Abstract
Internal carotid artery (ICA) trapping can be used for treating intracranial giant aneurysm, blood blister-like aneurysms and ICA rupture during the surgery. We present a novel ICA trapping technique which can be used with insufficient collaterals flow via anterior communicating artery (AcoA) and posterior communicating artery (PcoA). A patient was admitted with severe headache and the cerebral angiography demonstrated a typical blood blister-like aneurysm at the contralateral side of PcoA. For trapping the aneurysm, the first clip was placed at the ICA just proximal to the aneurysm whereas the distal clip was placed obliquely proximal to the origin of the PcoA to preserve blood flow from the PcoA to the distal ICA. The patient was completely recovered with good collaterals filling to the right ICA territories via AcoA and PcoA. This technique may be an effective treatment option for trapping the aneurysm, especially when the PcoA preservation is mandatory.
Keywords: Blood-blister like aneurysm, Internal carotid artery, Trapping, Subarachnoid hemorrhage
INTRODUCTION
A surgical trapping of the internal carotid artery (ICA) with or without extracranial-intracranial bypass has been commonly used an effective way to treat intracranial giant aneurysms, blood blister-like aneurysms (BBAs), and ICA rupture during the brain surgery5,8). Endovascular ICA trapping also can be used as an alternative treatment9), however, the exact positioning of endovascular materials (for example, GDCs) as saving posterior communicating artery (PcoA) and anterior choroidal artery is technically challenging.
We report a case of subarachnoid hemorrhage caused by a ruptured BBA and describe a successful technique of surgical trapping of the aneurysm, which can be an effective method to preserve collateral circulation from PcoA when collateral flow via anterior communicating artery (AcoA) is thought to be not sufficient for supply whole ICA vascular territories.
CASE REPORT
A 47-year-old woman was admitted with severe headache and drowsiness. Her initial Hunt-Hess (HH) grade was 3. A computed tomography (CT) scan revealed a thick clot throughout the basal region. The patient underwent 4-vessel cerebral angiography immediately and it demonstrated a funnel-shaped aneurysmal dilatation of the ICA at the contralateral side of the PcoA, which was typical of BBAs (Fig. 1). The patient was planned to undergo balloon test occlusion (BTO) in case of performing ICA trapping. However, the patients became irritable and unstable. Her consciousness became worse to stupor after 4-vessel cerebral angiography. BTO could not be carried out at this time. Then, we planned to operate, direct clipping of aneurysm or trapping of ICA with superficial temporal artery (STA)-middle cerebral artery (MCA) bypass. The patient was moved to operation room and her HH grade was 4 at that time.
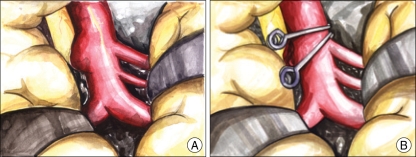
Fig. 1.

4-vessel cerebral angiography. A Blood-blister like aneurysm is demonstrated as a funnel-shaped dilation of the internal carotid artery at the contralateral side of the posterior communicating artery.
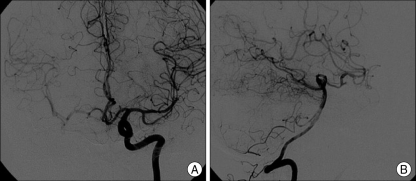
An ipsilateral pterional craniotomy was performed along with exposure of the cervical portion of the ICA. The sylvian fissure was dissected widely, and sufficient CSF was drained to prevent excessive retraction of the frontal lobe, which might have adhered to the aneurysm. The lesion was exposed through subpial dissection of the frontal lobe. Then, the ICA was trapped. The first clip was placed proximal to the aneurysm, and the distal clip was placed obliquely proximal to the origin of the PcoA so that blood flow from the PcoA to the distal ICA would be preserved while trapping the aneurysm-bearing segment of the ICA (Fig. 2). The patient became conscious in 4 days after the operation and there was no focal neurological deficit except drowsiness.
Fig. 2.
Illustrations of the internal carotid artery trapping. A : Blood-blister like aneurysm is seen on the dorsomedial wall of the internal carotid artery. B : Surgical trapping is performed by oblique clip application in order to preserve posterior communicating artery.
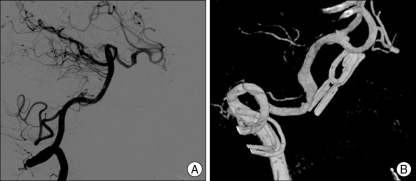
Follow-up angiography performed two weeks later revealed good collateral circulation from the ipsilateral PcoA and AcoA in both the anteroposterior and lateral views and complete obliteration of the aneurysm (Fig. 3). The patient recovered completely and was discharged 4 weeks later. One year follow-up angiography was performed. Ipsilateral PcoA was thicker in diameter, which showed better collateral circulation (Fig. 4).
Fig. 3.
Follow-up angiography at the time of discharge reveals good collateral circulation from the ipsilateral posterior communicating artery and anterior communicating artery in both the anteroposterior (A) and lateral views (B).
Fig. 4.
One year follow-up angiography. Lateral view (A) and 3-dementional rotation view (B). Ipsilateral posterior communicating artery is thicker in diameter, which shows better collateral circulation.
DISCUSSION
BBAs are thin-walled, broad-based aneurysms that lack an identifiable neck and are known to be one of the most difficult lesions to treat. They are fragile and can rupture during microsurgery. It also can cause postoperative rebleeding more frequently than saccular aneurysms2,12). The natural history of the BBA has not been clarified because this type of lesion is rare. Although several surgical strategies are available to treat BBAs, the safest treatment modality is still a matter of conjecture.
Recently, endovascular treatment (EVT), such as coiling or stenting, was tried as a treatment method of BBAs4,9,16). Kim et al.6) infer that a penetrating ulceration with focal wall defect combined with hemodynamic stress may play an important role in the development of an ICA BBA. They treated a BBA in the acute phase, conducting stent-assisted coil embolization because of the typical appearance of a BBA with small hemispherical bulge. Then, they inserted an additional stent into the ICA using the stent-within-a-stent technique to provide additional support of the fragile aneurysm neck and to decrease flow impingement, and also because they anticipated that this measure would accelerate aneurysm thrombosis and healing. They suggested that covered stents might be another option. However, they predicted that a covered stent might be too stiff to fully conform to the curved intracranial ICA wall, resulting in failure of the aneurysm sealing. Despite of this successful treatment, EVT is still hard to be an optimal treatment of BBAs so far and further studies will be needed.
Korja et al.7) reported stent-assisted coil embolization in two cases of BBAs, concluding that BBAs are not optimal targets for stent-assisted coil embolization. However, they suggested that stent-assisted coil embolization is an optional procedure for most clinics with endovascular facilities. Park et al.14), concluded that endovascular coiling of BBAs cannot be recommended due to the high rates of procedural rupture (75%), aneurysm regrowth, and rebleeding. Also, Meling et al.10) analyzed 14 patients with BBAs and did not recommend EVT in patients with BBAs. Coil placement failed in 10 cases and was judged to be unsuitable in one case. They thought that the ideal treatment of an ICA aneurysm such as BBA is aneurysm repair with parent artery preservation because they had results that trap or coil ligation of the ICA within 48 hours after SAH invariably led to poor outcomes : 6 of 7 patients died, 1survived in poor condition.
There are several surgical strategies available to treat BBAs. However, the most frightening characteristic of the BBAs was the high rate of intraoperative aneurysm rupture. Sim et al.15) experienced intraoperative rupture during dissection in 5 of 10 cases. Meling et al.10) reported, of the 11 patients treated surgically, aneurysm rupture during dissection occurred in 5 patients (45%). Therefore, a high degree of preoperative awareness and extremely careful dissection during surgery can prevent poor clinical outcomes15).
Some authors have recommended wrapping to reinforce the fragile transitional zone rather than clipping3,11). Several cases have been reported with description of successful arterial repair by suturing or vessel wrapping12,13); however, disastrous outcomes have been reported in other cases owing to ischemia using such repair techniques1). Another report was published to show a repairing method of a BBA with suturing and covering the aneurysm with an encircling aneurysm clip17).
Bypass surgery with trapping ICA can be generally accepted as one of the standard treatment methods for treating intracranial giant aneurysm, BBAs, and ICA rupture during the surgery5,8). If collateral flows via AcoA or PcoA are sufficient, trapping of the ICA either by surgical or endovascular means is well-tolerated by patients without requiring bypass surgery.
In our case, collateral flow via AcoA from contralateral ICA was noted by ipsilateral ICA compression test even though BTO was not performed due to clinically critical condition of the patient. Also, collateral flow from PcoA was good enough via intraoperative doppler monitoring so that we performed ICA trapping without bypass surgery. Also, intraoperative electroencephalogram (EEG) and somatosensory evoked potential (SSEP) monitoring revealed that there had been no change at all after ICA occlusion. The STA was prepared for possible bypass option because we could not guarantee the adequate collateral blood supply to the ipsilateral ICA before the surgery. However, bypass surgery was not performed, at last, due to enough collateral flow via PcoA after trapping of the ICA. During the surgery, the aneurysm was located just opposite site of the PcoA, complete wrapping the entire circumference of the ICA covering the lesions or using encircling clip was not feasible technically. There was adequate size of PcoA arisen at the opposite side of the blister lesion and all efforts were made to excluding the lesion from the circulation being preserved. The first clip was placed proximal to the aneurysm, and the distal clip was placed obliquely proximal to the origin of the PcoA so that blood flow from the PcoA to the distal ICA would be preserved while trapping the aneurysm-bearing segment of the ICA.
CONCLUSION
This trapping method by an oblique clip application with preserving PcoA may be an effective method for ICA trapping without bypass surgery. Even though enough collateral circulation via AcoA is noted at the preoperative angiogram, this method may be another insured method to add more blood flow to ICA via PcoA from the posterior circulation.
References
- 1.Abe M, Tabuchi K, Yokoyama H, Uchino A. Blood blister-like aneurysms of the internal carotid artery. J Neurosurg. 1998;89:419–424. doi: 10.3171/jns.1998.89.3.0419. [DOI] [PubMed] [Google Scholar]
- 2.Batjer H, Samson D. Intraoperative aneurysmal rupture : incidence, outcome, and suggestions for surgical management. Neurosurgery. 1986;18:701–707. doi: 10.1227/00006123-198606000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Ishikawa T, Nakamura N, Houkin K, Nomura M. Pathological consideration of a "blister-like" aneurysm at the superior wall of the internal carotid artery: Case report. Neurosurgery. 1997;40:403–405. doi: 10.1097/0006123-199702000-00038. discussion 405-406. [DOI] [PubMed] [Google Scholar]
- 4.Islam MS, Manabe H, Hasegawa S, Takamura A, Nagahata M. Successful staged treatment for ruptured blister-like dissecting aneurysm of the intracranial internal carotid artery: acute GDC embolization for the blister like aneurysm followed by proximal occlusion with extracranial intracranial bypass in the chronic stage. Minim Invasive Neurosurg. 2004;47:165–168. doi: 10.1055/s-2004-818490. [DOI] [PubMed] [Google Scholar]
- 5.Kai Y, Hamada J, Morioka M, Yano S, Mizuno T, Kuroda J, et al. Treatment strategy for giant aneurysms in the cavernous portion of the internal carotid artery. Surg Neurol. 2007;67:148–155. doi: 10.1016/j.surneu.2006.03.037. discussion 155. [DOI] [PubMed] [Google Scholar]
- 6.Kim BM, Chung EC, Park SI, Choi CS, Won YS. Treatment of blood blister-like anerysm of the internal carotid artery with stent-assisted coil embolization followed by stent-within-a-stent technique. Case report. J Neurosurg. 2007;107:1211–1213. doi: 10.3171/JNS-07/12/1211. [DOI] [PubMed] [Google Scholar]
- 7.Korja M, Rautio R, Valtonen S, Haapanen A. Primary treatment of ruptured blood blister-like aneurysms with stent-assisted coil embolization : report of two cases. Acta Radiol. 2008;49:180–183. doi: 10.1080/02841850701675735. [DOI] [PubMed] [Google Scholar]
- 8.Lawton MT, Hamilton MG, Morcos JJ, Spetzler RF. Revascularization and aneurysm surgery : current techniques, indications, and outcome. Neurosurgery. 1996;38:83–92. doi: 10.1097/00006123-199601000-00020. discussion 92-94. [DOI] [PubMed] [Google Scholar]
- 9.McNeely PD, Clarke DB, Baxter B, Vandorpe RA, Mendez I. Endovascular treatment of a "blister-like" aneurysm of the internal carotid artery. Can J Neurol Sci. 2000;27:247–250. doi: 10.1017/s0317167100000901. [DOI] [PubMed] [Google Scholar]
- 10.Meling TR, Sorteberg A, Bakke SJ, Slettebø H, Hernesniemi J, Sorteberg W. Blood blister-like aneurysms of the internal carotid artery trunk causing subarachnoid hemorrhage : treatment and outcome. J Neurosurg. 2008;108:662–671. doi: 10.3171/JNS/2008/108/4/0662. [DOI] [PubMed] [Google Scholar]
- 11.Nakagawa F, Kobayashi S, Takemae T, Suqita K. Aneurysms protruding from the dorsal wall of the internal carotid artery. J Neurosurg. 1986;65:303–308. doi: 10.3171/jns.1986.65.3.0303. [DOI] [PubMed] [Google Scholar]
- 12.Ogawa A, Suzuki M, Ogasawara K. Aneurysms at nonbranching sites in the supraclinoid portion of the internal carotid artery : internal carotid artery trunk aneurysms. Neurosurgery. 2000;47:578–583. doi: 10.1097/00006123-200009000-00008. discussion 583-586. [DOI] [PubMed] [Google Scholar]
- 13.Ogilvy CS. Repair of an arterial perforation of the internal carotid artery using Hemashield wrapping with aneurysm clip reinforcement : technical note. Neurosurgery. 1997;40:1312–1314. doi: 10.1097/00006123-199706000-00041. [DOI] [PubMed] [Google Scholar]
- 14.Park JH, Park IS, Han DH, Kim SH, Oh CW, Kim JE, et al. Endovascular treatment of blood blister-like aneurysms of the internal carotid artery. J Neurosurg. 2007;106:812–819. doi: 10.3171/jns.2007.106.5.812. [DOI] [PubMed] [Google Scholar]
- 15.Sim SY, Shin YS, Cho KG, Kim SY, Kim SH, Ahn YH, et al. Blood blister-like aneurysms at nonbranching sites of the internal carotid artery. J Neurosurg. 2006;105:400–405. doi: 10.3171/jns.2006.105.3.400. [DOI] [PubMed] [Google Scholar]
- 16.Tanoue S, Kiyosue H, Matsumoto S, Yamashita M, Nagatomi H, Mori H. Ruptured "blister-like" aneurysm with a pseudoaneurysm formation requiring delayed intervention with endovascular coil embolization. Case report. J Neurosurg. 2004;101:159–162. doi: 10.3171/jns.2004.101.1.0159. [DOI] [PubMed] [Google Scholar]
- 17.Yanaka K, Meguro K, Nose T. Repair of a tear at the base of a blister-like aneurysm with suturing and an encircling clip : Technical Note. Neurosurgery. 2000;50:218–221. doi: 10.1097/00006123-200201000-00037. [DOI] [PubMed] [Google Scholar]