Abstract
Nipah (NiV) and Hendra (HeV) viruses are emerging zoonotic paramyxoviruses that cause encephalitis in humans, with fatality rates of up to 75%. We designed a new high-throughput screening (HTS) assay for inhibitors of infection based on envelope glycoprotein pseudotypes. The assay simulates multicycle replication and thus identifies inhibitors that target several stages of the viral life cycle, but it still can be carried out under biosafety level 2 (BSL-2) conditions. These features permit a screen for antivirals for emerging viruses and select agents that otherwise would require BSL-4 HTS facilities. The screening of a small compound library identified several effective molecules, including the well-known compound chloroquine, as highly active inhibitors of pseudotyped virus infection. Chloroquine inhibited infection with live HeV and NiV at a concentration of 1 μM in vitro (50% inhibitory concentration, 2 μM), which is less than the plasma concentrations present in humans receiving chloroquine treatment for malaria. The mechanism for chloroquine's antiviral action likely is the inhibition of cathepsin L, a cellular enzyme that is essential for the processing of the viral fusion glycoprotein and the maturation of newly budding virions. Without this processing step, virions are not infectious. The identification of a compound that inhibits a known cellular target that is important for viral maturation but that had not previously been shown to have antiviral activity for henipaviruses highlights the validity of this new screening assay. Given the established safety profile and broad experience with chloroquine in humans, the results described here provide an option for treating individuals infected by these deadly viruses.
Nipah (NiV) and Hendra (HeV) viruses are newly emerging zoonoses that cause encephalitis in humans, with fatality rates of up to 75% (3, 7, 8, 12, 13, 30). NiV has caused at least nine significant outbreaks in Bangladesh and India since its emergence in Malaysia in 1998 (3, 7, 8, 12, 13, 30). The virus emerged from the fruit bat (flying fox) mammalian reservoir, via the pig, into the human population. However, direct transmission from bats to humans can bypass the pig host, and person-to-person transmission also has now become a primary mode of NiV spread (2, 5). HeV, via the same bat host, has caused disease in horses, with transmission to horse-handlers and veterinarians, and since 1995 has caused sporadic illness in Australia (12). Both viruses, in addition to acute disease, may cause asymptomatic infection in up to 60% of exposed people and may lead to late-onset disease or the relapse of encephalitis years after initial infection (25), as well as persistent or delayed neurological sequelae (11). The vast geographic range of the fruit bat mammalian reservoir raises the possibility of a wide spread of these human diseases, which presently have no clinical treatment or vaccine.
The first step in infection with HeV or NiV is binding to the target cells, via the interaction of the viral envelope protein (G) with specific receptor molecules on the cell surface. The receptor for HeV is Ephrin B2 (EFNB2) and for NiV is either EFNB2 or EFNB3 (11). The fusion of the viral envelope with the plasma membrane of the cell is then mediated by the viral fusion protein (F). The F protein is synthesized as a precursor protein (F0) that is proteolytically processed posttranslationally to form a trimer of disulfide-linked heterodimers (F1 + F2). This cleavage event places the fusion peptide at the F1 terminus in the mature F protein and is essential for membrane fusion activity. During viral entry, the fusion peptides, which are buried in the F trimer, must be exposed transiently so that they can insert into the target cell membrane. The conformational change that leads to the exposure of the fusion peptides requires an activation step (22), which is initiated by the interaction of G with its receptor. Only virions bearing the mature, cleaved F can undergo activation and thus are infectious (4, 14, 15).
We introduce here a biosafety level 2 (BSL-2)-amenable high-throughput screening (HTS) assay (9) for inhibitors that target several stages of the henipavirus viral cycle, based on envelope glycoprotein pseudotypes. The cell-based assay allows for the simultaneous evaluation of antiviral activity and the cytotoxicity of compounds. We have validated the method with several different classes of henipavirus entry inhibitors as well as protease inhibitors. For this assay, HeV envelope glycoproteins were pseudotyped onto a recombinant vesicular stomatitis virus (VSV) that expresses red fluorescent protein (RFP) but lacks its attachment protein, G (19, 20). The resulting pseudotyped virus bears the HeV binding and fusion proteins. The infection of target cells by pseudotyped virus in the absence and presence of compounds is quantified by assessing the production of red fluorescence. This pseudotyped viral entry assay, unlike previous ones (31), simulates multicycle replication because the monolayer cells, which express viral glycoproteins, will generate more pseudotyped particles when infected. Compounds found to be active in this assay may be those that either block binding, interfere with F activation or fusion, or interfere with the protease processing of F. However, the assay is safe, because these particles can only produce infectious progeny in cells expressing HeV G/F. These features allow experimentation and antiviral assessment for emerging viruses and select agents that otherwise would require BSL-4 HTS facilities. We report the use of this screen to discover effective inhibitors of henipavirus replication and the evaluation of a well-known compound with previously unidentified properties that may allow its immediate use for henipaviruses.
MATERIALS AND METHODS
Cells and virus.
293T (human kidney epithelial) and Vero (African green monkey kidney) cells were grown in Dulbecco's modified Eagle's medium (DMEM; Mediatech-Cellgro) supplemented with 10% fetal bovine serum and antibiotics at 37°C in 5% CO2. For Newcastle disease virus (NDV) infections, we used a recombinant green fluorescent protein (GFP)-expressing NDV B1 (vaccine strain) virus. Pseudotyped viruses were generated using VSV-ΔG-RFP, a recombinant VSV derived from the cDNA of VSV Indiana in which the G gene is replaced with the Ds-Red gene. Pseudotypes with HeV F and G were generated as described previously (28). Briefly, 293T cells were transfected with either VSV-G, HeV-G CT32 and HeV F, HeV-G CT32, HeV-F, or NDV-AV F. Twenty-four hours posttransfection, the dishes were washed and infected (multiplicity of infection [MOI] of 0.5) with VSV-ΔG-RFP complemented with VSV-G or NDV-B1-GFP (17). Supernatant fluid containing pseudotyped virus (HeV F/CT32-G or VSV-G) was collected 18 h postinfection and stored at −80°C. For single-cycle (entry only) infection assays, the HeV F/CT32-G or VSV-G pseudotype was used at an MOI of 0.25 to infect Vero cells in the absence of serum. For live virus testing with HeV or NiV, compounds were diluted serially five times by 1/2 log and analyzed as described previously (1). Briefly, compounds were mixed with cells and virus was added and incubated overnight, and then cells were fixed in methanol, removed from the BSL-4 facility, immunolabeled with polyclonal anti-N antibodies, and stained with horseradish peroxidase-conjugated anti-rabbit antisera. Viral proteins then were detected using a chemiluminescent horseradish peroxidase substrate reaction and read in a luminometer. Viral titers from each well were measured.
Chemicals.
Compound screening libraries that include marketed drugs, natural products, and combinatorially elaborated active pharmacophores were purchased from ChemDiv Inc., San Diego, CA; Cerep SA, Paris, France; Prestwick Inc., Strasbourg, France; and Microsource Discovery Systems Incorporated, Gaylordsville, CT. The MicroSource Spectrum Collection contains 2,000 biologically active compounds, including a diverse set of pure natural products. The ChemDiv Library contains 21,000 structurally diverse compounds based on 125 combinatorial templates. The Cerep Odyssey II collection contains 4,000 compounds derived from about 350 scaffolds, onto which biologically relevant pharmacophores were reacted with diverse sets of partners (more than 1,000 diversity points) to obtain final compounds with drug-like properties. The Prestwick library contains 880 compounds, of which more than 85% are marketed drugs. All libraries were received as powders, dissolved in dimethylsulfoxide (DMSO) to 5 mM, distributed in aliquots, and stored at −20°C until use.
Chloroquine diphosphate salt was obtained from MP Biomedicals (catalog no. 193919); quinine sulfate (catalog no. Q0132) and primaquine diphosphate (catalog no. 160393) were obtained from Sigma-Aldrich.
Pseudotyped entry assay mimicking multicycle replication.
HeV CT32-G and F glycoproteins were pseudotyped onto VSV-ΔG-RFP, and the resulting pseudotyped viruses were used to infect viral HeV glycoprotein-expressing cells for a simulation of multicycle replication. RFP production at 24, 48, and 72 h was analyzed by spectral emission confocal microscopy, which was performed with the Nikon C1-si system and on a microplate fluorescence reader (Spectramax M5).
Flow cytometry.
Flow cytometry was performed on a BD FACS Vantage SE with DiVa upgrade (BD Biosciences, San Jose, CA) equipped with a Stabilite 2017 argon laser tuned to 488 nm and a BeamLok 2060 argon-krypton laser tuned to 568 nm, both from Spectra-Physics (Mountain View, CA) at the Hospital for Special Surgery (New York, NY). For RFP detection, the cells were excited with the 568-nm laser, and the fluorescence of RFP emission was quantified after being passed through a BP610/20-nm filter.
Plasmids and reagents.
HeV wild-type (WT) G and WT F in pCAGGS were a gift from Lin-Fa Wang. NDV-AV F was a gift from Ronald Iorio. To generate the shortened cytoplasmic tail variant of HeV G (HeV G-CT32), an internal primer containing an EcoRI site and initiating at position 32 of the open reading frame was used for nested PCR. The primer sequence was 5′ GGAATTCGGCACAATGGACATCAAG 3′.
Antibodies.
Polyclonal antibodies were raised in rabbits by DNA immunization with plasmids expressing Hendra G and Hendra F (Genovac).
HeV viral entry compound screening. (i) Primary screening protocol.
A 25-μl volume of 104 293T cells that had been transfected with plasmids encoding HeV G and F and also with Venus-yellow fluorescent protein (YFP) was dispensed into 384-well polystyrene black/clear-bottom plates using a Matrix WellMate dispenser. The library compounds were stored as 5 mM stock solutions in DMSO in 384-well polypropylene microtiter plates and transferred into the cell-containing plates using a Perkin-Elmer Janus automated pipetting system, with a 384-well, 100-nl pin tool, to give a 10 μM final compound concentration. The plates then were centrifuged, and 25 μl of the pseudotyped VSV-ΔG-RFP virus stocks subsequently were added using a Matrix WellMate. The microtiter plates were incubated at 37°C for 48 h, frozen and thawed, and then read for two-channel fluorescence intensity in a Perkin-Elmer EnVision multifunction plate reader. For detecting RFP expression levels, the wells were read from the top with a 535-nm (40-nm bandpass) excitation filter and a 579-nm (25-nm bandpass) emission filter. For the detection of YFP expression, the wells were read from the bottom with a 510-nm (10-nm bandpass) excitation filter and 535-nm (25-nm bandpass) emission filter. To ensure the assays were not contaminated with bacteria, an additional read of absorbance at 590 nm was performed.
(ii) Data processing and normalization.
All HTS data were stored and processed using BioAssay Enterprise version 10.1 (CambridgeSoft Inc., Cambridge, MA, USA). GraphPad Prism 5 software also was used for generating concentration response curves for selected chloroquine analogs, using the nonlinear method of least squares. The basic assumption of the assay is that a compound that blocks the entry of the virus would manifest itself by a reduction in the expression of RFP alone and have no effect on general protein expression as manifested by YFP. Therefore, the final percent inhibition calculation included a ratio of the red channel to the yellow channel as counts579 nM/counts535 nM.
In every microtiter plate, controls included 16 wells with DMSO only (blank) and 16 wells with a peptide inhibitor (positive control) at sufficient concentration (1 μM) to block 100% of viral entry. An average of these control values was used in the calculation of percent inhibition.
The final percent inhibition was calculated with the formula [(ratiotest compound − ratioblank)/(ratiopeptide inhibitor − ratioblank)] × 100.
The Z′ values were used as an assessment of quality (32), using the 16 values of the peptide inhibitor and the blank for each microtiter plate with the formula 1 − [(3 × SDpeptide + 3 × SDblank)/(averagepeptide − averageblank)], where SD is standard deviations.
(iii) Concentration-response curves.
Compounds were picked by a Janus 8-tip VariSpan automated syringe pipette. A 5 mM compound stock solution (1.35 μl) in DMSO was transferred to a 384-well microtiter plate containing 28 μl of cell culture medium (Optimem, Invitrogen), yielding a 225 μM compound concentration. Eight twofold serial dilutions were made, and 5 μl of the above mixture was introduced into a 50-μl assay (as described above) to yield final concentrations of 20, 10, 5, 2.5, 1.25, 0.625, 0.3125, and 0.1562 μM. Assays were measured as described above. To calculate the 50% inhibitory concentration (IC50), the resulting data were fit to the symmetrical sigmoidal log concentration response equation % inhibition = maximal inhibition + [(minimal inhibition − maximal inhibition)/(1 + 10concentration − Log IC50)]. In cases where there was a poor fit (R2 < 0.8), the data were fit to a straight line or were considered inactive.
RESULTS
A new multicycle viral replication assay enables assessment of high-risk viral pathogens under BSL-2 conditions.
The strategy of the multicycle replication assay described above is diagrammed in Fig. 1a. Figure 1b and c establish the optimal conditions for this assay and show that infection, as measured by relative fluorescence units (RFU), is consistent in 96-well plates across a wide range of particle-forming units (PFU) and cell densities (x axis). In the experiment shown in Fig. 1b, different numbers of cells expressing HeV G/F (x axis) were infected with different numbers of pseudotyped VSV-ΔG-RFP-HeV F/G PFU in 96-well plates, and RFU (y axis) were measured after 72 h. The most favorable cell density for the assay occurs at 4 × 104 cells, since infection attains maximum values (RFU) regardless of the PFU/well. The highest fluorescence intensity in this experiment was obtained by infecting 4 × 104 cells with 80,000 PFU. The assay is reliably quantitative across a wide range of PFU/well, from approximately 625 to 80,000 PFU (Fig. 1c). However, the use of an intermediate number of PFU to initiate infection most clearly allows the effects of multicycle replication to be seen, because it spares the majority of cells from the initial round of infection so that they may be infected during later cycles. This condition allowed us to distinguish between the effect of compounds on receptor binding, F activation, fusion, and postinfection processing.
FIG. 1.
New multicycle viral replication assay. (a) When HeV G and F pseudotyped viruses infect permissive cells, red fluorescent cells indicate viral entry (top), and emerging particles are noninfectious. However, when the pseudotypes infect viral glycoprotein (G/F)-expressing cells (bottom), multicycle replication is simulated. New pseudotyped virions result from the budding of particles bearing the cell surface-expressed HeV G/F molecules. (b) Assay response is reliable across a range of virus-to-cell ratios. G/F-expressing cells in 96-well plates in the indicated numbers were infected with pseudotypes as shown. RFU were determined at 48 h postinfection. The most favorable cell density for the assay occurs at 4 × 104 cells, when the infection attains maximum RFU regardless of the PFU/well. (c) Multicycle replication is enriched by the use of an intermediate PFU range to infect 4 × 104 cells. Infection (RFU) was assessed at 24, 48, and 72 h, and the percent increase in infection during each 24-h period was calculated. While a greater PFU led to a greater percent increase in infection in the 24- to 48-h period, an intermediate PFU led to the greatest increase in infection for the 48- to 72-h period.
Inhibition of specific stages of the viral life cycle by soluble receptor competition, glycoprotein processing inhibition, and antibody neutralization: multicycle assay replicates live viral infection.
We next used inhibitors of particular steps in the viral life cycle to show that the pseudotyped multicycle replication assay accurately mimics the responses that should occur in a live virus infection (Fig. 2). For example (Fig. 2a), we found that a soluble form of EFNB2 inhibits HeV infection but does not inhibit infection with control VSV pseudotyped virus. In Fig. 2b, several different protease inhibitors were tested for the inhibition of multicycle replication. While these inhibitors should not inhibit entry, they should interfere with F protein processing. The pseudotyped viruses exiting infected cells bearing an uncleaved F protein would not be infectious and could not undergo multicycle replication. Protease inhibitors specific for cathepsin L (15) effectively blocked multicycle replication as predicted based on previous data (4), while chymostatin, which inhibits cathepsin A, B, and C but not cathepsin L, did not. Finally, Fig. 2c shows that anti-HeV G/F antibodies, which interfere with receptor binding, are highly effective at blocking infection. These experiments validated the utility of the pseudotyped virus assay for detecting various classes of entry inhibitors as well as inhibitors of F processing.
FIG. 2.
Multicycle replication assay demonstrates competitive inhibition by soluble receptor, interference with glycoprotein processing, and antibody neutralization. (a) Quantitative inhibition of infection by soluble receptor EFNB2. (b) Molecules that interfere with the protease processing of F block HeV G/F multicycle replication. Lactacystin, MG 132, E64D, or a cathepsin A, B, and C inhibitor (chymostatin) were tested for their ability to inhibit multicycle replication. (c) Neutralizing antibodies block entry and HeV G/F multicycle replication.
HTS screening of a small compound library identifies known and unknown inhibitors.
For the HTS of the compound libraries, cell monolayers transfected with viral glycoproteins (G/F) in 384-well plates were incubated with pseudotyped virus and compounds. As a positive control for inhibitory effect, we used an inhibitory peptide corresponding to the HRC domain of the F protein of human paramyxovirus type 3 (HPIV3), which we have shown inhibits HeV and NiV entry at nanomolar concentrations (19, 20) (Fig. 3). To address the issue of compound-mediated cytotoxicity, we introduced a dual-reporter system that combines the RFP-based fluorescence assessment of infection with a YFP-based assessment of cell viability. If compounds specifically inhibit virus replication, RFP production is reduced but YFP production is unchanged. Only compounds that affect red but not yellow fluorescence are considered to possess specific antiviral activity, and a calculation of the red-to-yellow fluorescence value identifies potential antiviral compounds that minimally reduce cell viability.
FIG. 3.
Adaptation of screening assay to HTS-amenable format. We compared inhibition by an HPIV3 peptide (HRC 36aa) in two different plate sizes. (a) Inhibition of pseudotyped virus entry by antiviral peptide (concentrations are on the x axis) in 96-well plates; (b) adaptation of the experiment described for panel a to the 384-well HTS format. The 96- and 384-well plates yield similar inhibitory curves.
Four commercially available, chemically diverse compound libraries containing 23,232 compounds were screened at a 10 μM concentration. These libraries include marketed drugs, natural products, and combinatorially elaborated active pharmacophores. The percent inhibition for each microtiter plate was calculated based on a relative 100% inhibition by the HRC inhibitory peptide. Across the entire screen, the average Z′ was 0.63 with a standard deviation of 0.11 (n = 65), suggesting excellent reproducibility.
Figure 4a shows the distribution of compound activities and demonstrates how the final hits were chosen and how chloroquine was identified. After the initial screen, 184 compounds that showed no cytotoxicity and greater than 50% inhibition were confirmed by dose-response experiments and assessed for specificity using VSV with its native glycoprotein (VSV-G). Of these, 53 compounds failed to inhibit VSV-G and showed a good dose-response relationship for the inhibition of the HeV pseudotypes (R2 = 0.6 or better). The IC50 of these ranged from 1.3 to 14 μM. Many of these compounds were partial inhibitors, inhibiting viral infection by less than 70% of the control peptide's activity, but 12 caused complete inhibition, with IC50s of less than 6 μM (see Table S1 in the supplemental material). Among these 12 compounds, three were triazines and three others were similar compounds, including the antimalarial drugs chloroquine and quinacrine and the antihistamine clemastine (Fig. 4a). In Fig. 4b, we show an example of the high-throughput dose-response curves used to confirm the activity of chloroquine and clemastine.
FIG. 4.
HTS screening of a small compound library. (a) Selection of chloroquine and similar compounds from HTS. The 23,232 screened compounds showed a distribution of in vitro anti-infective activities. A total of 3,365 of these gave 50% inhibition or more at 10 μM, of which 185 showed 90% retention of YFP expression, which was used as a cytotoxicity marker. Twelve compounds demonstrated reproducible concentration-dependent responses and the complete inhibition of HeV infectivity at 20 μM, of which three were related to chloroquine and clemastine. These three molecules all share structural features, including an aryl chlorine and a tertiary amine tethered together by an aliphatic chain. The library then was searched for chloroquine analogs, and a modified chlorostyryl-quinazoline diethylpentane diamine analog of chloroquine (CSDD) that had missed the cutoff criteria was identified. This compound showed a 75% inhibition of viral entry in the primary screen but was not pursued because it was cytotoxic, inhibiting the YFP signal by 30% at 10 μM. (b) Concentration-response curves for two inhibitory compounds identified in the HTS screen compared to results for a control peptide inhibitor.
Chloroquine: a well-known compound with new potential antiviral mechanism and utility.
Based on the safety profile and its established clinical use at the dosage and plasma concentrations shown to have in vitro antiviral potency against HeV, we focused the rest of our studies on chloroquine. The identification of chloroquine was especially intriguing in light of the mechanism of henipavirus fusion protein processing. Chloroquine concentrations greater than 1 μM entirely abolished F protein processing (16), leading to the conclusion that the cathepsin protease critical for the proteolytic processing of F protein is highly sensitive to changes in pH. However, it also has been shown that cathepsin L may be present in subcellular locations other than the endosome; that the enzyme can function at neutral pH; and that the inhibitory effect of chloroquine on cathepsin L is not solely attributable to its effect on pH but may involve a specific function outside the endocytic compartment (6). In fact, chloroquine, in contrast to concanamycin A and bafilomycin, was shown to inhibit the cathepsin L-mediated processing of the CDP/Cux transcription factor at neutral pH, raising the possibility that chloroquine directly inhibits the enzyme (6).
To analyze the mechanism of chloroquine's effects on henipavirus infection, we tested its inhibitory activity using the multicycle replication assay (Fig. 5). Increasing concentrations of chloroquine resulted in decreased RFP production, indicating reduced viral spread. In contrast, chloroquine did not inhibit the viral spread of NDV-B1-GFP, which does not require cathepsin L for infectivity. The addition of the inhibitory HRC peptide, which blocks virus entry, abolished RFP production, implying that inhibition by chloroquine occurs after the entry step and reduces spread rather than virus entry. The effects of chloroquine on live HeV and NiV were tested and compared to results for inhibition by ribavirin (Fig. 6), which is a nucleoside analog inhibitor of genome replication (1). The IC50s for the chloroquine inhibition of live HeV and NiV infection were 2.5 μM. Both chloroquine (10 μM shown) and ribavirin (100 μM shown) drastically reduced the titer of live HeV and NiV; however, ribavirin also prevented viral genome synthesis, which is consistent with its mechanism of action at the step of RNA replication. In contrast, chloroquine treatment did not inhibit viral genome synthesis, but it did reduce the amount of infectious virus released, which is consistent with the hypothesized mechanism of viral inactivation by chloroquine.
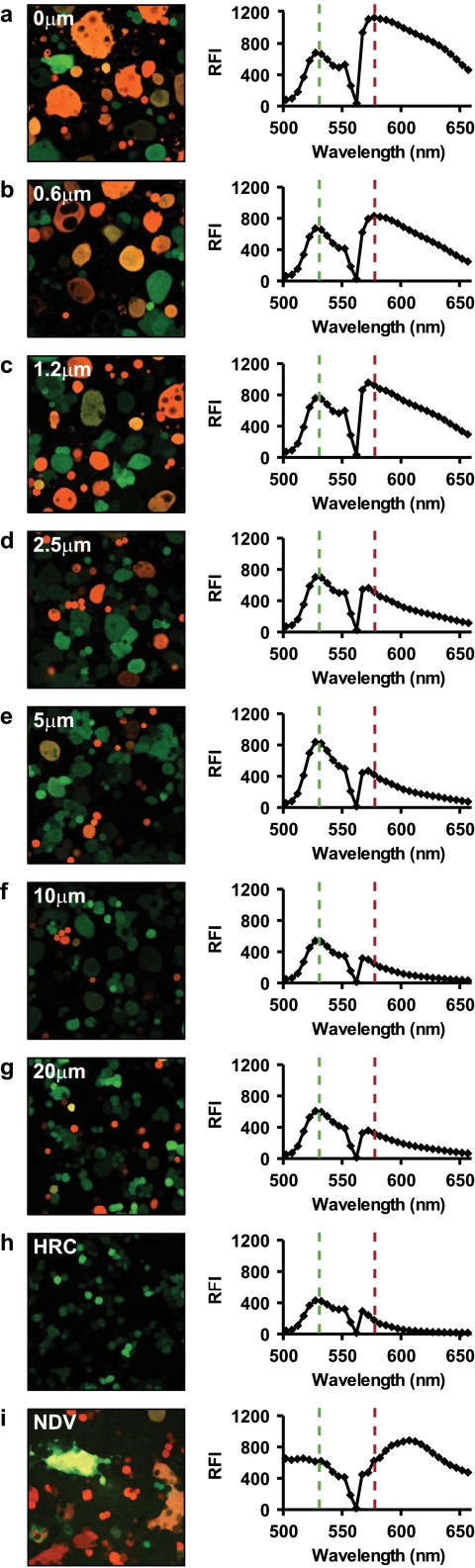
FIG. 5.
Identification of chloroquine validates the utility of HTS assay and suggests a promising antiviral for henipaviruses. Shown is the inhibition of multicycle replication and fusion by chloroquine (at concentrations from 0.6 to 20 μM) and relevant controls. Cells coexpressing HeV G/F and Venus-YFP or NDV AV-F and Cherry-RFP were infected with pseudotyped VSV-ΔG-RFP-HeV F/G or with NDV-B1-GFP, respectively (21). At the time of infection, the cells were treated with the indicated concentrations of chloroquine (a to g and i) or inhibitory peptide (h). Forty-eight hours later the relative fluorescence intensities (RFU) were determined, and the spectral emission from the cells was quantitated and converted into photographs. For each chloroquine treatment, the image on the left shows YFP-labeled cells. The graph on the right of each image shows spectral emission data quantitating the levels of green fluorescence (cell viability) and red fluorescence (infection) for that image. For cells coexpressing HeV G/F (a to h), green and red dotted lines mark the YFP emission peak (a marker for live transfected cells) and the RFP emission peak (indicating infection), respectively. As the concentration of chloroquine increases, the level of green fluorescence (cell viability) remains constant, while the level of red fluorescence (infection) decreases. The cell images on the left show that syncytium area and infection decrease as well. For the HRC peptide positive control (h), cells coexpressing HeV G/F were infected as described above in the presence of 5 μM inhibitory peptide. The image and graph indicate complete inhibition. For the NDV negative control (i), cells expressing NDV AV-F were infected with NDV-B1-GFP in the presence of 20 μM chloroquine (maximal treatment). The cotransfection of WT NDV F serves to complement the cleavage site mutant F in NDV-B1-GFP, allowing multicycle replication and fusion. For the NDV image and graph, GFP (the green dotted line in the graph) indicates infection, while RFP (the red line) is the marker for live transfected cells. The image and spectral emission data show a high level of infection in the presence of chloroquine.
FIG. 6.
Chloroquine is effective against live viruses. Shown is the inhibition of live HeV and NiV infection by chloroquine. Vero cell monolayers were infected with 1,000 50% tissue culture infective doses of HeV or NiV in the presence of 10 μM chloroquine or 100 μM ribavirin. The infectious viral titer of the culture medium was determined, and the cells were lysed to determine viral N gene levels as an indication of genome replication.
DISCUSSION
The screening of a small-compound library using a new HeV/NiV pseudotyped virus assay that simulates multicycle replication identified several effective molecules, including chloroquine, as highly active inhibitors. The identification of a compound that inhibits a known cellular target important for viral maturation, but that had not previously been shown to have antiviral activity for henipaviruses, highlights the validity of the new screening assay. Given the established safety profile and broad experience with chloroquine in humans (23), the results described here provide an option for treating individuals infected with these virulent viruses.
We propose that chloroquine acts by preventing the proteolytic cleavage of HeV and NiV F, likely by inhibiting cathepsin L, either directly or via an effect on endosomal pH. Without this processing step, virions are not infectious (4, 26). Other emerging pathogens, including Ebola virus (10, 24) and severe acute respiratory syndrome virus (SARS) (27), also require cathepsin L cleavage for virion infectivity, and the inhibition of this enzyme has been proposed as a potential antiviral strategy. Chloroquine was shown to inhibit SARS infection in vitro; however, the antiviral effect in those experiments was not attributed to an alteration in viral glycoprotein processing (29). It should be noted that while chloroquine was an effective inhibitor of human immunodeficiency virus (HIV) in vitro, it has shown fairly limited clinical utility (18), ostensibly because the proposed mechanism of action is different for HIV (e.g., the alteration of the glycosylation pattern of gp120) (23) than the proposed inhibition of cathepsin L for HeV and NiV. Additionally, cathepsin L is not required for HIV fusion glycoprotein processing (23).
The multicycle pseudotyped virus HTS assay was highly reproducible and served as a suitable surrogate for HTS assays using live virus, which normally require high-level biocontainment. The fact that a well-known compound (chloroquine) was identified from the screen as a potent inhibitor of HeV and NiV viral spread points to the validity of this unbiased approach. The proposed mechanism of action, the inhibition of a cellular enzyme required for virus infectivity, has the added advantage of being unlikely to elicit resistance, since the drug targets a host rather than a viral enzyme. An approved antipsychotic drug, chlorpromazine, which alters the proteolytic processing of F and was found by Maisner et al. to decrease the titer of live NiV (4) also was identified as inhibitory in our HTS screen. However, because chlorpromazine showed cytopathicity at the effective concentrations, we did not pursue it as a potential antiviral. Several other effective compounds that act via unidentified mechanisms emerged during the study, suggesting that this assay can identify novel viral and cellular targets for anti-infectives. Of note, this method also is valid for the assessment of anti-HeV/NiV neutralizing antibodies for either diagnosis or immunoprophylaxis. The assay strategy for antiviral molecules is widely applicable to other enveloped viruses and may be readily translated for use in screening for molecules to inhibit newly emerging viral pathogens.
While we show that ribavirin (at 100 μM) also drastically reduced the titer of live HeV and NiV in vitro, the distinct mechanisms of action of these compounds are of key importance. Ribavirin, acting at the level of RNA replication, prevented viral genome synthesis; however, chloroquine treatment reduced the amount of infectious virus released without inhibiting viral genome synthesis. Of note, the IC50 of chloroquine for live HeV and NiV is the same as that found using the pseudotyped virus assay and is in the clinically relevant range for patients receiving antimalarial therapy. Chloroquine inhibited infection with live HeV and NiV at a concentration of 1 μM in vitro (IC50 = 2 μM), which is lower than the plasma concentrations present in humans receiving chloroquine treatment for malaria (1.6 to 12.5 μM) (23).
Recent NiV outbreaks with human-to-human transmission (2, 5) have focused attention on NiV as a global health concern. During the summer of 2008, a veterinarian caring for an HeV-infected horse was infected and succumbed to HeV disease, despite state-of-the-art medical care. This case highlights the need for specific therapies for both HeV and NiV. We are concurrently developing antihenipavirus strategies that are based on inhibitory peptides as well as passive immunoprophylaxis; however, the fact that chloroquine is safe and widely used in humans bypasses many of the barriers normally associated with drug development. Given the continual reemergence of NiV in Bangladesh and HeV in Australia, the high fatality rates associated with these infections, and the complete lack of effective antiviral therapy, this report provides a feasible strategy that may allow the rapid identification of antivirals that could significantly contribute to the management of these lethal zoonotic pathogens.
Supplementary Material
Acknowledgments
This work was supported by NIH (NIAID) Northeast Center of Excellence for Bio-defense and Emerging Infections Disease Research grant no. U54AI057158, Developmental and Innovation Research grants to A.M. (PI of Center of Excellence grant: W. I. Lipkin), and NIH (NIAID) grant no. R56AI076335 to A.M. We are grateful to Ashton Kutcher, Jonathan Ledecky, and Nikon, Inc., for the support of our microscopy, to Dan and Nancy Paduano for the support of innovative research projects, and to the Friedman Family Foundation for the renovation of our laboratories at Weill Cornell Medical College.
We acknowledge the Northeast Center of Excellence for Bio-defense and Emerging Infections Disease Research's Proteomics Core for peptide synthesis and purification.
We thank Paolo Carta for technical support, and we acknowledge assistance with flow cytometry from Stanka Semova and Sergei Rudchenko in the Flow Cytometry Facility of the Hospital for Special Surgery/Weill Cornell Medical College.
Footnotes
Published ahead of print on 4 March 2009.
Supplemental material for this article may be found at http://jvi.asm.org/.
REFERENCES
- 1.Aljofan, M., M. Porotto, A. Moscona, and B. A. Mungall. 2008. Development and validation of a chemiluminescent immunodetection assay amenable to high throughput screening of antiviral drugs for Nipah and Hendra virus. J. Virol. Methods 14912-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Butler, D. 2004. Fatal fruit bat virus sparks epidemics in southern Asia. Nature 4297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chua, K. B., W. J. Bellini, P. A. Rota, B. H. Harcourt, A. Tamin, S. K. Lam, T. G. Ksiazek, P. E. Rollin, S. R. Zaki, W. Shieh, C. S. Goldsmith, D. J. Gubler, J. T. Roehrig, B. Eaton, A. R. Gould, J. Olson, H. Field, P. Daniels, A. E. Ling, C. J. Peters, L. J. Anderson, and B. W. Mahy. 2000. Nipah virus: a recently emergent deadly paramyxovirus. Science 2881432-1435. [DOI] [PubMed] [Google Scholar]
- 4.Diederich, S., L. Thiel, and A. Maisner. 2008. Role of endocytosis and cathepsin-mediated activation in Nipah virus entry. Virology 375391-400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Enserink, M. 2004. Emerging infectious diseases. Nipah virus (or a cousin) strikes again. Science 3031121. [DOI] [PubMed] [Google Scholar]
- 6.Goulet, B., A. Baruch, N. S. Moon, M. Poirier, L. L. Sansregret, A. Erickson, M. Bogyo, and A. Nepveu. 2004. A cathepsin L isoform that is devoid of a signal peptide localizes to the nucleus in S phase and processes the CDP/Cux transcription factor. Mol. Cell 14207-219. [DOI] [PubMed] [Google Scholar]
- 7.Harcourt, B. H., A. Tamin, T. G. Ksiazek, P. E. Rollin, L. J. Anderson, W. J. Bellini, and P. A. Rota. 2000. Molecular characterization of Nipah virus, a newly emergent paramyxovirus. Virology 271334-349. [DOI] [PubMed] [Google Scholar]
- 8.Hossain, M. J., E. S. Gurley, J. M. Montgomery, M. Bell, D. S. Carroll, V. P. Hsu, P. Formenty, A. Croisier, E. Bertherat, M. A. Faiz, A. K. Azad, R. Islam, M. A. Molla, T. G. Ksiazek, P. A. Rota, J. A. Comer, P. E. Rollin, S. P. Luby, and R. F. Breiman. 2008. Clinical presentation of nipah virus infection in Bangladesh. Clin. Infect. Dis. 46977-984. [DOI] [PubMed] [Google Scholar]
- 9.Inglese, J., R. L. Johnson, A. Simeonov, M. Xia, W. Zheng, C. P. Austin, and D. S. Auld. 2007. High-throughput screening assays for the identification of chemical probes. Nat. Chem. Biol. 3466-479. [DOI] [PubMed] [Google Scholar]
- 10.Kawaoka, Y. 2005. How Ebola virus infects cells. N. Engl. J. Med. 3522645-2646. [DOI] [PubMed] [Google Scholar]
- 11.Lee, B. 2007. Envelope-receptor interactions in Nipah virus pathobiology. Ann. N. Y. Acad. Sci. 110251-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murray, K., P. Selleck, P. Hooper, A. Hyatt, A. Gould, L. Gleeson, H. Westbury, L. Hiley, L. Selvey, B. Rodwell, et al. 1995. A morbillivirus that caused fatal disease in horses and humans. Science 26894-97. [DOI] [PubMed] [Google Scholar]
- 13.O'Sullivan, J. D., A. M. Allworth, D. L. Paterson, T. M. Snow, R. Boots, L. J. Gleeson, A. R. Gould, A. D. Hyatt, and J. Bradfield. 1997. Fatal encephalitis due to novel paramyxovirus transmitted from horses. Lancet 34993-95. [DOI] [PubMed] [Google Scholar]
- 14.Pager, C. T., W. W. Craft, Jr., J. Patch, and R. E. Dutch. 2006. A mature and fusogenic form of the Nipah virus fusion protein requires proteolytic processing by cathepsin L. Virology 346251-257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pager, C. T., and R. E. Dutch. 2005. Cathepsin L is involved in proteolytic processing of the Hendra virus fusion protein. J. Virol. 7912714-12720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pager, C. T., M. A. Wurth, and R. E. Dutch. 2004. Subcellular localization and calcium and pH requirements for proteolytic processing of the Hendra virus fusion protein. J. Virol. 789154-9163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Park, M. S., M. L. Shaw, J. Munoz-Jordan, J. F. Cros, T. Nakaya, N. Bouvier, P. Palese, A. Garcia-Sastre, and C. F. Basler. 2003. Newcastle disease virus (NDV)-based assay demonstrates interferon-antagonist activity for the NDV V protein and the Nipah virus V, W, and C proteins. J. Virol. 771501-1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paton, N. I., J. Aboulhab, and F. Karim. 2002. Hydroxychloroquine, hydroxycarbamide, and didanosine as economic treatment for HIV-1. Lancet 3591667-1668. [DOI] [PubMed] [Google Scholar]
- 19.Porotto, M., P. Carta, Y. Deng, G. Kellogg, M. Whitt, M. Lu, B. Mungall, and A. Moscona. 2007. Molecular determinants of antiviral potency of paramyxovirus entry inhibitors. J. Virol. 8110567-10574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Porotto, M., L. Doctor, P. Carta, M. Fornabaio, O. Greengard, G. Kellogg, and A. Moscona. 2006. Inhibition of Hendra virus membrane fusion. J. Virol. 809837-9849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Porotto, M., M. Murrell, O. Greengard, M. Lawrence, J. McKimm-Breschkin, and A. Moscona. 2004. Inhibition of parainfluenza type 3 and Newcastle disease virus hemagglutinin-neuraminidase receptor binding: Effect of receptor avidity and steric hindrance at the inhibitor binding sites. J. Virol. 7813911-13919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Porotto, M., M. Murrell, O. Greengard, and A. Moscona. 2003. Triggering of human parainfluenza virus 3 fusion protein(F) by the hemagglutinin-neuraminidase (HN): an HN mutation diminishing the rate of F activation and fusion. J. Virol. 773647-3654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rolain, J. M., P. Colson, and D. Raoult. 2007. Recycling of chloroquine and its hydroxyl analogue to face bacterial, fungal and viral infections in the 21st century. Int. J. Antimicrob. Agents 30297-308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schornberg, K., S. Matsuyama, K. Kabsch, S. Delos, A. Bouton, and J. White. 2006. Role of endosomal cathepsins in entry mediated by the Ebola virus glycoprotein. J. Virol. 804174-4178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sejvar, J. J., J. Hossain, S. K. Saha, E. S. Gurley, S. Banu, J. D. Hamadani, M. A. Faiz, F. M. Siddiqui, Q. D. Mohammad, A. H. Mollah, R. Uddin, R. Alam, R. Rahman, C. T. Tan, W. Bellini, P. Rota, R. F. Breiman, and S. P. Luby. 2007. Long-term neurological and functional outcome in Nipah virus infection. Ann. Neurol. 62235-242. [DOI] [PubMed] [Google Scholar]
- 26.Shiryaev, S. A., A. G. Remacle, B. I. Ratnikov, N. A. Nelson, A. Y. Savinov, G. Wei, M. Bottini, M. F. Rega, A. Parent, R. Desjardins, M. Fugere, R. Day, M. Sabet, M. Pellecchia, R. C. Liddington, J. W. Smith, T. Mustelin, D. G. Guiney, M. Lebl, and A. Y. Strongin. 2007. Targeting host cell furin proprotein convertases as a therapeutic strategy against bacterial toxins and viral pathogens. J. Biol. Chem. 28220847-20853. [DOI] [PubMed] [Google Scholar]
- 27.Simmons, G., A. J. Rennekamp, and P. Bates. 2006. Proteolysis of SARS-associated coronavirus spike glycoprotein. Adv. Exp. Med. Biol. 581235-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Takada, A., C. Robison, H. Goto, A. Sanchez, K. G. Murti, M. A. Whitt, and Y. Kawaoka. 1997. A system for functional analysis of Ebola virus glycoprotein. Proc. Natl. Acad. Sci. USA 9414764-14769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vincent, M. J., E. Bergeron, S. Benjannet, B. R. Erickson, P. E. Rollin, T. G. Ksiazek, N. G. Seidah, and S. T. Nichol. 2005. Chloroquine is a potent inhibitor of SARS coronavirus infection and spread. Virol. J. 269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang, L., B. H. Harcourt, M. Yu, A. Tamin, P. A. Rota, W. J. Bellini, and B. T. Eaton. 2001. Molecular biology of Hendra and Nipah viruses. Microbes Infect. 3279-287. [DOI] [PubMed] [Google Scholar]
- 31.Yonezawa, A., M. Cavrois, and W. C. Greene. 2005. Studies of Ebola virus glycoprotein-mediated entry and fusion by using pseudotyped human immunodeficiency virus type 1 virions: involvement of cytoskeletal proteins and enhancement by tumor necrosis factor alpha. J. Virol. 79918-926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang, J. H., T. D. Chung, and K. R. Oldenburg. 1999. A simple statistical parameter for use in evaluation and validation of high throughput screening assays. J. Biomol. Screen. 467-73. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.