Abstract
Objective
This study is a retrospective clinical study over more than 4 years of follow up to understand the mechanism of load sharing across the graft-bone interface in the static locking plate (SLP) fixation compared with non-locking plate (NLP).
Methods
Orion locking plates and Top non-locking plates were used for SLP fixation in 29 patients and NLP fixation in 24 patients, respectively. Successful interbody fusion was estimated by dynamic X-ray films. The checking parameters were as follows : screw angle (SA) between upper and lower screw, anterior and posterior height of fusion segment between upper and lower endplate (AH & PH), and upper and lower distance from vertebral endplate to the end of plate (UD & LD). Each follow-up value of AH and PH were compared to initial values. Contributions of upper and lower collapse to whole segment collapse were estimated.
Results
Successful intervertebral bone fusion rate was 100% in the SLP group and 92% in the NLP group. The follow-up mean value of SA in SLP group was not significantly changed compared with initial value, but follow-up mean value of SA in NLP group decreased more than those in SLP group (p=0.0067). Statistical analysis did not show a significant difference in the change in AH and PH between SLP and NLP groups (p>0.05). Follow-up AH of NLP group showed more collapse than PH of same group (p=0.04). The upper portion of the vertebral body collapsed more than the lower portion in the SLP fixation (p=0.00058).
Conclusion
The fused segments with SLP had successful bone fusion without change in initial screw angle, which was not observed in NLP fixation. It suggests that there was enough load sharing across bone-graft interface in SLP fixation.
Keywords: Cervical vertebrae, Spinal fusion, Surgical Fixation Devices
INTRODUCTION
Plate fixation combined with anterior cervical interbody fusion is a popular procedure to enhance immediate spinal stability after surgery and improve bone fusion rate. Anterior cervical plates can be classified as locking plates with static screw system (SLP) and non-locking plates (NLP) according to the presence of a lock screw system4,5,30,31). SLPs are known to have the advantages of stiff fixation, high fusion rate, and low instrument-related complication rate13,14,22,31). There is growing concern over the negative effects of the highly rigid fixation system of SLPs, which might result in decreased load sharing across the graft-bone interface and leads to reduced fusion rates. Biomechanical results of decreased load sharing in rigid screws of SLPs have led to the introduction of various dynamic cervical plates to accommodate the axial shortening of the graft1,3,4,11,28).
In spite of the negative effects of rigid fixation of SLPs, many studies reported SLP fixation achieved high cervical interbody fusion rates without specific instrument-related complications12-14,17,18,20,22,33). Furthermore, recent clinical studies reported that the fusion rate of SLPs was similar to or even higher than dynamic plates8,29). DuBois et al.8) reported that a higher rate of nonunion was actually seen in the dynamically plated patients compared to the SLPs. From these results, the authors thought that the decreased load sharing of SLPs in biomechanical tests cannot be applied to real clinical situations since the process of long-term adaptation in the human body is quite different from a biomechanical test carried out immediately after screw fixation.
This clinical study was conducted retrospectively to identify a real mechanism of axial load sharing of SLPs by observing changes at the site of anterior interbody fusion with plate fixation over more than 4 years. To evaluate and highlight the unique mechanism of SLPs, all data were compared to those obtained from NLPs.
MATERIALS AND METHODS
Patients
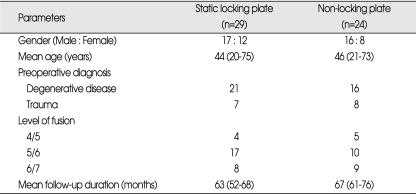
This study is based on a retrospective review of patients who had undergone anterior cervical interbody fusion and plate fixation between January 1999 and December 2002. Two types of cervical plates were used : Orion plate (Medtronic Sofamor Danek, Memphis, Tennessee, USA) and Top plate (Top Surgical Products, Karlstein, Germany) for SLP and NLP fixation, respectively. Of the 53 patients who had undergone anterior cervical plate fixation, Orion plates were used in 29 and Top plates in 24. In the SLP group (male : female=17 : 12) with mean age of 44 years (20-75 years), preoperative diagnoses were 22 for degenerative diseases and 7 for traumas. In the NLP group (male : female=16 : 8) with mean age of 46 years (21-73 years), preoperative diagnoses were 16 for degenerative diseases and 8 for traumas. We included mild subluxation trauma cases because the main objective of this study was to see the axial load transmission across the graft-bone interface. The average follow-up duration was 63 months (52-68 months) and 67 months (61-76 months) for the SLP and NLP groups, respectively (Table 1). Patients were allocated to each plate by random selection. There was no statistical difference in age and gender between the 2 groups (p>0.05).
Table 1.
Demographic and clinical characteristics of the patients
Surgical procedures
All surgical procedures were performed by the same surgeon. During surgery, patients were placed in the supine position under general anesthesia. Anterior cervical discectomy was performed using a routine Smith-Robinson technique for neural decompression. The major concern was the complete removal of the intervertebral disc and cartilaginous endplate using a high-speed drill and curettes. All patients underwent autologous tricortical iliac bone graft, which was harvested from the anterior iliac crest. Anterior cervical plates were placed after insertion of the iliac bone graft into the prepared intervertebral space and fixed by unicortical purchase using screws of 14 mm in length in both types of plates. Philadelphia neck collar was recommended to use for 1 month after surgery.
Evaluation of successful bone fusion
An interbody bone fusion was estimated by plain cervical X-ray film with anterior-posterior and lateral flexion-extension views. The presence of mature bridging bony trabeculae between vertebrae without a lucent gap and any movement at the fused segment on flexion and extension dynamic views was accepted as a successful fusion.
Radiological parameters
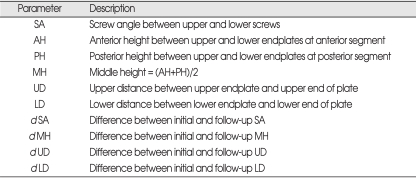
Radiological changes in the cervical spine were estimated using plain lateral X-ray film and compared to images taken immediately after surgery. For measuring the radiological parameters, we used quantitative measurement analysis software in a picture archiving and communication system workstation (Centricity 3.0, General Electrics Medical Systems, Milwaukee, WI, USA). The checking parameters using X-ray film were as follows : SA, AH & PH, and UD & LD (Table 2, Fig. 1).
Table 2.
Description of radiological parameters
Fig. 1.
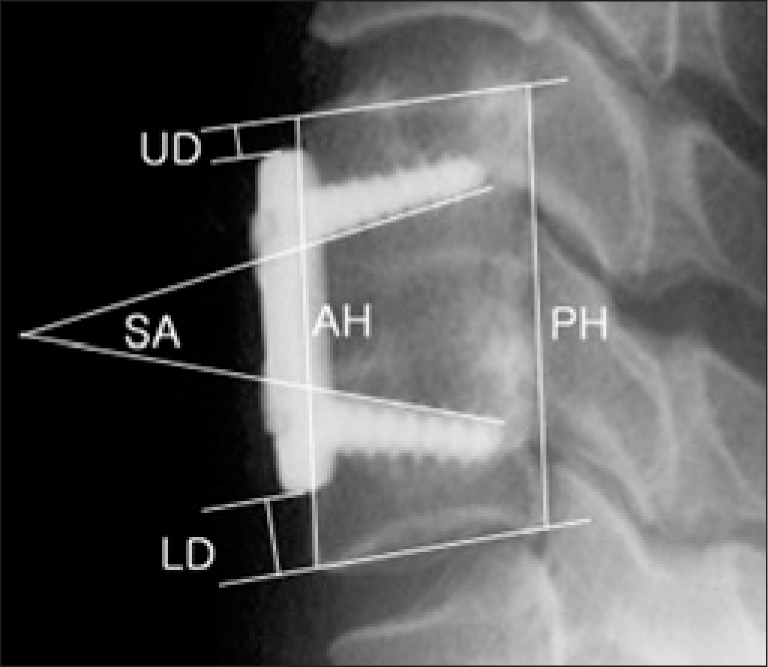
Radiological parameters on cervical lateral X-ray film to evaluate changes at the site of interbody bone fusion with anterior cervical plate fixation. ACD & PCD : anterior and posterior cortical distance between upper and lower endplate, SA : Screw angle between upper and lower screws, UD & LD : distance from upper and lower vertebral endplate to the plate.
SA was measured to see the ability to preserve initial fixation status of screws. The difference between initial and follow-up SA was defined as dSA. AH and PH were measured to detect the collapse at the anterior and posterior portions of fusion segments. Middle height (MH) of fusion segment was calculated to estimate average collapse of fusion segment : (AH+PH)/2. Each follow-up value of AH, PH, and MH was compared to initial value and described as a relative percentage (%) : follow-up value/initial value×100.
UD and LD were checked to detect the collapse at the upper and lower portions of fusion segment. The dUD, dLD and dMH were defined as the difference between initial and follow-up measurements. The percentage contribution of upper and lower portions to whole fusion segment collapse was calculated by dUD/dMH×100 and dLD/dMH×100, respectively.
Statistical analysis
We used SAS software for Windows (SAS version 9.1, SAS Institute Inc., Cary, NC, USA). Radiological parameters (SA, AH, MH, PH, UD, LD) were tested with Fishers' exact test. To compare fusion rates from the fused and nonfused groups, Student's 2-tailed t-test was used. Continuous variables (age and gender) of two groups were compared using Wilcoxon signed rank test. A p-value less than 0.05 was considered to be statistically significant.
RESULTS
Bone fusion rate and complication
The successful intervertebral bone fusion rate was 100% in the SLP group and 92% in the NLP group. There was no statistical difference between the fusion rates of two groups (p>0.05). Two patients with NLPs showed collapsed grafts with radiolucent gap in the intervertebral space. No instrument failure such as instrument breakage or screw loosening in both types of plates was found. A postoperative transient wound hematoma occurred in 1 patient after SLP fixation, which was managed by hema-toma evacuation without sequelae.
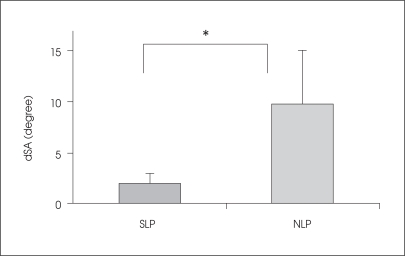
Changes in screw angle
Initial SA immediately after surgery was 32±7.6° for SLPs and 20±4.0° for NLPs. At the time of follow up, SA was 30±6.3° for SLPs and 11±7.9° for NLPs. As a result, dSA was 1.9±0.9° in SLPs and 9.8±5.3° in NLPs (Figs. 2, 3, 4). The comparison of dSA between the two groups showed significant differences (p=0.0067).
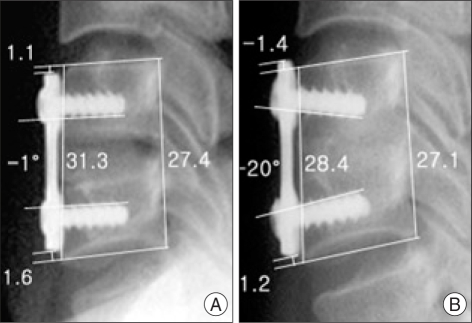
Fig. 2.
Cervical lateral X-ray images of static locking plate (Orion plate) fixation taken immediately (A) and 61 months (B) after surgery. Migration of screws inside the vertebral body with graft collapse is noticed with a minimal change in screw angle. Upper screws migrated more than lower screws.
Fig. 3.
Cervical lateral X-ray images of non-locking plate (Top plate) fixation taken immediately (A) and 65 months (B) after surgery. Breakage of screw angle at the plate-screw junction with graft collapse is noticed. Anterior part of fusion segment collapsed more than posterior part.
Fig. 4.
Difference between initial and follow-up screw angle. Screw angle of static locking plate showed little change, whereas screw angle of non-locking plate significantly changed at the follow-up (p=0.0067). *p<0.05. NLP : non-locking plate, SA : screw angle, SLP : static locking plate.
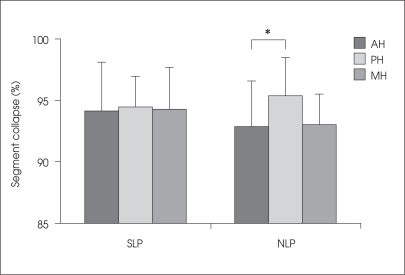
Changes in fused segment height
In the SLP group, follow-up AH, MH and PH were 94.1±3.9%, 94.2±3.4% and 94.4±2.4% of initial measurements, respectively. In the NLP group, follow-up AH, MH and PH were 92.9±3.1%, 93.0±2.5% and 95.4±3.1% of initial measurements, respectively (Figs 2, 3, 5). Statistical analysis showed that AH of NLPs showed significantly more collapse than PH of same group (p=0.04) while SLPs showed evenly decreased fusion height at the anterior and posterior parts. In comparisons of follow-up MH between SLPs and NLPs, there was no significant difference between both groups (p>0.05).
Fig. 5.
Collapsed anterior and posterior heights of fusion segments expressed as percentage to initial measurements. Static locking plate showed evenly decreased fusion height at the anterior and posterior parts, whereas anterior height of non-locking plate showed significantly higher collapse rate than posterior height (p=0.04). *p<0.05.
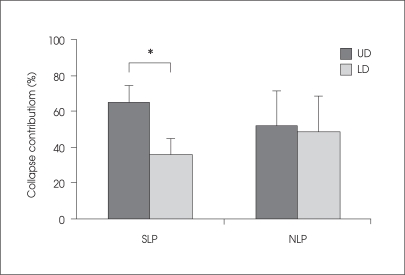
Changes in upper and lower segment
The contribution of the upper and lower portion (dUD/dMH×100 and dLD/dMH×100) to whole fusion segment collapse was 64.9±9.2% and 35.9±8.9% for SLPs and 51.6±20.1% and 48.7±19.8% for NLPs, respectively (Figs. 2, 3, 6). In SLPs, the contribution of the upper portion to whole graft shortening was significantly higher than the lower portion (p=0.00058). However, there was no significant difference between the upper and lower portions in the NLP group.
Fig. 6.
Percentage contribution of upper and lower portion of graft to whole fusion segment collapse. In static locking plate, contribution of the upper portion to whole graft shortening was significantly higher than in the lower portion (p=0.00058). In non-locking plate, the collapse rate was not different between the upper and lower portion of fusion segments. *p<0.05. LD : lower distance between lower endplate and lower end of plate, UD : upper distance between upper endplate and upper end of plate.
DISCUSSION
Anterior plate fixation after cervical discectomy and fusion has gained broad support because of excellent initial stability, increased fusion rates, decreased requirements for external immobilization, and an early return to work1,5,14,21,24). In biomechanical test of cervical plates, SLPs significantly increased the rigidity of the tested screw-plate systems initially and after cyclic loading compared to NLPs31). In clinical areas, SLPs have been used more frequently than NLPs in recent years and they are known to be safe and simple instrumentation with unicortical purchase of screws with high fusion rate, strong stability, and low instrument-related failure rate2,14,20,23,24).
Despite well-known clinical data on SLPs, the concept of decreased load sharing of rigid locking screw system was suggested in biomechanical test, and dynamic plates with semi-rigid variable angle screws or controlled settling system along the graft axis have been introduced to accommodate the shortening of the graft1,3,4,7,11,28). As far as the authors are concerned, there has been no clinical study about decreased load sharing of SLPs, except the biomechanical test. In this study, compared to the NLPs with toggling screws, SLPs allowed sufficient load sharing across the graft-bone interface without any change in initial screw fixation status.
In the biomechanical test by Brodke et al.3), load sharing of Orion locking plates was much lower than dynamic cervical plates. We thought that decreased load sharing in their biomechanical test was correct because load sharing was measured immediately after screw insertion into an artificial plastic vertebral body. However, in real clinical situations, screws are inserted into the vertebral body, which is mainly composed of cancellous bone, and an intravertebral adaptation occurs between the screw and vertebral body accompanied by continuous load sharing across the graft-bone interface in the fusion segment. During adaptation time, screws migrate along the vertical axis inside the vertebral body without breakage of initial screw angle. We call this "intravertebral screw migration". As far as we are aware, there has not been any reports about this concept of load sharing mechanism in SLPs. The authors think that continuous load sharing with progressive vertical migration of screws explains the high fusion rate without instrumental failure in SLPs.
Our study showed that, with regard to graft collapse in middle height, there was no significant difference between SLPs and NLPs. This means that the shortness of a graft occurs in both plate systems at similar collapse rates. However, the mechanism of graft collapse was quite different. In NLPs with toggling screws, the axial load was transmitted through a breakage of initial screw angle at the screw-plate junction. On the contrary, SLPs screws kept their initial status while the intervertebral graft collapsed evenly at the anterior and posterior portions. We think that early breakage of the screw angle in NLPs is a possible cause of more anterior graft collapse than posterior portion, which will result in postoperative segmental kyphosis. In the aspect of the sagittal balance of the vertebral column, the collapse rate at the anterior or posterior fusion segments is important because postoperative kyphotic angulation has adverse effects on clinical outcome15,18,30). This study reveals the possible mechanism of high postoperative segmental kyphosis in NLP fixation compared to SLP as indicated in previous reports19,24,32).
Successful intervertebral bone fusion is closely related to clinical results. The reported fusion rates differ by various methods : 88-92% for interbody fusion without instrumentation, 87-99% for interbody fusion with NLP fixation, and 95-100% for interbody fusion with SLP fixation5,6,10,17,18,25,27,33). In the present study, SLPs showed 100% of interbody fusion rate. We believe that excellent fusion rates of SLPs can also be explained by firmly fixed fusion segments and continuous load sharing.
This study showed 5-6% in graft collapse rate via "intravertebral migration of screws" in SLPs. If fusion levels were more than one, the collapsed portion would be longer with resultant increase in intravertebral screw migration. In such cases, screws may even migrate into the disc space if they are inserted near the adjacent disc space. An inappropriate long plate can result in contact of the plate tip with the disc space, which consequently affects disc degeneration and anterior bony spur formation on the adjacent segment16,26). We suggest that SLP screws with the shortest plate length should be inserted as near to the fusion site as possible.
A contribution of upper or lower fusion segments to the whole collapse is another considerable factor in anterior cervical instrumentation. Studies on adjacent segments after cervical fusion have reported that significant increases in intradiscal pressure and segmental motion occur at levels adjacent to fusion during normal range of motion9,26). Intradiscal pressure and segmental motion were increased more at the upper than lower segment, especially during neck flexion9,26). In our study, the upper fusion segment collapsed more than the lower segment, which may be affected by the greater load on the upper segment with resultant increase in intravertebral screw migration. It suggests that more attention should be paid to upper screw insertion when using SLP in multilevel fusion.
This study has a limitation in the use of plain X-ray films to estimate the morphological changes at fusion segment after plate fixation. For observation of the changes inside the vertebral body during intravertebral screw migration, additional CT scanning would be better. However, this study shows the mechanism how axial load transmits to the interbody graft in anterior cervical fixation using SLP. Concurrent mechanisms of rigid screw fixation and axial load transmission to the graft explain the excellent fusion and low instrumentation failure rates. SLP is still considered a good choice for anterior cervical fixation after interbody fusion according to our results.
CONCLUSION
This study has significance by showing the possible mechanism of load sharing in SLP fixation. SLPs transmitted axial load by the mechanism of intravertebral screw migration without change in initial status of screw fixation, which resulted in successful intervertebral bone fusion. In NLPs, load sharing was achieved through early breakage of screw angle at the screw-plate junction, and anterior part of the graft collapsed more than posterior part. The collapse rate of the fusion segment was not significantly different between SLPs and NLPs.
References
- 1.Balabhadra RS, Kim DH, Zhang HY. Anterior cervical fusion using dense cancellous allografts and dynamic plating. Neurosurgery. 2004;54:1405–1141. doi: 10.1227/01.neu.0000125543.38952.87. discussion 1411-1402. [DOI] [PubMed] [Google Scholar]
- 2.Bolesta MJ, Rechtine GR, 2nd, Chrin AM. One- and two-level anterior cervical discectomy and fusion: the effect of plate fixation. Spine J. 2002;2:197–203. doi: 10.1016/s1529-9430(02)00186-9. [DOI] [PubMed] [Google Scholar]
- 3.Brodke DS, Gollogly S, Alexander Mohr R, Nguyen BK, Dailey AT, Bachus aK. Dynamic cervical plates: biomechanical evaluation of load sharing and stiffness. Spine. 2001;26:1324–1329. doi: 10.1097/00007632-200106150-00010. [DOI] [PubMed] [Google Scholar]
- 4.Brodke DS, Klimo P, Jr, Bachus KN, Braun JT, Dailey AT. Anterior cervical fixation : analysis of load-sharing and stability with use of static and dynamic plates. J Bone Joint Surg Am. 2006;88:1566–1573. doi: 10.2106/JBJS.E.00305. [DOI] [PubMed] [Google Scholar]
- 5.Caspar W, Geisler FH, Pitzen T, Johnson TA. Anterior cervical plate stabilization in one- and two-level degenerative disease: overtreatment or benefit? J Spinal Disord. 1998;11:1–11. [PubMed] [Google Scholar]
- 6.Cauthen JC, Kinard RE, Vogler JB, Jackson DE, DePaz OB, Hunter OL, et al. Outcome analysis of noninstrumented anterior cervical discectomy and interbody fusion in 348 patients. Spine. 1998;23:188–192. doi: 10.1097/00007632-199801150-00008. [DOI] [PubMed] [Google Scholar]
- 7.Chung DY, Cho DC, Lee SH, Sung JK. Preliminary surgical result of cervical spine reconstruction with a dynamic plate and titanium cage. J Korean Neurosurg Soc. 2007;41:111–117. [Google Scholar]
- 8.DuBois CM, Bolt PM, Todd AG, Gupta P, Wetzel FT, Phillips FM. Static versus dynamic plating for multilevel anterior cervical discectomy and fusion. Spine J. 2007;7:188–193. doi: 10.1016/j.spinee.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 9.Eck JC, Humphreys SC, Lim TH, Jeong ST, Kim JG, Hodges SD, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine. 2002;27:2431–2434. doi: 10.1097/00007632-200211150-00003. [DOI] [PubMed] [Google Scholar]
- 10.Emery SE, Fisher JR, Bohlman HH. Three-level anterior cervical discectomy and fusion : radiographic and clinical results. Spine. 1997;22:2622–2624. doi: 10.1097/00007632-199711150-00008. discussion 2625. [DOI] [PubMed] [Google Scholar]
- 11.Epstein NE. The management of one-level anterior cervical corpectomy with fusion using Atlantis hybrid plates: preliminary experience. J Spinal Disord. 2000;13:324–328. doi: 10.1097/00002517-200008000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Geisler FH, Caspar W, Pitzen T, Johnson TA. Reoperation in patients after anterior cervical plate stabilization in degenerative disease. Spine. 1998;23:911–920. doi: 10.1097/00007632-199804150-00013. [DOI] [PubMed] [Google Scholar]
- 13.Grubb MR, Currier BL, Shih JS, Bonin V, Grabowski JJ, Chao EY. Biomechanical evaluation of anterior cervical spine stabilization. Spine. 1998;23:886–892. doi: 10.1097/00007632-199804150-00009. [DOI] [PubMed] [Google Scholar]
- 14.Heidecke V, Rainov NG, Burkert W. Anterior cervical fusion with the Orion locking plate system. Spine. 1998;23:1796–1802. doi: 10.1097/00007632-199808150-00014. discussion 1803. [DOI] [PubMed] [Google Scholar]
- 15.Herrmann AM, Geisler FH. Geometric results of anterior cervical plate stabilization in degenerative disease. Spine. 2004;29:1226–1234. doi: 10.1097/00007632-200406010-00012. [DOI] [PubMed] [Google Scholar]
- 16.Ipsen BJ, Kim DH, Jenis LG, Tromanhauser SG, Banco RJ. Effect of plate position on clinical outcome after anterior cervical spine surgery. Spine J. 2007;7:637–642. doi: 10.1016/j.spinee.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 17.Kaiser MG, Haid RW, Jr, Subach BR, Barnes B, Rodts GE., Jr Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery. 2002;50:229–236. doi: 10.1097/00006123-200202000-00001. discussion 236-238. [DOI] [PubMed] [Google Scholar]
- 18.Katsuura A, Hukuda S, Imanaka T, Miyamoto K, Kanemoto M. Anterior cervical plate used in degenerative disease can maintain cervical lordosis. J Spinal Disord. 1996;9:470–476. [PubMed] [Google Scholar]
- 19.Katsuura A, Hukuda S, Saruhashi Y, Mori K. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J. 2001;10:320–324. doi: 10.1007/s005860000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim KS. Long-term effects on the cervical spine after anterior locking plate fixation. J Korean Neurosurg Soc. 2001;30:493–500. [Google Scholar]
- 21.Lim TH, Kwon H, Jeon CH, Kim JG, Sokolowski M, Natarajan R, et al. Effect of endplate conditions and bone mineral density on the compressive strength of the graft-endplate interface in anterior cervical spine fusion. Spine. 2001;26:951–956. doi: 10.1097/00007632-200104150-00021. [DOI] [PubMed] [Google Scholar]
- 22.Lowery GL, McDonough RF. The significance of hardware failure in anterior cervical plate fixation. Patients with 2- to 7-year follow-up. Spine. 1998;23:181–186. doi: 10.1097/00007632-199801150-00006. discussion 186-187. [DOI] [PubMed] [Google Scholar]
- 23.McLaughlin MR, Purighalla V, Pizzi FJ. Cost advantages of two-level anterior cervical fusion with rigid internal fixation for radiculopathy and degenerative disease. Surg Neurol. 1997;48:560–565. doi: 10.1016/s0090-3019(97)00366-2. [DOI] [PubMed] [Google Scholar]
- 24.Mobbs RJ, Rao P, Chandran NK. Anterior cervical discectomy and fusion: analysis of surgical outcome with and without plating. J Clin Neurosci. 2007;14:639–642. doi: 10.1016/j.jocn.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 25.Paramore CG, Dickman CA, Sonntag VK. Radiographic and clinical follow-up review of Caspar plates in 49 patients. J Neurosurg. 1996;84:957–961. doi: 10.3171/jns.1996.84.6.0957. [DOI] [PubMed] [Google Scholar]
- 26.Park DH, Ramakrishnan P, Cho TH, Lorenz E, Eck JC, Humphreys SC, et al. Effect of lower two-level anterior cervical fusion on the superior adjacent level. J Neurosurg Spine. 2007;7:336–340. doi: 10.3171/SPI-07/09/336. [DOI] [PubMed] [Google Scholar]
- 27.Phillips FM, Carlson G, Emery SE, Bohlman HH. Anterior cervical pseudarthrosis. Natural history and treatment. Spine. 1997;22:1585–1589. doi: 10.1097/00007632-199707150-00012. [DOI] [PubMed] [Google Scholar]
- 28.Reidy D, Finkelstein J, Nagpurkar A, Mousavi P, Whyne C. Cervical spine loading characteristics in a cadaveric C5 corpectomy model using a static and dynamic plate. J Spinal Disord Tech. 2004;17:117–122. doi: 10.1097/00024720-200404000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Saphier PS, Arginteanu MS, Moore FM, Steinberger AA, Camins MB. Stress-shielding compared with load-sharing anterior cervical plate fixation: a clinical and radiographic prospective analysis of 50 patients. J Neurosurg Spine. 2007;6:391–397. doi: 10.3171/spi.2007.6.5.391. [DOI] [PubMed] [Google Scholar]
- 30.Smith SA, Lindsey RW, Doherty BJ, Alexander J, Dickson JH. An in-vitro biomechanical comparison of the Orosco and AO locking plates for anterior cervical spine fixation. J Spinal Disord. 1995;8:220–223. doi: 10.1097/00002517-199506000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Spivak JM, Chen D, Kummer FJ. The effect of locking fixation screws on the stability of anterior cervical plating. Spine. 1999;24:334–338. doi: 10.1097/00007632-199902150-00005. [DOI] [PubMed] [Google Scholar]
- 32.van Limbeek J, Jacobs WC, Anderson PG, Pavlov PW. A systematic literature review to identify the best method for a single level anterior cervical interbody fusion. Eur Spine J. 2000;9:129–136. doi: 10.1007/s005860050223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang JC, McDonough PW, Endow K, Kanim LE, Delamarter RB. The effect of cervical plating on single-level anterior cervical discectomy and fusion. J Spinal Disord. 1999;12:467–471. [PubMed] [Google Scholar]