Abstract
The potential use of Yersinia pestis as a bioterror agent is a great concern. Development of a stable powder vaccine against Y. pestis and administration of the vaccine by minimally invasive methods could provide an alternative to the traditional liquid formulation and intramuscular injection. We evaluated a spray-freeze-dried powder vaccine containing a recombinant F1-V fusion protein of Y. pestis for vaccination against plaque in a mouse model. Mice were immunized with reconstituted spray-freeze-dried F1-V powder via intramuscular injection, microneedle-based intradermal delivery, or noninvasive intranasal administration. By intramuscular injection, the reconstituted powder induced serum antibody responses and provided protection against lethal subcutaneous challenge with 1,000 50% lethal doses of Y. pestis at levels equivalent to those elicited by unprocessed liquid formulations (70 to 90% protection). The feasibility of intradermal and intranasal delivery of reconstituted powder F1-V vaccine was also demonstrated. Overall, microneedle-based intradermal delivery was shown to be similar in efficacy to intramuscular injection, while intranasal administration required an extra dose of vaccine to achieve similar protection. In addition, the results suggest that seroconversion against F1 may be a better predictor of protection against Y. pestis challenge than seroconversion against either F1-V or V. In summary, we demonstrate the preclinical feasibility of using a reconstituted powder F1-V formulation and microneedle-based intradermal delivery to provide protective immunity against plague in a mouse model. Intranasal delivery, while feasible, was less effective than injection in this study. The potential use of these alternative delivery methods and a powder vaccine formulation may result in substantial health and economic benefits.
Plague caused by gram-negative Yersinia pestis is one of the most deadly infectious diseases of animals and humans. Outbreaks of plague have caused the deaths of millions of people throughout human history. The pneumonic form of plague is the most dangerous, due to rapid onset and progression and the aerosol spread of the disease. Without proper early treatment, pneumonic plague can lead to mortality in close to 100% of cases (36).
Throughout recorded human history, there were three plague pandemics that caused countless human deaths (20). The use of plague as a weapon also has a long history. Starting from the 12th century, there were many cases of using the bodies of plague victims to defeat enemies during wars. Most recently, during World War II, the Japanese army dropped Y. pestis-infected fleas over populated areas of China, causing plague outbreaks (20).
Plague has been classified by the U.S. Centers for Disease Control and Prevention as a “category A” agent due to its potential threat to national security. Currently, however, there is no commercially available vaccine against plague approved for human use in the United States. The original plague vaccine licensed for use in the United States was a killed whole-cell bacterial vaccine. It provided some protection against bubonic plague, but not against aerosol exposure to Y. pestis (6, 10, 33, 40). Manufacture of the vaccine ceased in 1998 due to multiple side effects and short-term effectiveness.
The potential use of Y. pestis as a bioweapon, combined with the threat of antibiotic-resistant plague (13), makes the development of a safe and effective human plague vaccine a high priority. Conventional vaccines are formulated as liquids, which generally require refrigeration for storage and distribution. In recent years, there has been growing interest in powder formulations for extended storage stability and increased shelf life (5, 12, 19). We previously reported intranasal (i.n.) delivery of dry powder influenza vaccine in a rat model (17). The influenza vaccine powder formulation was shown to be more stable than the liquid vaccine and to induce increased systemic and nasal mucosal immune responses. We also reported that rabbits immunized nasally with a spray-freeze-dried (SFD) anthrax recombinant protective antigen (rPA) powder vaccine formulation were completely protected against lethal inhalational anthrax, while a liquid preparation of the same vaccine provided only 63 to 67% protection by the nasal route (18, 28).
The most common vaccine delivery route is intramuscular (i.m.) injection. Alternative delivery methods, such as the intradermal (i.d.) and i.n. routes, have attracted attention recently. The skin is a favorable site for vaccine delivery due to a rich population of antigen-presenting cells. I.d. delivery of vaccines has been shown to provide dose-sparing effects for rabies, hepatitis B, influenza, and rPA vaccines (1, 7, 8, 24, 28, 37). I.n. delivery has been shown to induce mucosal immunity (17, 31). In addition, it offers the advantages of noninvasive delivery and ease of use, reducing the need for highly trained health personnel to administer the vaccine.
In the current study, we evaluated the immunogenicity and protective efficacy of an SFD powder vaccine formulation of a recombinant F1-V fusion protein of Y. pestis in a mouse model. The recombinant fusion protein was composed of the F1 subunit, a capsule protein of Y. pestis, and the low-calcium-response V subunit (LcrV), or V antigen. LcrV caps the tips of the injectisome needles of the type III secretion system (30).
MATERIALS AND METHODS
Recombinant F1-V fusion protein and preparation of liquid and powder formulations.
The recombinant F1-V fusion protein of Y. pestis was obtained through the Biodefense and Emerging Infections Research Resources Repository, NIAID, NIH. The sample consisted of a monomer-enriched recombinant protein made from Escherichia coli (NR-2561) containing about 70% monomeric, 20% dimeric, and 10% multimeric forms of F1-V at pH 9.9 (product information sheet for NR-2651; BEI Resources). It is expected that at pH 10 F1-V would not be stable in solution form under refrigeration. Also, in its dried form, it would have decreased shelf stability. Therefore, it was deemed advisable to adjust the pH of the solution to 7.5. A direct change of the solution pH to 7.5 resulted in excessive aggregation of F1-V that included the formation of higher-order soluble and insoluble aggregates. The higher the heterogeneity within the product, the more difficult it is to characterize the various forms present, so it was important to minimize the heterogeneity in the F1-V solution so as to be able to characterize the formulation more thoroughly, as required by the various regulatory agencies. Therefore, it was necessary to refold F1-V with appropriate excipients, so that it would retain its predominant monomeric form. To carry out this refolding, F1-V was denatured using 8 M urea and refolded under refrigeration in the presence of 50 mM MgCl2, 0.1% Tween 80 in 20 mM Tris buffer at pH 7.5 using diafiltration over a 24-hour period. Diafiltration was carried out using an Amicon stirred cell (model 8040), along with a 10,000-molecular-weight cutoff membrane filter at a pressure of 10 lb/in2. The recovery of F1-V was approximately 70%. The refolded F1-V was used for further processing. Formulations were prepared for i.m. and i.d. administration so that each milliliter of the liquid and the reconstituted powder solutions contained 0.2 mg of F1-V, 0.7% (wt/vol) Tween 80, 16.7 mM MgCl2, 27.8 mg mannitol, 3.1 mg trehalose. Additionally, selected samples contained aluminum hydroxide adjuvant (Alhydrogel; Brenntag Biosector, Frederikssund, Denmark). These samples contained 1 mg aluminum per ml of solution (50 μg of Alhydrogel per 10 μg of F1-V). Formulations were prepared for i.n. administration so that each milliliter of the liquid and the reconstituted powder solutions contained 0.33 mg of F1-V, 1.1% (wt/vol) Tween 80, 27.8 mM MgCl2, 46.3 mg mannitol, 5.2 mg trehalose, and 1.3 mg lipopolysaccharide (LPS) (InvivoGen, San Diego, CA). Nasal groups contained LPS, a Toll-like receptor 4 agonist, as an adjuvant, as in previous studies, since aluminum hydroxide is not an appropriate adjuvant for nasal delivery (29).
The endotoxin limit of the F1-V fusion protein specified by the vendor (BEI Resources) was 5 endotoxin units/ml. The measured endotoxin level of F1-V fusion protein provided by the vendor was 0.44 endotoxin units/ml. The actual endotoxin level used in this study was even lower because of dilution during processing/delivery procedures.
SFD F1-V powders were prepared by spraying the liquid formulation, using a BD Accuspray nozzle, in liquid N2 contained in a glass container. The glass container was then transferred to a shelf lyophilizer (FTS Systems, Stone Ridge, NY). The samples were equilibrated at a shelf temperature of −40°C until most of the liquid N2 vaporized. Primary drying was carried out at a shelf temperature of −40°C for 5 min and at −20°C for 180 min. Secondary drying was carried out at shelf temperatures of 0°C for 5 min and 20°C for 360 min. Following secondary drying, the samples were held at 4°C until they were removed from the lyophilizer. Drying was performed at a chamber vacuum of 20 Pa, while the condenser was maintained at −45°C.
Animals and immunizations.
The mouse study was conducted in accordance with U.S. Department of Agriculture and National Institutes of Health guidelines for the care and use of animals and under protocols approved by an institutional animal care and use committee. The mice were housed at BD Technologies (Research Triangle Park, NC) for immunizations and at the U.S. Army Medical Research Institute for Infectious Diseases (USAMRIID) (Fort Detrick, MD) for subcutaneous (s.c.) challenge.
Female Swiss Webster mice (Charles River Laboratories, Wilmington, MA) were immunized with 10 μg of F1-V fusion protein (NIAID) via either i.m. injection, i.d. injection, or i.n. delivery, as shown in Table 1. The SFD powder formulations were reconstituted using water for injection immediately before delivery to the animals. I.m. injections were delivered at the quadriceps using a 30-gauge needle and a 1-ml syringe (BD, Franklin Lakes, NJ). I.d. injections were performed using a 34-gauge stainless steel microneedle (1, 27, 28) and a 1-ml syringe (BD, Franklin Lakes, NJ). Two injections of 25 μl, each at a different site, were administered for the i.m. and i.d. groups. For i.n. delivery groups, 30 μl of liquid formulations, each at 15 μl, was applied to each nostril of anesthetized mice via a pipette tip.
TABLE 1.
Experimental outline
| Dosing routea | Group | No. of doses | Formulation type | F1-V dose (μg) | Adjuvant |
|---|---|---|---|---|---|
| i.m. | 1 | 2 | SFD | 10 | AL |
| 2 | 2 | Liquid | 10 | AL | |
| 3 | 2 | Liquid | 10 | ||
| i.d. | 4 | 2 | SFD | 10 | AL |
| 5 | 2 | Liquid | 10 | AL | |
| 6 | 2 | Liquid | 10 | ||
| i.n. | 7 | 2 | SFD | 10 | LPS |
| 8 | 2 | Liquid | 10 | LPS | |
| 9 | 2 | Liquid | 10 | ||
| i.n. | 10 | 3 | SFD | 10 | LPS |
| 11 | 3 | Liquid | 10 | LPS | |
| 12 | 3 | Liquid | 10 | ||
| Naive | 13 |
All groups received mannitol/trehalose/Tween 80/MgCl2 as excipients except the naive group. AL, Alhydrogel [containing 0.3% Al(OH)3/dose]. LPS, 40μg/dose; SFD powder was reconstituted prior to injection.
All immunizations were performed on day 0 and day 28, with the exception of a set of i.n. delivery groups (groups 10 to 12), which were immunized on day 0, day 14, and day 28. Blood samples were collected on day 0, day 28, and day 42.
ELISA.
Anti-F1-V fusion protein antibody titers were determined by enzyme-linked immunosorbent assay (ELISA). Maxisorp 96-well plates (Nalgene Nunc, Rochester, NY) were coated with 100 μl of 1-μg/ml F1-V fusion protein at 4°C overnight and then blocked with phosphate-buffered saline-Tween 20 (Sigma) containing 5% nonfat dry milk at 37°C for 1 h. After three washes with wash solution (Sigma), double serial dilutions of sera (100 μl/well) were added and incubated at 37°C for 1 h. After being washed, the plates were incubated at 37°C for 45 min with horseradish peroxidase-conjugated goat anti-mouse immunoglobulin G (IgG) (Southern Biotechnology Associates, Inc., Birmingham, AL). The plates were developed by incubating them with 3,3′,5,5′-tetramethyl benzidine substrate (Sigma) for 30 min at room temperature and then were stopped by the addition of 0.5 M H2SO4. The plates were read at 450 nm (Tecan U.S. Inc., Research Triangle Park, NC). Endpoint titers were defined as the highest reciprocal dilution of sera yielding an optical density at 450 nm at least three times the background obtained from serum samples from unimmunized mice. All samples and controls were analyzed in duplicate.
F1 and V proteins were kindly provided by Bradford Powell of USAMRIID. Anti-F1 and anti-V antibody titers were determined using the same ELISA procedures, with the exception of coating antigens; for anti-F1 antibody titer determination, each well of the plates was coated with 100 μl of 1-μg/ml F1 protein. For anti-V antibody detection, 100 μl of 1-μg/ml V protein was used as the coating antigen. The endpoint titers for anti-V antibody response were determined from only selected groups. The percentage of seroconversion was based on an ELISA result of a serum IgG titer of ≥50.
S.c. challenge.
Mice were challenged with a mean dose of 1,000 times the 50% lethal dose (LD50) (2,000 CFU) of Y. pestis strain CO92 per mouse via the s.c. route 56 days after the mice were primed (39).
Statistics.
Due to the nature of the data distribution, parametric statistical analysis methods were not appropriate. Instead, a rank-based nonparametric method was used for distribution-free analysis. Pairwise comparisons among treatment groups of interest were made using a Behrens-Fisher rank-based nonparametric test procedure, with adjustment made for multiple comparisons. The test was implemented with the R software package (The R Foundation for Statistical Computing, Vienna, Austria, v. 2.6.0) using the NPMC library (Helms and Munzel, v. 1.0-6).
RESULTS
Serum antibody response via the i.m. route.
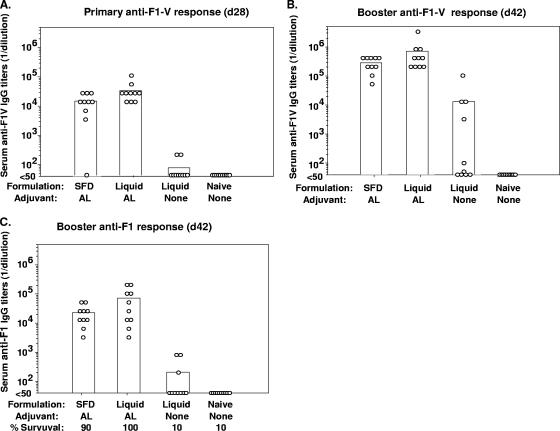
We initially examined the i.m. route to evaluate the potency of reformulated SFD powder F1-V vaccine. SFD powder was reconstituted with water for injection just before injection and was compared to a standard liquid formulation that was not subjected to the SFD process. After a single immunization, the reconstituted SFD vaccine stimulated a high level of antigen-specific antibodies that did not differ significantly (P > 0.05) from the response induced by the unprocessed liquid vaccine with adjuvant (Fig. 1A). I.m. injection of the liquid formulation without adjuvant induced very little detectable anti-F1-V antibody. Both reconstituted SFD and the standard liquid formulation induced an elevated antibody response following the second vaccination, with similar anti-F1-V titers at day 42 (Fig. 1B) (P > 0.05). Eight of 10 mice immunized with F1-V without adjuvant generated a detectable increase in antigen-specific antibodies; however, this response was on average 80-fold lower and more variable than in the groups immunized with F1-V containing adjuvant.
FIG. 1.
Serum F1-V-, F1-, or V-specific IgG titers following i.m. immunization with F1-V fusion protein in a Swiss Webster mouse plague model. Mice were given two immunizations at day 0 and day 28 (d28) with 10 μg F1-V fusion protein by i.m. injection. Unimmunized mice were used as negative controls. Each group contained 10 mice. (A) Anti-F1-V IgG titers at day 28. (B) Anti F1-V IgG titers at day 42. (C) Anti-F1 IgG titers at day 42 and protection efficacy following challenge with 1,000 LD50 Y. pestis via the s.c. route. (D) Anti-V IgG titer at day 42. The bars represent means, and the circles represent titers for individual mice. AL, Alhydrogel.
The F1- and V-specific responses were also measured at day 42 (Fig. 1C and D). Overall, anti-F1 titers were lower and more variable than those observed for anti-F1-V, although, as described above, there was not a significant difference in response between groups immunized with reconstituted SFD or unprocessed liquid formulations (P > 0.05). In contrast to the antibody response to F1, anti-V responses from day 42 (Fig. 1D) mirrored the results for anti-F1-V, with similar titers and seroconversion rates for anti-V and anti-F1-V antibodies (Fig. 1B and D).
Serum antibody response via the i.d. route.
I.d. delivery using standard needles is accomplished by the Mantoux technique (2, 11). This technique requires highly trained personnel to perform and often results in delivery variability. Microneedle-based i.d. delivery is able to overcome these drawbacks and potentially to ease the discomfort associated with Mantoux style injection (25). In this study, we also evaluated the immunogenicities and protective efficacies of F1-V vaccines delivered by microneedle.
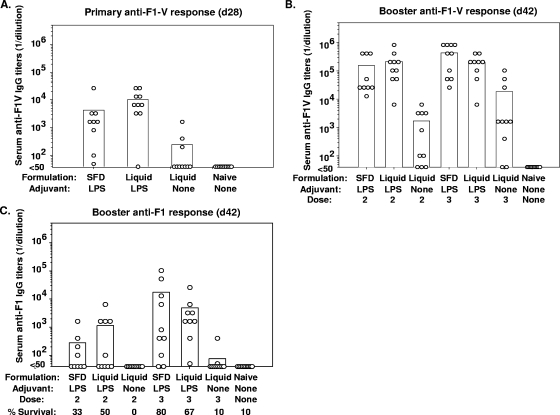
Twenty-eight days after the first immunization, the reconstituted SFD powder vaccine via the i.d. route stimulated a highly elevated serum antibody response that did not differ significantly (P > 0.05) from the response induced by the unprocessed liquid vaccine with adjuvant (Fig. 2A). In these groups, 90 to 100% positive seroconversion was achieved (Fig. 2A). The liquid vaccine formulation without adjuvant generated very little immune response. Both the reconstituted SFD and the standard liquid formulation induced a strong booster response with similar anti-F1-V titers at day 42 (Fig. 2B) (P > 0.05). Complete seroconversion was observed in these groups. The liquid formulation without adjuvant stimulated serum antibody levels that were 50-fold lower, and only 6 of 10 mice were seropositive. No elevated anti F1-V IgG titer was observed in untreated naive mice (Fig. 2B). Unprocessed liquid vaccine with adjuvant administered by the i.d. route elicited very high serum IgG titers that were equal to those elicited by i.m. vaccination (Fig. 1 and 2).
FIG. 2.
Serum F1-V- or F1-specific IgG titers following i.d. immunization with F1-V fusion protein in a Swiss Webster mouse plague model. Mice were given two immunizations at day 0 and day 28 (d28) with 10 μg F1-V fusion protein by i.d. injection. Unimmunized mice were used as negative controls. Each group contained 10 mice. (A) Anti-F1-V IgG titers at day 28. (B) Anti F1-V IgG titers at day 42. (C) Anti-F1 IgG titers at day 42 and protection efficacy following challenge with 1,000 LD50 Y. pestis via the s.c. route. The bars represent means, and the circles represent titers for individual mice. AL, Alhydrogel.
As with i.m. injection, the anti-F1 antibody response to a secondary i.d. vaccination with reconstituted SFD powder vaccine was not significantly different from the response resulting from administering the unprocessed liquid vaccine (Fig. 2C) (P > 0.05). In addition, anti-F1 antibody levels resulting from a secondary i.d. vaccination were generally lower and more variable than the corresponding anti-F1-V (Fig. 2B) or anti-V (data not shown) responses.
Serum antibody response via the i.n. route.
Our previous studies suggested that i.n. delivery of vaccine in some cases elicits lower serum antibody responses than injection, especially after a single dose (18, 28). In the current study, we evaluated immune responses following two or three doses of vaccine.
Twenty-eight days after primary vaccination, i.n. delivery elicited antibody responses that were in general more variable and lower than those elicited by the i.m. or i.d. route (Fig. 3A). Reconstituted powder vaccine delivered i.n. stimulated an antibody response comparable to the response generated by i.n. liquid vaccine (P > 0.05). The seroconversion rates for these groups were 90% or above (Fig. 3A). The liquid F1-V formulation without adjuvant elicited a fivefold-lower response than that generated by the liquid formulation with adjuvant (P < 0.05) and showed only 30% seroconversion after a single dose (Fig. 3A).
FIG. 3.
Serum F1-V- or F1-specific IgG titers following i.n. immunization with F1-V fusion protein in a Swiss Webster mouse plague model. Mice were given two immunizations at day 0 and day 28 (d28) or three immunizations at day 0, day 14, and day 28 with 10 μg F1-V fusion protein by i.n. delivery. Unimmunized mice were used as negative controls. Each group contained 10 mice. (A) Anti-F1-V IgG titers at day 28. (B) Anti F1-V IgG titers at day 42. (C) Anti-F1 IgG titers at day 42 and protection efficacy following challenge with 1,000 LD50 Y. pestis via the s.c. route. The bars represent means, and the circles represent titers for individual mice.
Forty-two days after the first vaccination, a similar pattern of serum anti-F1-V antibody responses was observed (Fig. 3B). Adding an extra dose of vaccine via the i.n. route boosted the antibody responses to levels comparable to those achieved by i.m. or i.d. injection.
We also evaluated day 42 anti-F1 antibody responses to i.n. vaccination with F1-V. As with the other routes of delivery, anti-F1 responses following i.n. administration were generally lower and more variable than the corresponding anti-F1-V (Fig. 3B) or anti-V (data not shown) antibody responses. Anti-F1 responses increased substantially in mice vaccinated three times compared to those vaccinated twice (Fig. 3C). In addition, the liquid formulation without LPS failed to induce an antibody response after two doses and induced only a small increase in antibody after three doses in 2 of 10 mice (Fig. 3C).
Protective efficacy.
Survival rates following lethal challenge with Y. pestis are shown in Fig. 1C, 2C, and 3C. In general, survival rates following lethal challenge with Y. pestis in mice vaccinated with the reformulated powder vaccines were similar to those resulting from administration of standard liquid vaccine. The reconstituted powders administered by the i.m. and i.d. routes protected animals at survival rates of 70 to 90%, while the original liquid formulation protected animals at rates ranging from 80 to 100% (Fig. 1C and 2C). Three doses of reconstituted powders delivered by the i.n. route provided 80% protection, comparable to the liquid vaccine, which protected 67% of the animals (Fig. 3C). I.d. delivery by microneedle induced survival similar to that with conventional i.m. injection for all of the formulations, while i.n. delivery required three doses of vaccine to achieve protection at levels similar to those achieved by two doses of injected vaccine (Fig. 1C, 2C, and 3C). Adjuvant enhanced immune protection regardless of the method of delivery, as groups immunized with F1-V without adjuvant were protected to a much lesser extent (10 to 30%) than corresponding groups immunized with protein plus adjuvant.
Survival as a function of seroconversion (i.e., mice with titers of at least 50) to IgG specific for F1-V fusion protein, as well as the F1 and V components, is displayed in Table 2. In all cases, seroconversion rates for V were very similar to those determined for F1-V. In contrast, lower seroconversion rates against the F1 component were apparent in many groups. This trend was especially true for groups with low survival rates. For example, group 8 displayed 50% survival and only a 50% seroconversion rate for IgG compared to 100% seroconversion for IgG recognizing F1-V or V. Similarly, group 12 had a survival rate of 10% with 20% F1 seroconversion compared to 80% F1-V and V seroconversion (Table 2). Overall, the antibody response to F1 appeared to be a better predictor of survival than levels of antibodies specific for the F1-V fusion protein or the V component.
TABLE 2.
% Survival versus seroconversion rate as determined based on anti-F1, anti-V, and anti-F1-V responses
| Group | Formulation type | No. of doses | % Survival | % Seroconversiona
|
||
|---|---|---|---|---|---|---|
| Anti-F1 | Anti-V | Anti-F1-V | ||||
| 1 | IM SFD/AL | 2 | 70 | 100 | 100 | 100 |
| 2 | IM liquid/AL | 2 | 80 | 100 | 100 | 100 |
| 3 | IM liquid | 2 | 30 | 40 | 90 | 80 |
| 4 | ID SFD/AL | 2 | 90 | 100 | 100 | 100 |
| 5 | ID liquid/AL | 2 | 100 | 100 | 100 | 100 |
| 6 | ID liquid | 2 | 10 | 30 | 60 | 60 |
| 7 | IN SFD/LPS | 2 | 33 | 44 | 100 | 100 |
| 8 | IN liquid/LPS | 2 | 50 | 50 | 100 | 100 |
| 9 | IN liquid | 2 | 0 | 0 | 70 | 70 |
| 10 | IN SFD/LPS | 3 | 80 | 80 | 100 | 100 |
| 11 | IN liquid/LPS | 3 | 67 | 100 | 100 | 100 |
| 12 | IN liquid | 3 | 10 | 20 | 80 | 80 |
| 13 | Naive | - | 10 | 0 | 0 | 0 |
Percent seroconversion was based on a serum IgG titer of ≥50. AL, Alhydrogel.
DISCUSSION
In the current study, we demonstrated that reconstituted SFD formulation of recombinant F1-V fusion protein elicited serum antibody responses and provided protection from plague at levels equivalent to those of a standard liquid formulation of F1-V. The fulminant nature of plague, the historical use of Y. pestis as a bioweapon, and the lack of a licensed human plague vaccine in the United States have created a need for safe and effective plague vaccines for human use. Powder vaccine formulations have drawn attention recently due to their potential advantages over conventional liquid vaccines, including greater stability and extended shelf life, as well as the elimination of refrigeration for storage and distribution, thereby facilitating mass vaccination (17, 21, 34). In previous studies, we demonstrated the immunogenicity and protective efficacy of powder vaccine formulations administered by the i.n. route, including whole inactivated influenza virus and anthrax rPA (17, 18, 28). Immunogenicity and protective efficacy for liquid vaccines were also demonstrated following delivery by the i.d. route using microneedles (1, 27, 28).
Consistent with the previous studies (18, 28, 35), serum antibody responses and protective efficacy following two doses of nasal vaccine were lower than those following i.m. or i.d. injection of two doses of vaccine. I.n. administration required three doses to achieve responses and protection comparable to those elicited by the i.m. or i.d. route. These observations might be explained by the more variable absorption of vaccines through nasal mucosal membranes than via direct injection. Furthermore, there is a possibility that a 15-μl dosing volume might cause reconstituted vaccine to run through the nasal cavity and be swallowed. Nasal anatomic variability and pathological changes in nasal anatomy for individual animals could also contribute to the absorption variability. Notably, in a rabbit model, anthrax rPA administered by the nasal route was shown to protect against lethal inhalational challenge to an extent similar to that with injection and without the need for additional doses compared to injection (28).
In the current study, differences in serum antibody titers were observed for anti-F1-V, anti-F1, and anti-V in relation to animal survival. Based on previous studies, both the F1 and V antigens have been identified as virulent factors that play very important roles in the pathogenesis of plague (14, 38). The discontinued killed whole-cell plague vaccine was found to protect efficiently against bubonic plague caused by an F1+ Y. pestis strain, but it did not protect against aerosol challenge in animal and clinical studies (6, 10, 33, 40). Vaccination with the whole-cell vaccine did not protect against plague caused by an F1− Y. pestis strain (3, 6, 26, 42). The reduced efficacy of whole-cell vaccines was attributed to a lack of the V antigen in the formulation (3, 22, 41). The serum anti-F1 antibody response is very important and was shown to be correlated with protection (6, 9). Passive immunization with anti-F1 antibody protected mice against F1+ Y. pestis challenge (4). Other studies also found that anti-V antibody protected mice against Y. pestis challenge by active (3, 42) or passive (16) immunization. Subunit vaccines containing the F1-V fusion protein or admixed F1 and V antigens were shown to protect against the pneumonic form of plague (14, 23, 32, 42) and to act synergistically to enhance protection against challenge (15). Our data demonstrate that, regardless of variable animal survival rates, anti-F1-V antibody titers were consistently high and showed few differences between groups vaccinated with F1-V plus adjuvants. We also tested anti-V antibody responses, which mirrored the responses measured against the F1-V fusion protein. Because the seroconversion rate of anti-F1 antibody appeared to correlate better with plague survival rates than anti-V antibody, anti-F1 antibody titers may also be more predictive of protection against challenge in animals immunized with the F1-V fusion protein.
In summary, we have demonstrated the preclinical feasibility of using reconstituted powder F1-V formulation and microneedle-based i.d. delivery to provide protective immunity against plague in a mouse model. Needle-free nasal delivery, while feasible, was less effective than injection in this study. The potential use of these alternative delivery methods and powder vaccine formulations may directly benefit biodefense vaccination programs and, ultimately, facilitate mass vaccination.
Acknowledgments
We thank Vicki Pierson of NIAID for coordinating the source of F1-V fusion protein, BEI Resources for kindly providing F1-V fusion protein (NR-2561), Bradford Powell of USAMRIID for kindly providing F1 and V antigens, and Elaine McVey and Perry Haaland of BD Technologies for statistical support.
Financial support was provided, in part, by funding from the U.S. Army Medical Research and Materiel Command, agreements number DAMD17-03-2-0037 (V.J.S.) and C.2 X001 04 RD B (R.G.U.) from the Defense Threat Reduction Agency.
Footnotes
Published ahead of print on 4 March 2009.
REFERENCES
- 1.Alarcon, J. B., A. W. Hartley, N. G. Harvey, and J. A. Mikszta. 2007. Preclinical evaluation of microneedle technology for intradermal delivery of influenza vaccines. Clin. Vaccine Immunol. 14375-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Thoracic Society and Centers for Disease Control and Prevention. 2000. Diagnostic standards and classification of tuberculosis in adults and children. Am. J. Respir. Crit. Care Med. 1611376-1395. [DOI] [PubMed] [Google Scholar]
- 3.Anderson, G. W., Jr., S. E. Leary, E. D. Williamson, R. W. Titball, S. L. Welkos, P. L. Worsham, and A. M. Friedlander. 1996. Recombinant V antigen protects mice against pneumonic and bubonic plague caused by F1-capsule-positive and -negative strains of Yersinia pestis. Infect. Immun. 644580-4585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson, G. W., Jr., P. L. Worsham, C. R. Bolt, G. P. Andrews, S. L. Welkos, A. M. Friedlander, and J. P. Burans. 1997. Protection of mice from fatal bubonic and pneumonic plague by passive immunization with monoclonal antibodies against the F1 protein of Yersinia pestis. Am. J. Trop. Med. Hyg. 56471-473. [DOI] [PubMed] [Google Scholar]
- 5.Anderson, J., E. Fishbourne, A. Corteyn, and A. I. Donaldson. 2000. Protection of cattle against rinderpest by intranasal immunisation with a dry powder tissue culture vaccine. Vaccine 19840-843. [DOI] [PubMed] [Google Scholar]
- 6.Andrews, G. P., D. G. Heath, G. W. Anderson, Jr., S. L. Welkos, and A. M. Friedlander. 1996. Fraction 1 capsular antigen (F1) purification from Yersinia pestis CO92 and from an Escherichia coli recombinant strain and efficacy against lethal plague challenge. Infect. Immun. 642180-2187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Belshe, R. B., F. K. Newman, J. Cannon, C. Duane, J. Treanor, C. Van Hoecke, B. J. Howe, and G. Dubin. 2004. Serum antibody responses after intradermal vaccination against influenza. N. Engl. J. Med. 3512286-2294. [DOI] [PubMed] [Google Scholar]
- 8.Bryan, J. P., M. H. Sjogren, P. Macarthy, E. Cox, L. J. Legters, and P. L. Perine. 1992. Persistence of antibody to hepatitis B surface antigen after low-dose, intradermal hepatitis B immunization and response to a booster dose. Vaccine 1033-38. [DOI] [PubMed] [Google Scholar]
- 9.Burrows, T. W. 1963. Virulence of Pasteurella pestis and immunity to plague. Ergeb. Mikrobiol. Immunitatsforsch. Exp. Ther. 3759-113. [DOI] [PubMed] [Google Scholar]
- 10.Cohen, R. J., and J. L. Stockard. 1967. Pneumonic plague in an untreated plague-vaccinated individual. JAMA 202365-366. [PubMed] [Google Scholar]
- 11.Cohn, D., and R. J. O'Brien. 2000. Targeted tuberculin testing and treatment of latent tuberculosis infection. MMWR Morb. Mortal. Wkly. Rep. 491-54.10993565 [Google Scholar]
- 12.de Swart, R. L., C. LiCalsi, A. V. Quirk, G. van Amerongen, V. Nodelman, R. Alcock, S. Yuksel, G. H. Ward, J. G. Hardy, H. Vos, C. L. Witham, C. I. Grainger, T. Kuiken, B. J. Greenspan, T. G. Gard, and A. D. Osterhaus. 2007. Measles vaccination of macaques by dry powder inhalation. Vaccine 251183-1190. [DOI] [PubMed] [Google Scholar]
- 13.Galimand, M., A. Guiyoule, G. Gerbaud, B. Rasoamanana, S. Chanteau, E. Carniel, and P. Courvalin. 1997. Multidrug resistance in Yersinia pestis mediated by a transferable plasmid. N. Engl. J. Med. 337677-680. [DOI] [PubMed] [Google Scholar]
- 14.Heath, D. G., G. W. Anderson, Jr., J. M. Mauro, S. L. Welkos, G. P. Andrews, J. Adamovicz, and A. M. Friedlander. 1998. Protection against experimental bubonic and pneumonic plague by a recombinant capsular F1-V antigen fusion protein vaccine. Vaccine 161131-1137. [DOI] [PubMed] [Google Scholar]
- 15.Hill, J., C. Copse, S. Leary, A. J. Stagg, E. D. Williamson, and R. W. Titball. 2003. Synergistic protection of mice against plague with monoclonal antibodies specific for the F1 and V antigens of Yersinia pestis. Infect. Immun. 712234-2238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hill, J., S. E. Leary, K. F. Griffin, E. D. Williamson, and R. W. Titball. 1997. Regions of Yersinia pestis V antigen that contribute to protection against plague identified by passive and active immunization. Infect. Immun. 654476-4482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang, J., R. J. Garmise, T. M. Crowder, K. Mar, C. R. Hwang, A. J. Hickey, J. A. Mikszta, and V. J. Sullivan. 2004. A novel dry powder influenza vaccine and intranasal delivery technology: induction of systemic and mucosal immune responses in rats. Vaccine 23794-801. [DOI] [PubMed] [Google Scholar]
- 18.Huang, J., J. A. Mikszta, M. S. Ferriter, G. Jiang, N. G. Harvey, B. Dyas, C. J. Roy, R. G. Ulrich, and V. J. Sullivan. 2007. Intranasal administration of dry powder anthrax vaccine provides protection against lethal aerosol spore challenge. Hum. Vaccin. 390-93. [DOI] [PubMed] [Google Scholar]
- 19.Illum, L., I. Jabbal-Gill, M. Hinchcliffe, A. N. Fisher, and S. S. Davis. 2001. Chitosan as a novel nasal delivery system for vaccines. Adv. Drug Deliv. Rev. 5181-96. [DOI] [PubMed] [Google Scholar]
- 20.Inglesby, T. V., D. T. Dennis, D. A. Henderson, J. G. Bartlett, M. S. Ascher, E. Eitzen, A. D. Fine, A. M. Friedlander, J. Hauer, J. F. Koerner, M. Layton, J. McDade, M. T. Osterholm, T. O'Toole, G. Parker, T. M. Perl, P. K. Russell, M. Schoch-Spana, K. Tonat, et al. 2000. Plague as a biological weapon: medical and public health management. JAMA 2832281-2290. [DOI] [PubMed] [Google Scholar]
- 21.Jiang, G., S. B. Joshi, L. J. Peek, D. T. Brandau, J. Huang, M. S. Ferriter, W. D. Woodley, B. M. Ford, K. D. Mar, J. A. Mikszta, C. R. Hwang, R. Ulrich, N. G. Harvey, C. R. Middaugh, and V. J. Sullivan. 2006. Anthrax vaccine powder formulations for nasal mucosal delivery. J. Pharm. Sci. 9580-96. [DOI] [PubMed] [Google Scholar]
- 22.Jones, S. M., K. F. Griffin, I. Hodgson, and E. D. Williamson. 2003. Protective efficacy of a fully recombinant plague vaccine in the guinea pig. Vaccine 213912-3918. [DOI] [PubMed] [Google Scholar]
- 23.Jones, T., J. J. Adamovicz, S. L. Cyr, C. R. Bolt, N. Bellerose, L. M. Pitt, G. H. Lowell, and D. S. Burt. 2006. Intranasal Protollin/F1-V vaccine elicits respiratory and serum antibody responses and protects mice against lethal aerosolized plague infection. Vaccine 241625-1632. [DOI] [PubMed] [Google Scholar]
- 24.Kenney, R. T., S. A. Frech, L. R. Muenz, C. P. Villar, and G. M. Glenn. 2004. Dose sparing with intradermal injection of influenza vaccine. N. Engl. J. Med. 3512295-2301. [DOI] [PubMed] [Google Scholar]
- 25.Laurent, P. E., S. Bonnet, P. Alchas, P. Regolini, J. A. Mikszta, R. Pettis, and N. G. Harvey. 2007. Evaluation of the clinical performance of a new intradermal vaccine administration technique and associated delivery system. Vaccine 258833-8842. [DOI] [PubMed] [Google Scholar]
- 26.Meyer, K. F. 1970. Effectiveness of live or killed plague vaccines in man. Bull. W. H. O. 42653-666. [PMC free article] [PubMed] [Google Scholar]
- 27.Mikszta, J. A., J. P. Dekker III, N. G. Harvey, C. H. Dean, J. M. Brittingham, J. Huang, V. J. Sullivan, B. Dyas, C. J. Roy, and R. G. Ulrich. 2006. Microneedle-based intradermal delivery of the anthrax recombinant protective antigen vaccine. Infect. Immun. 746806-6810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mikszta, J. A., V. J. Sullivan, C. Dean, A. M. Waterston, J. B. Alarcon, J. P. Dekker III, J. M. Brittingham, J. Huang, C. R. Hwang, M. Ferriter, G. Jiang, K. Mar, K. U. Saikh, B. G. Stiles, C. J. Roy, R. G. Ulrich, and N. G. Harvey. 2005. Protective immunization against inhalational anthrax: a comparison of minimally invasive delivery platforms. J. Infect. Dis. 191278-288. [DOI] [PubMed] [Google Scholar]
- 29.Moyle, P. M., and I. Toth. 2008. Self-adjuvanting lipopeptide vaccines. Curr. Med. Chem. 15506-516. [DOI] [PubMed] [Google Scholar]
- 30.Mueller, C. A., P. Broz, S. A. Muller, P. Ringler, F. Erne-Brand, I. Sorg, M. Kuhn, A. Engel, and G. R. Cornelis. 2005. The V-antigen of Yersinia forms a distinct structure at the tip of injectisome needles. Science 310674-676. [DOI] [PubMed] [Google Scholar]
- 31.Neutra, M. R., and P. A. Kozlowski. 2006. Mucosal vaccines: the promise and the challenge. Nat. Rev. Immunol. 6148-158. [DOI] [PubMed] [Google Scholar]
- 32.Powell, B. S., G. P. Andrews, J. T. Enama, S. Jendrek, C. Bolt, P. Worsham, J. K. Pullen, W. Ribot, H. Hines, L. Smith, D. G. Heath, and J. J. Adamovicz. 2005. Design and testing for a nontagged F1-V fusion protein as vaccine antigen against bubonic and pneumonic plague. Biotechnol. Prog. 211490-1510. [DOI] [PubMed] [Google Scholar]
- 33.Russell, P., S. M. Eley, S. E. Hibbs, R. J. Manchee, A. J. Stagg, and R. W. Titball. 1995. A comparison of plague vaccine, USP and EV76 vaccine induced protection against Yersinia pestis in a murine model. Vaccine 131551-1556. [DOI] [PubMed] [Google Scholar]
- 34.Sullivan, V. J., J. A. Mikszta, P. Laurent, J. Huang, and B. Ford. 2006. Noninvasive delivery technologies: respiratory delivery of vaccines. Exp. Opin. Drug Deliv. 387-95. [DOI] [PubMed] [Google Scholar]
- 35.Uddowla, S., L. C. Freytag, and J. D. Clements. 2007. Effect of adjuvants and route of immunizations on the immune response to recombinant plague antigens. Vaccine 257984-7993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.USAMRIID. 2005. USAMRIID's Medical Management of Biological Casualties Handbook, 6th ed. USAMRIID, Frederick, MD.
- 37.Warrell, M. J., D. A. Warrell, P. Suntharasamai, C. Viravan, A. Sinhaseni, D. Udomsakdi, R. Phanfung, C. Xueref, J. C. Vincent-Falquet, K. G. Nicholson, D. Bunnag, and T. Harinasuta. 1983. An economical regimen of human diploid cell strain anti-rabies vaccine for post-exposure prophylaxis. Lancet ii301-304. [DOI] [PubMed] [Google Scholar]
- 38.Welkos, S. L., K. M. Davis, L. M. Pitt, P. L. Worsham, and A. M. Freidlander. 1995. Studies on the contribution of the F1 capsule-associated plasmid pFra to the virulence of Yersinia pestis. Contrib. Microbiol. Immunol. 13299-305. [PubMed] [Google Scholar]
- 39.Welkos, S. L., A. M. Friedlander, and K. J. Davis. 1997. Studies on the role of plasminogen activator in systemic infection by virulent Yersinia pestis strain C092. Microb. Pathog. 23211-223. [DOI] [PubMed] [Google Scholar]
- 40.Williamson, E. D. 2001. Plague vaccine research and development. J. Appl. Microbiol. 91606-608. [DOI] [PubMed] [Google Scholar]
- 41.Williamson, E. D., S. M. Eley, K. F. Griffin, M. Green, P. Russell, S. E. Leary, P. C. Oyston, T. Easterbrook, K. M. Reddin, A. Robinson, et al. 1995. A new improved sub-unit vaccine for plague: the basis of protection. FEMS Immunol. Med. Microbiol. 12223-230. [DOI] [PubMed] [Google Scholar]
- 42.Williamson, E. D., S. M. Eley, A. J. Stagg, M. Green, P. Russell, and R. W. Titball. 1997. A sub-unit vaccine elicits IgG in serum, spleen cell cultures and bronchial washings and protects immunized animals against pneumonic plague. Vaccine 151079-1084. [DOI] [PubMed] [Google Scholar]