an average of 18 (range, 14–24) teachable moments per day, and ATSs reported an average of 19 (range, 13–24) per day. Table 2 illustrates the frequency of each description provided by the participants.
Table 2.
Frequency of Perceived Teachable Moments by Participants
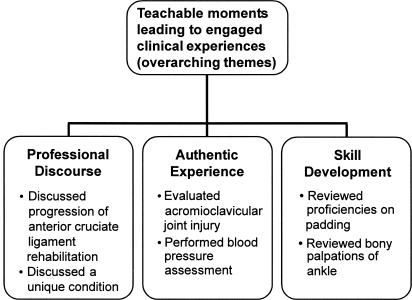
Definition of a Teachable Moment
Based on the information gathered and analyzed herein, the teachable moment was defined as occurring when a CI and ATS actively participate and interact with each other to enhance learning and foster intellectual curiosity in the clinical education environment. Three major themes emerged and clearly supported this definition: professional discourse, authentic experience, and skill development. I discuss each of these themes in detail. During the selective coding process, the integration of these themes led to an overarching theme of engaged clinical experiences. Professional discourse, authentic experience, and skill development are integral components of the teachable moment that keep students engaged in clinical experiences (Figure 1).
Figure 1. Conceptual framework from analyzed qualitative data: engaged clinical experiences.
Professional Discourse
When describing teachable moments, the first theme identified was professional discourse. From these data, professional discourse refers to discussions or conversations that took place between the CI and ATS and were related to clinical practice. Forty-six percent of the identified teachable moments were related to this theme. The CIs and ATSs recognized discussion about current research, special cases, or new techniques as a teachable moment. Using downtime to discuss injury situations and how they are handled, whether real or contrived, was a common example that the participants provided. The CIs described a teachable moment in the following ways:
The moment that the student is seeing something new for the first time, and there is an opportunity to explain and educate the student. (CI1)
The time after which something has happened that the ATS has seen in which questions can be answered and thoughts and ideas expressed to help the ATS gain better knowledge about what went on. (CI7)
Students described a teachable moment in the following ways:
A teachable moment is the exchange of knowledge between CIs and their students. The knowledge exchanged increases or clarifies misunderstood concepts. This includes hands-on demonstrations as well. (ATS1)
A period of time that an ATC [certified athletic trainer] and an ATS can spend discussing an injury, rehab plan, or any other aspect of AT [athletic training]. This can either be a brief explanation from the ATC or an actual discussion between 2 people. (ATS7)
Examples provided by CIs that illustrate professional discourse included
One of my athletes has a unique condition; we talked about it, I showed her an article about it and explained the test the athlete is going to have on Friday to hopefully find the diagnosis. (CI1)
My student asked questions regarding an injury situation with a soccer player. (CI7)
The moment the student and I can talk about different topics and toss back and forth different ideas. (CI10)
The ATSs provided the following examples that illustrate professional discourse:
At practice we talked about classes and organization and future plans after graduating. (ATS2)
My [CI] and I can discuss treatments, injuries, and events that pertain to athletic training and can further my knowledge in the field. (ATS8)
[CI] discussed patella subluxation treatment and rehab for one of the athletes. (ATS11)
Authentic Experience
The second theme describing teachable moments was authentic experience, in which the ATS was actually able to gain hands-on experience either in the athletic training facility or on the field. Eighteen percent of all teachable moments identified in this study composed this theme. These experiences were not contrived; they were opportunities for the ATS to interact with the athletes either in an emergent situation on the field or in the performance of clinical athletic training skills in the athletic training room. Several students described opportunities, such as helping to design a rehabilitation program, taking athletes through the plan, and performing injury evaluations, as authentic experiences. One ATS's description included the following:
Specifically, a teachable moment can't be simulated in a classroom. Specific evaluations and examinations on athletes, rehabilitation methods, on-the-field situations and emergencies, as well as learning how to deal with the politics of sports and the different situations that may arise. (ATS5)
Examples provided by participants included
I evaluated an AC [acromioclavicular joint] injury on the field. (ATS9)
I learned how to perform a blood pressure assessment on an athlete with elevated blood pressure. (ATS5)
An athlete was injured at practice on the field and after practice, the ATC [certified athletic trainer] asked me to evaluate him. (ATS3)
Had my student perform a full neck evaluation on an athlete. (CI6)
Allowed my student to conduct a shoulder evaluation on an athlete and discussed findings afterwards. (CI9)
Skill Development
The last theme describing teachable moments was skill development, whereby the CIs provided the ATSs with skill instruction and with skill practice through role playing and injury simulations. In this study, whether the CI was demonstrating new skills for the students or simply allowing the students to work on skills previously learned in the classroom, both the CI and the ATS recognized that these were favorable times for learning. Thirty-five percent of teachable moments identified in this study were skill development. Statements supporting this theme included
We went over and practiced special tests of the wrist and hand. (CI1)
Student reviewed various proficiencies on padding. (CI2)
Practiced taping ankles and techniques with student. (CI10)
We reviewed palpation for the wrist and he asked me different questions about the anatomy of the wrist. (ATS4)
We reviewed bony and soft tissue palpation for the foot and ankle. (ATS6)
Reviewed and practiced taping ankles. (ATS11)
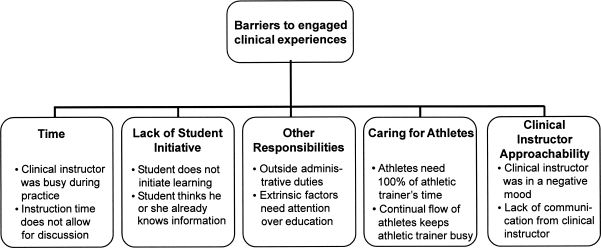
Barriers Perceived to Prevent Initiating a Teachable Moment
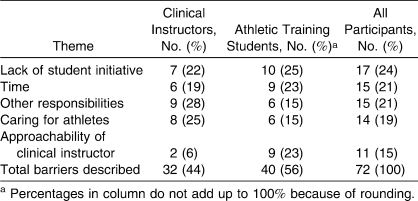
When a participant perceived a teachable moment, he or she was faced with the decision either to initiate the teachable moment through action or discussion or to dismiss the learning opportunity. On the TMQ, participants identified 72 (CIs = 32, ATSs = 40) barriers that may prevent one from initiating a teachable moment (Figure 2). Table 3 illustrates the 5 major themes of barriers identified.
Figure 2. Barriers to engaged clinical experiences.
Table 3.
Barriers Perceived to Prevent Initiating a Teachable Moment
Barriers Perceived by CIs
The CIs noted that the most predominant barrier to initiating a teachable moment was performing other responsibilities (28%), followed closely by caring for athletes (25%) and lack of student initiative (22%). The barrier of other responsibilities implied that other job responsibilities demanded the attention of the CI and did not allow him or her to focus on capturing the teachable moment. This barrier was supported by CI statements:
If I am doing other duties that must be done in the athletic training room to keep it functioning properly. (CI1)
Outside administrative influence. (CI3)
Extrinsic factors needing attention over education. (CI4)
The second most common barrier identified by CIs was caring for athletes. Examples included
When athletes need 100% of my time. (CI1)
Continual flow of athletes keeping me busy. (CI2)
Restricted time due to number of athletes. (CI11)
The third most common barrier was lack of student initiative. Clinical instructors felt that the ATSs were not committed to learning at that particular time or were not motivated to take advantage of a learning opportunity. Comments supporting this theme included the following:
When the student does not ask any questions or take any initiative. (CI1)
Student does not initiate the learning. (CI8)
Student thinks they know the information already. (CI10)
Barriers Perceived by ATSs
Interestingly, for the ATSs, the most commonly perceived barrier preventing the initiation of a teachable moment was lack of student initiative (25%), followed by time (23%) and approachability of CI (23%). Lack of student initiative was illustrated by the following statement:
I don't feel like going over proficiencies today. (ATS2)
Time was a prominent barrier illustrated by the following students' statements:
I don't want to interfere or take up too much of my [CI's] time. (ATS4)
[CI] is too busy during practice. (ATS5)
Time does not allow for discussion. (ATS6)
Often, the ATSs noted that the CIs had little time to answer questions or to discuss an injury. Approachability of CI was another common barrier identified by the students. The CI's mood or personality seemed to be an influential factor in determining the experiences of the ATSs during their assigned clinical experiences. This was supported by comments such as
[CI] may be in a negative mood. (ATS1)
I felt uncomfortable with my [CI]. (ATS6)
Lack of communication by [CI]. (ATS10)
In the follow-up interviews, 45% (n = 10) of all participants expressed that the ATS was more likely to initiate a teachable moment. However, 32% (n = 7) of all participants thought that the CI and the ATS were equally likely to initiate the teachable moment, and 23% (n = 5) felt that the CI was more likely to initiate a teachable moment.
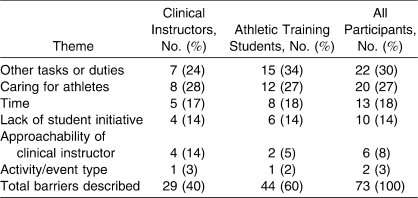
Barriers Perceived to Prevent a Response to a Teachable Moment
When the teachable moment is identified, the CI or ATS can either take advantage of or ignore the learning opportunity. For example, if a student recognizes the opportunity to try a new skill (identifies the teachable moment) and asks his or her CI for the opportunity to act, the CI can respond in 1 of 2 ways. This response may be to facilitate the teachable moment by encouraging the student to try the new skill or to prevent the teachable moment from occurring because of other circumstances or barriers. Similar to the perceived barriers to initiating a teachable moment, participants identified 73 (CIs = 29, ATSs = 44) barriers preventing a response to a teachable moment. Table 4 highlights the frequency of the 6 major themes of barriers identified.
Table 4.
Barriers Perceived to Prevent a Response to a Teachable Moment
Overall, 9 participants (41%) felt that the CI was more likely to be responsible for acting on the teachable moment; however, 9 participants (41%) also felt that the CI and ATS were equally likely to act on the identified teachable moment. If an equal opportunity exists for the teachable moment to be created, then these results underscore the importance of the ATS taking ownership in his or her clinical education by seeking out educational opportunities. Only 4 participants (18%) felt that the ATS would be more likely to be responsible for acting on the teachable moment.
Barriers Perceived by CIs
The CIs identified caring for athletes (28%), other tasks or duties (24%), and time (17%) as the top 3 barriers preventing a response to a teachable moment. The CIs recognized that their duties to provide injury care or rehabilitation took precedence over responding to the teachable moment. Their examples that illustrate caring for athletes included
When I am concentrating on my athletes. (CI1)
Presence of an athlete would delay teachable moment response pending situation/extent of injury. (CI2)
The barrier other tasks or duties relates to other responsibilities that the CI may have that interfere with his or her ability to respond to the teachable moment. The CIs noted
Outside administrative influence. (CI3)
Completing other tasks that need to be done. (CI6)
The CIs identified time as the third most common barrier that prevented a response to the teachable moment. They felt that, at times, they were “too busy” or did not have “enough time” to respond to the teachable moment.
Barriers Perceived by ATSs
Similarly, the ATSs recognized other tasks or duties (34%), caring for athletes (27%), and time (18%) as barriers preventing a response to a teachable moment. Lack of student initiative, approachability of CI, and activity/event type were other common barriers identified by the ATSs. A statement illustrating lack of student initiative included
I don't feel like going over proficiencies today. (ATS2)
The barrier of approachability of CI was noted by the ATSs:
If I felt someone would not listen or looked busy, I would not approach them. (ATS1)
Personality characteristics of my [CI]—my [CI] is shy and quiet. (ATS5)
The last barrier preventing a response to the teachable moment was activity/event type. This relates to students or CIs serving sporting activities in the off-season or running light practices where the probability of injury is low. Statements corroborating this theme included
No contact at practice. (ATS3)
Out of season, not as much interaction with the athletes. (ATS5)
Standout Teachable Moments
In the follow-up interview, all participants were asked if one teachable moment stood out in their minds when compared with other teachable moments they described. Nineteen individuals identified standout teachable moments, whereas 3 did not perceive any of the teachable moments to be of special importance. Of those standout teachable moments identified, 9 were related to professional discourse, 7 were authentic experiences, and 3 were skill development. A CI and an ATS provided the following explanations when asked to recall whether one teachable moment stood out:
The eye injury—during the football scrimmage there was an eye injury and the eye swelled shut. I listened and watched [CI3] during the evaluation and got ice for the athlete. I had not seen this injury before. (ATS3)
We were able to watch films be taken with the fluoroscan on an athlete with a history of a tib-fib [tibia-fibula] ORIF [open reduction, internal fixation], and then explained to the student what the films showed and procedure. (CI5)
Discrepancies in Identifying Teachable Moments
Although both the CI and ATS recognized that teachable moments occur, they recognized identical situations as being a teachable moment only 22% (35 of 158) of the time. The following statements illustrate simultaneous recognition of a teachable moment by the CI and ATS:
I learned how to perform a blood pressure assessment on an athlete with elevated blood pressure. (ATS5)
Student was able to learn and perform blood pressure readings due to a circumstance with an athlete that was being seen by a physician for elevated blood pressure. (CI5)
My [CI] and I did rehab on an athlete and I could see what kind of rehab exercises you can do for an athlete with an ACL [anterior cruciate ligament] injury. (ATS4)
We discussed progression criterion for an ACL [anterior cruciate ligament] rehabilitation while working with the athlete. (CI4)
Of those 35 teachable moments identified by both the CI and the ATS, 16 (46%) were categorized as professional discourse, 15 (43%) were skill development, and 4 (11%) were authentic experiences.
Missed Teachable Moments and Raised Awareness
In the follow-up interviews, I asked participants if they felt it was possible that teachable moments were missed. Eighteen of the 22 (82%) individuals noted that teachable moments possibly were missed. Statements included
I spent a lot of time at doctor's offices today and may have missed an opportunity. (ATS9)
Most likely (teachable moments were missed) because of busyness or timing of situation. (CI4)
The potential reasons for missed teachable moments provided by the participants included lack of time (56%), lack of communication (28%), not recognizing a teachable moment (2%), and lack of motivation or initiative by either the CI or the ATS (1%). Statements supporting the reasons for missed teachable moments included
I was busy helping other players (ATS5) (lack of time);
Communication barrier between the [CI] and the student (CI10) (lack of communication);
I didn't realize when the teachable moment occurred. (CI8) (not recognizing a teachable moment); and
Motivation to work on skills by both [CI] and student lacked on certain days. (ATS2) (lack of motivation or initiative)
Nineteen of the 22 participants (86%) felt that this study raised their awareness of recognizing a teachable moment, and, after the study, all of the participants looked for teachable moments to occur. Two of the CIs stated the following:
When something would happen this week, I would look for [ATS3]. (CI3)
I would try to become more proactive in initiating a teachable moment. (CI4)
All of the ATSs stated that they would ask more questions in future clinical experiences and realized the potential for learning opportunities in a clinical setting. Statements corroborating this included
This study increased my awareness of different kinds of teachable moments. It forced reflection on what I have learned. I will try to ask more questions in the future. (ATS3)
I will keep a better eye out for it, take advantage of the opportunity and try not to be shy. (ATS5)
DISCUSSION
For some time, educators and CIs have been advised to capture the ever-elusive teachable moment, whether it occurs in the classroom or in a clinical education setting. The results from my study indicate that professional discourse, authentic experience, and skill development are critical concepts illustrating the definition of a teachable moment. A teachable moment occurs when a CI and an ATS actively participate and interact with each other to enhance learning and foster intellectual curiosity in the clinical education environment. In the process of defining the teachable moment, these participants noted an increased awareness of the teachable moment and actively sought out these moments. Teachable moments occur when ATSs are provided with hands-on opportunities, thereby enhancing clinical education.27 They allow students the opportunity to openly discuss specific cases, protocols, and current research, thus keeping students actively involved in their education. The results of this study emphasize the importance of interaction between the ATS and the CI during the clinical experience.4,28 A conceptual framework for facilitating engaged clinical experiences was created by integrating these concepts of a teachable moment (Figure 1). The 3 emergent descriptions of a teachable moment (professional discourse, authentic experience, and skill development) in this study are strategies to keep students engaged in clinical experiences. Often, these engaged clinical experiences lead to discussion and subsequent learning opportunities for the CI and ATS.
Engaged Clinical Experiences
The results of my study indicated 3 ways a teachable moment can keep ATSs involved in their clinical experience. The first way is through professional discourse. Most CIs and ATSs in my study agreed that taking time to discuss an issue pertinent to clinical education constituted a teachable moment. The underlying theme of professional discourse describing the teachable moment is the element of dialogue. Research in clinical education has indicated that the CI should possess effective communication skills and that these skills are essential in facilitating the teaching-learning exchange.4,28
Most standout teachable moments identified in my study were simply dialogue exchanges between the CI and the ATS. Again, this emphasizes the importance and necessity of communication and interaction between the CI and the ATS. This interaction is imperative in clinical education and is well supported not only in the athletic training literature3,4,28 but also in allied health education literature.29 In their survey of physical therapy CIs and students, Jarski et al30 revealed that communication skills, interpersonal skills, and the provision of information through discussion are considered essential behaviors of CIs.
As mentioned, clinical education is designed to supplement the student's classroom and laboratory instruction with real-life experience.4,16,31–34 Authentic experiences were identified as another means of keeping an ATS engaged in his or her clinical education. According to Hutsick,14 these authentic experiences tend to be more memorable experiences for the ATS. When ATSs were asked to identify a teachable moment that stood out during the week, some participants identified the authentic experience of treating a “live” athlete. However, authentic experiences identified by the CIs and ATSs occurred less frequently than professional discourse or time for skill development. Only 20% of the teachable moments identified in this study were authentic experiences. Thus, these authentic experiences seem to compose a very small segment of clinical education. Several factors that may have contributed to this finding include the small window of time that data were collected for this study, the time of year for the sport rotation (in-season versus off-season), and the skill level and competency of the ATS (lower-level ATSs may not be allowed to perform same skills as upper-level ATSs). When compared with other clinical education programs (eg, medical and nursing), clinical experiences appear to provide students with more real-life experiences. Medical students reported an average of 83 patient encounters (defined as taking a history and completing a physical examination) during a 6-week clerkship in family practice, 104 patient encounters during a 6-week pediatric clerkship, and 170 patient encounters during a 12-week internal medicine clerkship.35 Furthermore, virtually all the medical students recognized that constructive feedback played an integral role. Authors of several studies concur that the CI should be available to ATSs to suggest different ways of performing clinical proficiencies or positively reinforcing desired clinical skills.3,4,28
Although a large part of clinical education is based upon real-life experiences, an ATS will not always encounter all the experiences necessary to achieve entry-level competence.34 Rather, the CI is faced with the challenge of creating times for skill development, which is the third strategy identified to keep the ATS engaged in clinical experiences. My findings suggest that a large part of the interaction between the CI and the ATS occurs when the CI provides time for the ATS to practice skills or instruct a new skill. The ATSs recognized that time spent practicing skills while being supervised by their CIs was a valuable use of downtime in clinical rotations. Interestingly, the nursing, allied health, and medical education literature has not directly described skill development as a teachable moment. However, whether real or contrived, skills practice is essential to the development of the health care professional.11,13
Discrepancies in Identifying Teachable Moments
Regardless of the type of teachable moment identified, the results illustrate that CIs and ATSs do not always identify similar teachable moments. For instance, an ATS may point out that the CI engaged in discussion with the coach regarding an athlete's injury and playing status. The ATS saw this as a teachable moment because the CI was modeling desired professional behaviors (effective communication skills and professionalism) and the student learned how to interact appropriately with coaches. However, the CI may not document that discussion as a teachable moment, although ATSs and CIs have identified modeling professional behaviors as a helpful CI characteristic.4 Similarly, the CI may view one situation or circumstance as a teachable moment, whereas the ATS does not. Perhaps this discrepancy in identifying similar teachable moments is a function of experience. For example, the CI may believe that a specific skill or rehabilitation technique not taught in the classroom is valuable in clinical practice and takes time to explain that technique to an ATS. However, the ATS may not see that as a teachable moment simply because he or she does not fully understand or grasp the importance of that particular skill.
Perceived Barriers of Engaged Clinical Experience
The CIs and ATSs identified several barriers as preventing a response to or initiation of teachable moments. Common barriers cited included lack of time, caring for athletes, the CI performing other tasks or duties, lack of student initiative, and approachability of CI. With the exception of student initiative, the underlying barrier may be a function of the CI's day-to-day responsibilities. Weidner and Henning36 warned that the CI is encountering role strain because he or she serves as a clinician and as a clinical educator. Duties contributing to role strain for the CI encompassed communication skills, instructional skills, supervisory and administrative skills, and student performance evaluations.36 If the CI is attempting to juggle multiple tasks and duties simultaneously, he or she is likely to push aside efforts at initiating a teachable moment or taking time to respond to potential teachable moments.32
Often, these barriers prevent students from being engaged in meaningful clinical activities. Although all participants identified barriers, 45% of the participants felt the ATS was more likely to initiate the teachable moment. This result is not surprising because most of the participants felt it was the ATS's responsibility to take initiative to learn in the clinical education experiences. The CIs reported that they are willing to instruct an ATS who shows interest rather than take time to instruct an ATS who is indifferent. The concept of students initiating the teachable moment is not well supported by the medical literature. Most researchers have suggested that the CI or preceptor is responsible for initiating teachable moments.7,9–13 Wagner and Ash11 believed that the CI or teacher creates this phenomenon. However, Hyun and Marshall6 believed that both student and teacher can create a teachable moment. Therefore, the importance of students taking an active role in their education is emphasized. Collectively, CIs and ATSs should seek out learning opportunities.
Limitations
Generalizability of the results of this study is limited. Using a qualitative approach and studying a small, nonrandom sample limited inference of the results. In addition, I studied only 1 institution and only 1 type of clinical education setting (collegiate sports medicine facility). Further investigation across different institutions, as well as athletic training clinical education settings (high school, physical therapy clinic, and physician's clinic), may provide insight into how often teachable moments occur in those settings and may provide different perspectives from other allied health care professionals on defining the teachable moment.
CONCLUSIONS
In my study, CIs and ATSs provided insight regarding their perceptions and understandings of teachable moments. The teachable moment occurs when a CI and an ATS actively participate and interact with each other to enhance learning and foster intellectual curiosity in the clinical education environment. The CIs and ATSs were clearly able to identify teachable moments, and the results indicate that teachable moments are perceived to occur in a collegiate clinical education setting. Recognizing teachable moments may enhance the quality of clinical instruction and education for both the CI and the ATS. Asking CIs and ATSs to describe teachable moments, either in a clinical education course or in a workshop, may increase awareness of teachable moments and subsequently may increase the frequency of teachable moments. Upon completion of this investigation, many of the participants indicated increased awareness of teachable moments, and several found themselves seeking them out. My study not only illustrates that numerous learning opportunities are present in the clinical education setting but also illustrates that several barriers prevent the CI and the ATS from acting on these opportunities, which is a problem warranting future investigation.
Acknowledgments
I thank Dr James Eison for being the inspiration for this study, Dr Micki Cuppett for providing guidance, and Dr Gene Burns for revising and editing this article.
Footnotes
Valerie J. Rich, PhD, ATC, CSCS, WEMT-B, contributed to conception and design; acquisition and analysis and interpretation of the data; and drafting, critical revision, and final approval of the article.
REFERENCES
- 1.Weidner T.G, Henning J.M. Being an effective athletic training clinical instructor. Athl Ther Today. 2002;7(5):6–11. [Google Scholar]
- 2.Platt Meyer L.S. Leadership characteristics as significant predictors of clinical-teaching effectiveness. Athl Ther Today. 2002;7(5):34–39. [Google Scholar]
- 3.Curtis N, Helion J.G, Domsohn M. Student athletic trainer perceptions of clinical supervisor behaviors: a critical incident study. J Athl Train. 1998;33(3):249–253. [PMC free article] [PubMed] [Google Scholar]
- 4.Laurent T, Weidner T.G. Clinical instructors' and student athletic trainers' perceptions of helpful clinical instructor characteristics. J Athl Train. 2001;36(1):58–61. [PMC free article] [PubMed] [Google Scholar]
- 5.Leist J.C, Kristofco R.E. The changing paradigm for continuing medical education: impact of information on the teachable moment. Bull Med Libr Assoc. 1990;78(2):173–179. [PMC free article] [PubMed] [Google Scholar]
- 6.Hyun E, Marshall J.D. Teachable-moment-oriented curriculum practice in early childhood education. J Curriculum Stud. 2003;35(1):111–127. [Google Scholar]
- 7.Rea D. Sustaining teachable moments on the complex edge of chaos. Paper presented at: American Educational Research Association Conference; April 21–25, 2003; Chicago, IL.
- 8.Bentley M.L. Making the most of the teachable moment: carpe diem. Sci Act. 1995;32(3):23–27. [Google Scholar]
- 9.McBride C.M, Emmons K.M, Lipkus I.M. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003;18(2):156–170. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- 10.Pediatrics in Practice. Education: educating families through teachable moments. http://www.pediatricsinpractice.org/pdfs/Education/Education_handout1-1-r.pdf. Accessed January 29, 2007.
- 11.Wagner P.S, Ash K.L. Creating the teachable moment. J Nurs Educ. 1998;37(6):278–280. doi: 10.3928/0148-4834-19980901-14. [DOI] [PubMed] [Google Scholar]
- 12.Badgett R.G, O'Keefe M, Henderson M.C. Using systematic reviews in clinical education. Ann Intern Med. 1997;126(11):886–891. doi: 10.7326/0003-4819-126-11-199706010-00006. [DOI] [PubMed] [Google Scholar]
- 13.Buyck D, Lang F. Teaching medical communication skills: a call for great uniformity. Fam Med. 2002;34(5):337–343. [PubMed] [Google Scholar]
- 14.Hutsick M. Seizing the teachable moment. Paper presented at: 57th annual meeting and clinical symposia of the National Athletic Trainers' Association; June 14–18, 2006; Atlanta, GA.
- 15.Wagner R. Utilizing technology to enhance clinical education. Paper presented at: Athletic Training Educators' Conference of the National Athletic Trainers' Association; January 12–14, 2007; Dallas, TX.
- 16.Geisler P.R, Parker E.A. Interconnecting the didactic with the clinical: enhancing student cognition, motivation and responsibility with individual clinical education plans. Paper presented at: Athletic Training Educators' Conference of the National Athletic Trainers' Association; January 20–23, 2005; Del Lago, TX.
- 17.Creswell J.W. Qualitative Inquiry and Research Design: Choosing Among Five Traditions. Thousand Oaks, CA: Sage Publications, Inc; 1998. pp. 118–120. [Google Scholar]
- 18.Johnson B, Christensen L. Educational Research: Quantitative, Qualitative, and Mixed Approaches. 2nd ed. Boston, MA: Allyn and Bacon; 2004. pp. 197–223.pp. 412–431. [Google Scholar]
- 19.Carnegie Foundation for the Advancement of Teaching. Category definitions. http://www.carnegiefoundation.org/classification. Accessed January 29, 2007.
- 20.Leech N.L, Onwuegbuzie A.J. A typology of mixed methods research designs. Paper presented at: Annual meeting of the Mid-South Educational Research Association; November 17–19, 2004; Gatlinburg, TN.
- 21.Strauss A.L, Corbin J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. 2nd ed. Thousand Oaks, CA: Sage Publications, Inc; 1998. pp. 48–52.pp. 212 [Google Scholar]
- 22.Ryan G.W, Bernard H.R. Data management and analysis methods. In: Denzin N.K, Lincoln Y.S, editors. Handbook of Qualitative Research. 2nd ed. Thousand Oaks, CA: Sage Publications, Inc; 2000. pp. 769–802. [Google Scholar]
- 23.Leech N.L, Onwuegbuzie A.J. Increasing rigor in qualitative research: the array of tools for qualitative analysis. Paper presented at: Annual meeting of the Southwest Educational Research Association; February 9–12, 2005; New Orleans, LA.
- 24.Glaser B.G, Strauss A.L. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL: Aldine; 1967. pp. 238–245. [Google Scholar]
- 25.Onwuegbuzie A.J, Teddlie C. A framework for analyzing data in mixed methods research. In: Tashakkori A, Teddlie C, editors. Mixed Methodology: Combining Qualitative and Quantitative Approaches. Thousand Oaks, CA: Sage Publications, Inc; 2003. pp. 351–383. [Google Scholar]
- 26.Onwuegbuzie A.J. Validity and qualitative research: an oxymoron. Paper presented at: Annual conference of the Mid-South Educational Research Association; November 6–8, 2002; Chattanooga, TN.
- 27.Mensch J.M, Ennis C.D. Pedagogic strategies perceived to enhance student learning in athletic training education. J Athl Train. 2002;37(4 suppl):S199–S207. [PMC free article] [PubMed] [Google Scholar]
- 28.Weidner T.G, Henning J.M. Development of standards and criteria for the selection, training, and evaluation of athletic training Approved Clinical Instructors. J Athl Train. 2004;39(4):335–343. [PMC free article] [PubMed] [Google Scholar]
- 29.Jarski R.W, Kulig K, Olson R.E. Allied health perceptions of effective clinical instruction. J Allied Health. 1989;18(5):469–478. [PubMed] [Google Scholar]
- 30.Jarski R.W, Kulig K, Olson R.E. Clinical teaching in physical therapy: student and teacher perceptions. Phys Ther. 1990;70(3):173–178. doi: 10.1093/ptj/70.3.173. [DOI] [PubMed] [Google Scholar]
- 31.Commission on Accreditation of Athletic Training Education. Standards for the accreditation of entry-level athletic training education programs. http://caate.net/documents/Standards.6.30.08.pdf. Accessed November 17, 2008.
- 32.Weidner T.G, Henning J.M. Historical perspective of athletic training clinical education. J Athl Train. 2002;37(4 suppl):S222–S228. [PMC free article] [PubMed] [Google Scholar]
- 33.Weidner T.G, Henning J.M. Clinical-education–setting standards are helpful in the professional preparation of employed, entry-level certified athletic trainers. J Athl Train. 2002;37(4 suppl):S248–S254. [PMC free article] [PubMed] [Google Scholar]
- 34.Miller M.G, Berry D.C. An assessment of athletic training students' clinical-placement hours. J Athl Train. 2002;37(4 suppl):S229–S235. [PMC free article] [PubMed] [Google Scholar]
- 35.Rattner S.L, Louis D.Z, Rabinowitz C, et al. Documenting and comparing medical students' clinical experiences. JAMA. 2001;286(9):1035–1040. doi: 10.1001/jama.286.9.1035. [DOI] [PubMed] [Google Scholar]
- 36.Weidner T.G, Henning J.M. Importance and applicability of approved clinical instructor standards and criteria to certified athletic trainers in different clinical education settings. J Athl Train. 2005;40(4):326–332. [PMC free article] [PubMed] [Google Scholar]