Abstract
There is a need to identify vaccines that can protect against Brucella, a potential bioterrorism agent. We have developed mouse models of infection with aerosolized Brucella melitensis and Brucella suis and demonstrated their utility for the evaluation of vaccines using the model live B. melitensis vaccine strain Rev.1.
Brucellosis is a zoonotic disease that is caused by Brucella species. Four species, Brucella melitensis, Brucella abortus, Brucella suis, and Brucella canis, are currently known to be pathogenic to humans (1, 5, 14). In animals, brucellosis can have a huge economic impact, since infection can lead to abortions, stillbirths, and the loss of fertility in livestock. In comparison, brucellosis in humans is a debilitating disease characterized by fever, sweats, and aches. In approximately 5% of cases it can be fatal when complications, usually endocarditis, arise (4). The illness can last a number of weeks, and even with antibiotic treatment, relapses can occur. Brucellosis is common in developing countries and areas without effective animal disease control policies. In these countries, the microorganisms are usually transmitted through ingestion, inhalation, or direct skin contact. Unpasteurized milk is a common source of infection, as is inhalation from carcasses among abattoir workers (5, 11). There are several live attenuated vaccines licensed for use in animals. Of these, the most widely used are B. melitensis Rev.1 and B. abortus S19 or RB51 (reviewed in reference 17). These vaccines are unsuitable for use in humans since they are insufficiently attenuated and still cause disease (1, 17).
Brucellosis is one of the most-common laboratory-acquired infections; it is readily aerosolized and highly infectious. Brucella species have been considered potential biological warfare agents and are classed as category B threat agents (15). B. suis was the first agent weaponized by the United States, in 1952 (6). Furthermore, there are also claims that Brucella bacteria were used by the Japanese Manchuria Unit and were developed by the former Soviet Union Biopreparat offensive biological weapon program (15). Since it is possible that a bioterrorist attack with Brucella bacteria would result in aerosolized bacteria causing inhalational infection, there is a requirement to develop and utilize appropriate animal models of aerosolized Brucella infection in order to evaluate the efficacy of vaccines or therapies for human brucellosis.
A small-rodent model of brucellosis offers advantages over the use of larger animals for preliminary studies, including the relative ease of use, ethical acceptability, and cost. Here we describe the development and characterization of mouse models of infection with aerosolized B. melitensis and B. suis bacteria and demonstrate the utility of these models in evaluating vaccines and therapeutics for inhalational brucellosis using the model live attenuated B. melitensis Rev.1 vaccine. A mouse model of intranasal (i.n.) infection with B. melitensis has previously been described (12), and since we started this work, two other laboratories have described studies of infection of mice with aerosolized Brucella bacteria. Kahl-McDonagh et al. described aerosol infection of BALB/c mice with B. abortus 2308 and B. melitensis 16 M and the use of these models for the evaluation of protective efficacy of deletion mutants (10). Olsen et al. similarly described the infection of BALB/c mice with aerosolized strain 16 M or 2308 and demonstrated that vaccination with the live attenuated animal vaccine B. abortus RB51 provided protection against intraperitoneal but not aerosolized B. abortus challenge (13). Our findings both support and extend the data generated in these studies.
Infection of mice with aerosolized B. melitensis 16 M bacteria.
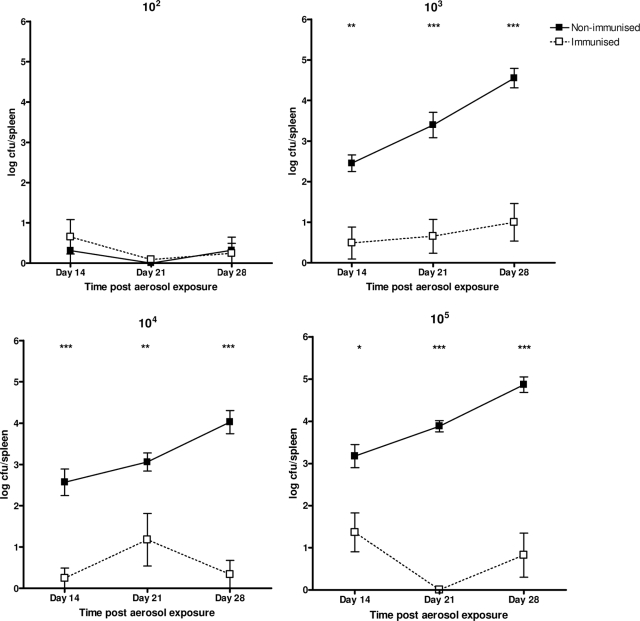
In all experiments described in this study, mice were handled in accordance with the Animal (Scientific Procedures) Act (1986). In order to establish the optimal dose of aerosolized B. melitensis 16 M bacteria required for infection in BALB/c mice, groups of 12 animals (6 to 7 weeks old; Charles River Laboratories) were exposed to retained doses of 102, 103, 104, or 105 CFU of aerosolized B. melitensis 16 M bacteria. For aerosolization, B. melitensis 16 M bacteria (obtained from the culture collection at the Veterinary Laboratories Agency, Weybridge, United Kingdom) were grown to stationary phase in Brucella broth at 37°C. Bacteria were aerosolized by using a Collison atomizer and conditioned within a Henderson apparatus (2, 9). Mice were exposed for 10 min, and impinger samples were collected for 1 min during each exposure, enabling viable counts following serial dilution and routine culture on chocolate agar plates. Calculations were used to determine the retained dose of bacteria inhaled by each mouse (7, 8). Thirty days before exposure, six animals per group were immunized via the subcutaneous (s.c.) route with the model live attenuated vaccine B. melitensis strain Rev.1. After 14, 21, and 28 days, immunized and nonimmunized mice were culled and the bacterial loads in the spleens were determined. Spleens were homogenized in phosphate-buffered saline using the barrel of a syringe and a 40-μm cell strainer (Falcon). The homogenates were serially diluted in phosphate-buffered saline and plated onto chocolate agar and tryptose soy agar containing 10 U/ml penicillin (which does not support B. melitensis Rev.1) to enumerate and differentiate the viable bacteria (Fig. 1). Protection was assessed by comparison of bacterial numbers of B. melitensis 16 M in the spleens of immunized and nonimmunized mice, and the results were analyzed by one-way analysis of variance (ANOVA) to determine differences at the 95% confidence level using Bonferroni's multiple-comparison test (GraphPad PRISM version 4.0 for Windows). At the lowest retained dose of 102 CFU, there was no difference in the splenic loads of immunized or nonimmunized mice at any time. However, following retained doses of 103, 104, or 105 CFU, there were significant differences in splenic colonization in the immunized and nonimmunized animals, indicating that protection against infection could be measured in the model (Fig. 1). B. melitensis Rev.1 was not detected in the spleen, indicating that the vaccine strain had been cleared by 2 weeks postchallenge. Overall, these results suggest that a retained dose of at least 103 CFU of aerosolized B. melitensis 16 M bacteria is suitable for the initiation of a significant infection in BALB/c mice, confirming findings described by Kahl-McDonagh et al. (10). Additionally, we have demonstrated that this model is suitable for the evaluation of protection against B. melitensis infection using, as a model vaccine candidate, the live attenuated animal vaccine B. melitensis Rev.1.
FIG. 1.
Kinetics of splenic colonization in BALB/c mice following exposure to aerosolized B. melitensis 16 M bacteria. Groups of 12 mice were exposed to retained doses of 102, 103, 104, or 105 CFU of B. melitensis 16 M as indicated. Half of each group of mice were immunized s.c. with the live vaccine B. melitensis Rev.1 30 days prior to the exposure to B. melitensis 16 M. The remaining mice were not immunized. At 14, 21, and 28 days postchallenge, all mice were culled, spleens were homogenized, and recovered B. melitensis 16 M bacteria were enumerated. One-way ANOVA was used to compare log-transformed bacterial numbers of B. melitensis 16 M in the spleens of Rev.1-immunized mice to the numbers in the spleens of nonimmunized mice. Error bars show standard deviations. Statistical significance values are as follows: *, P < 0.05; **, P < 0.01; ***, P < 0.001.
A subsequent experiment was performed to confirm and further characterize this mouse model of aerosolized B. melitensis 16 M infection. Groups of 12 Rev.1-immunized or nonimmunized mice received a retained dose of 104 CFU aerosolized B. melitensis 16 M. Animals were culled on days 7, 14, 21, and 28 postinfection, and spleens, livers, lungs, and uteruses were aseptically removed. Organs were homogenized for enumeration as described above. High levels of B. melitensis 16 M bacteria were found in the lungs of nonimmunized mice at each time point studied (data not shown). While the result was not significantly different, Rev.1-immunized mice harbored lower numbers of B. melitensis 16 M bacteria in their lungs (data not shown). Nonimmunized and immunized mice harbored B. melitensis 16 M in their livers from days 7 and 21, respectively. B. melitensis 16 M bacteria were recovered from the uteruses of a high proportion of nonimmunized mice at all times but were found in the uteruses of immunized mice only on day 28 postexposure. Importantly, there were significant differences in the numbers of viable B. melitensis 16 M bacteria recovered from the spleens of immunized and nonimmunized mice at 14, 21, and 28 days postexposure, confirming the data from our initial experiment. In immunized mice, B. melitensis Rev.1 was detected in the liver up to 14 days postinfection and in the spleen on day 7 postexposure only. No B. melitensis 16 M bacteria were recovered from blood samples cultured in Brucella broth at any time.
Using a retained dose of 104 CFU of B. melitensis 16 M, a further experiment was performed to determine the bacterial loads in livers, lungs, and spleens at 2, 5, and 8 weeks postchallenge. The results of this experiment showed that bacterial loads in the spleen were at their highest at 5 weeks postchallenge (data not shown). In the lungs there was a decrease in bacterial load over time, and in the livers there was a slight increase over time (data not shown). Again, these findings are consistent with those of Kahl-McDonagh et al. (10) and with those of Mense et al. (12), who followed the course of infection in BALB/c mice administered B. melitensis 16 M via the i.n. route. In addition, our data showed consistent protection afforded by Rev.1 at 2 to 4 weeks after exposure to B. melitensis 16 M, demonstrating a time frame during which the protective efficacy of a treatment can be evaluated in this model.
Infection of mice with aerosolized B. suis 1330.
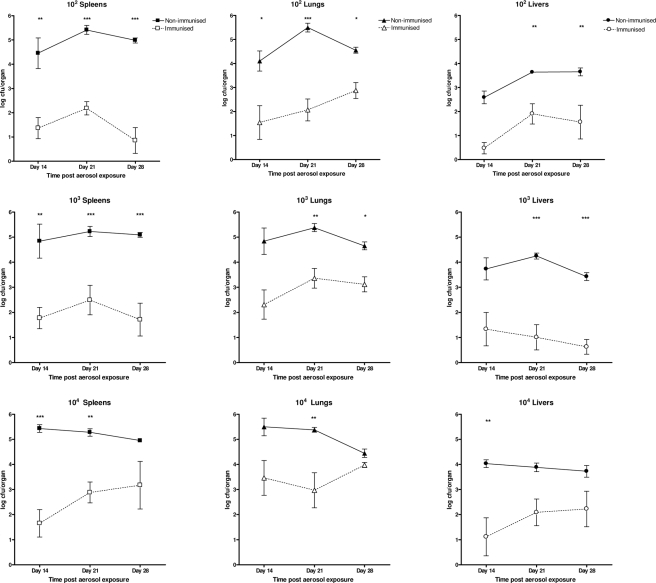
In order to extend our study to inhalational brucellosis caused by B. suis, groups of 12 mice were immunized with the model vaccine Rev.1 via the s.c. route (6 animals) or left nonimmunized (6 animals) and then received retained doses of 102, 103, or 104 CFU of aerosolized B. suis 1330 (obtained and cultured as described for B. melitensis 16 M). After 2, 3, and 4 weeks, animals were culled and viable counts were performed on spleen, lung, and liver homogenates to determine bacterial loads (Fig. 2). The homogenates were plated onto chocolate agar and blood agar base media containing 2.5 mg/liter erythromycin (does not support B. suis 1330) to enumerate and differentiate the viable bacteria. Following B. suis challenge, the B. melitensis Rev.1 live vaccine strain could still be recovered from spleens and lungs at 4 weeks postexposure (8 weeks after immunization). Specifically, 255 CFU of B. melitensis Rev.1 was recovered from the spleen of one mouse after exposure to 102 CFU of B. suis; 43 to 500 CFU of B. melitensis Rev.1 was present in the spleens of three mice, and 3,000 CFU of Rev.1 was found in the lung of a single mouse after exposure to 103 CFU of B. suis; 187 and 268 CFU of B. melitensis Rev.1 were recovered from the spleens of two mice after exposure to 104 CFU of B. suis. Protection was afforded by the vaccine in this infection model (Fig. 2). There were significantly lower bacterial loads in the spleens at all time points when mice received a retained dose of 102 or 103 CFU of B. suis. Bacterial loads were significantly lower in the lungs of immunized mice than in those of nonimmunized mice at all time points after a retained dose of 102 CFU and at 3 and 4 weeks after a retained dose of 103 CFU of B. suis. Protection in the liver varied (Fig. 2). However, at the highest retained dose of 104 CFU of B. suis 1330, protection afforded by the vaccine was observed in the spleen only at 2 and 3 weeks postchallenge, in the liver only at 2 weeks postchallenge, and in the lungs only at 3 weeks postchallenge. At 4 weeks postchallenge, no protection was observed against a retained dose of 104 CFU B. suis. B. suis bacteria were also isolated from the uteruses of nonimmunized mice at each time point.
FIG. 2.
Kinetics of infection in BALB/c mice following exposure to aerosolized B. suis 1330. Groups of mice were exposed to retained doses of 102 (top row), 103 (middle row), or 104 CFU (bottom row) of B. suis 1330. Half of the mice in each group were immunized s.c. with the B. melitensis Rev.1 live vaccine 30 days prior to challenge with B. suis. The remaining mice remained nonimmunized. At 14, 21, and 28 days postchallenge, all mice were culled, organs were homogenized, and recovered B. suis 1330 bacteria in spleens (first column), lungs (second column), and livers (third column) were enumerated. One-way ANOVA was used to compare bacterial numbers of B. suis 1330 in the organs of immunized mice to the numbers in the organs of nonimmunized mice. Error bars show standard deviations. Statistical significance values are as follows: *, P < 0.05; **, P < 0.01; ***, P < 0.001.
The isolation of B. suis and B. melitensis bacteria from the uteruses of infected animals demonstrates the tropism that the species has for this tissue and supports the suitability of the mouse model, reflecting the findings that Brucella bacteria are often identified in the reproductive systems of ruminant animals and have also been isolated from the uteruses of seals and otters (3). In comparison, Brucella bacteria were isolated from the blood of infected mice only on one occasion during this study (B. suis at 2 weeks postexposure to the highest retained dose), reflecting the finding that bacteremia in brucellosis is transient and can often go undetected (16). Positive blood cultures in human cases can vary from 10% to 90%, indicating that blood culturing is not a reliable method to indicate infection.
This study has shown, to our knowledge for the first time, that aerosolized B. suis 1330 bacteria are able to cause a systemic infection in the BALB/c mouse, providing an additional mouse model of aerosolized Brucella infection. Since B. suis was the first agent weaponized in the United States (6, 15) and is considered a potential bioterrorism agent today, the development of this model is an important addition to the arsenal of models that could be used for testing vaccines or therapies for human brucellosis. In comparison to infection with B. melitensis, infection of mice with aerosolized B. suis bacteria appears to cause a more acute infection, with higher numbers of bacteria colonizing the spleens and lungs and bacterial loads peaking earlier. Unlike infection with B. melitensis, a low retained dose of 102 CFU of B. suis bacteria is sufficient to cause a significant infection, and protection afforded by the model Rev.1 vaccine can be measured against this low dose.
Effect of the route of administration of B. melitensis Rev.1 live vaccine.
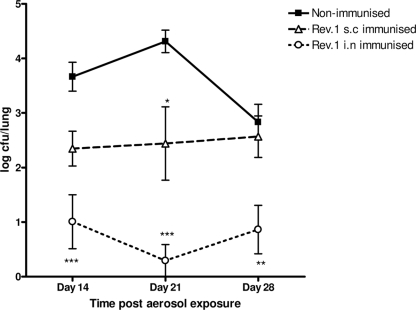
Our initial experiments demonstrated protection against brucellosis afforded by s.c. administration of the model vaccine Rev.1, evidenced by a decreased bacterial load in the spleen compared with that in nonimmunized mice. We hypothesized that immunization by the i.n. route may be more effective in providing protection against inhalational brucellosis. Groups of eight mice were immunized with 2 × 105 CFU of B. melitensis Rev.1 administered by either the s.c. or i.n. route, and groups of eight mice remained nonimmunized. To immunize via the i.n. route, mice were lightly anesthetized before administration to the nostrils. After 30 days, immunized and nonimmunized mice received a retained aerosol dose of 4 × 103 CFU of B. melitensis 16 M. Spleen, liver, and lung bacterial counts were taken at 2, 3, and 4 weeks postchallenge. Significantly lower bacterial loads were observed in the lungs of mice immunized via the i.n. route than in the lungs of nonimmunized mice at all times (Fig. 3). Reduced bacterial burdens were observed in the spleens and livers at 3 and 4 weeks postchallenge (P < 0.05; results not shown). Conversely, s.c. administration of Rev.1 led to protection in the spleen at all times (P < 0.001; not shown) but protection in the lungs (Fig. 3) and livers (not shown) at only one time point. The results of this experiment indicate that consideration of the route of administration may be important in developing therapeutics for inhalational brucellosis.
FIG. 3.
Rev.1 vaccination by the i.n. route provides protection in the lungs of mice infected with B. melitensis 16 M. Groups of mice were challenged with a retained dose of 4 × 103 CFU of B. melitensis 16 M. Two groups had previously been immunized with the Rev.1 vaccine by either the s.c. or i.n. route. At 2, 3, or 4 weeks postchallenge, B. melitensis 16 M was recovered from the lungs of nonimmunized, s.c. Rev.1-immunized, and i.n. Rev.1-immunized mice. One-way ANOVA was used to compare bacterial numbers of B. melitensis 16 M in the lungs of nonimmunized mice to the numbers in the lungs of those immunized by the s.c. or i.n. route. Error bars show standard deviations. Statistical significance values for individual immunization routes are as follows: *, P < 0.05; **, P < 0.01; ***, P < 0.001.
Overall, we have developed mouse models of infection with aerosolized B. melitensis 16 M or B. suis 1330 that may be applied to the evaluation of vaccines or therapeutics for brucellosis, and we now aim to undertake such studies in our laboratory.
Footnotes
Published ahead of print on 25 March 2009.
REFERENCES
- 1.Cutler, S. J., A. M. Whatmore, and N. J. Commander. 2005. Brucellosis—new aspects of an old disease. J. Appl. Microbiol. 981270-1281. [DOI] [PubMed] [Google Scholar]
- 2.Druett, H. A. 1969. A mobile form of the Henderson apparatus. J. Hyg. (London) 67437-448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Foster, G., K. L. Jahans, R. J. Reid, and H. M. Ross. 1996. Isolation of Brucella species from cetaceans, seals and an otter. Vet. Rec. 138583-586. [DOI] [PubMed] [Google Scholar]
- 4.Franco, M. P., M. Mulder, R. H. Gilman, and H. L. Smits. 2007. Human brucellosis. Lancet Infect. Dis. 7775-786. [DOI] [PubMed] [Google Scholar]
- 5.Godfroid, J., A. Cloeckaert, J. P. Liautard, S. Kohler, D. Fretin, K. Walravens, B. Garin-Bastuji, and J. J. Letesson. 2005. From the discovery of the Malta fever's agent to the discovery of a marine mammal reservoir, brucellosis has continuously been a re-emerging zoonosis. Vet. Res. 36313-326. [DOI] [PubMed] [Google Scholar]
- 6.Greenfield, R. A., D. A. Drevets, L. J. Machado, G. W. Voskuhl, P. Cornea, and M. S. Bronze. 2002. Bacterial pathogens as biological weapons and agents of bioterrorism. Am. J. Med. Sci. 323299-315. [DOI] [PubMed] [Google Scholar]
- 7.Guyton, A. C. 1947. Measurement of the respiratory volumes of laboratory animals. Am. J. Physiol. 15070-77. [DOI] [PubMed] [Google Scholar]
- 8.Harper, G. J., and J. D. Morton. 1962. A method for measuring the retained dose in experiments on airborne infection. J. Hyg. (London) 60249-257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Henderson, D. W. 1952. An apparatus for the study of airbourne infection. J. Hyg. (London) 5053-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kahl-McDonagh, M. M., A. M. Arenas-Gamboa, and T. A. Ficht. 2007. Aerosol infection of BALB/c mice with Brucella melitensis and Brucella abortus and protective efficacy against aerosol challenge. Infect. Immun. 754923-4932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Memish, Z. A., and H. H. Balkhy. 2004. Brucellosis and international travel. J. Travel Med. 1149-55. [DOI] [PubMed] [Google Scholar]
- 12.Mense, M. G., L. L. Van De Verg, A. K. Bhattacharjee, J. L. Garrett, J. A. Hart, L. E. Lindler, T. L. Hadfield, and D. L. Hoover. 2001. Bacteriologic and histologic features in mice after intranasal inoculation with Brucella melitensis. Am. J. Vet. Res. 62398-405. [DOI] [PubMed] [Google Scholar]
- 13.Olsen, S. C., W. R. Waters, and W. S. Stoffregen. 2007. An aerosolized Brucella spp. challenge model for laboratory animals. Zoonoses Public Health 54281-285. [DOI] [PubMed] [Google Scholar]
- 14.Pappas, G., N. Akritidis, M. Bosilkovski, and E. Tsianos. 2005. Brucellosis. N. Engl. J. Med. 3522325-2336. [DOI] [PubMed] [Google Scholar]
- 15.Pappas, G., P. Panagopoulou, L. Christou, and N. Akritidis. 2006. Brucella as a biological weapon. Cell. Mol. Life Sci. 632229-2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pappas, G., and P. Papadimitriou. 2007. Challenges in Brucella bacteraemia. Int. J. Antimicrob. Agents 30(Suppl. 1)S29-S31. [DOI] [PubMed] [Google Scholar]
- 17.Schurig, G. G., N. Sriranganathan, and M. J. Corbel. 2002. Brucellosis vaccines: past, present and future. Vet. Microbiol. 90479-496. [DOI] [PubMed] [Google Scholar]