Abstract
Context:
Underconditioned patellar stabilizing muscles could be a predisposing factor for patellar instability.
Objective:
To examine the effect of 2 modes of weight training on the size of the vastus medialis obliquus (VMO), the resting position and passive mobility of the patella, and the strength of the knee extensor muscles.
Design:
Prospective intervention, repeated measures in 3 groups.
Setting:
Orthopaedic and sports sciences research laboratory.
Patients or Other Participants:
48 healthy adults free from back and lower extremity injuries.
Intervention(s):
Participants were randomly assigned to muscle hypertrophy training, muscle strength training, or the control group. Those in the training groups pursued training 3 times per week for 8 weeks.
Main Outcome Measure(s):
Magnetic resonance imaging and ultrasound cross-sectional area of the VMO, patellar tilt angle on magnetic resonance imaging, instrumented passive patellar mobility, and isometric knee extension torque of the dominant leg.
Results:
Participants in both training groups had comparable gains in VMO size, passive patellar stability, and knee extension force, all of which were greater than for the control group (P < .05).
Conclusions:
Both short-term muscle hypertrophy and strength training programs can reinforce the patellar stabilizers in previously untrained volunteers.
Keywords: quadriceps muscles, patellofemoral joint, magnetic resonance imaging
Key Points
Previously untrained participants who underwent 8 weeks of either muscle hypertrophy or muscle strength training increased vastus medialis obliquus size, passive patellar stability, and knee extension force compared with a control group that did not weight train.
In previously untrained volunteers, the patellar stabilizers were reinforced with both muscle hypertrophy and muscle strength training programs.
Patellar instability has been regarded as a predisposing factor for patellofemoral pain syndrome and patellar subluxation and dislocation.1–3 Static instability of the patella can be defined as occurring when the patellofemoral joint is inherently unstable or unable to maintain equilibrium in response to an external perturbation4 and is determined by the extensibility of the patellar retinaculum and the patellofemoral joint congruency.1 In dynamic instability, the patella cannot be optimally maintained within the femoral trochlea during postural loading or functional movements.5 Dynamic instability usually leads to excessive lateral patellar tracking rather than medial maltracking; thus, underconditioning of the vastus medialis obliquus (VMO) muscle has been reported to be the predisposing factor.5–8
The VMO not only stabilizes the patella medially, it also determines patellofemoral joint contact stress. When patellofemoral joint pressure was tested in 5 human knee specimens with different VMO tensions in weight-bearing positions, an increase in the lateral patellofemoral joint contact pressure was noted, with a decrease in VMO tension at 30° and 90° of knee flexion.9 Also, according to a finite element model analysis, if VMO muscle strength increased by 20%, lateral patellar cartilage shear stress shifted medially without a rise in total patellar cartilage shear stress during squatting.10
Although physical exercise has long been reported to lead to strengthening of the skeletal muscles, tendons, and ligaments, which are important for sports injury prevention,11–16 information is lacking on the effects of physical conditioning on patellofemoral joint stabilization.
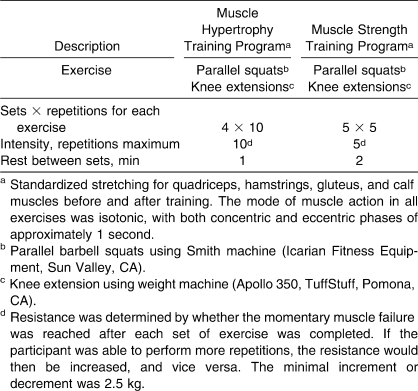
Physiologically, only those motor units that are recruited in the exercise are subject to adaptational changes with weight training. A motor unit is composed of either all slow-twitch or all fast-twitch muscle fibers. According to the Henneman size principle for recruitment of motor units, the low-threshold motor units (composed of slow-twitch muscle fibers) are recruited first. As the demands of weight training rise with increasing resistance, progressively higher-threshold motor units (composed predominantly of fast-twitch fibers) are recruited.17–19 Thus, weight training for muscular strength (eg, 5 sets of 5 repetitions, separated by 2 minutes of rest) could recruit more muscle fibers than training for muscle hypertrophy (eg, 4 sets of 10 repetitions, separated by 1 minute of rest). Muscle hypertrophy training provides longer and more frequent stimulus for the muscle fibers in a given session than does the muscle strength training program because a relatively higher number of repetitions and shorter rest times are required.20
Different prescriptions of weight training programs can result in diverse development of muscular endurance, power, strength, and mass.21 We conducted the present study to evaluate and compare 2 popular modes of weight training on bodybuilding (muscle hypertrophy) and power lifting (muscular strength) to determine the factors contributing to patellar stability, including the relationship of the size of the VMO to dynamic patellar stability6–8; passive lateral mobility of the patella, which reflects static patellar stability9,22; patellar tilt angle (PTA), which indicates resting patellar position; patellofemoral joint congruency23,24; and strength of the knee extensors25 before and after the weight training programs.
Because the patella's resting position is largely determined by the length and stiffness of the adjacent muscle and connective tissues,1–4 we hypothesized that muscle hypertrophy training, which should elicit a relatively larger volume gain in the skeletal muscle and connective tissues, may have more effect on patellar positioning and mobility, whereas muscle strength training should result in relatively greater improvement in knee extensor force.
Thus, our hypotheses were as follows:
Different modes of 8 weeks of weight training for muscle hypertrophy and muscle strengthening would result in distinguishable adaptations of VMO size and quadriceps strength enhancement.
Both modes of weight training would decrease passive lateral patellar mobility.
Both modes of weight training would alter the PTA.
METHODS
Participants
Forty-eight volunteers (36 men, 12 women), ages 18 to 35 years, were recruited for this study by convenience sampling. None of the participants had engaged in regular weight training or regular exercise before the study. None had any known injuries or illnesses, including pain or injury in the lower limbs or back, for at least 6 months before the study. The study was reviewed and approved by the Human Ethics Subcommittee of the administering institution, and all volunteers gave informed written consent before the study began.
Modes of Weight Training
Authors26–31 of most of the previous studies focusing on the effects of weight training suggested that if the principal goal of training was to induce muscle hypertrophy, such as for bodybuilders, the training protocol should include moderate loads and a moderate number of repetitions (eg, 4 sets of 8 to 12 repetitions maximum). Conversely, if the principal goal was to enhance muscular strength, such as for power lifters, the training should include high loads and a low number of repetitions (eg, 5 sets of 2 to 6 repetitions maximum). These training principles have been accepted by the National Strength and Conditioning Association.32
Based on the above training principles, the participants were randomly allocated into 1 of 3 groups: muscle hypertrophy training (program H), muscle strength training (program S), and no-exercise control group. So that the number of men and women was equal in each group, we applied stratified allocation for sex. Both program H and program S contained 24 sessions, distributed evenly over a period of 8 weeks, with 3 sessions per week and a minimum 48-hour rest between sessions (Table 1). All sessions were conducted by the same trainer (a certified strength and conditioning specialist) with each participant on an individual basis.
Table 1.
Two Modes of Progressive and Supervised Weight Training Programs
Dependent Variables
Dependent variables were measured for the dominant leg of the volunteers. Leg dominance was defined as the leg that the individual preferred for kicking a ball.
Measurement of Cross-Sectional Area of the VMO
Magnetic resonance imaging (MRI) and B-mode ultrasound imaging techniques were used for measuring the cross-sectional area of the VMO. Half the participants in each training group had MRIs before and after the 8-week training program. The other volunteers in the training groups and everyone in the control group underwent B-mode ultrasound imaging. Two modes of measurements were used to assess VMO size because the MRI became unavailable midway through the study; thus, the later participants were assessed with B-mode ultrasound. Both MRI and ultrasound measurements have been confirmed to be valid and repeatable for lower limb muscle size.33–36 The volunteers were asked to refrain from vigorous physical activities for 48 hours before imaging because strenuous activities may boost local vasodilatations and thus temporarily increase muscle girth because of fluid retention.
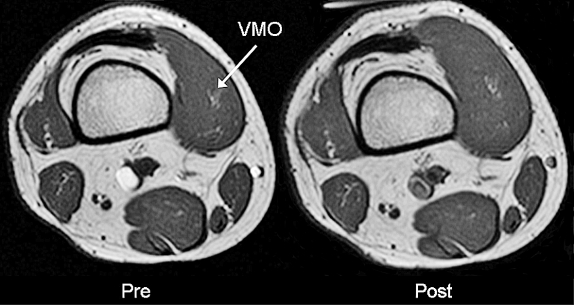
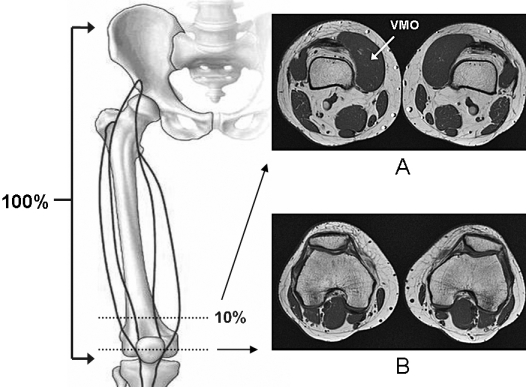
For the MRI examinations, participants were positioned supine, with the knees extended and the feet held together by adhesive tape for standardizing the hip and knee angles. A 1.5-T MRI scanner with surface coils (Magnetom Avanto; Siemens AG, Erlangen, Germany) was used to record the axial T1-weighted images (repetition time [TR]/echo time [TE] = 420 milliseconds/50 milliseconds, slice thickness = 3 mm, interslice gap = 0.3 mm, field of view = 35 × 20 cm, matrix = 448 × 256) of the volunteers' knees and thighs. Foam inserts were used to support the surface coils and keep the anterior thighs and knees from being compressed by the coils. Image datasets were saved in DICOM format (National Electrical Manufacturers Association, Rosslyn, VA) for offline analysis. A line was drawn from the lateral knee joint line to the ipsilateral anterior-superior iliac spine, and the image obtained on a plane 10% proximal to the knee joint line was used for VMO cross-sectional area measurement (Figure 1). The 10% section was chosen for standardizing the selected VMO area, which represented the oblique VMO fibers well. With imaging analysis software (MIPAV, version 2.0; National Institutes of Health, Bethesda, MD) and a graphic digitizer (model CTE-430; Wacom, Vancouver, WA), we manually traced the borders of the VMO muscle. The test-retest reliability of the MRI measurement for the vasti muscles was 0.99 (Pearson coefficient).37 Our pilot study of 3 volunteers revealed the intrarater intraclass correlation coefficient (ICC) to be 0.97 (95% confidence interval [CI] = 0.81, 0.99, consistency).
Figure 1. Selected axial magnetic resonance images. A, Vastus medialis obliquus (VMO) muscle at the distal 10% of the length between the anterior-superior iliac spine and the lateral knee joint line, and B, at the midtransverse patella level.
For the ultrasound imaging, participant positioning and procedures for locating the VMO followed those for the MRI examination. A diagnostic B-mode ultrasound scanner and a 4-MHz annular array probe with 7-cm curved window length and 63° field of view (Voyager; Ardent Sound, Inc, Mesa, AZ) were used to capture the VMO muscle cross-sectional area. The probe was totally supported by a custom-made mechanical stand that was adjustable in height and inclination angle. A premolded ultrasound gel pad (Aquaflex; Ardent Laboratories, Inc, Fairfield, NJ) was used as a medium between the ultrasound probe and the VMO underneath (Figure 2). The images of the VMO were stored in tagged image file format for later analysis with Kodak 1D Image Analysis software (version 3.5; Eastman Kodak Co, Rochester, NY) and manual tracing with a graphic digitizer (model CTE-430; Wacom). In a pilot study with 6 volunteers, the validity coefficient between the MRI and ultrasound measurements for VMO size was high (Pearson coefficient = 0.97), and the between-days ultrasound measurement was repeatable (intrarater ICC = 0.96, 95% CI = 0.89, 0.99, consistency).38
Figure 2. A, Hands-free ultrasound imaging. B, Corresponding ultrasound image. The laser provided a reference for positioning the participant and locating the vastus medialis obliquus.

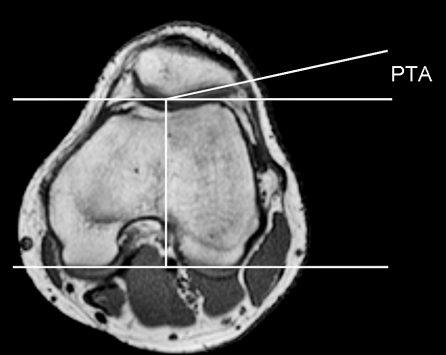
Patellar Tilt Angle
Only those participants in the training groups who received the MRI had their PTA measured at the midtransverse patellar axial view (Figure 1)39; PTA was marked by the intersection of the lateral patellar facet line and the posterior condylar reference line (Figure 3).40 A decrease in PTA has been reported to be related to static patellar instability and patellofemoral pain syndrome and was considered a sign of increased lateral patellofemoral joint pressure or tightness of lateral patellar retinaculum.22,23,38 The MRI-based PTA measurement was previously found to be repeatable by Sathe et al41 (ICC = 0.95) and in our pilot study with 3 volunteers (intrarater ICC = 0.98, 95% CI = 0.79, 0.99).
Figure 3. The patellar tilt angle (PTA) is formed by the intersection of the lateral patellar facet line and the posterior condylar reference line.
Patellar Mobility Measurement
Manual passive patellar gliding is a routine clinical examination for patellofemoral joint mobility.1,2 We used instrumented patellar gliding with 0.5-mm accuracy; between-days reliability of this technique has been reported in previous studies (intrarater ICC = 0.96, 95% CI = 0.94, 0.98, absolute agreement).42,43 Briefly, with the participants supine, knees extended, and feet together, the ankles and lower legs were secured to restrict lower limb movements. A patellar glide device comprising a force gauge transducer (model AEF-5; Aikon Engineering Co, Osaka, Japan), an electromagnetic motion tracker (model pciBIRD; Ascension Technology Corp, Burlington, VT), and a custom-made plastic liner bearing an adjustable platform (Poly-Jaque plastic lab jack; Scienceware, Pequannock, NJ) was used to glide the volunteer's patella laterally at a constant velocity of 2 cm/s (Figure 4). The gliding force was 15 N, and the linear displacement of the patella was collected at a sampling rate of 100 Hz for postacquisition analysis with Excel software (Office 2000; Microsoft Corp, Redmond, WA).
Figure 4. Passive patellar mobility measurement. E indicates electromagnetic tracker; M, mechanomyography biofeedback; F, force gauge.
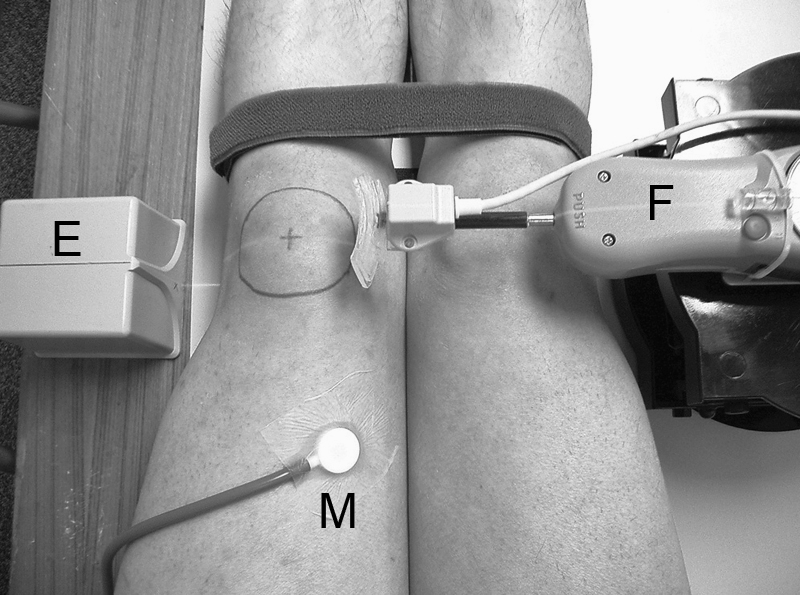
We tested both knees with 3 continuous passive gliding tests and averaged these results to minimize any random error. To ensure that the participants had relaxed their quadriceps muscle during the measurement, mechanomyographic muscle signals were detected via an air-coupled transducer (pulse wave pickup, model 21051D; Hewlett-Packard Co, Palo Alto, CA).44 The mechanomyographic signals were fed to a biofeedback unit (Myotrac; Thought Technology, Ltd, Montreal, Quebec, Canada), which provided an audio alarm when the quadriceps' signal (root mean square = 100 milliseconds time constant) was over the preset threshold set of 1 µV.45
Knee Extension Force
A dynamometer (Cybex Norm; Henley Healthcare, Hauppauge, NY) was used to measure the slow-ramp maximal isometric knee extension force of each volunteer with the knee at 45° and hip at 85° of flexion. The test lasted for 5 seconds and was repeated 3 times, with a 2-minute rest between trials. Only the highest force developed during the 3 trials was used for data analysis. The maximal isometric knee extension torque has been reported as repeatable for between-days measurements with a Pearson coefficient of 0.8846; its within-days reliability measured by ICC was 0.93.47 The tests were performed twice, 8 weeks apart, similarly to all other measurements in that both legs were measured and the results included in data analysis and all measurements were taken by the same investigator.
Statistical Analysis
Data analysis was performed using SPSS software (version 11.5; SPSS Inc, Chicago, IL) for the following:
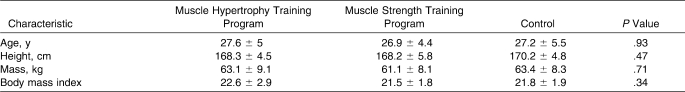
Baseline characteristics: between-groups comparison by 1-way analysis of variance (ANOVA; Table 2)
VMO size, patellar mobility, and knee extensor torque: between-groups comparison for pretraining and posttraining measurements with 3 (groups) × 2 (measurements) factorial ANOVA
Patellar tilt angle: pretraining and posttraining PTA was compared with 2 (groups) × 2 (measurements) factorial ANOVA
Table 2.
Participants' Baseline Characteristics (Mean ± SD)
If the analyses in items 2 and 3 were significant (P < .05), a 1-way ANOVA with post hoc least-squares difference method and paired t tests was used to identify the difference (Table 3). The level of significance was set at .05 for all analyses.
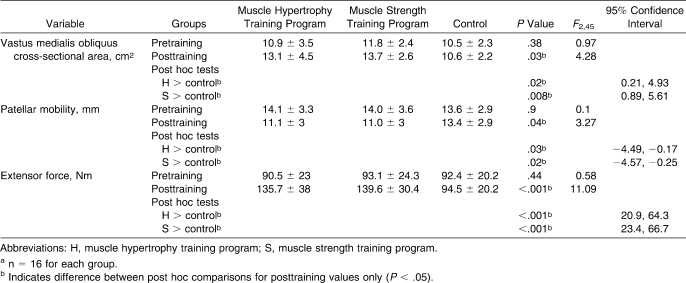
Table 3.
Pretraining and Posttraining Measurements of the Dominant Leg by 1-Way Analysis of Variance (Mean ± SD)a
RESULTS
Participant compliance was good, with 28 of 32 volunteers in the intervention groups completing all 24 sessions and the other 4 completing 21 sessions. No physical injuries were reported during the 8 weeks of training.
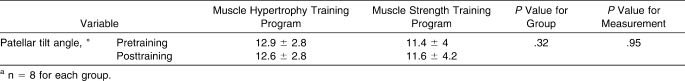
The 3 groups had comparable baseline characteristics (Table 2) and pretraining measurements (Table 3). After 8 weeks, the participants in both training groups had improved in all measurements as compared with those in the control group, with an increase in VMO size (F2,45 = 4.28, P = .03), decrease in passive lateral patellar mobility (F2,45 = 3.27, P = .04), and increase in knee extension torque (F2,45 = 11.09, P < .001; Table 3, Figure 5). When comparing the training groups, no difference was noted in posttraining measurements. For the PTA, however, training resulted in no change (Table 4).
Figure 5. Magnetic resonance image of the vastus medialis obliquus (VMO) of the right leg, pretraining (Pre) and posttraining (Post), from a representative volunteer in the muscle hypertrophy training group.
Table 4.
Pretraining and Posttraining Patellar Tilt Angle Values of the Dominant Leg by 2 × 2 Factorial Analysis of Variance (Mean ± SD)a
DISCUSSION
Eight weeks of weight training programs targeting either improved muscle strength or muscle size resulted in comparable gains in passive patellar stability, quadriceps strength, and hypertrophy of the VMO muscle in the dominant leg in previously untrained participants. We hypothesize that 8 weeks, which consisted of 24 weight training sessions, might not be long enough to detect a difference in the outcome measurements between groups in programs H and S.
Although all volunteers were requested to maintain their lifestyles, including their dietary and sleeping habits, during the 8 weeks, whether these potential confounding factors could have affected the outcomes is unknown. As Biolo et al48 and Esmarck et al49 have noted, skeletal muscle building is a nutritionally modulated process, and a supplementary amount of protein intake can enhance muscle synthesis postexercise. Also, inadequate sleep can hinder weight training performance and exercise-induced muscle growth.50
Although we did not study the vastus lateralis, the enlarged VMO induced by training may imply a potentially greater medial stabilizing force on the patella. In most cases of acute patellar dislocation, the VMO is injured and even torn,51 so we hypothesize that both modes of weight training, being effective for VMO muscle building, may have a protective effect on the VMO when lateral patellar tracking is excessive. We suggest future study to examine whether weight training has a global or specific effect on the VMO and vastus lateralis.
Lateral hypermobility of the patella has been identified as a predisposing factor for anterior knee pain in both prospective and cross-sectional studies.20–22 Our finding that lateral patellar mobility decreased after the weight training program is consistent with the findings of Reeves et al52 that after 14 weeks of resistance training for previously untrained persons, superior patellar mobility and patellar tendon elongation decreased at a given isometric knee extension force as detected by B-mode ultrasound. Thus, the connective tissues bridging the patella to the femur and tibia may be able to adapt to repetitive mechanical loading.53 The medial patellofemoral ligament (MPFL), which bridges the adductor tubercle and medial patella, contributes 53% of the resistance to lateral patellar translation at full knee extension, whereas the medial patellomeniscal ligament contributes 22% of the resistance.54 Although we could not conduct any direct biomechanical test on the physical properties of these ligaments in vivo, our finding of decreased lateral patellar translation after the training programs might imply that the MPFL, the medial patellomeniscal ligament, or both were stiffened as a result of the training. However, because the lateral patellar mobility test was performed in a quasistatic manner, the effect of weight training on the dynamic patellar tracking during faster and more functional movements warrants further investigation.
The VMO muscle attaches to the medial one-third of the MPFL. When the VMO contracts, the MPFL is pulled proximally and tightened. Therefore, the VMO not only acts directly to stabilize the patella but also acts indirectly through the MPFL.55,56 The stiffened MPFL may be more effective in force transmission between the VMO and the patella57 and, theoretically, may help to prevent the patella from excessive lateral tracking in postural loading and dynamic actions.
Ingersoll and Knight58 reported that patellofemoral joint congruence in asymptomatic participants who received 3 weeks of resistance or EMG biofeedback training to the quadriceps changed on Merchant view examination. They hypothesized that the shortened knee extensor muscles could induce more favorable patellar tracking, thus reducing the predisposition to lateral patellar instability. We did not use the Merchant method because it was reported to be less reliable than the PTA measurement59 and not sensitive enough in detecting small changes in patellar tilt.60 A PTA of less than 8° was closely correlated with the presence of anterior knee pain.23,24 Among the 16 volunteers included in the PTA examination, only 2 had a marginally abnormal PTA (6° to 7.5°). Therefore, the finding of no change in PTA after training may be from a ceiling effect, because most participants had a normal PTA before the study. The unchanged PTA may indicate that the enlarged VMO has an insignificant effect on resting patellar position. However, we were unable to obtain PTA data on the control group because of limited MRI availability.
We believe our study is the first of its kind to examine the effects of different modes of weight training on the size of the VMO muscle and passive lateral patellar stability. The positive findings suggest that a suitable weight training program may help to minimize lateral patellar instability in people engaged in physical activities. However, because we studied only asymptomatic and young volunteers, the findings may not be generalizable to people with patellar disorders or those of different ages. Future authors may focus on dynamic patellar tracking before and after weight training and compare the incidence of patellofemoral joint-related injuries among participants with and without physical conditioning.
CONCLUSIONS
Eight-week weight training programs aimed at building either muscle mass or muscle strength could lead to hypertrophy of the VMO and improve knee extension strength and passive lateral patellar stability for previously untrained adults.
Footnotes
Yiu-ming Wong, PhD, contributed to conception and design; acquisition and analysis and interpretation of the data; and drafting, critical revision, and final approval of the article. Suk-tak Chan, PhD, contributed to acquisition of the data and drafting, critical revision, and final approval of the article. Kwok-wing Tang, MBBS, contributed to acquisition of the data and critical revision and final approval of the article. Gabriel Y. F. Ng, PhD, contributed to conception and design, analysis and interpretation of the data, and drafting, critical revision, and final approval of the article.
REFERENCES
- 1.Fulkerson J.P. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med. 2002;30(3):447–456. doi: 10.1177/03635465020300032501. [DOI] [PubMed] [Google Scholar]
- 2.LaBella C. Patellofemoral pain syndrome: evaluation and treatment. Prim Care. 2004;31(4):977–1003. doi: 10.1016/j.pop.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 3.Hughston J.C, Walsh W.M, Puddu G. Patellar Subluxation and Dislocation. Philadelphia, PA: WB Saunders; 1984. pp. 128–150. [Google Scholar]
- 4.Padua D.A, Blackburn J.T. Muscle stiffness and biomechanical stability. Athl Ther Today. 2003;8(6):45–47. [Google Scholar]
- 5.McConnell J. Rehabilitation and nonoperative treatment of patellar instability. Sports Med Arthrosc. 2007;15(2):95–104. doi: 10.1097/JSA.0b013e318054e35c. [DOI] [PubMed] [Google Scholar]
- 6.Fox T.A. Dysplasia of the quadriceps mechanism: hypoplasia of the vastus medialis muscle as related to the hypermobile patella syndrome. Surg Clin North Am. 1975;55(1):199–226. doi: 10.1016/s0039-6109(16)40542-6. [DOI] [PubMed] [Google Scholar]
- 7.Fisher R.L. Conservative treatment of patellofemoral pain. Orthop Clin North Am. 1986;17(2):269–272. [PubMed] [Google Scholar]
- 8.Wilk K.E, Davies G.J, Mangine R.E, Malone T.R. Patellofemoral disorders: a classification system and clinical guidelines for nonoperative rehabilitation. J Orthop Sports Phys Ther. 1998;28(5):307–322. doi: 10.2519/jospt.1998.28.5.307. [DOI] [PubMed] [Google Scholar]
- 9.Ng G.Y.F, Tang A, Mak A, Chan K. A study of vastus medialis obliquus tension on patellofemoral joint pressure in a simulated weight bearing position. Paper presented at: Australian Conference of Science and Medicine in Sport; October 15, 1998; Adelaide, Australia.
- 10.Besier T.F, Gold G.E, Beaupre G.S, Delp S.L. A modeling framework to estimate patellofemoral joint cartilage stress in vivo. Med Sci Sports Exerc. 2005;37(11):1924–1930. doi: 10.1249/01.mss.0000176686.18683.64. [DOI] [PubMed] [Google Scholar]
- 11.Reid S.E, Schiffbauer W. Role of athletic trainers in prevention, care and treatment of injuries. J Lancet. 1957;77(3):83–84. [PubMed] [Google Scholar]
- 12.Adams A. Effect of exercise on ligament strength. Res Q. 1966;37(2):163–167. [PubMed] [Google Scholar]
- 13.Cahill B.R, Griffith E.H. Effect of preseason conditioning on the incidence and severity of high school football knee injuries. Am J Sports Med. 1978;6(4):180–184. doi: 10.1177/036354657800600406. [DOI] [PubMed] [Google Scholar]
- 14.Hejna W, Rosenberg A, Buturusis D, Krieger A. The prevention of sports injuries in high school students through strength training. Natl Strength Coaches Assoc J. 1982;4(1):28–31. [Google Scholar]
- 15.Hewett T.E, Lindenfeld T.N, Riccobene J.V, Noyes F.R. The effect of neuromuscular training on the incidence of knee injury in female athletes: a prospective study. Am J Sports Med. 1999;27(6):699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 16.Heidt R.S, Jr, Sweeterman L.M, Carlonas R.L, Traub J.A, Tekulve F.X. Avoidance of soccer injuries with preseason conditioning. Am J Sports Med. 2000;28(5):659–662. doi: 10.1177/03635465000280050601. [DOI] [PubMed] [Google Scholar]
- 17.Henneman E, Clamann H.P, Gillies J.D, Skinner R.D. Rank order of motoneurons within a pool: law of combination. J Neurophysiol. 1974;37(6):1338–1349. doi: 10.1152/jn.1974.37.6.1338. [DOI] [PubMed] [Google Scholar]
- 18.Ebbeling C.B, Clarkson P.M. Exercise-induced muscle damage and adaptation. Sports Med. 1989;7(4):207–234. doi: 10.2165/00007256-198907040-00001. [DOI] [PubMed] [Google Scholar]
- 19.Duchateau J, Semmler J.G, Enoka R.M. Training adaptations in the behavior of human motor units. J Appl Physiol. 2006;101(6):1766–1775. doi: 10.1152/japplphysiol.00543.2006. [DOI] [PubMed] [Google Scholar]
- 20.Witvrouw E, Lysens R, Bellemans J, Cambier D, Vanderstraeten G. Intrinsic risk factors for the development of anterior knee pain in an athletic population: a two-year prospective study. Am J Sports Med. 2000;28(4):480–489. doi: 10.1177/03635465000280040701. [DOI] [PubMed] [Google Scholar]
- 21.Kujala U.M, Kvist M, Osterman K, Friberg O, Aalto T. Factors predisposing Army conscripts to knee exertion injuries incurred in a physical training program. Clin Orthop Relat Res. 1986;210:203–212. [PubMed] [Google Scholar]
- 22.Fithian D.C, Mishra D.K, Balen P.F, Stone M.L, Daniel D.M. Instrumented measurement of patellar mobility. Am J Sports Med. 1995;23(5):607–615. doi: 10.1177/036354659502300516. [DOI] [PubMed] [Google Scholar]
- 23.Pookarnjanamorakot C, Jaovisidha S, Apiyasawat P. The patellar tilt angle: correlation of MRI evaluation with anterior knee pain. J Med Assoc Thai. 1998;81(12):958–963. [PubMed] [Google Scholar]
- 24.Kujala U.M, Jaakkola L.H, Koskinen S.K, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9(2):159–163. doi: 10.1016/s0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 25.Callaghan M.J, Oldham J.A. Quadriceps atrophy: to what extent does it exist in patellofemoral pain syndrome. Br J Sports Med. 2004;38(3):295–299. doi: 10.1136/bjsm.2002.002964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berger R. Optimum repetitions for the development of strength. Res Q. 1962;33(3):334–338. [Google Scholar]
- 27.Kaneko M, Fuchimoto T, Toji H, Suei K. Training effect of different loads on force-velocity relationship and mechanical power output in human muscle. Scand J Sports Sci. 1983;5(2):50–55. [Google Scholar]
- 28.Kraemer W.J, Patton J.F, Gordon S.E, et al. Compatibility of high-intensity strength and endurance training on hormonal and skeletal muscle adaptation. J Appl Physiol. 1995;78(3):976–989. doi: 10.1152/jappl.1995.78.3.976. [DOI] [PubMed] [Google Scholar]
- 29.Kramer J.B, Stone M.H, O'Bryant H.S, et al. Effects of single versus multiple sets of weight training: impact of volume, intensity, and variation. J Strength Cond Res. 1997;11(3):143–147. [Google Scholar]
- 30.Campos G.E, Luecke T.J, Wendeln H.K, et al. Muscular adaptations in response to three different resistance-training regimens: specificity of repetition maximum training zones. Eur J Appl Physiol. 2002;88(1–2):50–60. doi: 10.1007/s00421-002-0681-6. [DOI] [PubMed] [Google Scholar]
- 31.Ronnestad B.R, Egeland W, Kvamme N.H, Refsnes P.E, Kadi F, Raastad T. Dissimilar effects of one- and three-set strength training on strength and muscle mass gains in upper and lower body in untrained subjects. J Strength Cond Res. 2007;21(1):157–163. doi: 10.1519/00124278-200702000-00028. [DOI] [PubMed] [Google Scholar]
- 32.Baechle T.R, Earle R.W, Wathen D. Resistance training. In: Baechle T.R, Earle R.W, editors. Essentials of Strength Training & Conditioning. 2nd ed. Champaign, IL: Human Kinetics; 2000. pp. 395–426. [Google Scholar]
- 33.Beneke R, Neuerburg J, Bohndorf K. Muscle cross-section measurement by magnetic resonance imaging. Eur J Appl Physiol Occup Physiol. 1991;63(6):424–429. doi: 10.1007/BF00868073. [DOI] [PubMed] [Google Scholar]
- 34.Lund H, Christensen L, Savnik A, Boesen J, Danneskiold-Samsøe B, Bliddal H. Volume estimation of extensor muscles of the lower leg based on MR imaging. Eur Radiol. 2002;12(12):2982–2987. doi: 10.1007/s00330-002-1334-1. [DOI] [PubMed] [Google Scholar]
- 35.Miyatani M, Kanehisa H, Kuno S, Nishijima T, Fukunaga T. Validity of ultrasonograph muscle thickness measurements for estimating muscle volume of knee extensors in humans. Eur J Appl Physiol. 2002;86(3):203–208. doi: 10.1007/s00421-001-0533-9. [DOI] [PubMed] [Google Scholar]
- 36.Reeves N.D, Maganaris C.N, Narici M.V. Ultrasonographic assessment of human skeletal muscle size. Eur J Appl Physiol. 2004;91(1):116–118. doi: 10.1007/s00421-003-0961-9. [DOI] [PubMed] [Google Scholar]
- 37.Mitsiopoulos N, Baumgartner R.N, Heymsfield S.B, Lyons W, Gallagher D, Ross R. Cadaver validation of skeletal muscle measurement by magnetic resonance imaging and computerized tomography. J Appl Physiol. 1998;85(1):115–122. doi: 10.1152/jappl.1998.85.1.115. [DOI] [PubMed] [Google Scholar]
- 38.Wong Y.M, Ng G.Y.F. Reliability of hand-free ultrasound measurement for vastus medialis obliquus. Paper presented at: Annual meeting of the American Society of Biomechanics; August 24, 2007; San Francisco, CA.
- 39.Shibanuma N, Sheehan F.T, Stanhope S.J. Limb positioning is critical for defining patellofemoral alignment and femoral shape. Clin Orthop Relat Res. 2005;434:198–206. doi: 10.1097/01.blo.0000155078.52475.63. [DOI] [PubMed] [Google Scholar]
- 40.Guzzanti V, Gigante A, Di Lazzaro A, Fabbriciani C. Patellofemoral malalignment in adolescents: computerized tomographic assessment with or without quadriceps contraction. Am J Sports Med. 1994;2(1):55–60. doi: 10.1177/036354659402200110. [DOI] [PubMed] [Google Scholar]
- 41.Sathe V.M, Ireland M.L, Ballantyne B.T, Quick N.E, McClay I.S. Acute effects of the Protonics system on patellofemoral alignment: an MRI study. Knee Surg Sports Traumatol Arthrosc. 2002;10(1):44–48. doi: 10.1007/s001670100249. [DOI] [PubMed] [Google Scholar]
- 42.Wong Y.M, Ng G.Y.F. Correlation between MRI and mechanical measurements for patellar stability. Paper presented at: Annual meeting of the American Society of Biomechanics; September 7, 2006; Blacksburg, VA.
- 43.Wong Y.M, Ng G.Y. The relationships between the geometrical features of the patellofemoral joint and patellar mobility in able-bodied subjects. Am J Phys Med Rehabil. 2008;87(2):134–138. doi: 10.1097/PHM.0b013e31815b62b9. [DOI] [PubMed] [Google Scholar]
- 44.Bolton C.F, Parkes A, Thompson T.R, Clark M.R, Sterne C.J. Recording sound from human skeletal muscle: technical and physiological aspects. Muscle Nerve. 1989;12(2):126–134. doi: 10.1002/mus.880120207. [DOI] [PubMed] [Google Scholar]
- 45.Evetovich T.K, Conley D.S, Todd J.B, Roger D.C, Stone T.L. Effect of mechanomyography as a biofeedback method to enhance muscle relaxation and performance. J Strength Cond Res. 2007;21(1):96–99. doi: 10.1519/00124278-200702000-00018. [DOI] [PubMed] [Google Scholar]
- 46.Welsch M.A, Williams P.A, Pollock M.L, Graves J.E, Foster D.N, Fulton M.N. Quantification of full-range-of-motion unilateral and bilateral knee flexion and extension torque ratios. Arch Phys Med Rehabil. 1998;79(8):971–978. doi: 10.1016/s0003-9993(98)90097-1. [DOI] [PubMed] [Google Scholar]
- 47.Bonhannon R.W. Hand-held compared with isokinetic dynamometry for measurement of static knee extension torque (parallel reliability of dynamometers) Clin Phys Physiol Meas. 1990;11(3):217–222. doi: 10.1088/0143-0815/11/3/004. [DOI] [PubMed] [Google Scholar]
- 48.Biolo G, Tipton K.D, Klein S, Wolfe R.R. An abundant supply of amino acids enhances the metabolic effect of exercise on muscle protein. Am J Physiol. 1997;273(1, pt 1):E122–E129. doi: 10.1152/ajpendo.1997.273.1.E122. [DOI] [PubMed] [Google Scholar]
- 49.Esmarck B, Andersen J.L, Olsen S, Richter E.A, Mizuno M, Kjaer M. Timing of postexercise protein intake is important for muscle hypertrophy with resistance training in elderly humans. J Physiol. 2001;535:301–311. doi: 10.1111/j.1469-7793.2001.00301.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Reilly T, Piercy M. The effect of partial sleep deprivation on weight-lifting performance. Ergonomics. 1994;37(pt 1):107–115. doi: 10.1080/00140139408963628. [DOI] [PubMed] [Google Scholar]
- 51.Sallay P.I, Poggi J, Speer K.P, Garrett W.E. Acute dislocation of the patella: a correlative pathoanatomic study. Am J Sports Med. 1996;24(1):52–60. doi: 10.1177/036354659602400110. [DOI] [PubMed] [Google Scholar]
- 52.Reeves N.D, Maganaris C.N, Narici M.V. Effect of strength training on human patella tendon mechanical properties of older individuals. J Physiol. 2003;548(pt 3):971–981. doi: 10.1113/jphysiol.2002.035576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wren T.A, Beaupre G.S, Carter D.R. Tendon and ligament adaptation to exercise, immobilization, and remobilization. J Rehabil Res Dev. 2000;37(2):217–224. [PubMed] [Google Scholar]
- 54.Conlan T, Garth W.P, Jr, Lemons J.E. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75(5):682–693. doi: 10.2106/00004623-199305000-00007. [DOI] [PubMed] [Google Scholar]
- 55.Tuxoe J.I, Teir M, Winge S, Nielson P.I. The medial patellofemoral ligament: a dissection study. Knee Surg Sports Traumatol Arthrosc. 2002;10(3):138–140. doi: 10.1007/s00167-001-0261-z. [DOI] [PubMed] [Google Scholar]
- 56.Nomura E, Inoue M, Kobayashi S. Generalized joint laxity and contralateral patellar hypermobility in unilateral recurrent patellar dislocators. Arthroscopy. 2006;22(8):861–865. doi: 10.1016/j.arthro.2006.04.090. [DOI] [PubMed] [Google Scholar]
- 57.Bojsen-Moller J, Magnusson S.P, Rasmussen L.R, Kjaer M, Aagaard P. Muscle performance during maximal isometric and dynamic contractions is influenced by the stiffness of the tendinous structures. J Appl Physiol. 2005;99(3):986–994. doi: 10.1152/japplphysiol.01305.2004. [DOI] [PubMed] [Google Scholar]
- 58.Ingersoll C.D, Knight K.L. Patellar location changes following EMG biofeedback or progressive resistive exercises. Med Sci Sports Exerc. 1991;23(10):1122–1127. [PubMed] [Google Scholar]
- 59.Delgado-Martinez A.D, Rodriguez-Merchan E.C, Ballesteros R, Luna J.D. Reproducibility of patellofemoral CT scan measurements. Int Orthop. 2000;24(1):5–8. doi: 10.1007/s002640050002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Inoue M, Shino K, Hirose H, Horibe S, Ono K. Subluxation of the patella. Computed tomography analysis of patellofemoral congruence. J Bone Joint Surg Am. 1988;70(9):1331–1337. [PubMed] [Google Scholar]