Abstract
Background: At the turn of the 20th century, women commonly died in childbirth due to rachitic pelvis. Although rickets virtually disappeared with the discovery of the hormone vitamin D, recent reports suggest vitamin D deficiency is widespread in industrialized nations. Poor muscular performance is an established symptom of vitamin D deficiency. The current U.S. cesarean birth rate is at an all-time high of 30.2%. We analyzed the relationship between maternal serum 25-hydroxyvitamin D [25(OH)D] status, and prevalence of primary cesarean section.
Methods: Between 2005 and 2007, we measured maternal and infant serum 25(OH)D at birth and abstracted demographic and medical data from the maternal medical record at an urban teaching hospital (Boston, MA) with 2500 births per year. We enrolled 253 women, of whom 43 (17%) had a primary cesarean.
Results: There was an inverse association with having a cesarean section and serum 25(OH)D levels. We found that 28% of women with serum 25(OH)D less than 37.5 nmol/liter had a cesarean section, compared with only 14% of women with 25(OH)D 37.5nmol/liter or greater (P = 0.012). In multivariable logistic regression analysis controlling for race, age, education level, insurance status, and alcohol use, women with 25(OH)D less than 37.5 nmol/liter were almost 4 times as likely to have a cesarean than women with 25(OH)D 37.5 nmol/liter or greater (adjusted odds ratio 3.84; 95% confidence interval 1.71 to 8.62).
Conclusion: Vitamin D deficiency was associated with increased odds of primary cesarean section.
Vitamin D deficiency is common in pregnant women. A multivariate logistic regression analysis revealed women who were vitamin D deficient were more likely to have a caesarian section than women who were vitamin D sufficient.
At the turn of the 20th century, rickets ran rampant in the newly industrialized cities of Europe and North America, and rachitic pelvis was a common cause of death in childbirth (1). Cesarean sections became established, in part, to manage this condition: “… malformed pelvises often prohibited normal delivery. As a result the rate of cesarean section went up markedly.” (2) Although rickets virtually disappeared with the discovery of the hormone vitamin D and its subsequent addition to milk, recent reports suggest its reemergence, (3,4) and that vitamin D deficiency is widespread in industrialized nations (5,6,7). Meanwhile, research into vitamin D deficiency and awareness of its range of acute and chronic consequences have proliferated (8,9,10,11,12). Poor muscular performance (5,11,12,13,14,15,16) is an established symptom of vitamin D deficiency. The term rachitic pelvis has fallen into disuse, but an association has been noted between cesarean birth and a narrow pelvis (17).
The current U.S. cesarean birth rate is 30.2% (18), a record high for the nation (18), up from 5% in 1970, and characterized by steep increases in primary as well as repeat cesareans (19). Common reasons for cesareans in industrialized nations include dystocia (20) and failure to progress (21). Recent research suggests that maternal calcium status plays a role both in preterm labor (22) and in the initiation of labor (23). This analysis assessed the relationship between maternal vitamin D status (serum 25-hydroxyvitamin D [25(OH)D]) at birth and primary cesarean section.
Subjects and Methods
Recruitment
Women were enrolled between March 21, 2005, and March 20, 2007, on the postpartum unit at Boston Medical Center, an urban teaching hospital in Boston, MA, within 72 h of giving birth.
Enrollment was evenly distributed over time to ensure data were representative of season because seasonal sunlight exposure affects vitamin D status (3). Women were ineligible if they had spent more than 2 months away from Boston during pregnancy; if they were not of black, white, or Hispanic race/ethnicity (due to low numbers of women available in other racial/ethnic groups); if they did not speak English, French, or Spanish; if the infant was admitted to intensive care, premature; or if the mother had a history of parathyroid, renal, or liver disease or was using illegal drugs. Women having a repeat cesarean were also excluded from this analysis because of the strong causal relationship between primary and repeat cesareans. Enrolled women answered a questionnaire on the postpartum unit within 72 h of birth, and venipuncture was performed on the mother before discharge. None of the patients were receiving an iv infusion at the time of the venipuncture.
Diagnostic test
Serum 25(OH)D, accepted as the indicator of vitamin D status in children and adults, was measured by competitive protein binding as described by Chen et al. (24) Because the serum half-life for 25(OH)D is about 21 d, it was minimally influenced by fasting or changes in dietary intake during a short fasting. This method measures both 25(OH)D2 and 25(OH)D3 equally well and was compared with liquid chromatography tandem mass spectroscopy with excellent correlation (25). The lower limit of detection was 12.5 nmol/liter (5 ng/ml), and the intra- and interassay coefficients of variation 5.0–10 and 10%–15%, respectively. The reference range was 50–250 nmol/liter (20–100 ng/ml).
Definitions
Certain definitions pertinent to U.S., or more specific regional descriptions, are summarized here. GED indicates graduate equivalency degree, a high school diploma alternative for individuals who do not graduate high school. Healthy Start is perinatal, state-funded insurance for women who are ineligible for other insurance programs; it is frequently used by women of illegal immigration status. The Special Supplemental Nutrition Program for Women, Infants, and Children provides food and nutrition counseling for low income families with children younger than 5 yr. In Massachusetts, applicant income must fall at or below 185% of the federal poverty guidelines.
Outcome measures and data analysis
The dependent variable was maternal vitamin D deficiency, defined as serum 25(OH)D less than 37.5 nmol/liter (15 ng/ml), per the Centers for Disease Control and Prevention definition for adults (26). Recent research has found 25(OH)D less than 37.5 to be an unacceptably low state of deficiency and that less than 50 nmol/liter is considered to be vitamin D deficiency and 51–74 nmol/liter as vitamin D insufficiency (3,7,8,11,12). Race/ethnicity and skin color were analyzed as two variables because skin color by ethnicity alone can vary from white to dark brown, and skin pigmentation affects vitamin D synthesis (3). Skin color (black, brown, or white) was based on the skin type matrix of Fitzpatrick et al. (27). Prenatal vitamin use was analyzed by any reported use in each trimester (data in Table 1) as well as by frequency of use in each trimester; neither measure was associated with type of delivery. Body mass index (BMI) information before pregnancy was obtained from the medical record. Continuous values of BMI were categorized for analysis (17 to <25, 25 to <30, 30 to <35, 35+ kg/m2) according to World Health Organization ranges (http://www.who.int/bmi/index.jsp?intoPage=intro3.html). Reasons for cesarean were obtained from the mother’s medical record. Response frequencies for categorical variables are presented in Table 1. Continuous variables (maternal age, BMI, and 25(OH)D level) are presented as medians with binomially obtained 95% confidence intervals (CI) in Table 1.
Table 1.
Characteristics of study sample by delivery mode
| Vaginal, n = 210, n (%) | Primary cesarean section, n = 43, n (%) | P value | |
|---|---|---|---|
| Median age, yr (95% CI) | 26.2 (24.8–27.1) | 24.8 (22.8–28.1) | 0.579a |
| Race/ethnicity | 0.006 | ||
| Black non-Hispanic | 81 (86) | 13 (14) | |
| Caucasian non-Hispanic | 18 (62) | 11 (38) | |
| Hispanic | 111 (85) | 19 (15) | |
| Skin color | 0.734 | ||
| Black | 72 (83) | 15 (17) | |
| Brown | 79 (85) | 14 (15) | |
| White | 57 (80) | 14 (20) | |
| Season of birth | 0.648 | ||
| Spring | 53 (80) | 13 (20) | |
| Summer | 43 (83) | 9 (17) | |
| Fall | 47 (89) | 6 (11) | |
| Winter | 67 (82) | 15 (18) | |
| Infant gender | 0.255 | ||
| Male | 107 (80) | 26 (20) | |
| Female | 103 (86) | 17 (14) | |
| Maternal birthplace | 0.023 | ||
| United States | 141(87) | 21 (13) | |
| Not United States | 69 (76) | 22 (24) | |
| Median maternal BMI, kg/m2 | 25.0 | 24.0 | 0.634a |
| 95% CI | (24.0–26.1) | (23.1–25.8) | |
| Maternal BMI, kg/m2 | 0.281 | ||
| 17 to <25 | 101 (80) | 26 (20) | |
| 25 to <30 | 56 (86) | 9 (14) | |
| 30-<35 | 29 (91) | 3 (12) | |
| 35+ | 14 (74) | 5 (26) | |
| Education | 0.484 | ||
| Less than high school | 91 (82) | 20 (18) | |
| High school/GED | 67 (87) | 10 (13) | |
| More than high school | 51 (80) | 13 (20) | |
| Insurance status | 0.389 | ||
| Private | 20 (71) | 8 (29) | |
| Public | 167 (84) | 31 (16) | |
| Healthy Start | 15 (83) | 3 (17) | |
| Other | 7 (88) | 1 (13) | |
| WIC status | 0.236 | ||
| No | 33 (77) | 10 (23) | |
| Yes | 176 (84) | 33 (16) | |
| Marital status | 0.421 | ||
| Single/divorced/widowed | 147 (82) | 33 (18) | |
| Married | 61 (86) | 10 (14) | |
| Any prenatal vitamin use | |||
| First trimester | 0.499 | ||
| No | 48 (80) | 12 (20) | |
| Yes | 160 (84) | 31 (16) | |
| Second trimester | 0.978 | ||
| No | 24 (83) | 5 (17) | |
| Yes | 185 (83) | 38 (17) | |
| Third trimester | 0.978 | ||
| No | 24 (83) | 5 (17) | |
| Yes | 185 (83) | 38 (17) | |
| (Continued) |
Table 1A.
Continuous
| Vaginal, n = 210, n (%) | Primary cesarean section, n = 43, n (%) | P value | |
|---|---|---|---|
| Calcium supplements | 0.857 | ||
| Never | 145 (83) | 29 (17) | |
| Occasionally | 23 (79) | 6 (21) | |
| Almost daily | 41 (84) | 8 (16) | |
| Drank milk in pregnancy | 0.083b | ||
| Yes | 177 (81) | 41 (19) | |
| No | 31 (94) | 2 (6) | |
| Ever used sunscreen | 0.073 | ||
| Yes | 67 (77) | 20 (23) | |
| No | 141 (86) | 23 (14) | |
| Drank alcohol in pregnancy | 0.039 | ||
| Yes | 11 (65) | 6 (35) | |
| No | 198 (84) | 37 (16) | |
| Median maternal 25(OH)D, nmol/liter | 62.5 | 45.0 | 0.007a |
| 95% CI | (57.4–68.2) | (36.5–62.0) | |
| Maternal 25(OH)D, nmol/liter | 0.012 | ||
| 25(OH)D, ≥37.5 | 168 (86) | 27 (14) | |
| 25(OH)D, <37.5 | 41 (72) | 16 (28) |
Not all cells total 253 because of missing data. WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
P value determined by Wilcoxon rank sum test. 95% CI for mothers’ median age, BMI; 25(OH)D is binomially obtained.
Fisher’s exact test used where expected cell value was less than 5.
The statistical significance of differences in maternal factors associated with cesarean delivery was assessed using Pearson’s χ2 test. Multivariate logistic regression analysis tested all variables with P < 0.25 in univariate analysis. Backward selection techniques were used to derive the final model, which maintained variables with P ≤ 0.05. Statistical analyses were conducted using Stata/SE 9.2 for Windows (Stata Corp., College Station, TX). The study obtained approval from the Boston University Medical Center Institutional Review Board, and women signed informed consent before participating.
Results
Between March 21, 2005, and March 20, 2007, we enrolled 253 women, of whom 43 (17%) had a primary cesarean section. In this same time period, 370 women refused enrollment, primarily because they did not want blood drawn on themselves or their infant. Based on a random sample of 95 refusers, 51% of enrolled women were Hispanic, whereas only 30% of women who refused had Hispanic race/ethnicity recorded in their medical record (P < 0.001). This difference probably arose from the practice of asking women who are enrolled in the study their race and whether they are Hispanic, which is not done for the record. No other significant differences existed between consented and refusing women with regard to age, infant birth weight, or gestational age. The method of delivery did not differ between mothers who enrolled in the study and those who refused (76% vaginal delivery, and 24% cesarean section delivery, both groups).
Of the 277 women enrolled, 210 had vaginal deliveries and 67 had cesarean deliveries, of which 43 were primary cesareans. This analysis was limited to women with vaginal deliveries or primary cesareans. Thus, of the 253 eligible women enrolled, 43 (17%) had a primary cesarean. Reasons for cesarean included failure to progress (17 of 43); nonreassuring fetal tracing (11 of 43); malpresentation (such as breech) (six of 43); and three each of cephalopelvic disproportion, variable fetal heart rate, and other.
We found that 28% of women with serum 25(OH)D less than 37.5 nmol/liter had a primary cesarean section, compared with only 14% of women with 25(OH)D 37.5 nmol/liter or greater [P = 0.012; unadjusted odds ratio (OR) = 2.43; 95% CI 1.20–4.92]. In addition, women who had cesareans had a lower median 25(OH)D level than women who delivered vaginally (45.0 vs. 62.5 nmol/liter, P = 0.007). Compared with women who had vaginal births, women who had cesareans were also significantly more likely to be Caucasian/non-Hispanic than black and/or Hispanic (P = 0.006); OR 3.81; 95% CI 1.47–9.86), to be U.S. born (P = 0.023; OR 2.14; 95% CI 1.10–4.16), and to have used alcohol in pregnancy (P = 0.039; OR 2.92; 95% CI 1.02–8.38) (Table 1).
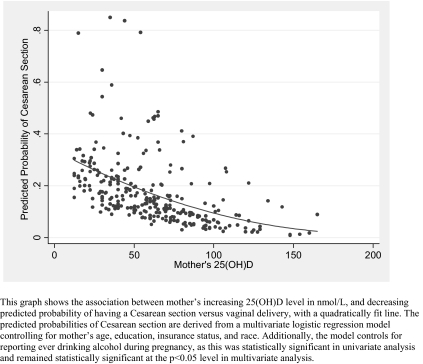
In multivariate logistic regression analysis controlling for race, age, education level, insurance status, maternal birthplace, and alcohol use (Table 2), women with vitamin D deficiency (<37.5 nmol/liter) were almost 4 times as likely to have a primary cesarean section as women without deficiency (OR 3.84 95% CI 1.71–8.62). Caucasian women and those who reported any alcohol use during pregnancy also had increased likelihood of primary cesarean. Maternal birthplace was no longer statistically significant. Figure 1 shows the association between mother’s increasing 25(OH)D level in nanomoles per liter and decreasing predicted probability (from multivariate analysis) of having a Cesarean section vs. vaginal delivery. Thus, women with the highest serum 25(OH)D had the lowest probability of requiring a cesarean section.
Table 2.
Multivariate logistic regression analysis: factors associated with having primary cesarean section delivery, n = 250a
| Adjusted OR | 95% CI | P value | |
|---|---|---|---|
| Mother’s race/ethnicity | |||
| Black, non-Hispanic | Ref | ||
| Caucasian, non-Hispanic | 4.79 | 1.60–14.4 | 0.005 |
| Hispanic | 1.16 | 0.48–2.88 | 0.733 |
| Mother’s 25(OH)D, nmol/liter | |||
| ≥37.5 | Ref | ||
| <37.5 | 3.84 | 1.71–8.62 | 0.001 |
| Used alcohol during pregnancy | |||
| No | Ref | ||
| Yes | 3.21 | 1.02–10.11 | 0.046 |
| Mother’s educational status | |||
| Less than high school or GED | Ref | ||
| High school or GED | 0.63 | 0.25–1.56 | 0.317 |
| More than high school | 0.75 | 0.27–2.11 | 0.588 |
| Mother’s insurance status | |||
| Private | Ref | ||
| Public | 0.49 | 0.16–1.56 | 0.230 |
| Healthy start | 0.87 | 0.16–4.83 | 0.874 |
| Other | 0.29 | 0.03–3.13 | 0.307 |
| Mother’s age, yr | 0.97 | 0.91–1.04 | 0.364 |
The model is adjusted for all variables presented. Ref, Reference category.
Women with missing data were excluded from multivariate analysis.
Figure 1.
Mother’s 25(OH)D level (nanomoles per liter) and predicted probability of primary cesarean section delivery.
Discussion
In our analysis, women who were severely vitamin D deficient [25(OH)D <37.5 nmol/liter] at the time of delivery had almost 4 times the odds of cesarean birth than women who were not deficient. One explanation for our findings is the fact that skeletal muscle contains the vitamin D receptor (8,11). Vitamin D deficiency has been associated with proximal muscle weakness (11) as well as suboptimal muscle performance and strength (5,11,12,13,14,15,16). Moreover, vitamin D deficiency is a possible risk factor for preeclampsia (9,28).
Serum calcium status, which is regulated by vitamin D, plays a role in smooth muscle function in early labor (23,29). Papandreou et al. (23) reported significantly higher serum calcium levels in pregnant women at the time of vaginal delivery compared with term women not in labor or women who did not labor but delivered by scheduled cesarean. It was speculated that the higher serum calcium levels played a role in the mechanism of initiation of labor. Because vitamin D is critically important for the maintenance of calcium homeostasis, it is possible that vitamin D deficiency, which causes a slight lowering of the serum calcium, is related to both skeletal muscle and smooth muscle strength and may play a role in initiation of early labor. It is also possible that vitamin D deficiency might be related to specific types of cesareans (such as cephalopelvic disproportion or failure to progress) than to others (such as breech), although we did not have a large enough sample to be able to analyze this. This would be a critical area for future research.
There are other potential explanations for the association of vitamin D deficiency and cesarean section. The simplest explanation is that the iv hydration would have diluted the blood and give an artificially lower level of 25(OH)D. However, the amount of iv fluids relative to the blood loss is essentially the same. We did a subset analysis of five women in whom we obtained serum 25(OH)D before and after the cesarean section, and they were statistically the same, i.e. the 25(OH)D before surgery was 80 ± 25 nmol/liter and after surgery 97 ± 33 nmol/liter P > 0.1. Vitamin D status is linked to immune status (30,31). Certain infections have been associated with preeclampsia (32), and preeclampsia in turn increases the odds of cesarean (33). Vitamin D deficiency may thus be a marker for a compromised immune system and an associated, higher risk of cesarean.
A study performed in 1994–1995 by Brunvand et al. (34) found no association between vitamin D deficiency at the time of delivery and obstructed labor in a case control study of Indian women giving birth in Karachi. Their findings bear little relevance for the present study however; outcomes were measured only for cesareans due to cephalopelvic disproportion; the sample consisted of largely undernourished impoverished women, and 71% of study participants were severely vitamin D deficient [25(OH)D <30 nmol/liter]. In addition, the paper does not satisfactorily clarify the use of the term cephalopelvic disproportion (as opposed, for example, to alternative, yet closely related reasons such as fetal distress). The specific validity of the term cephalopelvic disproportion has been questioned for more than 50 yr (35,36).
We also found some interesting trends regarding other interactions in our baseline data (Table 1). Whereas skin color, independent of race/ethnicity and based on the skin type matrix of Fitzpatrick et al. (27) was not related to risk of cesarean delivery, women who self-identified as being non-Hispanic whites had a significantly elevated risk of cesarean delivery; 38% of non-Hispanic whites underwent primary cesareans, compared with 14% of non-Hispanic blacks, and 15% of Hispanics (P = 0.006). This is not reflective of national data, in which the primary cesarean rate among black, non-Hispanic primiparas is approximately one percentage point higher than the rate in Hispanic and white, non-Hispanic women (37).
Drinking milk in pregnancy and reported use of sunscreen were both marginally related with an increased risk of cesarean, but both these risks disappeared in the multivariate model and were probably a result of small sample size or confounding variables. On the other hand, maternal report of alcohol use during pregnancy was strongly associated with an increased risk of cesarean even after multivariate analysis, an unanticipated finding that clearly requires further investigation.
Maternal vitamin D deficiency is a widespread public health problem. Lee et al. (38) reported that 50% of mothers and 65% of newborns infants were severely vitamin D deficient [25(OH)D <30 nmol/liter] at the time of birth despite the fact that the mother was taking a prenatal vitamin containing 400 IU of vitamin D and drinking two glasses of vitamin D fortified milk (100 IU per 8 oz glass). This mirrors the observation of Hollis and Wagner (39) and Bodnar et al. (40), who found a high incidence of vitamin D deficiency in pregnant and lactating women. Whereas other factors, such as increased liability for obstetricians (41), undoubtedly play a role in the staggering rise in primary cesareans, the rate of primary cesareans with no medical or obstetrical indication is also rising; the current U.S. rate of primary cesareans with no reported medical or obstetrical indication is between 3 and 7% (19). As Declercq et al. (37) noted in a study to examine reasons for cesarean increases, apparent risk factors remained stable: shifts in primary cesarean rates during the study period were not related to shifts in maternal risk profiles. A randomized clinical trial is now needed to determine whether adequate vitamin D supplementation during pregnancy to raise blood levels of 25(OH)D above at least 37.5 nmol/liter can reduce the cesarean section rate and whether increasing it above 75 nmol/liter provides any additional reduction as suggested by our data.
Footnotes
This work was supported by the Department of Health and Human Services, Bureau of Maternal Child Health (Grant R40MC03620-02-00) and the Department of Agriculture Cooperative State Research, Education, and Extension Service Award 2005-35200-15620.
Disclosure Statement: A.M., S.D.M., T.C.C., and H.B. have nothing to declare. M.F.H. consults for Merck, Procter & Gamble, and Quest Diagnostics and received lecture fees from Merck and Procter & Gamble.
First Published Online December 23, 2008
Abbreviations: BMI, Body mass index; CI, confidence interval; GED, graduate equivalency degree; 25(OH)D, 25-hydroxyvitamin D; OR, odds ratio.
References
- Loudon I 1986 Deaths in childbed from the eighteenth century to 1935. Med Hist 30:1–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sewell JE 1993 Cesarean delivery: a brief history. A brochure to accompany an exhibition on the history of cesarean section at the National Library of Medicine. American College of Obstetricians and Gynecologists, Washington, DC [Google Scholar]
- Holick MF 2006 Resurrection of vitamin D deficiency and rickets. J Clin Invest 116:2062–2072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wharton B, Bishop N 2003 Rickets. Lancet 362:1389–1400 [DOI] [PubMed] [Google Scholar]
- Hanley DA, Davison KS 2005 Vitamin D insufficiency in North America. J Nutr 135:332–337 [DOI] [PubMed] [Google Scholar]
- Holick MF 2003 Vitamin D: a millennium perspective. J Cell Biochem 88:296–307 [DOI] [PubMed] [Google Scholar]
- Holick MF 2005 The vitamin D epidemic and its health consequences. J Nutr 135:2739S–2748S [DOI] [PubMed] [Google Scholar]
- Holick MF 2007 Vitamin D deficiency. N Engl J Med 357:266–281 [DOI] [PubMed] [Google Scholar]
- Bodnar LM, Catov JM, Simhan HN, Holick MF, Powers RW, Roberts JM 2007 Maternal vitamin D deficiency increases the risk of preeclampsia. J Clin Endocrinol Metab 92:3517–3522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hypponen E, Hartikainen AL, Sovio U, Jarvelin MR, Pouta A 2007 Does vitamin D supplementation in infancy reduce the risk of pre-eclampsia? Eur J Clin Nutr 61:1136–1139 [DOI] [PubMed] [Google Scholar]
- Bischoff-Ferrari H, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B 2006 Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr 84:18–28 [DOI] [PubMed] [Google Scholar]
- Holick MF 2004 Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr 80(Suppl 6):1678S–1688S [DOI] [PubMed] [Google Scholar]
- Torres CF, Forbes GB, Decancq GH 1986 Muscle weakness in infants with rickets: distribution, course, and recovery. Pediatr Neurol 2:95–98 [DOI] [PubMed] [Google Scholar]
- Staud R 2005 Vitamin D: more than just affecting calcium and bone. Curr Rheumatol Rep 7:356–364 [DOI] [PubMed] [Google Scholar]
- Molgaard C, Michaelsen KF 2003 Vitamin D and bone health in early life. Proc Nutr Soc 62:823–828 [DOI] [PubMed] [Google Scholar]
- Siddiqui TS, Rai MI 2005 Presentation and predisposing factors of nutritional rickets in children of Hazara Division. J Ayub Med Coll Abbottabad 17:29–32 [PubMed] [Google Scholar]
- Stalberg K, Bodestedt A, Lyrenas S, Axelsson O 2006 A narrow pelvic outlet increases the risk for emergency cesarean section. Acta Obstet Gynecol Scand 85:821–824 [DOI] [PubMed] [Google Scholar]
- Hamilton BE, Martin JA, Ventura SJ 2006 Births: preliminary data for 2005. Natl Vital Stat Rep 55:1–18 [PubMed] [Google Scholar]
- Menacker F, Declercq E, Macdorman MF 2006 Cesarean delivery: background, trends, and epidemiology. Semin Perinatol 30:235–241 [DOI] [PubMed] [Google Scholar]
- Liu S, Rusen ID, Joseph KS, Liston R, Kramer MS, Wen SW, Kinch R 2004 Recent trends in cesarean delivery rates and indications for cesarean delivery in Canada. J Obstet Gynaecol Can 26:735–742 [DOI] [PubMed] [Google Scholar]
- Kolas T, Hofoss D, Daltveit AK, Nilsen ST, Henriksen T, Hager R, Ingemarsson I, Oian P 2003 Indications for cesarean deliveries in Norway. Am J Obstet Gynecol 188:864–870 [DOI] [PubMed] [Google Scholar]
- Gaunekar NN, Crowther CA 2004 Maintenance therapy with calcium channel blockers for preventing preterm birth after threatened preterm labour. Cochrane Database Syst Rev CD004071 [DOI] [PubMed] [Google Scholar]
- Papandreou L, Chasiotis G, Seferiadis K, Thanasoulias NC, Dousias V, Tsanadis G, Stefos T 2004 Calcium levels during the initiation of labor. Eur J Obstet Gynecol Reprod Biol 115:17–22 [DOI] [PubMed] [Google Scholar]
- Chen TC, Turner AK, Holick MF 1990 A method for the determination of the circulating concentration of 25-hydroxyvitamin D. J Nutr Biochem 1:315–319 [DOI] [PubMed] [Google Scholar]
- Holick MF, Siris ES, Binkley N, Beard MK, Khan A, Katzer JT, Petruschke RA, Chen E, de Papp AE 2005 Prevalence of vitamin D inadequacy among postmenopausal North American women receiving osteoporosis therapy. J Clin Endocrinol Metab 90:3215–3224 [DOI] [PubMed] [Google Scholar]
- Standing Committee on the Scientific Evaluation of Dietary Reference Intakes, Food and Nutrition Board, Institute of Medicine 1997 Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride: National Academy of Sciences, Washington, DC [Google Scholar]
- Fitzpatrick TB, Wolf K, Johnson RA 2000 Color atlas and synopsis of clinical dermatology: common and serious diseases. 4th ed. Columbus, OH: McGraw-Hill Professional Publishing [Google Scholar]
- Hypponen E 2005 Vitamin D for the prevention of preeclampsia? A hypothesis. Nutr Rev 63:225–232 [DOI] [PubMed] [Google Scholar]
- Hofmeyr GJ, Atallah AN, Duley L 2006 Calcium supplementation during pregnancy for preventing hypertensive disorders and related problems. Cochrane Database Syst Rev CD001059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams JS, Hewison M 2008 Unexpected actions of vitamin D: new perspectives on the regulation of innate and adaptive immunity. Nat Clin Pract Endocrinol Metab 4:80–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams JS, Liu PT, Chun R, Modlin RL, Hewison M 2007 Vitamin D in defense of the human immune response. Ann NY Acad Sci 1117:94–105 [DOI] [PubMed] [Google Scholar]
- Conde-Agudelo A, Villar J, Lindheimer M 2008 Maternal infection and risk of preeclampsia: systematic review and metaanalysis. Am J Obstet Gynecol 198:7–22 [DOI] [PubMed] [Google Scholar]
- Vanek M, Sheiner E, Levy A, Mazor M 2004 Chronic hypertension and the risk for adverse pregnancy outcome after superimposed pre-eclampsia. Int J Gynaecol Obstet 86:7–11 [DOI] [PubMed] [Google Scholar]
- Brunvand L, Shah SS, Bergstrom S, Haug E 1998 Vitamin D deficiency in pregnancy is not associated with obstructed labor. A study among Pakistani women in Karachi. Acta Obstet Gynecol Scand 77:303–306 [PubMed] [Google Scholar]
- Lydon-Rochelle MT, Holt VL, Cardenas V, Nelson, JC, Easterling TR, Gardella C, Callaghan WM 2005 The reporting of pre-existing maternal medical conditions and complications of pregnancy on birth certificates and in hospital discharge data. Am J Obstet Gynecol 193:125–134 [DOI] [PubMed] [Google Scholar]
- Gibberd GF 1953 Can we correctly assess cephalopelvic disproportion? Am J Obstet Gynecol 65:1284–1292 [DOI] [PubMed] [Google Scholar]
- Declercq E, Menacker F, Macdorman M 2006 Maternal risk profiles and the primary cesarean rate in the United States, 1991–2002. Am J Public Health 96:867–872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JM, Smith JR, Philipp BL, Chen TC, Mathieu J, Holick MF 2007 Vitamin D deficiency in a healthy group of mothers and newborn infants. Clin Pediatr (Phila) 46:42–44 [DOI] [PubMed] [Google Scholar]
- Hollis BW, Wagner CL 2004 Assessment of dietary vitamin D requirements during pregnancy and lactation. Am J Clin Nutr 79:717–726 [DOI] [PubMed] [Google Scholar]
- Bodnar LM, Simhan HN, Powers RW, Frank MP, Cooperstein E, Roberts JM 2007 High prevalence of vitamin D insufficiency in black and white pregnant women residing in the northern United States and their neonates. J Nutr 137:447–452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murthy K, Grobman WA, Lee TA, Holl JL 2007 Association between rising professional liability insurance premiums and primary cesarean delivery rates. Obstet Gynecol 110:1264–1269 [DOI] [PubMed] [Google Scholar]