Abstract
Hantavirus cardiopulmonary syndrome (HCPS) is a highly pathogenic emerging disease (40% case fatality rate) caused by New World hantaviruses. Hantavirus infections are transmitted to humans mainly by inhalation of virus-contaminated aerosol particles of rodent excreta and secretions. At present, there are no antiviral drugs or immunotherapeutic agents available for the treatment of hantaviral infection, and the survival rates for infected patients hinge largely on early virus recognition and hospital admission and aggressive pulmonary and hemodynamic support. In this study, we show that Andes virus (ANDV) interacts with human apolipoprotein H (ApoH) and that ApoH-coated magnetic beads or ApoH-coated enzyme-linked immunosorbent assay plates can be used to capture and concentrate the virus from complex biological mixtures, such as serum and urine, allowing it to be detected by both immunological and molecular approaches. In addition, we report that ANDV-antigens and infectious virus are shed in urine of HCPS patients.
Hantaviruses are segmented RNA viruses belonging to the genus Hantavirus in the family Bunyaviridae (43). Hantaviral genomes are tripartite, consisting of three different single-stranded RNA segments, designated large (L), medium (M), and small (S), that are packed into helical nucleocapsids (39, 42). These segments encode the RNA polymerase, a glycoprotein precursor that is cotranslationally processed to yield two envelope glycoproteins (Gc and Gn) and a nucleocapsid (N) protein. Hantaviruses are maintained in various rodent reservoirs, in which the hosts are persistently infected but lack disease symptoms (28, 32). Virus transmission to humans does not require direct human-to-rodent contact. Instead, human hantaviral infections are acquired by the respiratory route, most commonly through inhalation of virus-contaminated aerosol particles of rodent excreta (feces, saliva, or urine). Hantaviruses are known to cause two serious and often fatal human diseases, hemorrhagic fever with renal syndrome and hantavirus cardiopulmonary syndrome (HCPS) (19, 31). Of the two diseases, HCPS is more severe, with a mortality rate of approximately 40% (19). Hemorrhagic fever with renal syndrome is a mild-to-severe disease characterized by the development of an acute influenza-like febrile illness that may lead to hemorrhagic manifestations, and renal failure is caused by pathogenic Old World hantaviruses, which include Seoul, Hantaan, Dobrava, Tula, and Puumala viruses (28, 32, 42). The New World hantaviruses are responsible for HCPS, which is characterized by a febrile phase (prodrome) and pulmonary infection, cardiac depression, and hematologic manifestations (18, 31). HCPS pathogenesis generally includes capillary leak syndrome, which selectively involves the pulmonary bed, noncardiogenic pulmonary edema, thrombocytopenia, hypotension, and/or cardiogenic shock (19, 31). The pathogenesis of HCPS, like that of many other viral hemorrhagic fevers, is poorly understood. However, the long incubation period for illness, the generally well-advanced adaptive immune response at the time of onset of the disease, and the apparent absence of direct lytic damage to vascular endothelium, all characteristics shared with other hemorrhagic fevers, are among the findings that strongly suggest that HCPS pathogenesis is largely immune mediated (22, 27). The lack of an FDA-approved vaccine for HCPS, the absence of specific antiviral drugs or immunotherapeutic agents, and the high overall mortality rate for hantavirus infection highlight the medical significance of New World hantavirus (5, 8, 19, 28, 32).
Survival rates for patients with hantaviral infection hinge largely on early virus recognition and hospital admission and aggressive pulmonary and hemodynamic support (19, 31). The diagnosis, clinical course, and supportive care of patients with New World hantaviral infections have recently been reviewed (19, 31). Unfortunately, early diagnosis of New World hantaviral infections is complex, as the prodrome leading to acute cardiopulmonary deterioration in HCPS can be confused with febrile phases produced by, for example, mycoplasmas and chlamydophilial infections (52).
Human apolipoprotein H (ApoH), also known as beta 2-glycoprotein I, is a constituent of human plasma (0.2 mg/ml) notorious for binding to negatively charged surfaces (3, 7, 14, 17, 44, 45). Several reports show that ApoH also interacts with viral proteins, such as the hepatitis B virus (HBV) antigen and proteins p18, p26, and gp160 of the human immunodeficiency virus (12, 30, 46, 47). Interestingly, studies involving binding to the HBV antigen suggest that ApoH specifically binds DNA-containing HBV particles, thus discriminating, through an undefined mechanism, between active replicating virus and empty noninfectious particles (47). These findings prompted us to assess a possible interaction between ApoH and Andes virus (ANDV), which is the major etiological agent of HCPS in South America and is unique among hantaviruses in its reported ability to be transmitted from person to person (19, 29, 34). The mechanism of person-to-person dissemination of ANDV remains to be elucidated, yet it is likely that person-to-person transmission of ANDV could be explained by mechanisms similar to those described for rodent-to-rodent and rodent-to-human transmission. If so, a compulsory condition for ANDV dissemination among humans is that the infected host must shed the pathogen in, for example, urine.
In this study, we show that when fixed to a solid matrix, ApoH can be used to capture and concentrate ANDV from complex biological samples, including serum and urine, allowing virus detection by both immunological and molecular approaches. Furthermore, we took advantage of the ApoH-ANDV interaction to develop a high-throughput screening assay and show for the first time ANDV-antigen shedding in the urine of patients with acute HCPS. We also report the presence of infectious viral particles in the urine of two patients with HCPS.
MATERIALS AND METHODS
Virus and cells.
ANDV strain CHI-7913 was propagated in Vero E6 cells (Vero C1008; ATCC CRL 156) as previously described (11). Cells were maintained in Eagle's minimal essential medium with Earle's salts containing 10% fetal bovine serum, 10 mM HEPES (pH 7.4), and antibiotics (penicillin [100 U/ml], streptomycin [100 μg/ml], and gentamicin sulfate [50 μg/ml]) at 37°C in a 5% CO2 incubator.
Patients and controls.
Serum and urine samples from patients with acute HCPS were selected on the basis of their availability in the laboratory. Samples had been collected as part of the research initiative “Hantavirus ecology and disease in Chile,” directed by G. Mertz, and were kindly supplied for this study. Donor patients met the clinical criteria for acute HCPS (Ministry of Health of Chile; http://www.minsal.cl) and harbored immunoglobulin M (IgM) antibodies reactive with hantavirus antigens, as described by Ferres et al. (10). Peripheral blood was collected in Vacutainer serum tubes (Becton Dickinson) or EDTA-containing Vacutainer tubes (Becton Dickinson) for the recovery of serum or plasma, respectively. Serum and plasma samples were stored at −80°C until use. All samples used in this study were collected between 2000 and 2002. Some patients were characterized as having infections from household contact; thus, their initial samples were negative in both molecular and serological ANDV analyses. However, all patients in the study had confirmed cases of HCPS. ANDV-reactive antibodies were identified through an IgM capture enzyme-linked immunosorbent assay (ELISA) performed with human sera by using inactivated Laguna Negra virus, which was kindly provided by T. Ksiazek from the CDC (Atlanta, GA), by following well-established protocols (25). The presence of ANDV genomic RNA in plasma was confirmed by reverse transcription-PCR (RT-PCR) following a protocol established in-house (see below). Urine was collected in urine collection cups (Deltalab, Barcelona, Spain) and stored at −80°C until use. Participants in this study completed a written consent form approved by two independent Chilean ethical committees from both medical institutions responsible for sample collection, namely, the Clínica Alemana de Chile and the Pontificia Universidad Católica de Chile University Hospital ethical review boards, before donating biological samples.
Extraction and analysis of RNA.
Total RNA was extracted using a High Pure viral nucleic acid kit (Roche Molecular Biochemicals) following the manufacture's protocol and amplified by RT-PCR/heminested PCR as previously described (10). In brief, the method uses primers designed to partially encompass the S segment open reading frame (forward primer S, nucleotides [nt] 49 to 69; reverse primer R, nt 1107 to 1129; and reverse primer A, nt 262 to 283) of the ANDV strain CHI-7913 (GenBank accession no. AY228237) (10). Amplicons were analyzed by gel electrophoresis. Fragments of the expected sizes were recovered from the gels and sequenced, confirming the amplification of the ANDV genome. A real-time-based method was used for the quantification of ex vivo-cultured ANDV genomes, by following previously established protocols (10). Variations were introduced into the described protocols to fit the equipment present in the laboratory. Real-time PCR was performed using a MX3000 instrument (Stratagene) using Brilliant II quantitative RT-PCR (QRT-PCR) reagents (Stratagene) by following the manufacturer's guidelines. The specificity of the amplicons was confirmed by melting point analysis and by sequencing. When indicated in the text and legend to Fig. 4, a direct RT-PCR (SuperScript III One-Step RT-PCR system with Platinum Taq High Fidelity; Invitrogen) using the forward primer F-HantaS (5′-ACACGAACAACAGCTCGTGAC-3′) and the reverse primer R-HantaR (5′-AGGCTCAAGCCCTGTTGGATC-3′), targeting the nucleocapsid coding region (S genomic RNA), was used by following the manufacturer's protocol.
FIG. 4.
ApoH-coated magnetic beads can capture infectious ANDV. (A) ApoH-captured virus from urine samples (US) was used to infect Vero E6 cells, and at 16 days postinfection, ANDV-nucleocapsid protein was detected by an indirect IF assay in 2 of the 65 cultures tested (samples 53 and 54; US53 and US54, respectively). Cells were costained with DAPI. White arrows indicate ANDV-positive cells. Noninfected Vero E6 cells were used as a negative control, while cells infected with the ANDV CHI-7913 strain were used as positive controls. FITC, fluorescein isothiocyanate. (B) Direct one-step RT-PCR assay using total RNA extracted from ANDV CHI-7913-infected Vero E6 cells (positive control) [(C+), lane 1], noninfected VeroE6 cells (negative control) [(C−), lane 2], Vero E6 cells (C) infected with urine sample 53 (US53, lane 3), or supernatants (S) of these cells (lane 4) or Vero E6 cells infected with urine sample 54 (US54, lane 5) or supernatants of these cells (lane 6). An additional water control for the RT-PCR (−) (lane 7) was included. M lanes correspond to the 1-kb marker (Fermentas). The arrow indicates the expected amplicon.
ApoH-coated magnetic beads and ApoH-coated ELISA plates.
ApoH was purified from human plasma albumin solutions as previously described (46) and used to coat magnetic beads (Merck Chimie S.A.S., Paris, France) and ELISA plates (96-well flat-bottom microplates). ApoH-coated magnetic beads and plates used in this study were supplied by ApoH Technologies S.A. (Villeneuve Saint Georges, France). Beads were equilibrated in phosphate-buffered saline (PBS) (137 mM NaCl, 2.7 mM KCl, 4.3 mM Na2HPO4·7H2O, 1.4 mM KH2PO4 [pH 7.4]) before use, and 10 μl of a 50% bead slurry in PBS was used for each 1.5 ml of serum or urine. After a 2-h incubation period at 37°C with constant gentle rolling for the single-sample assays, beads were recovered using a MagneShere Technology magnetic separation stand (Promega), and multiple samples were simultaneously isolated by using a Dynal MPC-S (Dynal Biotech; Invitrogen). After being washed three times with PBS, the beads were directly resuspended in RNA extraction buffer (High Pure viral nucleic acid kit; Roche), and RNA was extracted according to the manufacturer's protocols. Urine samples (100 μl) were directly added to each well of the ApoH-coated ELISA plates, which were incubated at 37°C for 1 h. The supernatant was discarded, and the wells were washed with PBS-0.1% Tween 20 (PBST), blocked with PBST containing 5% nonfat dry milk, and incubated with serum from a Chilean HCPS patient (1:200; patient number 08S), or anti-ANDV glycoprotein monoclonal antibodies (1:1,000) against GcA and GcB (see below) for 1 h at 37°C in a humidified chamber. Subsequently, the plate was washed and incubated with goat anti-human IgG horseradish peroxidase (HRP)-conjugated antibody (1:4,000; Chemicon) or a mixture of goat anti-rat HRP- and goat anti-Peromyscus leucopus IgG HRP-conjugated antibodies (1:2,500; KPL Laboratories, MD) for 1 h, washed with PBST, and developed using a 2,2′-azino-bis(3-ethylbenzthiazoline-6-sulfonic acid) (ABTS) peroxidase substrate system (KPL laboratories, MD). Data are expressed as optical densities (OD) (A405 − A630).
SIA.
IgM and IgG antibodies against ANDV were detected in serum samples using a strip immunoblot assay (SIA) vacuum blot test as previously described (18). Affinity-purified recombinant ANDV and Seoul N antigen, kindly provided by B. Hjelle (University of New Mexico, Albuquerque, NM), were suctioned onto a wetted nitrocellulose membrane under a vacuum. As internal controls, two levels (level I, the low control; level II, the high control) of human IgG were applied to the blot. The membrane was cut lengthwise with a paper shredder into 3-mm strips, and each strip was placed into a well in a Western blot tray containing 1 ml of milk-PBST buffer and 5 μl of patient serum. The membranes were rocked gently overnight at 4°C. The strips were washed three times with PBST, and 1:1,000 dilutions of goat anti-human IgM or IgG alkaline phosphatase-conjugated antibodies (KPL Laboratories, MD) were applied; the strips were then subjected to gentle rocking for 1 h at room temperature. The blot was developed according to the 5-bromo-4-chloro-3-indolyl phosphate-nitroblue tetrazolium protocol (5-bromo-4-chloro-3-indolylphosphate [BCIP]/Nitro Blue tetrazolium chloride; KPL Laboratories, MD).
Development of monoclonal antibodies against ANDV Gc glycoprotein.
The coding regions for the ANDV Gc glycoprotein amino (N)- and carboxyl (C)-terminal fragment were recovered from the cDNA clone of ANDV strain CHI-7913 (GenBank accession no. AY228238) by PCR amplification using primers 5′-GAAGGTCGACAAATGGCCGCAAGTGCAGAGACTCCA-3′ and 5′-CAGTCTCGACCTAGCACCATTGTTTAAGGATGAC-3′ to recover the N-terminal coding region (amino acids 647 to 866; GcA) and primers 5′-ATCCGTCGACTAATGCCATCTGTGAAGGTTTGTATA-3′ and 5′-AGGACTCGAGGCGGCCGCTTAGACAGTTTTCTTGTGCCC-3′ for the C-terminal region (amino acids 829 to 1138; GcB) (49). Escherichia coli BL21 cells were then transformed with plasmids pET32(a)/GcA and pET32(a)/GcB, which were generated by cloning of the PCR amplification products GcA and GcB into vector pET32(a) (Novagen; Merck Biosciences). After a 3-h induction period, using 1 mM isopropyl β-d-thiogalagtopyranoside, the thioredoxin 1 (Trx1)-GcA and -GcB fused proteins were purified from the cell lysates with nickel-nitriloacetate agarose beads as specified by the manufacturer (Qiagen, Germany) and used to generate monoclonal antibodies as previously described (23). With this procedure, two monoclonal antibodies, 2H4/F6 anti-GcA and 6C5/D12 anti-GcB, were generated. The specificities of 2H4/F6 anti-GcA and 6C5/D12 anti-GcB were assessed by ELISAs evaluating their reactivity toward recombinant GcA and GcB proteins, respectively. Both antibodies showed no reactivity to the Trx1 protein.
Vero E6 cell infection with ANDV.
ApoH-coated ELISA plates (96 wells) were incubated with 50 μl per well of either supernatants of Vero E6 (negative control), supernatants of Vero E6 infected with ANDV-CHI-7913 (positive control), or urine samples (frozen between 2000 and 2002) from patients with ANDV-associated HCPS for 1 h at 37°C. Two wells were used for each sample. Cell supernatants or urine were then aspirated, and the wells were washed three times with 1× PBS. Fresh Vero E6 cells were seeded at 1 × 105 cells/well directly over each ApoH-coated well, and the wells were incubated overnight. Vero E6 cells were removed and seeded onto 24-well plates. After 1 week, the cells were trypsinized, recovered, and seeded into a T25 culture flask for virus propagation. All ANDV isolation and propagation studies were conducted in a biosafety level 3 facility.
ANDV nucleocapsid protein detection by indirect IF assay.
The immunofluorescence (IF) assay was performed with 1 × 105 cells. Following a cytospin (Mikro 22; Hettich) for 7 min at 1,100 rpm, the cells were fixed for 30 min at −20°C in a mixture of acetone and methanol (1:1 [vol/vol]). The cells were blocked for 30 min at room temperature in PBS containing 1% bovine serum albumin. After being washed three times, the slides were incubated at 37°C for 30 min in a humidified box with the anti-ANDV nucleocapsid antibody (1:500) (50). Slides were incubated at 37°C for 30 min in a humidified box with anti-mouse antibody conjugated with fluorescein isothiocyanate (1:200). Staining with 4′,6′-diamidino-2-phenylindole (DAPI) was performed for 7 min at room temperature (1 μg/ml final concentration). Slides were mounted (mounting fluid; Diagnostic Hybrids, Athens, OH) prior to analysis. Photographs were taken using a high-resolution IEEE 1394 FireWireTM digital charge-coupled-device color camera with high-speed real-time viewing and a MicroPublisher 3.3 RTV camera in conjunction with an Olympus microscope at 40× and digitally analyzed using QCapture PRO 6 software (QImaging, Surrey, British Columbia, Canada).
RESULTS
Hantavirus interacts with human ApoH, allowing for virus concentration.
The discovery that ApoH interacts with viral proteins and that this binding property could be useful in the capture of infectious viruses (47) prompted us to undertake studies to determine if human ApoH binds ANDV. We reasoned that a valid approach to assess a putative interaction between ApoH and ANDV would be through an in vitro capture assay using the ApoH protein fixed to a solid matrix as bait. Latex beads coated with a magnetic pigment were chosen as the solid matrix, while supernatants from ANDV strain CHI-7913-infected Vero E6 cells were used as the source of virus in spiking assays (11). Infected-cell supernatants containing known amounts of ANDV genomic equivalents (ranging from 2 × 104 to 1 × 105, as estimated by QRT-PCR) (10) were diluted in different volumes of PBS. A fixed volume of 10 μl of a 50% slurry of ApoH-coated magnetic beads was added to each mixture. The beads were recovered and washed, and the RNA from viruses associated with the beads was isolated. The ANDV-RNA associated with the beads was quantified by real-time RT-PCR (10), and the percentages of recovery from three independent experiments conducted using independent sources of virus (different cultures) are summarized in Table 1. Under the experimental conditions used, ApoH-coated magnetic beads allowed for the concentration of ANDV from a mixture of PBS and virus-containing Vero E6 culture medium.
TABLE 1.
Virus spiking experiments
| Sample no. | Vol (μl)
|
% Recovery ± SDa
|
|||
|---|---|---|---|---|---|
| ANDV-positive supernatant | PBS or urine | Final sample | PBS | Urine | |
| 1 | 100 | 400 | 500 | 75.5 ± 33.4 | 41.9 ± 7.4 |
| 2 | 100 | 900 | 1,000 | 62.9 ± 27.6 | 45.2 ± 10.7 |
| 3 | 100 | 1,400 | 1,500 | 69.1 ± 11.7 | 66.6 ± 12.9 |
| 4 | 100 | 1,900 | 2,000 | 50.4 ± 10.2 | 42.0 ± 14.7 |
Values are the percentages of recovery ± standard deviations from four independent experiments.
We next sought to determine if ApoH-coated beads could be used to isolate ANDV when serum samples from patients with acute HCPS were used as the source of virus. Preliminary studies of ANDV infections suggest that plasma and serum viral loads are too often below the limit of detection of the assay to be useful in the prediction of disease severity (53). However, we speculated that if ApoH interacts with ANDV as efficiently as has been reported for HBV (47), and if serum components did not interfere with ApoH-virus binding, ApoH-coated magnetic beads would be capable of capturing ANDV even when present in a complex biological mixture. To test this possibility, we compared results of the standard RT-PCR/heminested PCR assay used for ANDV detection (10) with and without the incorporation of a virus concentration step by ApoH. Results (Fig. 1) show that ApoH-coated magnetic beads capture ANDV, permitting virus concentration. Out of 10 serum samples tested, results from 2 samples, those from patient 1 (S1) and from patient 2 (S2), are shown in Fig. 1. These samples were selected as they highlight the advantages of the ApoH virus capture assay for ANDV detection. In parallel assays, we determined the presence of circulating anti-ANDV antibodies for each patient through a SIA vacuum blot test using affinity-purified recombinant ANDV and Seoul virus N antigen as bait (18). Patient S1 showed IgM antibodies reactive to hantaviral antigens (Fig. 1A, lane 2) but lacked detectable amounts of anti-hantavirus IgGs (Fig. 1B, lane 2), while patient S2 displayed both IgM (Fig. 1A, lane 3) and IgG (Fig. 1B, lane 3) anti-hantavirus antibodies. Unexpectedly, when RNA was extracted from 300 μl of serum by means of a High Pure viral nucleic acid kit (Roche) by following the manufacturer's protocol (Fig. 1C, lanes 5 and 8), both patients came up negative for viral genomic RNA. However, when a step of ANDV capture and concentration from 1.5 ml of serum by ApoH-coated magnetic beads was incorporated into the overall RNA isolation-detection procedure, ANDV genomic RNA was readily detected for both HCPS patients (Fig. 1C, lanes 6 and 9). No viral RNA could be detected when uncoated or bovine serum albumin-coated magnetic beads were used as bait with serum samples from HCPS patients (data not shown) or when RNA was extracted from the sera of healthy, noninfected donors (Fig. 1C, lanes 1 and 2). Thus, we conclude that ANDV binds ApoH and that the incorporation of a capture-concentration step using ApoH-coated magnetic beads to currently used detection protocols improves the sensitivity of virus diagnosis.
FIG. 1.
ANDV binds serum-purified human ApoH. Serum from patients S1 and S2 were tested for the presence of anti-hantavirus IgM (A) and IgG (B) antibodies by SIA using affinity-purified recombinant ANDV and Seoul virus N antigen (18). As internal controls, two levels (+1 and +3) of human IgG were applied to the blot. Serum from a negative donor (−) and of a known HCPS-positive patient (+) were used as controls. Coomassie blue (CB) was used to determine the orientation of the strip. (C) Serum samples from patients S1 and S2 were divided in two. RNA was directly extracted from 300 μl of sample one without the addition of ApoH beads [(−) B; lanes 5 and 8]. In parallel, the second sample of each patient was submitted to an additional step of ANDV capture by ApoH-coated magnetic beads prior to RNA extraction [(+) B; lanes 6 and 9]. Extracted RNA was used as the template in a RT-PCR/heminested PCR assay performed as described in a previous report (10). As an additional control, total RNA extracted from sera of healthy negative donors with [(−) SC (+) B; lane 2] or without [(−) SC (−) B; lane 1] a step of virus capture and concentration by ApoH-coated magnetic beads was used as the negative control. Water controls for the RT-PCR (C1; lane 3) and heminested PCR (C2; lane 4) were included. In vitro-transcribed RNA corresponding to the ANDV S segment was used as a positive control for RT-PCR (HV RNA; lane 7). The arrow indicates the expected amplicon.
ANDV antigens are shed in the urine of HCPS patients.
Person-to-person transmission of ANDV has been reported (29, 35, 37, 51), but the mechanism of person-to-person virus dissemination remains to be elucidated. As hantaviruses are shed in the urine of infected rodents (21, 24, 41), we speculated that this biological fluid would be a good starting point to document ANDV shedding in infected humans. Additionally, a recent epidemiological study supports this possibility (10).
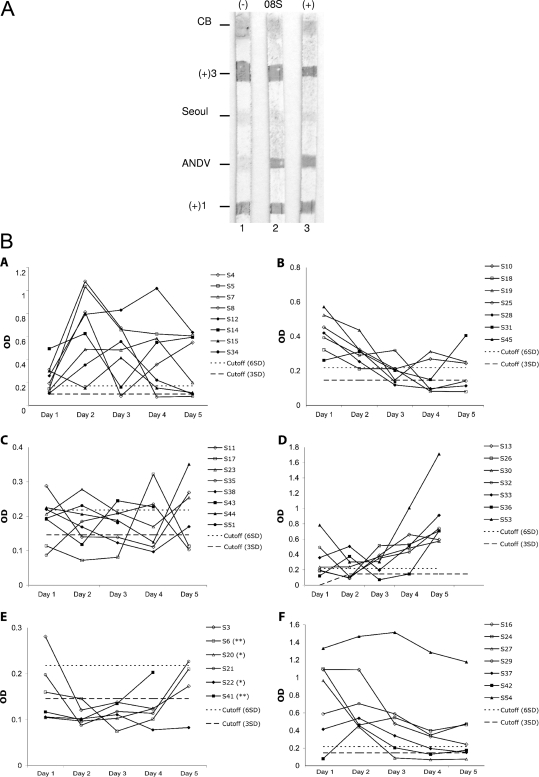
As a first approach for the validation of our experimental procedure, supernatants from infected cells containing known amounts of ANDV genomic equivalents (ranging from 2 × 104 to 1 × 105 as estimated by QRT-PCR) (10) were spiked in different volumes of noninfected urine samples. A fixed volume of 10 μl of a 50% slurry of ApoH-coated magnetic beads was added to each mixture. The beads were recovered and washed, and the RNA from viruses associated with the beads was isolated. The ANDV-RNA associated with the beads was quantified by real time RT-PCR, and the percentages of recovery from four independent experiments conducted using independent sources of virus (different cultures) are summarized in Table 1. ApoH-coated magnetic beads allowed the concentration of ANDV from a mixture of urine and virus-containing Vero E6 culture medium, confirming an ApoH-ANDV interaction. Although ApoH-coated magnetic beads proved effective for ANDV capture and concentration from serum (Fig. 1) and was advantageous for testing for virus in urine (Table 1), the overall procedure proved to be cumbersome and not suitable for the simultaneous screening of a great number of samples. Consequently, we evaluated the feasibility of using ApoH-coated 96-well ELISA plates in an ANDV high-throughput screening assay. Serum from a patient with acute HCPS (08S) with IgG reactive to ANDV antigens (Fig. 2A) was used as source of the primary antibodies, while a goat anti-human IgG HRP-conjugated antibody was used as a secondary antibody. Urine samples from 41 negative donors were used to establish the assay's cutoff value. The mean OD values (as defined in Materials and Methods) for 20 independent measurements using PBS (mean OD, 0.039 ± 0.011) or ANDV-negative urine samples (mean OD, 0.074 ± 0.024) was calculated. The cutoff for this screening procedure was established as the mean OD value obtained for the ANDV-negative donors plus three standard deviations (0.146) (Fig. 2B). Urine samples from 52 patients with acute ANDV HCPS (arbitrarily called S3 to S54), collected on different days (1 through 5) following their hospitalizations, were screened for ANDV antigens. For summaries of the row data, see Table S1 in the supplemental material (all patients tested) and Fig. 2B (only patients with a complete, 5-day series of data). When the experimental cutoff was established as the mean OD value obtained for the ANDV-negative donors plus three standard deviations (Fig. 2B), only 2 patients out of 52, namely, S20 and S22 (see Table S1 in the supplemental material; highlighted by asterisks), showed no sign of antigen shedding at any time posthospitalization (days 1 through 5). When the cutoff value was set as the mean OD value for ADNV-negative donors plus six standard deviations (0.218) (Fig. 2B), only three additional patients, S6, S41, and S52 (see Table S1 in the supplemental material; highlighted by double asterisks), showed no sign of antigen shedding at any time posthospitalization. Therefore, even with a stringent cutoff value (six standard deviations), 47 out of 52 HCPS patients tested positive for shedding ANDV antigens in urine on at least 1 day during the sample collection period (see Table S1 in the supplemental material) (Fig. 2B).
FIG. 2.
ANDV antigens are shed in the urine of HCPS patients. (A) Serum 08S, obtained from a known HCPS-positive patient, was tested for the presence of anti-hantavirus IgG antibodies by SIA using affinity-purified recombinant ANDV and Seoul virus N antigen (18). As internal controls, two levels (+1 and + 3) of human IgG were applied to the blot. Sera from a negative donor (−) and of a different HCPS-positive patient (+) were used as controls. Coomassie blue (CB) was used to determine the orientation of the strip. (B) ApoH-coated 96-well ELISA plates were used to screen for the presence of ANDV in urine. Serum 08S was used as source of the primary antibodies. The estimated cutoffs for three standard deviations (3SD) and six standard deviations (6SD) are indicated. Urine samples from 50 patients with confirmed acute ANDV-HCPS were collected on different days following hospitalization (1 through 5) and screened for virus.
Unexpectedly, the kinetics of antigen shedding fluctuated in all 47 patients who tested positive, hindering the establishment of a general pattern to describe the presence of viral antigens in urine (see Table S1 in the supplemental material) (Fig. 2B). Moreover, as this study was developed using previously collected frozen urine samples (from the years 2000 to 2002), we were unable to ascertain the exact day of infection and therefore were incapable of correlating our observations with the natural history of the ANDV infectious cycle. A correlation between the virus titer in serum (genomes/milliliter) and the presence of viral antigen in urine could not be established (data not shown), suggesting an unexplained complexity in antigen excretion in the urine of HCPS-infected individuals.
Detection of ANDV antigens in urine samples from HCPS patients by using anti-hantavirus monoclonal antibodies.
The preceding experiments relied on serum from a patient with acute HCPS (08S) as the source of the primary anti-ANDV antibodies (Fig. 2). Selection of the serum to be used as the hantavirus antibody source was not a minor issue, as circulating ApoH antibodies have been identified in the sera of patients with different infectious conditions (6, 9, 13, 16, 20, 55). Based on these observations, we next sought to challenge our findings by using monoclonal antibodies developed against the ANDV Gc glycoprotein, a protein found at the surface of the viral particle. For this purpose, two anti-ANDV Gc glycoprotein monoclonal antibodies, 2H4/F6 (anti-GcA) and 6C5/D12 (anti-GcB), were developed (Materials and Methods). Due to the limited amount of biological material, only four urine samples, from patients S46 (day 4), S12 (day 4), S33 (day 5), and S4 (day 1), were available for these additional tests. Each sample was evaluated with both antibodies (2H4/F6 and 6C5/D12), and each assay was conducted in triplicate for both 2H4/F6 and 6C5/D12. As before, the cutoff for this screening procedure using 2H4/F6 (anti-GcA) and 6C5/D12 (anti-GcB) monoclonal antibodies was established as the mean OD value obtained for the hantavirus-negative donors plus three or six standard deviations (Fig. 3; 0.069 or 0.094, respectively). In order to allow a direct comparison of the data, the final cutoff value was the highest value obtained considering both monoclonal antibodies. As shown in Fig. 3A, data were generated with each of the two antibody clusters, stressing the reproducibility of the developed assay. However, compared to serum 08S (Fig. 2B), the overall absorbance obtained with 2H4/F6 and 6C5/D12 was low, as were the antibody background levels (compare cutoff values for serum 08S and monoclonal antibodies), an observation most probably related to the use of polyclonal (08S) versus monoclonal (2H4/F6 and 6C5/D12) antibodies as shown in Fig. 2 versus Fig. 3, respectively. Next, we sought to evaluate ANDV antigen shedding in urine by using the 2H4/F6 and 6C5/D12 monoclonal antibodies. For these assays, urine samples (day 1 through 5) from three patients, S12, S19, and S29 were used. The selection of patients was strictly related to urine sample availability. As expected from earlier experiments (Fig. 3A), compared to serum 08S (Fig. 2B), the read absorbance and cutoff values with both monoclonal antibodies was low, yet the overall trend obtained (day 1 through 5) using 2H4/F6 and 6C5/D12 was comparable to that seen for 08S (Fig. 2B and Fig. 3B). In consequence, and based on these observations, we conclude that our previous data are reliable and extend our observations by asserting that glycoproteins of at least ANDV are shed in urine of HCPS patients.
FIG. 3.
Anti-ANDV glycoprotein monoclonal antibodies detect ANDV antigens in the urine of HCPS patients. (A) ApoH-coated 96-well ELISA plates were used to screen for the presence of ANDV in the urine of patients S4 (day 1) [S4(d1)], S12 (day 4) [S12(d4)], S33 (day 5) [S33(d5)], S37 (day 2) [S37(d2)], and S46 (day 4) [S46(d4)] on specific days posthospitalization as described for Fig. 2B, but using anti-ANDV glycoprotein monoclonal antibodies 2H4/F6 (GcA) or 6C5/D12 (GcB). Each assay is presented in triplicate [designated (1) to (3)]. The estimated cutoffs for three standard deviations (3SD) and six standard deviations (6SD) are indicated. (B) Urine samples from patients S12, S19, and S29, collected on different days following hospitalization (1 through 5), were screened for ANDV using monoclonal antibodies 2H4/F6 (GcA) and 6C5/D12 (GcB). The estimated cutoffs for three and six standard deviations are indicated.
ANDV shed in urine samples of HCPS patients can be infectious.
We next sought to determine if ApoH-captured ANDV was to some degree infectious. In these experiments, urine samples (for 5 days) from 13 patients, S4, S5, S7, S9, S12, S13, S26, S29, S34, S36, S45, S53, and S54, selected based on availability and virus antigen concentration within the sample (see Table S1 in the supplemental material) (Fig. 2B), were overlaid onto ApoH-coated 96-well ELISA plates. Upon ApoH virus capture, the urine was discarded, wells were washed, and Vero E6 cells were directly overlaid onto the wells, and the plates were incubated overnight as described in Materials and Methods. Cells were recovered and kept in culture. Infected Vero E6 cells were periodically (days 8, 16, and 22 postinfection) tested for the presence of ANDV nucleocapsid protein by IF assay. At day 16 postinfection, ANDV-positive Vero E6 cells could be readily identified in two cultures, namely, S53 (day 4) and S54 (day 3), by indirect IF using a primary antibody that targets the viral nucleocapsid protein (Fig. 4A) (50). IF for the ANDV nucleocapsid protein also showed a positive result for Vero E6 cultures infected with samples S53 (day 4) and S54 (day 3) on day 22 postinfection (data not shown). New ANDV-positive Vero E6 cell cultures that originated from other urine samples were not identified at this later stage. To further confirm the presence of ANDV in S53 (day 4)- and S54 (day 3)-infected Vero E6 cells and their respective supernatants, total RNA was extracted from both compartments and used as the template in a direct one-step RT-PCR assay targeting the nucleoprotein coding region (genomic S RNA). Supporting our IF data, the presence of ANDV genomic RNA was confirmed for the cells (Fig. 4B, lanes 3 and 5) and their culture supernatants (Fig. 4B, lanes 4 and 6), suggesting active virus replication. Consequently, based on our observations, we conclude that ANDV-infected patients can shed infectious virus in urine.
DISCUSSION
The development of fast, sensitive, and reliable diagnostics is a key element in the control of emergent pathogens, such as hantavirus. Diagnosis of hantavirus is currently based on clinical and serological findings (25, 26, 36). Detection of hantavirus-specific IgM using recombinant N in an ELISA format is the most widely used test for diagnosing acute-phase hantaviral infections (26, 36). Direct viral detection by molecular techniques involving amplification of viral RNA by RT-PCR have been increasingly used; however, since the viremia in the acute phase of the disease is of relatively short duration, direct amplification is not a widely used technique and does not yet replace serology for diagnosis (48). One of the main issues concerning direct pathogen detection in clinical and environmental samples by molecular techniques is the generation of false-negative results. This problem is due partly to low pathogen concentrations in the biological samples normally available for these diagnostic assays and partly to the presence, in these samples, of inhibitors of nucleic acid amplification (1, 2). In this complex scenario, the use of an ApoH-based capture assay showed itself to be advantageous. Results indicate that when fixed to a solid matrix, ApoH can be used to capture and concentrate ANDV even when the virus present in complex biological mixtures, such as serum and urine, allowing detection of the virus by both direct immunological and molecular methods (Fig. 1 to 3). As shown in Fig. 1C, the ApoH capture assay increases the sensitivity of virus detection by a RT-PCR/heminested PCR (compare lanes 5 and 6 and lanes 8 and 9). This apparent enhancement in sensitivity most probably stems from the fact that virus is being concentrated from a larger sample volume (1.5 ml instead of 300 μl). Thus, even though the virus is present at only a low concentration, sufficient virus is pulled down to exceed the lower detection limit of the molecular method employed. Additionally, it is possible that inhibitors of RT-PCR, known to be present in complex biological samples, are washed out during the capture procedure. Either possibility highlights the potential utility of ApoH-ANDV interaction for the development of novel molecular approaches for virus detection.
Person-to-person transmission of HCPS in North America has never been documented, and contact with hantavirus-infected rodents remains the primary source of human exposure. However, in South America, sporadic person-to-person transmissions of ANDV have been reported (10, 29, 35, 37, 51). To date, the mechanism of virus dissemination in person-to-person-transmitted cases of HCPS remains obscure. Nevertheless, virus shedding by infected individuals is a sine qua non condition for person-to-person virus transmission. Consequently, our study helps shed some light on this issue by providing original observations which suggest that ANDV-infected individuals may shed infectious virus. We document the presence of ADNV antigens (see Table S1 in the supplemental material; polyclonal serum) (Fig. 2) and Gc glycoprotein (Fig. 3, monoclonal antibodies) in the urine of patients with acute HCPS. Since 1975, a total of 580 confirmed cases of ANDV-induced HCPS have been reported in Chile (to November 2008; Chilean Ministry of Health website, http://epi.minsal.cl/epi/html/bolets/reportes); thus, our study includes almost 10% of all confirmed HCPS cases. Strikingly, 90% of the tested individuals shed viral antigens in their urine (see Table S1 in the supplemental material) (Fig. 2B). Unexpectedly, our data show that ANDV antigen excretion in HCPS patients is not constant though time. Although puzzling, this observation is not without precedent, as earlier studies report that in both experimentally inoculated and wild-caught Seoul virus-infected rats (4, 54), experimentally inoculated Puumala-infected bank voles (15), wild-caught Sin Nombre virus-infected deer mice (40), and wild-caught ANDV-infected rodents (33), virus shedding in the urine and saliva follows fluctuating kinetics. These observations suggest that variations in antigen/virus concentrations in the urine of infected rodents (4, 15, 40, 54) and humans (Fig. 2B) may be a normal feature of the still ill-understood mechanism of virus dissemination.
Hantaviruses have been very difficult to isolate from human sources despite many attempts to do so (53). To date, there is only one report describing a human hantavirus isolate (ANDV isolate CHI-7913) in the Americas (11). In this case, ANDV CHI-7913 was isolated from a serum sample from a seropositive Chilean HCPS patient (11). Here, we show that ApoH captured infectious virus from the urine of patients with acute HCPS (2 of 65 samples tested). ANDV nucleocapsid protein was promptly identified in infected VeroE6 cells by indirect IF (Fig. 4A), and the presence of viral genome in both infected cells and their supernatants was confirmed by a direct RT-PCR (Fig. 4B), strongly implying active virus replication. Although the success rate was low (2 of 65), our observations suggest that urine might harbor minor quantities of infectious ANDV and strongly suggest that urine is a plausible source of infectious viral particles. Even though our data raise a number of concerns with respect to ANDV transmission, they should be regarded with caution, as sequencing of the S segment revealed that both urine isolates were identical to the published sequence for ANDV isolate CHI-7913 (GenBank accession no. AY228237). The exact meaning of this observation is still not clear.
It should be stressed that our study remains qualitative and does not describe the absolute amount of antigens or infectious viral particles shed in urine. In light of the tantalizing insight into ANDV transmission that the present data provide, quantitative measurements of genomic RNA content, quantitative assessments of virus infectivity, and a full characterization of ANDV infectivity will be addressed in future studies.
In summary, we demonstrate that ApoH binds ANDV and can be used to capture the virus from complex biological mixtures. Using the ApoH capture assay, we show that ANDV antigens are found in urine samples of 47 out of 52 tested patients with acute HCPS. Moreover, we show that infectious ANDV, albeit in very low concentrations, was found in the urine samples from two patients. Together, these data not only lend support to the possibility that during human infection ANDV might be shed in urine but also raise the intriguing prospect that infectious virus might be present in other biological secretions. Interestingly, other members of the New World Hantavirus group, such as Sin Nombre virus, which do not show person-to-person transmission, are not shed in urine, and infectious virus is not found in other biological specimens, such as tracheal aspirate (53). Therefore, the ability of infectious ANDV to be shed in biological fluid might represent a unique mechanism that confers to this virus the ability to be transmitted from person to person.
Supplementary Material
Acknowledgments
We thank T. Ksiazek (CDC, Atlanta, GA) and B. Hjelle (University of New Mexico, Albuquerque, NM) for kindly providing hantavirus-associated reagents and G. Mertz and his associates in the NIH/NIAID UNM/Chile ICIDR program (AI 45452) for sharing serum and urine samples from patients with acute HCPS. We are grateful to C. Villota for assistance with the microscopy and M. Rau for critical reading and editing of the manuscript.
This work was supported by EU grant LSHB-CT-2006-037560, Ultra-Sensitive Diagnosis for Emerging Pathogens (USDEP) project, to M.L.-L., F.V., and E.S.; the Jeunes Equipes Associées à l'IRD (JEAI) program and grant PCBT/RUE 25 to M.L.-L.; and U.S. Public Health Service grant AI 45452 to M.F. and P.V. P.R. was supported by a MECESUP-Universidad Andrés Bello doctoral fellowship. M.L.-L. and D.M. are members of the Núcleo Milenio de Inmunología e Inmunoterapia (NMII). D.M. was initially supported by a NMII postdoctoral fellowship and currently holds a FONDECYT (3085029) postdoctoral fellowship.
Footnotes
Published ahead of print on 11 March 2009.
Supplemental material for this article may be found at http://jvi.asm.org/.
REFERENCES
- 1.Al-Soud, W. A., L. J. Jonsson, and P. Radstrom. 2000. Identification and characterization of immunoglobulin G in blood as a major inhibitor of diagnostic PCR. J. Clin. Microbiol. 38345-350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Soud, W. A., and P. Radstrom. 2001. Purification and characterization of PCR-inhibitory components in blood cells. J. Clin. Microbiol. 39485-493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Balasubramanian, K., and A. J. Schroit. 1998. Characterization of phosphatidylserine-dependent beta2-glycoprotein I macrophage interactions: implications for apoptotic cell clearance by phagocytes. J. Biol. Chem. 27329272-29277. [DOI] [PubMed] [Google Scholar]
- 4.Botten, J., K. Mirowsky, C. Ye, K. Gottlieb, M. Saavedra, L. Ponce, and B. Hjelle. 2002. Shedding and intracage transmission of Sin Nombre hantavirus in the deer mouse (Peromyscus maniculatus) model. J. Virol. 767587-7594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Courouble, P., D. Vanpee, E. Delgrange, J. Donckier, J. M. Pochet, and J. B. Gillet. 2001. Hantavirus infections: clinical presentation in the emergency room. Eur. J. Emerg. Med. 817-20. [DOI] [PubMed] [Google Scholar]
- 6.de Larrañaga, G. F., R. R. Forastiero, L. O. Carreras, and B. S. Alonso. 1999. Different types of antiphospholipid antibodies in AIDS: a comparison with syphilis and the antiphospholipid syndrome. Thromb. Res. 9619-25. [DOI] [PubMed] [Google Scholar]
- 7.Del Papa, N., Y. H. Sheng, E. Raschi, D. A. Kandiah, A. Tincani, M. A. Khamashta, T. Atsumi, G. R. Hughes, K. Ichikawa, T. Koike, G. Balestrieri, S. A. Krilis, and P. L. Meroni. 1998. Human beta 2-glycoprotein I binds to endothelial cells through a cluster of lysine residues that are critical for anionic phospholipid binding and offers epitopes for anti-beta 2-glycoprotein I antibodies. J. Immunol. 1605572-5578. [PubMed] [Google Scholar]
- 8.Dull, S. M., J. C. Brillman, S. Q. Simpson, and D. P. Sklar. 1994. Hantavirus pulmonary syndrome: recognition and emergency department management. Ann. Emerg. Med. 24530-536. [DOI] [PubMed] [Google Scholar]
- 9.Faghiri, Z., W. A. Wilson, F. Taheri, E. N. Barton, O. S. Morgan, and A. E. Gharavi. 1999. Antibodies to cardiolipin and beta2-glycoprotein-1 in HTLV-1-associated myelopathy/tropical spastic paraparesis. Lupus 8210-214. [DOI] [PubMed] [Google Scholar]
- 10.Ferres, M., P. Vial, C. Marco, L. Yanez, P. Godoy, C. Castillo, B. Hjelle, I. Delgado, S. J. Lee, and G. J. Mertz. 2007. Prospective evaluation of household contacts of persons with hantavirus cardiopulmonary syndrome in Chile. J. Infect. Dis. 1951563-1571. [DOI] [PubMed] [Google Scholar]
- 11.Galeno, H., J. Mora, E. Villagra, J. Fernandez, J. Hernandez, G. J. Mertz, and E. Ramirez. 2002. First human isolate of hantavirus (Andes virus) in the Americas. Emerg. Infect. Dis. 8657-661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gao, P. J., Y. F. Piao, X. D. Liu, L. K. Qu, Y. Shi, X. C. Wang, and H. Y. Yang. 2003. Studies on specific interaction of beta-2-glycoprotein I with HBsAg. World J. Gastroenterol. 92114-2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.González, C., A. Lestón, B. García-Berrocal, A. Sánchez-Rodriguez, J. A. Martín-Oterino, I. Alberca, M. Cordero, R. Jorge, J. A. Navajo, and J. M. González-Buitrago. 1999. Antiphosphatidylserine antibodies in patients with autoimmune diseases and HIV-infected patients: effects of Tween 20 and relationship with antibodies to β2-glycoprotein I. J. Clin. Lab. Anal. 1359-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guerin, J., Y. Sheng, S. Reddel, G. M. Iverson, M. G. Chapman, and S. A. Krilis. 2002. Heparin inhibits the binding of beta 2-glycoprotein I to phospholipids and promotes the plasmin-mediated inactivation of this blood protein: elucidation of the consequences of the two biological events in patients with the anti-phospholipid syndrome. J. Biol. Chem. 2772644-2649. [DOI] [PubMed] [Google Scholar]
- 15.Hardestam, J., M. Karlsson, K. I. Falk, G. Olsson, J. Klingstrom, and A. Lundkvist. 2008. Puumala hantavirus excretion kinetics in bank voles (Myodes glareolus). Emerg. Infect. Dis. 141209-1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harel, M., A. Aron-Maor, Y. Sherer, M. Blank, and Y. Shoenfeld. 2005. The infectious etiology of the antiphospholipid syndrome: links between infection and autoimmunity. Immunobiology 210743-747. [DOI] [PubMed] [Google Scholar]
- 17.Harper, M. F., P. M. Hayes, B. R. Lentz, and R. A. Roubey. 1998. Characterization of beta2-glycoprotein I binding to phospholipid membranes. Thromb. Haemost. 80610-614. [PubMed] [Google Scholar]
- 18.Hjelle, B., S. Jenison, N. Torrez-Martinez, B. Herring, S. Quan, A. Polito, S. Pichuantes, T. Yamada, C. Morris, F. Elgh, H. W. Lee, H. Artsob, and R. Dinello. 1997. Rapid and specific detection of Sin Nombre virus antibodies in patients with hantavirus pulmonary syndrome by a strip immunoblot assay suitable for field diagnosis. J. Clin. Microbiol. 35600-608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jonsson, C. B., J. Hooper, and G. Mertz. 2008. Treatment of hantavirus pulmonary syndrome. Antivir. Res. 78162-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kalt, M., and E. Gertner. 2001. Antibodies to beta 2-glycoprotein I and cardiolipin with symptoms suggestive of systemic lupus erythematosus in parvovirus B19 infection. J. Rheumatol. 282335-2336. [PubMed] [Google Scholar]
- 21.Kariwa, H., M. Fujiki, K. Yoshimatsu, J. Arikawa, I. Takashima, and N. Hashimoto. 1998. Urine-associated horizontal transmission of Seoul virus among rats. Arch. Virol. 143365-374. [DOI] [PubMed] [Google Scholar]
- 22.Kilpatrick, E. D., M. Terajima, F. T. Koster, M. D. Catalina, J. Cruz, and F. A. Ennis. 2004. Role of specific CD8+ T cells in the severity of a fulminant zoonotic viral hemorrhagic fever, hantavirus pulmonary syndrome. J. Immunol. 1723297-3304. [DOI] [PubMed] [Google Scholar]
- 23.Köhler, G., and C. Milstein. 1975. Continuous cultures of fused cells secreting antibody of predefined specificity. Nature 256495-497. [DOI] [PubMed] [Google Scholar]
- 24.Lee, H. W., P. W. Lee, L. J. Baek, C. K. Song, and I. W. Seong. 1981. Intraspecific transmission of Hantaan virus, etiologic agent of Korean hemorrhagic fever, in the rodent Apodemus agrarius. Am. J. Trop. Med. Hyg. 301106-1112. [DOI] [PubMed] [Google Scholar]
- 25.Lee, H. W., C. Calisher, and C. Schmaljohn (ed.). 1999. Manual of hemorrhagic fever with renal syndrome and hantavirus pulmonary syndrome. WHO Collaborating Center for Virus Reference and Research (Hantaviruses), Asan Institute for Life Sciences, Seoul, Korea.
- 26.Li, Z., X. Bai, and H. Bian. 2002. Serologic diagnosis of Hantaan virus infection based on a peptide antigen. Clin. Chem. 48645-647. [PubMed] [Google Scholar]
- 27.Luplertlop, N., D. Misse, D. Bray, V. Deleuze, J. P. Gonzalez, V. Leardkamolkarn, H. Yssel, and F. Veas. 2006. Dengue-virus-infected dendritic cells trigger vascular leakage through metalloproteinase overproduction. EMBO Rep. 71176-1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maes, P., J. Clement, I. Gavrilovskaya, and M. Van Ranst. 2004. Hantaviruses: immunology, treatment, and prevention. Viral Immunol. 17481-497. [DOI] [PubMed] [Google Scholar]
- 29.Martinez, V. P., C. Bellomo, J. San Juan, D. Pinna, R. Forlenza, M. Elder, and P. J. Padula. 2005. Person-to-person transmission of Andes virus. Emerg. Infect. Dis. 111848-1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mehdi, H., M. J. Kaplan, F. Y. Anlar, X. Yang, R. Bayer, K. Sutherland, and M. E. Peeples. 1994. Hepatitis B virus surface antigen binds to apolipoprotein H. J. Virol. 682415-2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mertz, G. J., B. Hjelle, M. Crowley, G. Iwamoto, V. Tomicic, and P. A. Vial. 2006. Diagnosis and treatment of new world hantavirus infections. Curr. Opin. Infect. Dis. 19437-442. [DOI] [PubMed] [Google Scholar]
- 32.Muranyi, W., U. Bahr, M. Zeier, and F. J. van der Woude. 2005. Hantavirus infection. J. Am. Soc. Nephrol. 163669-3679. [DOI] [PubMed] [Google Scholar]
- 33.Padula, P., R. Figueroa, M. Navarrete, E. Pizarro, R. Cadiz, C. Bellomo, C. Jofre, L. Zaror, E. Rodriguez, and R. Murua. 2004. Transmission study of Andes hantavirus infection in wild sigmodontine rodents. J. Virol. 7811972-11979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Padula, P. J., S. B. Colavecchia, V. P. Martínez, M. O. Gonzalez Della Valle, A. Edelstein, S. D. L. Miguel, J. Russi, J. Mora Riquelme, N. Colucci, M. Almirón, and R. D. Rabinovich. 2000. Genetic diversity, distribution, and serological features of hantavirus infection in five countries in South America. J. Clin. Microbiol. 383029-3035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Padula, P. J., A. Edelstein, S. D. Miguel, N. M. Lopez, C. M. Rossi, and R. D. Rabinovich. 1998. Hantavirus pulmonary syndrome outbreak in Argentina: molecular evidence for person-to-person transmission of Andes virus. Virology 241323-330. [DOI] [PubMed] [Google Scholar]
- 36.Padula, P. J., C. M. Rossi, M. O. Della Valle, P. V. Martinez, S. B. Colavecchia, A. Edelstein, S. D. Miguel, R. D. Rabinovich, and E. L. Segura. 2000. Development and evaluation of a solid-phase enzyme immunoassay based on Andes hantavirus recombinant nucleoprotein. J. Med. Microbiol. 49149-155. [DOI] [PubMed] [Google Scholar]
- 37.Pinna, D. M., V. P. Martinez, C. M. Bellomo, C. Lopez, and P. Padula. 2004. New epidemiologic and molecular evidence of person to person transmission of hantavirus Andes Sout. Medicina (Buenos Aires) 6443-46. (In Spanish.) [PubMed] [Google Scholar]
- 38.Reference deleted.
- 39.Plyusnin, A., O. Vapalahti, and A. Vaheri. 1996. Hantaviruses: genome structure, expression and evolution. J. Gen. Virol. 772677-2687. [DOI] [PubMed] [Google Scholar]
- 40.Safronetz, D., M. A. Drebot, H. Artsob, T. Cote, K. Makowski, and L. R. Lindsay. 2008. Sin Nombre virus shedding patterns in naturally infected deer mice (Peromyscus maniculatus) in relation to duration of infection. Vector Borne Zoonotic Dis. 897-100. [DOI] [PubMed] [Google Scholar]
- 41.Safronetz, D., R. Lindsay, A. Dibernardo, B. Hjelle, R. Xiao, H. Artsob, and M. A. Drebot. 2005. A preliminary study of the patterns of Sin Nombre viral infection and shedding in naturally infected deer mice (Peromyscus maniculatus). Vector Borne Zoonotic Dis. 5127-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schmaljohn, C. S. 1999. Hantavirus (Bunyaviridae), p. 621-630. In A. Granoff and R. G. Webster (ed.), Encyclopedia of virology, 2nd ed., vol. 1. Academic Press Limited, San Diego, CA. [Google Scholar]
- 43.Schmaljohn, C. S., and J. M. Dalrymple. 1983. Analysis of Hantaan virus RNA: evidence for a new genus of Bunyaviridae. Virology 131482-491. [DOI] [PubMed] [Google Scholar]
- 44.Schousboe, I. 1988. Inositolphospholipid-accelerated activation of prekallikrein by activated factor XII and its inhibition by beta 2-glycoprotein I. Eur. J. Biochem. 176629-636. [DOI] [PubMed] [Google Scholar]
- 45.Schwarzenbacher, R., K. Zeth, K. Diederichs, A. Gries, G. M. Kostner, P. Laggner, and R. Prassl. 1999. Crystal structure of human beta2-glycoprotein I: implications for phospholipid binding and the antiphospholipid syndrome. EMBO J. 186228-6239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stefas, E., M. Rucheton, H. Graafland, M. Moynier, C. Sompeyrac, E. M. Bahraoui, and F. Veas. 1997. Human plasmatic apolipoprotein H binds human immunodeficiency virus type 1 and type 2 proteins. AIDS Res. Hum. Retrovir. 1397-104. [DOI] [PubMed] [Google Scholar]
- 47.Stefas, I., M. Rucheton, A. D. D'Angeac, C. Morel-Baccard, J. M. Seigneurin, J. P. Zarski, M. Martin, M. Cerutti, J. P. Bossy, D. Misse, H. Graafland, and F. Veas. 2001. Hepatitis B virus Dane particles bind to human plasma apolipoprotein H. Hepatology 33207-217. [DOI] [PubMed] [Google Scholar]
- 48.Terajima, M., J. D. Hendershot III, H. Kariwa, F. T. Koster, B. Hjelle, D. Goade, M. C. DeFronzo, and F. A. Ennis. 1999. High levels of viremia in patients with the hantavirus pulmonary syndrome. J. Infect. Dis. 1802030-2034. [DOI] [PubMed] [Google Scholar]
- 49.Tischler, N. D., J. Fernandez, I. Muller, R. Martinez, H. Galeno, E. Villagra, J. Mora, E. Ramirez, M. Rosemblatt, and P. D. Valenzuela. 2003. Complete sequence of the genome of the human isolate of Andes virus CHI-7913: comparative sequence and protein structure analysis. Biol. Res. 36201-210. [DOI] [PubMed] [Google Scholar]
- 50.Tischler, N. D., M. Rosemblatt, and P. D. Valenzuela. 2008. Characterization of cross-reactive and serotype-specific epitopes on the nucleocapsid proteins of hantaviruses. Virus Res. 1351-9. [DOI] [PubMed] [Google Scholar]
- 51.Wells, R. M., S. Sosa Estani, Z. E. Yadon, D. Enria, P. Padula, N. Pini, J. N. Mills, C. J. Peters, E. L. Segura, et al. 1997. An unusual hantavirus outbreak in southern Argentina: person-to-person transmission? Emerg. Infect. Dis. 3171-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wilson, M., L. Otth, H. Fernandez, I. Hofmann, and M. Navarrete. 2001. Antibodies anti-Chlamydia pneumoniae and anti-Mycoplasma pneumoniae in patients with negative serology for hantavirus: retrospective study. Mem. Inst. Oswaldo Cruz 961135-1136. [DOI] [PubMed] [Google Scholar]
- 53.Xiao, R., S. Yang, F. Koster, C. Ye, C. Stidley, and B. Hjelle. 2006. Sin Nombre viral RNA load in patients with hantavirus cardiopulmonary syndrome. J. Infect. Dis. 1941403-1409. [DOI] [PubMed] [Google Scholar]
- 54.Yanagihara, R., H. L. Amyx, and D. C. Gajdusek. 1985. Experimental infection with Puumala virus, the etiologic agent of nephropathia epidemica, in bank voles (Clethrionomys glareolus). J. Virol. 5534-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yuste, J. R., and J. Prieto. 2003. Anticardiolipin antibodies in chronic viral hepatitis. Do they have clinical consequences? Eur. J. Gastroenterol. Hepatol. 15717-719. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.