Abstract
Oculomotor nerve palsy (ONP) with subarachnoid hemorrhage (SAH) occurs usually when oculomotor nerve is compressed by growing or budding of posterior communicating artery (PcoA) aneurysm. Midbrain injury, increased intracranial pressure (ICP), or uncal herniation may also cause it. We report herein a rare case of ONP associated with SAH which was caused by middle cerebral artery (MCA) bifurcation aneurysm rupture. A 58-year-old woman with clear consciousness suffered from headache and sudden onset of unilateral ONP. Computed tomography showed SAH caused by the rupture of MCA aneurysm. The unilateral ONP was not associated with midbrain injury, increased ICP, or uncal herniation. The patient was treated with coil embolization, and the signs of oculomotor nerve palsy completely resolved after a few days. We suggest that bloody jet flow from the rupture of distant aneurysm other than PcoA aneurysm may also be considered as a cause of sudden unilateral ONP in patients with SAH.
Keywords: Oculomotor nerve palsy, Middle cerebral artery aneurysm, Subarachnoid hemorrhage
INTRODUCTION
Unilateral oculomotor nerve palsy (ONP) associated with subarachnoid hemorrhage (SAH) is a clinical manifestation due to direct compression of the internal carotid-posterior communicating artery (IC-PcoA) junction aneurysm5,6). Midbrain injury or uncal herniation associated with increased intracranial pressure (ICP) could also be the causes of ONPs indirectly from the rupture of distant aneurysm other than PcoA aneurysm4).
We report herein a rare case of ONP associated with SAH which was caused by a direct injury by the bloody jet flow from the rupture of middle cerebral artery (MCA) bifurcation aneurysm without usual causes.
CASE REPORT
A 58-year-old woman was admitted to our hospital because of mild headache without any loss of consciousness. There was no history of diabetes mellitus, hypertension, heart disease, stroke, or cancer. On admission, the patient showed no neurological deficits. Computed tomography (CT) revealed only moderate SAH, and left MCA bifurcation aneurysm was found on CT angiography. After a few hours, the patient suddenly complained of ptosis and diplopia. The left pupil was 5 mm in diameter and nonreactive to light. Repeated CT revealed increased SAH on the left sylvian fissure, which was suspected of rebleeding. However, there were no radiological evidence of midbrain injury and uncal herniation on the brain CT scan (Fig. 1). In addition, the patient was alert without any neurological deficit except ONP. Immediately, the patient underwent 4-vessel angiography, and only the left MCA bifurcation aneurysm was found with no other aneurysms elsewhere (Fig. 2). The aneurysm was treated with coil embolization immediately after the 4-vessel angiography (Fig. 3). On the first day after the embolization of the aneurysm, the left pupil became isocoric. The ptosis was partially improved and the diplopia was disappeared on day 3. Magnetic resonance imaging (MRI) on day 3 showed no abnormal lesion in the midbrain or basal cistern (Fig. 4). Although the patient had motor dysphasia due to vasospasm on day 6, the ptosis disappeared completely on day 10. The patient was discharged on day 21 and did not have any neurological deficit during 6-month follow-up.
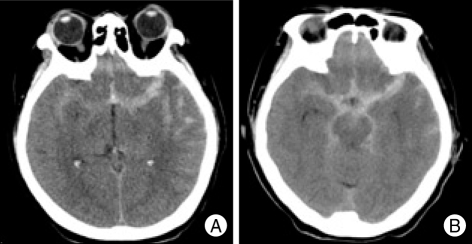
Fig. 1.
Computed tomography (CT) revealed only moderate subarachnoid hemorrhage (A), and repeated CT revealed minimally thicker subarachnoid hemorrhage on the left sylvian fissure and basal cistern (B), suggesting rebleeding. However, there were no evidence of midbrain injury and uncal herniation.
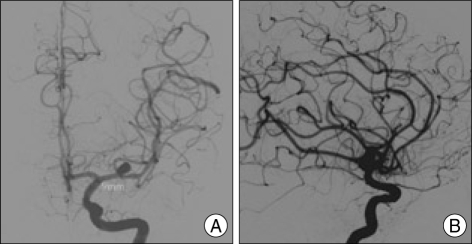
Fig. 2.
4-vessel angiography anterior-posterior view (A) and lateral view (B). Only the left middle cerebral artery bifurcation aneurysm is noted with no other aneurysms elsewhere. There is a short M1 (9 mm from internal carotid artery bifurcation to middle cerebral artery bifurcation), which makes the aneurysm closer to the nerve than normal length of M1.
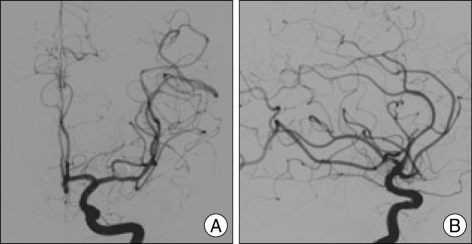
Fig. 3.
The aneurysm was treated with coil embolization anterior-posterior view (A) and lateral view (B).
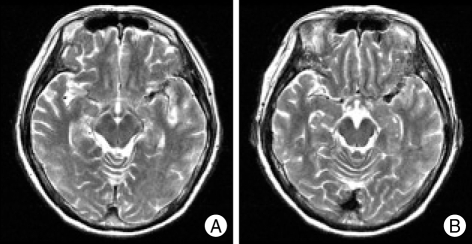
Fig. 4.
Magnetic resonance imaging on Day 3 shows no abnormal lesion in the midbrain or basal cistern.
DISCUSSION
ONP is one of the manifestations of intracranial aneurysms and SAH, and IC-PcoA aneurysm is the most common cause of ONP (34-56%)2,12). However, it is also possible that the rupture of distant aneurysms or anomalous vessel may cause ONP. Aiba and Fukuda1) reported anomaly of basilar arteries, posterior cerebral arteries, and superior cerebellar arteries as well as posterior cerebral artery and superior cerebellar artery inversion might cause ONP.
Fox4) classified the mechanisms of ONP with an intracranial aneurysm : midbrain hemorrhage9), direct local pressure by aneurysms, and hemorrhagic dissection of the nerve were considered as a direct cause, whereas increased ICP (from clot, edema, or hydrocephalus) which results in uncal herniation was classified as an indirect cause.
In the present case, however, it is very unusual because MCA bifurcation aneurysm was not in the vicinity of the oculomotor nerve. It is highly likely the ONP was induced by the bloody jet flow due to rupture of MCA bifurcation aneurysm. Saito et al.10) reported a case of ruptured ICA aneurysm with contralateral ONP and suggested that bloody jet flow from the rupture of distant aneurysm could rarely induce ONP.
In the present study, we speculate possible a mechanism of ONP in our patient as bloody jet flow from the rupture of distant aneurysm. First, initial and repeated CT revealed no evidence of midbrain hemorrhage, basilar artery anomaly, hemorrhagic dissection, and uncal herniation with ICP. MRI also revealed no evidence of abnormality of midbrain and basal cisterns, indicating direct cause of ONP being excluded. Second, the patient had short M1 (9 mm from internal carotid artery bifurcation to middle cerebral artery bifurcation), indicating that the aneurysm was closer to the nerve than normal length of M1 (Fig. 2). Third, the direction of the bloody jet flow from the second rupture (rebleeding) might have been changed inferiorly to the way of the oculomotor nerve beside PcoA because of the superiorly placed blood clot from the previous rupture. Fourth, clinical symptom of the patient was correlated with the extrinsic cause, indicating typical ONP (unilateral pupil dilation, ptosis, and partial extraocular palsies). Considering the location of the aneurysm, the bloody jet flow could have direction on superomedial portion of the nerve, resulting in typical ONP. Kurokawa et al.7) described that the anatomical relationship between the exit of the PcoA and the entry of the oculomotor nerve into the cavernous sinus that would usually result in superomedial compression of the nerve by the aneurysm. Typical ONP in this situation may manifest as unilateral pupil dilation, ptosis, incomplete or partial extraocular palsies, and oculomotor synkinesis. Finally, the ONP of the present case was recovered completely after 10 days, which is quite unusual and not easy to explain. ONP is usually recovered very slowly, ranging from a few weeks to months3,8,11). Chen et al.3) reported that the time to complete resolution of ONP takes about 6 months. Furthermore, early treatment might contribute to early recovery. Indeed, Leivo et al.8) recommended early treatment for aneurysm-induced third nerve palsy, preferably within 3 days, to avoid functionally and cosmetically unwanted disability.
These mechanisms may explain a rare case of ONP associated with SAH which was caused by a direct injury by the bloody jet flow from the rupture of middle cerebral artery (MCA) bifurcation aneurysm.
CONCLUSION
ONP induced by a ruptured MCA aneurysm is very rare, and it would better be kept in mind that the ONP with SAH may occur by the rupture of distant intracranial aneurysms.
References
- 1.Aiba T, Fukuda M. Unilateral oculomotor nerve paresis associated with anterior communicating artery aneurysm rupture. Neurol Med Chir (Tokyo) 2003;43:484–487. doi: 10.2176/nmc.43.484. [DOI] [PubMed] [Google Scholar]
- 2.Arle JE, Abrahams JM, Zager EL, Taylor C, Galetta SL. Pupil-sparing third nerve palsy with preoperative improvement from a posterior communicating artery aneurysm. Surg Neurol. 2002;57:423–426. doi: 10.1016/s0090-3019(02)00717-6. discussion 426-427. [DOI] [PubMed] [Google Scholar]
- 3.Chen PR, Amin-Hanjani S, Albuquerque FC, McDougall C, Zabramski JM, Spetzler RF. Outcome of oculomotor nerve palsy from posterior communicating artery aneurysms : comparison of clipping and coiling. Neurosurgery. 2006;58:1040–1046. doi: 10.1227/01.NEU.0000215853.95187.5E. discussion 1040-1046. [DOI] [PubMed] [Google Scholar]
- 4.Fox JL. Intracranial aneurysms. New York: Springer; 1983. pp. 163–183. [Google Scholar]
- 5.Fujiwara S, Fujii K, Nishio S, Matsushima T, Fukui M. Oculomotor nerve palsy in patients with cerebral aneurysms. Neurosurg Rev. 1989;12:123–132. doi: 10.1007/BF01741485. [DOI] [PubMed] [Google Scholar]
- 6.Kissel JT, Burde RM, Klingele TG, Zeiger HE. Pupil-sparing oculomotor palsies with internal carotid-posterior communicating artery aneurysms. Ann Neurol. 1983;13:149–154. doi: 10.1002/ana.410130207. [DOI] [PubMed] [Google Scholar]
- 7.Kurokawa Y, Ishizaki E, Inaba KI. Incomplete oculomotor nerve palsy caused by an unruptured internal carotid-anterior choroidal artery aneurysm : case report. Neurol Med Chir (Tokyo) 2005;45:143–147. doi: 10.2176/nmc.45.143. [DOI] [PubMed] [Google Scholar]
- 8.Leivo S, Hernesniemi J, Luukkonen M, Vapalahti M. Early surgery improves the cure of aneurysm-induced oculomotor palsy. Surg Neurol. 1996;45:430–434. doi: 10.1016/0090-3019(95)00432-7. [DOI] [PubMed] [Google Scholar]
- 9.Mizushima H, Seki T. Midbrain hemorrhage presenting with oculomotor nerve palsy : case report. Surg Neurol. 2002;58:417–420. doi: 10.1016/s0090-3019(02)00902-3. [DOI] [PubMed] [Google Scholar]
- 10.Saito G, Otawara Y, Ogawa A. [A case report of ruptured internal carotid artery aneurysm with contralateral oculomotor nerve paresis] No Shinkei Geka. 2005;33:365–368. [PubMed] [Google Scholar]
- 11.Yeon JY, Hong SC, Kim JC. Improvement of unilateral oculomotor nerve palsy after clipping of Internal carotid-posterior Communicating Artery Aneurysm. J Korean Neurosurg Soc. 2004;35:153–156. [Google Scholar]
- 12.Zimmer DV. Oculomotor nerve palsy from posterior communicating artery aneurysm. J La State Med Soc. 1991;143:22–25. [PubMed] [Google Scholar]