Abstract
BACKGROUND:
The prevalence and mortality of chronic obstructive pulmonary disease (COPD) in women have been predicted to overtake that of men within the next decade. These predictions are based in part on data from surveys using self-reports of a COPD diagnosis. Whether these predictions have been realized is unknown.
METHODS:
The prevalence and mortality of men and women in British Columbia were compared from fiscal years 1992/1993 to 2003/2004 using administrative health services data. Case definitions for COPD were developed using International Classification of Diseases ninth and 10th revision (ICD-9/10) codes applied to medical and hospital data. Individuals 45 years and older, who had at least two physician visits or one hospitalization for specified COPD ICD-9/10 codes within a 365-day window, were considered to be cases. Cases were ascertained from 1992 to 2004.
RESULTS:
In 2003/2004, men had a greater prevalence (4.7% versus 4.0% in women) and a higher all-cause mortality rate (5.4% versus 4.1% in women) than women. Both men and women with COPD had low COPD medication use (45%) and low referral for lung function testing (55%). Including the ICD-9 code for ‘bronchitis, not specified as acute or chronic’ (ICD-9 490) in the case definition resulted in a greater prevalence of COPD in women than in men overall, and in the 45 to 64 year age group.
CONCLUSION:
Prevalence and mortality measured with administrative health data do not show evidence of relative increase in the prevalence of COPD for women in British Columbia. However, further analysis of ICD-9 490 may identify an early ‘at-risk’ group, specifically in women.
Keywords: Administrative database, Chronic obstructive pulmonary disease, Epidemiology, Gender, Mortality, Prevalence, Sex, Spirometry utilization
Abstract
HISTORIQUE :
On avait prévu que la prévalence et la mortalité de la maladie pulmonaire obstructive chronique (MPOC) chez les femmes dépasseraient celles des hommes d’ici dix ans. Ces prévisions se fondent en partie sur des données tirées d’enquêtes d’autoévaluation d’un diagnostic de MPOC. On ne sait pas si ces prévisions se sont réalisées.
MÉTHODOLOGIE :
Les auteurs ont comparé la prévalence et la mortalité des hommes et des femmes de la Colombie-Britannique de l’exercice 1992–1993 à l’exercice 2003–2004 au moyen de données administratives des services de santé. Ils ont établi les définitions de cas de la MPOC au moyen des codes des neuvième et dixième révisions de la Classification internationale des maladies (CIM-9/10) appliqués aux données médicales et hospitalières. Les personnes de 45 ans et plus qui avaient consulté le médecin au moins deux fois ou été hospitalisées au moins une fois pour les codes CIM-9/10 de MPOC dans une fenêtre de 365 jours étaient considérées comme des cas. Ces cas ont été contrôlés de 1992 à 2004.
RÉSULTATS :
En 2003–2004, les hommes avaient une plus forte prévalence (4,7 % par rapport à 4,0 % chez les femmes) et un plus fort taux de mortalité toutes causes confondues (5,4 % par rapport à 4,1 %) que les femmes. Tant les hommes que les femmes atteints d’une MPOC utilisaient peu de médicaments contre la MPOC (45 %) et étaient peu aiguillés pour faire évaluer leur fonction pulmonaire (55 %). Si on incluait dans la définition de cas le code de la CIM-9 pour la bronchite dont la chronicité ou l’acuité n’étaient pas précisée (CIM-9 450, version anglaise), on obtenait une plus forte prévalence de MPOC chez les femmes que chez les hommes dans l’ensemble, ainsi que dans le groupe des 45 à 64 ans.
CONCLUSION :
La prévalence et la mortalité mesurées au moyen de données administratives de santé ne procurent pas de résultats probants quant à l’augmentation relative de la prévalence de MPOC chez les femmes de la Colombie-Britannique. Toutefois, une analyse plus approfondie de la CIM-9 450 peut permettre de repérer un groupe précoce « à risque », justement chez les femmes.
The prevalence of chronic obstructive pulmonary disease (COPD) is increasing in women (1,2) and is likely due, in part, to changes in cigarette smoking patterns and possibly a greater susceptibility of women to develop COPD (3–6). In 2001, Health Canada released a report entitled Respiratory Disease in Canada (7) predicting that by 2002, the epidemiological trends of COPD would shift, with prevalence, hospitalizations and mortality for women with COPD surpassing those for men. There have been few studies to determine whether these predicted sex differences have been realized on a population-based scale and whether these differences translate into sex differences in diagnostic testing or treatment. To date, Canadian estimates for COPD prevalence have been largely based on self-report of diagnosis. It is not known whether an increased susceptibility for COPD in women can be detected in larger, population-based administrative data.
Administrative health databases provide a valuable method for identifying sex differences in the epidemiology of COPD, because they provide large sample sizes, have strong statistical power, are relatively inexpensive studies to conduct, and can link information on diagnosis, treatment and mortality. These databases may represent the ‘real world’ more accurately and characterize sex differences more fully than do other data sources.
The purpose of the present study was to determine whether administrative health data from British Columbia (BC) could be used to detect the predicted increase in women in prevalence and mortality of COPD from 1992/1993 to 2003/2004 compared with men. We also tested for sex differences in referral for diagnostic (lung function) testing and use of COPD medications.
METHODS
COPD cases were abstracted from the BC Ministry of Health (MOH) administrative health service databases. Individuals were considered to have COPD if they were 45 years of age or older, and had at least one hospitalization or two physician visits coded with an International Classification of Diseases ninth or 10th revision (ICD-9/10) code for COPD (Table 1) within any 365-day window between April 1, 1992, and March 31, 2004. For cases ascertained from hospital data, the ICD-9/10 code for COPD could be any one of the diagnoses from the hospital discharge summary. Individuals whose sex was unknown were excluded. On meeting these criteria, individuals were considered to have COPD until death or emigration from BC. Prevalent cases of COPD for each year were defined as cumulative incident cases of COPD from April 1, 1992, to the end of each fiscal year, less those lost due to death or emigration before the start of the fiscal year. Population estimates for the denominators were obtained from the MOH registry of insured residents. Rates were age-standardized to the 2001 BC census population estimates using direct standardization and five-year age groups. Cases may have had codes for other chronic lung diseases in addition to COPD, such as asthma, tuberculosis or interstitial lung disease; however, overlap with other chronic lung diseases was not measured in the present study.
TABLE 1.
International Classification of Diseases ninth and 10th revision (ICD-9/ICD-10) codes included in the case definition for chronic obstructive pulmonary disease
| ICD-9 description | Code |
|---|---|
| Chronic bronchitis | 491 |
| Emphysema | 492 |
| Chronic airways obstruction, not elsewhere classified | 496 |
| ICD-10 description | Code |
| Simple and mucopurulent chronic bronchitis | J41 |
| Unspecified chronic bronchitis | J42 |
| Emphysema | J43 |
| Other chronic obstructive pulmonary disease | J44 |
Some studies (8–11) have included the ICD-9 code 490 (bronchitis, not specified as acute or chronic) in their COPD case definition, but the validity of including this ICD-9 code has been questioned (12). Therefore, COPD prevalence, the use of medication and spirometry use were measured with and without ICD-9 code 490 included in the case definition to determine the impact of this code on sex differences in prevalence. As with the other COPD codes, individuals with ICD-9 code 490 were required to have two physician visits or one hospitalization coded with ICD-9 code 490 within any 365-day window.
Data on lung function testing were retrieved from the Medical Services Plan database, which includes records on outpatient billable diagnostic tests or procedures. The prevalence of ever having lung function testing was compared between 1992 and 2004, for men and women with COPD who were alive and residing in BC in the 2003/2004 fiscal year.
Medication use data were obtained from the PharmaNet database, which contains records for all prescriptions filled in BC. To be considered a user of COPD medications, an individual had to fill at least two prescriptions of any medication within any of 12 major medication categories (Table 2) during the time period. Using the 2003/2004 prevalent cases, the odds of men and women filling prescriptions for COPD medications from April 1, 2002, to March 31, 2004, were compared.
TABLE 2.
Chronic obstructive pulmonary disease (COPD) medication categories*
| Medication category |
|---|
| Bronchodilators – solution |
| Bronchodilator – short-acting inhaler |
| Bronchodilator – long-acting inhaler |
| Bronchodilator – oral |
| Anticholinergics – short-acting inhaler |
| Anticholinergics – short-acting solution |
| Anticholinergics – long-acting inhaler |
| Bronchodilator/anticholinergic combination therapy inhaler |
| Leukotriene receptor agonists |
| Corticosteroids – inhaler |
| Corticosteroids – solution |
| Bronchodilator/corticosteroid combination therapy inhaler |
To be counted as receiving COPD medications, each patient had to fill at least two prescriptions for any medication within a medication category at some time between 2002 and 2004
All-cause mortality data were obtained from the MOH for all COPD cases by sex and age category for the years 1992/1993 to 2003/2004. In addition, the all-cause mortality for COPD versus non-COPD was compared.
Trends for age-standardized prevalence of COPD between April 1, 1992, and March 31, 2004, were estimated by dividing prevalent cases by the number of insured residents in BC for each fiscal year, and expressed by sex. Comparisons between sexes for prevalence, medication use or lung function testing are expressed using proportions or unadjusted ORs using the software package SAS version 8 (SAS Institute Inc, USA).
The data analysis was conducted within the BC MOH and was approved by the BC MOH and the University of British Columbia, Vancouver, BC.
RESULTS
Prevalence
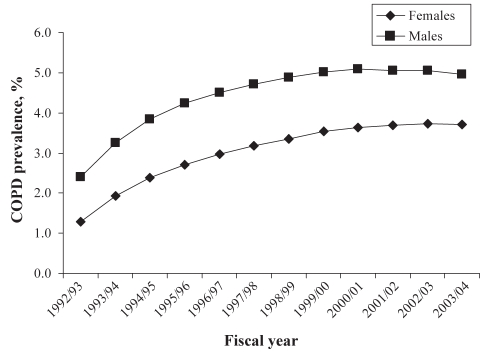
There were 1,713,759 insured individuals in BC who were 45 years of age or older in the fiscal year 2003/2004. Approximately 5341 of these individuals did not have sex listed in the database, leaving 1,708,418 individuals who made up the total population denominator for analysis. Of these, 38,458 men (crude prevalence 4.7%) and 34,960 women (crude prevalence 4.0%) met the case definition for COPD at some time between 1992 and 2004, and were still alive and residing in BC in 2003/2004. Age-standardized prevalence increased for both men and women from 1992/1993 to 2003/2004 (Figure 1), but there was no substantial relative increase in prevalence in women compared with men. Data on a concurrent diagnosis of asthma were not available for this analysis.
Figure 1).
Chronic obstructive pulmonary disease (COPD) age-standardized prevalence by sex, 1992/1993 to 2003/2004
Lung function testing and medication use
Approximately 55% of the 2003/2004 COPD population had lung function testing billed during the period 1992/1993 to 2003/2004. Only 45% of the 2003/2004 prevalent COPD cases had filled prescriptions for COPD-related medications in the period from 2002 to 2004. Similar proportions of men and women underwent lung function testing.
The majority of filled prescriptions (53%) were for short-acting bronchodilator medications (beta2-agonists and anti-cholinergics) followed by inhaled corticosteroids (21%) and long-acting bronchodilators (10%). Women were slightly more likely than men to have filled a prescription for any COPD medication (OR 1.16, 95% CI 1.13 to 1.20). Long-acting bronchodilator medication made up 10% of all COPD prescriptions filled for men but only 5% of prescriptions filled for women. In the period from 2002 to 2004, long-acting beta2-agonists were available to all COPD patients in BC. Long-acting anticholinergics (tiotropium) were available but not paid for under the government prescription reimbursement program; hence, few tiotropium prescriptions were filled.
Mortality
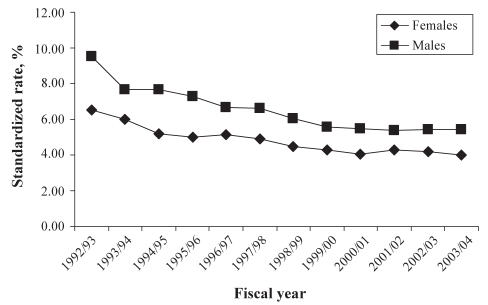
From 1992/1993 to 2003/2004 there was a steady decline in the age-standardized mortality rate for both sexes, although this trend reached a plateau by 1999/2000 (Figure 2). A progressive increase in the number of female deaths or in age-specific female mortality rate in COPD cases over the study period was not observed.
Figure 2).
Age-standardized all-cause mortality for people with chronic obstructive pulmonary disease by sex, 1992/1993 to 2003/2004
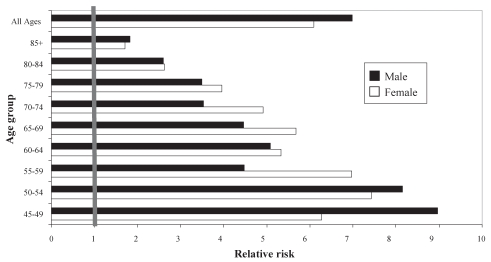
Individuals with COPD had a much higher risk of all-cause mortality than individuals without COPD for all age groups, but the excessive risk was most striking in the younger age groups (Figure 3). For all ages combined, the COPD versus non-COPD risk of all-cause mortality was higher for men than for women, but this appeared to be largely driven by a higher risk of mortality in COPD versus non-COPD males in the 45 to 49 and 50 to 54 year age groups. A higher risk for all-cause mortality in COPD versus non-COPD patients was seen for women than for men in the 55 to 59, 65 to 69 and 70 to 74 year age groups.
Figure 3).
Risk of all-cause mortality for individuals with chronic obstructive pulmonary disease compared with individuals without chronic obstructive pulmonary disease, by sex, 2003/2004
Inclusion of ICD-9 code 490 (bronchitis, not specified as acute or chronic) in the case definition
The inclusion of ICD-9 code 490 in the COPD case definition doubled the prevalence of COPD in BC (Table 3). When ICD-9 code 490 was included in the case definition, the prevalence of COPD cases fulfilling the case definition due to a hospital contact decreased from 44% to 3%. There were important sex differences in the prevalence of COPD by age group when ICD-9 code 490 was included in the case definition. In those aged 65 years and older, the prevalence of COPD was greater in men than in women, regardless of inclusion or exclusion of ICD-9 code 490. However, in those aged 45 to 64 years, women had a higher prevalence of COPD compared with men when ICD-9 code 490 was included. Sex differences in this younger age group disappeared when ICD-9 code 490 was excluded from the COPD case definition. Lung function testing and COPD medication use was much lower in those coded with ICD-9 490 exclusively compared with those with ICD-9 codes 491 (chronic bronchitis), 492 (emphysema) and/or 496 (unspecified COPD).
TABLE 3.
International Classification of Diseases ninth revision (ICD-9) code 490 (bronchitis, not specified as acute or chronic) analysis
| Prevalence | COPD prevalence: ICD-9 491, 492, 496; %
|
COPD prevalence: ICD-9 491, 492, 496; 490; %
|
||
|---|---|---|---|---|
| Male | Female | Male | Female | |
| All ages | 4.70 | 4.00 | 9.50 | 10.50 |
| Age 65 years and older | 10.80 | 7.90 | 16.30 | 15.10 |
| Age 45–64 years | 1.90 | 1.60 | 6.30 | 7.80 |
|
Subgroup: ICD-9 491, 492, 496 only; % |
Subgroup: ICD-9 490 only; % |
|||
| COPD medication use | 45 | 11 | ||
| Lung function testing | 55 | 23 | ||
ICD-9 codes 491: chronic bronchitis; 492: emphysema; and 496: unspecified chronic obstructive pulmonary disease (COPD)
DISCUSSION
In the present study, we used administrative health services data from BC to estimate sex differences in COPD prevalence, mortality, lung function testing and the use of medication. Specifically, we aimed to see whether the predicted increase of COPD prevalence and mortality in women could be detected in the BC population using administrative health data. We did not see evidence of a dramatic shift in the epidemiological trends of COPD in this province but discovered that differences in medical coding may be influencing COPD prevalence estimates. In addition, our study did not demonstrate any difference in the use of lung function testing between men and women, and found only a small increase in the likelihood of women with COPD filling prescriptions for COPD medications.
COPD prevalence has been estimated in a number of ways, including self-report or measurement of airflow obstruction. All methods have problems with their validity. Self-report likely underestimates the true prevalence of COPD because many affected individuals may not see a doctor until the disease is quite advanced. Population-based random sampling and subsequent measurement of airflow obstruction is likely the most accurate method of determining the true prevalence of COPD in an area, but have limited external validity beyond the community that is sampled. In addition, the enormous expense of conducting such studies precludes the repeated measurement that is required to identify epidemiological trends.
We used administrative data as an alternative method of estimating the prevalence of COPD. Administrative data are routinely used in COPD for morbidity and hospitalization surveillance (13). A key issue in using this data source is the validity of the case definition in accurately identifying COPD cases. The validity of administrative data for epidemiological studies of COPD has been tested in several studies. Two Canadian studies (14,15) found that COPD patients identified from medical records were accurately coded in physician service claims data. Another study (16) from the United Kingdom found moderate agreement between administrative database-identified COPD patients and their medical records. Lacasse et al (12) did question the validity of using administrative data to identify COPD cases but used as their gold standard the self-report prevalence data from the National Population Health Survey, in itself a source that has not been validated against medical records. Their prevalence estimate was also based on a less stringent case definition, which required only one contact for COPD within the five-year period.
Our estimates were lower than those reported by Health Canada (1) using survey data. Their survey estimated prevalence by asking a random, population-based sample whether they had COPD as diagnosed by a health professional. Their 1998/1999 estimates were similar to our estimates for women but were much lower than our estimates for men (2.8% versus 4.7%, respectively). It has been suggested that sex bias in COPD could occur (17) and this bias could result in a lower estimate of prevalence for women. However, if this bias did occur in our sample, we would also expect that it could be detected in the self-report data on health professional-diagnosed COPD, yet women had a higher prevalence of COPD than men in the Health Canada estimates. Whether differences in self-report behaviours between men and women result in different prevalent estimates is unknown.
Our prevalence estimates are much lower than those estimated from studies using randomly sampled, population-based lung function measurement. In the United States, the 1988 to 1994 prevalence of COPD as measured by lung function was 7.4% and 5.8% for moderate disease for men and women, respectively (2). In Canada, results of the Burden of Lung Disease (BOLD) study (18) estimated that 19.3% of those 40 years of age and older and living in Vancouver, BC, had airflow obstruction consistent with COPD. Even when the diagnosis was limited to Global Initiative for Chronic Obstructive Lung Disease stage 2 or greater (likely signifying clinically significant disease) the prevalence of COPD was 8.2% – a much higher prevalence than in our study. The reasons why administrative health data estimates of COPD prevalence are much lower than population-based studies are not clear. It is possible that symptoms do not begin and diagnosis is not made until the disease reaches Global Initiative for Chronic Obstructive Lung Disease stage 3 or 4. An additional factor may be that COPD is underdiagnosed or coded at either the general practitioner or hospital level. Recent data from other jurisdictions support the latter hypothesis; it has been suggested that as many as 75% of Europeans and 50% of Americans with COPD are undiagnosed (19).
Our mortality data differ from those of Health Canada (1) in that we report all-cause mortality of individuals previously coded for COPD, whereas the Health Canada data reported mortality rates of death thought to be due to COPD itself. Nevertheless, our results show a trend of decreasing age-standardized mortality rates from 1992/1993 to 2000/2001, followed by a stable mortality rate from 2001 onward for both men and women with COPD. On the other hand, Health Canada reported an increase for women older than 75 years and an increase for men older than 80 years of age over a similar time period. Because we used all-cause mortality data, decreasing trends in mortality in our COPD patients could be due to decreasing trends in mortality in other causes of death, such as cardiovascular disease, or decreased exposure to risk factors, such as cigarette smoking. However, there was no similar trend of decreasing mortality in the non-COPD group over the same time period (data not shown).
It was surprising that the COPD versus non-COPD risk for all-cause mortality was higher in women than in men for several age groups. Why men would have a higher risk than women in the younger age groups (45 to 49 years, 50 to 54 years) and women would show a higher risk in the older age groups up to the 75 to 79 year group is unclear. Of note, the onset of menopause has been linked to more rapid decline in lung function in female COPD patients who continue to smoke (6). Whether such an effect would result in increased mortality in women with COPD is unknown, but our data highlight the importance of measuring mortality in men and women by age group in addition to reporting aggregate results.
We found that including ICD-9 code 490 (bronchitis, not specified as acute or chronic) had a substantial effect on estimates of COPD prevalence, nearly doubling it in our cohort. However, these individuals coded with ICD-9 490 may not have COPD because only 11% of individuals coded solely with ICD-9 490 were on COPD medications. However, COPD cannot be ruled out in this group, which had an even lower prevalence of lung function testing than the COPD patients coded with ICD-9 491, 492 or 496. Although it seems likely that these individuals do not yet have clinically significant COPD, they may represent an ‘early’ COPD group; ie, it is possible that these individuals may have chronic bronchitis but may or may not have airflow obstruction. Because lung function testing was rarely performed, it is difficult to ascertain whether they have COPD. Because chronic cough is also a feature of asthma, this may also represent an untreated asthma group.
The inclusion of ICD-9 code 490 had a large impact on the sex differences in prevalence of ‘COPD’ in the younger age groups, where prevalence of COPD in women was much higher than that of men. Whether these younger women who have repeated episodes of bronchitis (at least two doctor’s visits for bronchitis within one year) represent the beginning of the ‘female COPD epidemic’ is unknown, but longitudinal studies on the outcomes of this group could provide valuable information on this issue. Specifically, further investigation on the concurrent diagnosis of asthma, the use of respiratory medications over time (including antibiotics), health care utilization and hospitalization rates would help determine whether these individuals have clinically significant disease.
Only 55% of the COPD population had lung function testing over the 10-year period. Our results reflect outpatient lung function testing only, because administrative health services data from BC does not capture bedside spirometry, which may occur during a hospital admission. However, it is recommended that spirometry to confirm a diagnosis of COPD should be done when the patient is stable with no recent history of an exacerbation (20). Therefore, we would expect that the majority of lung function testing associated with good clinical practice, including during the diagnostic period, would occur on an outpatient basis. Similarly, less than one-half of our COPD population had filled prescriptions for COPD-related medications. This may reflect mild disease severity in this population, or be due to poor adherence to COPD guidelines. Although we do not have data on disease severity, we can assume that on an individual basis the disease had progressed to the point of the patient experiencing symptoms that necessitated a physician visit. It is possible that COPD is undertreated. Foster et al (21) found that only 25% of American primary care physicians reported using guidelines to aid decision-making in treating COPD, and of those, only 50% would use long-acting bronchodilators to treat persistent dyspnea. Similarly, in a 2003 Japanese study, Takahashi et al (22) reported that 31% of COPD patients with moderate to severe COPD did not receive any clinical intervention. Clearly, this is an area that requires further investigation.
In the present study, we estimated prevalence by calculating the cumulative incidence of COPD for each year from 1992/1993 to 2003/2004. A patient remained in the COPD database even if the physician subsequently changed the diagnosis. This accumulation of false positives would overestimate prevalence and also could explain the increase in prevalence we measured over the study time period. Conversely, it is likely that our estimates have also included individuals with predominantly symptomatic moderate and severe COPD but have not captured the milder cases, which could underestimate prevalence. In addition, our relatively short observation period (approximately 10 years) could have limited our ability to detect sex differences in the epidemiology of COPD.
CONCLUSION
We used data from large administrative health databases to describe the sex differences in COPD prevalence, mortality, lung function testing and medication use. We did not see strong evidence of a rapid increase in prevalence or mortality from COPD in women over the period 1992/1993 to 2003/2004. Similar proportions of male and female COPD patients underwent lung function testing and had filled prescriptions for COPD medications. Finally, the reversal of male versus female prevalence in the younger age group when ICD-9 code 490 was included in the case definition brings up the possibility that this group of younger individuals with ‘bronchitis’ may represent early COPD. Further studies of these individuals, including patterns of health care use, may better characterize this group.
Acknowledgments
This report represents a joint collaboration between the British Columbia Ministry of Health (Chronic Diseases Management Branch) and respiratory clinician researchers affiliated with the University of British Columbia.
Footnotes
FUNDING: This research study was funded by the British Columbia Ministry of Health. Pat Camp is funded by a Canadian Institutes of Health Research fellowship, a Canadian Respiratory Health Professionals fellowship and by ICEBERGS, a Canadian Institutes of Health Research Interdisciplinary Capacity Enhancement research team focused on sex and COPD.
INSTITUTIONS WHERE WORK WAS PERFORMED: British Columbia Ministry of Health and University of British Columbia.
REFERENCES
- 1.Canadian Institute for Health Information, Canadian Lung Association, Health Canada, Statistics Canada . Respiratory Disease in Canada. Ottawa: Health Canada; 2001. pp. 45–55. [Google Scholar]
- 2.Mannino D, Homa DM, Akinbami LG, Ford ES, Redd SC. Chronic obstructive pulmonary disease surveillance – United States, 1971–2000. MMWR CDC Surveill Summ. 2002;51:1–16. [PubMed] [Google Scholar]
- 3.Chen Y, Horne SL, Dosman JA. Increased susceptibility to lung dysfunction in female smokers. Am Rev Respir Dis. 1991;143:1224–30. doi: 10.1164/ajrccm/143.6.1224. [DOI] [PubMed] [Google Scholar]
- 4.Xu X, Li B, Wang L. Gender difference in smoking effects on adult pulmonary function. Eur Respir J. 1994;7:477–83. doi: 10.1183/09031936.94.07030477. [DOI] [PubMed] [Google Scholar]
- 5.Silverman EK, Weiss ST, Drazen JM, et al. Gender-related differences in severe, early-onset chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2000;162:2152–8. doi: 10.1164/ajrccm.162.6.2003112. [DOI] [PubMed] [Google Scholar]
- 6.Gan WQ, Man SF, Postma DS, Camp P, Sin DD. Female smokers beyond the perimenopausal period are at increased risk of chronic obstructive pulmonary disease: A systematic review and meta-analysis. Respir Res. 2006;7:52. doi: 10.1186/1465-9921-7-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Public Health Agency of Canada Respiratory Disease in Canada<www.phac-aspc.gc.ca/publicat/rdc-mrc01/index-eng.php> (Version current at November 3, 2008).
- 8.Lacasse Y, Brooks D, Goldstein RS. Trends in the epidemiology of COPD in Canada, 1980 to 1995. Chest. 1999;116:306–13. doi: 10.1378/chest.116.2.306. [DOI] [PubMed] [Google Scholar]
- 9.Anthonisen NR, Dik N, Manfreda J, Roos LL. Spirometry and obstructive lung disease in Manitoba. Can Respir J. 2001;8:421–6. doi: 10.1155/2001/572825. [DOI] [PubMed] [Google Scholar]
- 10.Sin DD, Stafinski T, Ng YC, Bell NR, Jacobs P. The impact of chronic obstructive pulmonary disease on work loss in the United States. Am J Respir Crit Care Med. 2002;165:704–7. doi: 10.1164/ajrccm.165.5.2104055. [DOI] [PubMed] [Google Scholar]
- 11.Sin DD, Wells H, Svenson LW, Man SF. Asthma and COPD among aboriginals in Alberta, Canada. Chest. 2002;121:1841–6. doi: 10.1378/chest.121.6.1841. [DOI] [PubMed] [Google Scholar]
- 12.Lacasse Y, Montori VM, Lanthier C, Maltais F. The validity of diagnosing chronic obstructive pulmonary disease from a large administrative database. Can Respir J. 2005;12:251–6. doi: 10.1155/2005/567975. [DOI] [PubMed] [Google Scholar]
- 13.Public Health Agency of Canada Chronic Disease Infobase <http://204.187.39.30/surveillance/Mapdb/Infobase_e.htm> (Version current at November 3, 2008).
- 14.McKnight J, Scott A, Menzies D, Bourbeau J, Blais L, Lemiere C. A cohort study showed that health insurance databases were accurate to distinguish chronic obstructive pulmonary disease from asthma and classify disease severity. J Clin Epidemiol. 2005;58:206–8. doi: 10.1016/j.jclinepi.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 15.Rawson NS, D’Arcy C. Assessing the validity of diagnostic information in administrative health care utilization data: Experience in Saskatchewan. Pharmacoepidemiol Drug Safety. 1998;7:389–98. doi: 10.1002/(SICI)1099-1557(199811/12)7:6<389::AID-PDS380>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 16.Soriano JB, Maier WC, Visick G, Pride N. Validation of general practitioner-diagnosed COPD in the UK General Practice Research Database. Eur J Epidemiol. 2001;17:1075–80. doi: 10.1023/a:1021235123382. [DOI] [PubMed] [Google Scholar]
- 17.Chapman KR, Tashkin DP, Pye DJ. Gender bias in the diagnosis of COPD. Chest. 2001;119:1691–5. doi: 10.1378/chest.119.6.1691. [DOI] [PubMed] [Google Scholar]
- 18.Buist AS, McBurnie MA, Vollmer WM, et al. International variation in the prevalence of COPD (The BOLD Study): A population-based prevalence study. Lancet. 2007;370:741–50. doi: 10.1016/S0140-6736(07)61377-4. [DOI] [PubMed] [Google Scholar]
- 19.Tinkelman DG, Price DB, Nordyke RJ, Halbert RJ. Misdiagnosis of COPD and asthma in primary care patients 40 years and older. J Asthma. 2006;43:75–80. doi: 10.1080/02770900500448738. [DOI] [PubMed] [Google Scholar]
- 20.O’Donnell DE, Aaron S, Bourbeau J, et al. Canadian Thoracic Society recommendations for management of chronic obstructive pulmonary disease – 2007 update. Can Respir J. 2007;14(Supp B):5B–32B. doi: 10.1155/2007/830570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Foster JA, Yawn BP, Maziar A, Jenkins T, Rennard SI, Casebeer L. Enhancing COPD management in primary care settings. MedGenMed. 2007;9:24. [PMC free article] [PubMed] [Google Scholar]
- 22.Takahashi T, Ichinose M, Inoue H, Shirato K, Hattori T, Takishima T. Underdiagnosis and undertreatment of COPD in primary care settings. Respirology. 2003;8:504–8. doi: 10.1046/j.1440-1843.2003.00501.x. [DOI] [PubMed] [Google Scholar]