Abstract
Purpose: Although it is widely recognized that caregivers of individuals with dementia experience elevated stress that places them at increased risk for health problems, little is known about how caregiving stress may be alleviated among underserved ethnic minority populations. The purpose of this study was to compare a complementary and alternative medicine therapy, polarity therapy (PT), to an enhanced respite control condition (ERC) to reduce stress and depression and improve quality of life for American Indian (AI) and Alaskan Native family caregivers.Design and Methods: Forty-two AI family caregivers of individuals with dementia, living on and off reservations in the Pacific Northwest, were randomized to an 8-session trial of PT or ERC. PT is a touch therapy that uses gentle pressure on energy points and biofields to help the client achieve physiological relaxation. ERC included respite care for the person with dementia and a choice of activities for the caregiver. Average age of caregivers was 50 years (range 27–69 years); 90% were women; 52% daughters, 10% wives, 7% sons, and 31% other relatives. Outcome assessments administered at baseline and posttreatment included caregiver perceived stress, depression, quality of life, sleep quality, worry, and physical health. Results: PT participants improved significantly more than ERC participants on stress (p = .01), depression (p = .045.), bodily pain (p = .02), vitality (p = .03), and general health (p = .01). Implications: These results indicate that the delivery of PT to AI dementia family caregivers is feasible and culturally acceptable and may be an important approach to reducing stress, depression, and pain.
Keywords: Polarity therapy, Touch therapy, Massage, Complementary and alternative medicine
American Indian (AI) tribes comprise more than 690 (recognized and unrecognized) heterogeneous nations and peoples. Between 1980 and 1990, the aging AI population grew by 52% (Department of Health and Human Services, Office for American Indian Alaskan Native and Native Hawaiian Programs, 1997). The number of AI elderly adults countrywide is expected to exceed 700,000 (twice as many women as men) by the year 2050 (Jervis & Manson, 2002), and many of these individuals will either be caregivers for relatives or require a family caregiver as they become more physically and cognitively frail. However, little is known about dementia caregiving within AI populations (Jervis & Manson; Jervis, Jackson, & Manson, 2002), and there are no published studies of interventions to support or assist AI caregivers.
In the general population, caring for a family member with dementia creates conditions of chronic stress that increase the risk of poor physical and psychological health (Belle et al., 2006). For example, caregivers have high rates of depression (Covinsky et al., 2003) and a diminished immune response (Li et al., 2007), leading to higher utilization of primary care and higher mortality (Schulz & Beach, 1999). Caregiver stress and burden result in a reciprocal decrement in the quality of life for the care recipient and often lead to institutionalization of the person with dementia (Mittelman et al., 1993).
Data on caregiving for relatives with dementia in AI communities are sparse (Dilworth-Anderson, Williams, & Gibson, 2002; Jervis & Manson, 2002; Jervis et al., 2002), although the imperative to provide care for elders has been identified as a core cultural value (Jervis & Manson). In an investigation of caregiving among AIs, a survey of Pueblo Indian caregivers reported that 86% of primary caregivers were women (54% were daughters and 11% were wives) and that caregiving placed a strain on the community as a whole as well as on individual caregivers (John, Hennessy, Dyeson, & Garrett, 2001). AI caregivers face the same challenges as non-Indians, including competing demands of family and work, distance, and lack of resources. For AI caregivers, however, there are often additional stressors and obstacles to delivering care, including poverty, lack of access to support services, and lack of systemic understanding of individual needs (Jervis et al.). A recent analysis of 2000 U.S. Census data revealed increased levels of functional limitation in AI older adults compared with White and African American older adults (Goins, Moss, Buchwald, & Guralnik, 2007), which may further exacerbate caregiver stress and burden. Research data on delivery of long-term care support services to these individuals are at a nascent stage, and caregiver support services such as support groups, assisted living, home care, and respite care are rarely available within AI communities (Jervis et al., 2002). Thus, there is a need to identify services and service provision strategies that are acceptable, effective, and can be made available to AI caregivers.
Traditional medicine (defined as healing practices located within a specific cultural tradition) is widely accepted and used among AIs (Buchwald, Beals, & Manson, 2000; Rÿser, 1998) and may be linked to culturally specific practices or shared across tribal and cultural contexts. Traditional medicine is also frequently used in conjunction with conventional western medicine or with complementary and alternative medicine (CAM). For example, in a survey of 869 urban-dwelling AI primary care patients in the Pacific Northwest, 70% reported using some form of traditional medicine, and of those, 95% reported that the traditional health activities they used were helpful (Buchwald et al., 2000). More recently, in an investigation of CAM use in California, among 334 AI respondents, 13% had visited a native healer or participated in a healing ritual, 10% had seen an acupuncturist, and 49% had seen a chiropractor (Hsiao et al., 2006). Similarly, a high rate of CAM use was found in nonminority older adults in a recent survey in Minnesota, in which 63% of respondents reported some form of CAM use (Cheung, Wyman, & Halcon, 2007).
Among Indians of the Pacific Northwest, traditional medicine practitioners frequently employ hands-on healing, including energy healing and a variety of massage techniques, as well as use of herbs, drumming and singing, sweats, and the winter dance. One focus of traditional medicine is on the restoration of energy or spirit balance (Jilek, 1982). The concept of balancing energy flow and vitalizing the life force is commonly described as part of many indigenous healing systems (World Health Organization, 2001).
Touch and energy therapies have potential as a culturally congruent CAM intervention for stress reduction in AI caregivers. A growing body of research indicates that touch therapy reduces autonomic reactivity, depression, pain, and anxiety. For example, touch therapies have been effective in reducing physical and emotional stress, physical pain, and sleep difficulties for family caregivers receiving hospice services (MacDonald, 1998). Physiological studies also support the efficacy of massage and biofield touch therapies to decrease pain (Pierce, 2007), anxiety (Kim & Buschmann, 1999), and depression (Wardell & Engebretson, 2001), while improving energy (Lee et al., 2001) and sleep (Smith, Stallings, Mariner, & Burrall, 1999).
Polarity therapy (PT) is a specific type of biofield touch therapy that may be particularly acceptable and effective with AI caregivers. PT is an energy therapy taught in courses ranging from 155 to 650 hr at established training programs (Korn, 2000). The practitioner applies manual pressure (both static and pulsating) on soft tissue pressure points, against vertebral areas, and on opposing locations simultaneously (e.g., left hand on forehead and right hand on abdomen or left hand on abdomen and right hand on knee). It also includes rocking on bony or soft tissue surfaces. PT theory suggests that this “polarizes” and thus unblocks and balances the energy flow (Roscoe, Matteson, Mustian, Padmanaban, & Morrow, 2005). There is empirical support for the use of PT in other populations experiencing high degrees of stress. In a randomized controlled trial of PT with cancer patients (Roscoe et al., 2005), PT significantly reduced radiotherapy-related cancer fatigue. PT is less invasive than other CAM methods involving touch or energy medicine. Acupuncture, for example, requires needle insertion and can be painful. Massage generally requires disrobing, whereas PT uses gentle pressure and rocking with fully clothed clients. This feature makes PT more acceptable to many older adults. Finally, the types and range of touch used in PT approximate the range of biofield touch therapies used to rebalance the body and mind among various AI traditions (Jilek, 1982; Rÿser, 1998); yet, it is not associated with culturally specific healing practices that would limit its acceptance by individuals from different tribal groups.
The goal of this study was to compare a standardized 8-session PT protocol with an 8-session enhanced respite control (ERC) condition in reducing stress, depression, and anxiety and improving health, sleep, and quality of life in AI dementia family caregivers.
Methods
Participants
Forty-two AI dementia caregivers in four counties of western Washington state participated in this community-based study. An AI tribal liaison and AI clinical coordinator worked directly with tribal health programs and health fairs and by word of mouth to identify and contact potential participants.
Inclusion criteria included AI or Alaskan Natives who had been the primary caregiver of a family member with dementia for at least 6 months. They were required to be currently providing at least 4 hr of direct assistance per day, to have access to a telephone, and to plan to remain in the community for at least 6 months. Exclusion criteria were designed to identify medical conditions that would preclude the use of PT including acute infection, deep vein thrombosis, diabetic neuropathy, current substance abuse, cardiac arrhythmia, or other conditions associated with severe disability or high risk of death. The National College of Naturopathic Medicine in Portland, Oregon, provided institutional review board review and study approval. Informed consent was obtained prior to study participation. All participants who enrolled in the study received a choice of a fresh salmon or a small gift basket (value $30.00) following their participation.
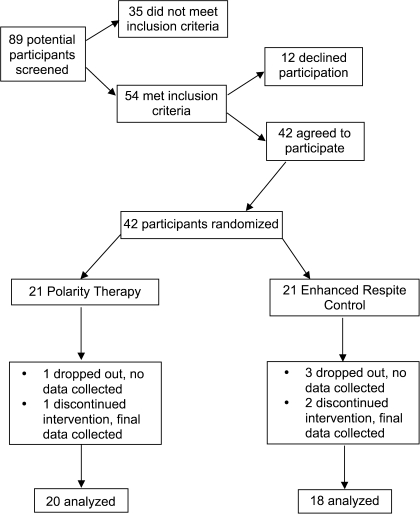
As illustrated in Figure 1, during 18 months of recruitment, 89 individuals were screened; 54 were eligible, and 42 agreed to participate and were randomized. Of the 12 people who declined to participate, six were too busy, five were not interested, and one reported no stress. Of the four people who dropped out immediately after baseline and the three participants who discontinued the intervention prior to completion, lack of time was given as the reason.
Figure 1.
Flow of participants through the trial.
Demographics of participants are presented in Table 1. Sixty percent of participants belonged to indigenous Salish tribes of the Pacific Northwest, and the rest were from other AI or Alaskan Native nations living on, near, and off reservations in urban and rural western Washington. Average age of participants was 50 years, with a range of 27–69 years. Most (90%) were women and had attended some college (71%). The ages of the care recipients ranged from 32 to 89 years with 57% aged 70 and older. The two care recipients who were younger than 35 years were diagnosed with dementia due to a stroke and to the sequelae of a failed suicide attempt. Most caregivers had provided care between 6 months and 3 years, but nine caregivers (21%) had provided care for 5 years or more. Sixty percent of caregivers reported previous experience with hands-on healing, 57% had experienced acupuncture, 55% had used herbal medicine, and 50% participated in ceremonial healing. As is common in AI populations (Manson, Beals, Klein, Croy, & AI-SUPERPFP Team, 2005), there was significant exposure to traumatic events in this sample with 37 caregivers (90%) reporting exposure to at least one traumatic event including violence, sexual or physical abuse, and/or traumatic accidents.
Table 1.
Baseline Characteristics of Participants (N = 42)
| Variable | Description | PT (n = 21), n (%) | ERC (n = 21), n (%) |
| Caregiver age (years) | <50 | 6 (29) | 12 (57) |
| >50 | 15 (71) | 9 (43) | |
| Gender | Female | 18 (86) | 20 (95) |
| Male | 3 (14) | 1 (5) | |
| Tribal affiliation | Salish | 13 (62) | 12 (57) |
| Non-Salish | 8 (38) | 9 (43) | |
| Residence | Rural | 10 (48) | 10 (48) |
| Urban | 11 (52) | 11 (52) | |
| Education | Up to high school | 6 (28) | 6 (28) |
| Up to baccalaureate | 13 (62) | 13 (62) | |
| Postbaccalaureate | 1 (5) | 2 (10) | |
| Missing | 1 (5) | 0 | |
| Relationship to care recipient | Daughtera | 13 (62) | 9 (43) |
| Wife | 3 (14) | 1 (5) | |
| Son | 3 (14) | 0 | |
| Niece | 0 | 3 (14) | |
| Sister | 0 | 2 (10) | |
| Cousin | 1 (5) | 1 (5) | |
| Other | 1 (5) | 5 (24) | |
| Care recipient’s age (years)b | <50 | 3 (14) | 1 (5) |
| 50–69 | 5 (24) | 9 (43) | |
| >70 | 13 (62) | 11 (53) | |
| Duration of care (months)c | 6–36 | 15 (71) | 11 (52) |
| 37–60 | 2 (10) | 5 (24) | |
| >60 | 4 (19) | 5 (24) | |
| History of trauma | No | 2 (10) | 3 (14) |
| Yes | 19 (90) | 17 (81) | |
| Missing | 0 | 1 (5) | |
| Type of traumad | Accident | 13 | 12 |
| Interpersonal | 17 | 14 | |
| Natural disaster | 9 | 4 | |
| Traditional medicine or CAM used | Acupuncture | 10 | 14 |
| Hands-on healing | 14 | 11 | |
| Ceremonial | 12 | 9 | |
| Energy healing | 7 | 3 | |
| Herbal medicine | 13 | 10 | |
| Other | 1 | 4 | |
| None | 1 | 1 |
Notes: CAM = complementary and alternative medicine; ERC = enhanced respite control; PT = polarity therapy.
One participant was caring for both her mother and her spouse.
Five participants were taking care of more than one family member.
One participant reported two different “duration of care” times for two family members.
Participants may report more than one type or use.
Interventions
Polarity Therapy.—
A 21-point PT protocol was developed and standardized to safely optimize reduction of sympathetic activity, promote a sense of well-being, and stimulate improvement in functional areas most affected by psychosomatic stress (Korn, Loytomaki, Hinman, & Rÿser, 2007; Korn & Rÿser, 2007). The protocol was based on the work of Stone (1986) and the American Polarity Therapy Association Standards for Practice (American Polarity Therapy Association, 1996). Trained practitioners administered the standard 21-point protocol to participants during eight 50-min sessions. The intervention was carried out at the Center for Traditional Medicine in Olympia, Washington, and at four tribal health clinics. The rooms for PT sessions were standardized to include uninterrupted quiet, a low level of light, a massage table with pillow for knee support, and a blanket for warmth.
To maintain consistent treatment implementation (Burgio et al., 2001), a therapist manual was developed with implementation and communication scripts, and comprehensive anatomy and physiology and point location charts were designed (Korn et al., 2007; Korn & Rÿser, 2007). The first author (Leslie Korn) trained and supervised six therapists in the PT protocol. All the therapists were trained massage therapists with an average of 11.8 years of massage experience. Four of the therapists were also experienced polarity practitioners with an average of 7.8 years of polarity practice. Therapist effects were examined, and there was no significant difference in outcomes among therapists. The therapist and research assistant kept process logs, and immediately after the intervention or control condition, the clinical coordinator ascertained if there were any protocol deviations.
Enhanced Respite Control.—
Control caregivers participated in eight sessions of respite, in which they were provided with a trained companion to stay at home with their care recipient, although they were free to participate in activities of their own choosing. To encourage caregivers to participate in respite, transportation, admission costs, and supplies for a choice of activities were provided. Five individuals chose music therapy, three participated in a yoga class, two swam and used the sauna at the YMCA, three attended a basket-making circle, two attended “tea and hot-tub” at a bed and breakfast, two undertook activities with friends including movies, dinners, and pedicures, and one individual gardened at home. The only activities that were precluded were any form of touch therapy.
The duration of PT sessions was 50 min, and the ERC activity ranged from 60 to 120 min. Both PT and ERC provided the same amount of time (3 hr) of paid care for the care recipient. This allowed time for transportation to and from activities. The protocols for both conditions were designed to equalize social interaction received by the groups. The same communication scripts requiring a total of 10 min of interaction were used with both the intervention and the control groups and delivered by the same therapist and research assistant, respectively. These included five questions asked just prior to and immediately following each session such as “Please tell me how you feel,” “Is there anything you wish to tell me about your experience last week?”, and “Is there anything you wish to tell me about your experience today?”
Randomization–Stratification
The study statistician randomized caregivers into PT or ERC groups. In order to ensure that conditions were balanced according to stress level (the primary outcome), randomization was carried out separately in each of two strata defined by baseline scores on the Perceived Stress Scale (PSS). The cutoff point for the high-stress group was a score of 17 or above. Following randomization of 15 participants, the statistician confirmed that the cutoff score was producing a balanced method of randomization–stratification.
Measures
Physical examinations were conducted, and self-report assessments were collected at baseline and posttreatment (following completion of all eight sessions). Caregivers were instructed not to reveal which treatment they had received; a protocol deviation log was maintained by the nurse and clinical coordinator to record if blinding was broken and in no case did that occur. Physical examinations were conducted to ensure that participants had no medical conditions that would preclude their involvement in the study and to ensure that no adverse physical effects occurred as a result of their participation. Primary outcomes were evaluated using the following measures.
Perceived Stress Scale.—
The PSS is a 10-item scale for measuring the perception of stress. The mean score for community-dwelling nonminority Whites is 12.8 and for minorities is 14.0 (Cohen & Williamson, 1988). The change in PSS from baseline to posttreatment assessment was designated in advance of the trial as the primary outcome.
Center for Epidemiological Studies–Depression Scale.—
The Center for Epidemiological Studies–Depression scale (CES-D; Radloff, 1977) is a 20-item self-report measure that assesses frequency of depressive symptoms during the past 2 weeks. Good internal consistency and reliability were found in a sample of chronically ill older AIs from the Pacific Northwest (Somervell et al., 1993).
SF-36.—
The Short Form (SF)-36 (Ware, 2000) is a widely used health-related quality-of-life questionnaire that yields a profile of scores on eight health attributes. The psychometric properties of the SF-36 have been found to be within acceptable limits with AI populations (Beals et al., 2006).
Quality of Life–AD (Caregiver Version).—
The caregiver Quality of Life–Alzheimer's disease (AD) (Logsdon, Gibbons, McCurry, & Teri, 2002) is a brief 13-item checklist that covers additional domains not addressed by the SF-36. It has been found to have good reliability and validity (Logsdon, Gibbons, McCurry, & Teri, 2005). Total scores range from 13 to 52, with higher scores indicating higher ratings of quality of life.
Pittsburgh Sleep Quality Index.—
The Pittsburgh Sleep Quality Index (PSQI) is a self-rated questionnaire that measures the quality and patterns of sleep in older adults. The PSQI has good internal reliability and validity (Buysse, Reynolds, Monk, Berman, & Kupfer, 1989).
Penn State Worry Questionnaire.—
The Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec, 1990) is a 16-item self-report measure that assesses the generality, excessiveness, and uncontrollability of worry without focusing on specific domains of worry. The reliability and validity of the PSWQ have been widely researched and appear to have sound psychometric properties (Brown, 2003).
Statistical Methods
All outcomes were analyzed on an intent-to-treat basis using data from all participants who could be assessed. Of 42 participants, 35 completed the entire course of PT or ERC and the posttreatment assessment, three dropouts did not complete their assigned treatment but did complete the posttreatment assessment (and were included in the outcome analysis), and four dropouts completed neither their assigned treatment nor the posttreatment assessment. Thus, the change in outcome measures from baseline until the end of the trial is based on 38 of 42 participants. There were no differences in baseline scores between those that did and did not complete the posttreatment assessment.
The treatment difference between PT and ERC was analyzed using t tests for the PT versus ERC difference in mean change of each outcome measure between baseline and posttreatment. We examined histograms and boxplots of each outcome measure to determine if they were reasonably consistent with a normal distribution. The distribution of the role-emotional scale from the SF-36 battery differed from normality sufficiently that we used the nonparametric Mann–Whitney test to compare the two treatment groups. Results are presented as means and standard deviations (SDs) and the statistical significance of treatment differences.
We also carried out a multivariate analysis of the treatment difference controlling for potential confounding variables. Specifically, for dependent variables, we fitted a regression model including the treatment effect (a dichotomous dummy variable) and, one at a time, each of the potential confounders: baseline value of the outcome variable, presence/absence of a history of trauma, number of trauma events, education, gender, caregiver relationship to the care recipient, tribal affiliation, and prior CAM use. If any individual confounders were statistically significant in these regression analyses, we built a final multivariate model starting from all significant predictor variables. We examined residuals from these regression analyses to determine if they were reasonably consistent with the assumption of normality.
Results
There were no significant differences on primary or secondary measures between groups at baseline. Both groups improved from baseline to posttreatment on the primary outcome measure of stress (Table 2), but the PT group improved significantly more than the ERC group (p = .01). For PT recipients, scores on the PSS declined by an average of 8.3 points (SD = 7.5), whereas scores for the ERC group declined by 2.5 points (SD = 6.2).
Table 2.
Changes in Five Self-Report Outcome Measures During a Randomized Trial of PT (T) Versus ERC (C)
| Variable | Baseline mean | PT change | ERC change | p Value |
| Perceived Stress Scale | 19.3 ± 7.2 (T); 19.1 ± 8.2 (C) | −8.3 ± 7.54 | −2.5 ± 6.2 | .01 |
| Center for Epidemiological Studies–Depression | 19.7 ± 6.4 (T); 20.0 ± 10.6 (C) | −7.9 ± 8.25 | −1.9 ± 9.5 | .045 |
| Pittsburgh Sleep Quality Index | 9.0 ± 3.2 (T); 9.3 ± 4.2 (C) | −3.1 ± 3.88 | −1.4 ± 3.2 | .16 |
| Quality of Life–AD | 33.4 ± 5.3 (T); 32.7 ± 8.1 (C) | 5.2 ± 4.66 | 3.4 ± 7.3 | .39 |
| Penn State Worry Questionnaire | 48.9 ± 18.4 (T); 45.9 ± 23.1 (C) | −18.0 ± 18.02 | −9.9 ± 17.3 | .17 |
Note: AD = Alzheimer's disease; ERC = enhanced respite control; PT = polarity therapy.
Secondary outcomes where PT yielded a statistically significant greater improvement than ERC (shown in Tables 2 and 3) included depression, bodily pain, general health, and vitality. On the CES-D, PT recipients’ depression scores improved by a mean of almost 8 points, whereas ERC recipients’ depression scores improved by 2 points (p = .045). On the SF-36 bodily pain subscale, PT recipients reported decreased pain (indicated by increased scores on the scale), whereas ERC recipients reported little change (p = .02). The SF-36 general health and vitality subscales also improved for PT compared with ERC (p = .01 and p = .03, respectively).
Table 3.
Changes in SF-36 Measures During a Randomized Trial of PT (T) Versus ERC (C)
| Variable | Baseline mean | PT change | ERC change | p Value |
| Physical functioning | 67.9 ± 27.9 (T); 62.4 ± 28.7 (C) | 1.5 ± 24.3 | 5.3 ± 25.7 | .64 |
| Role physical | 53.6 ± 42.8 (T); 58.3 ± 43.5 (C) | −28.8 ± 37.4 | −22.2 ± 26.9 | .55 |
| Bodily pain | 48.4 ± 25.6 (T); 55.0 ± 25.6 (C) | 21.3 ± 20.9 | 1.9 ± 26.3 | .02 |
| General health | 59.6 ± 21.5 (T); 60.8 ± 21.7 (C) | 17.3 ± 15.4 | −0.1 ± 23.9 | .01 |
| Vitality | 41.9 ± 21.4 (T); 37.6 ± 20.3 (C) | 25.0 ± 23.4 | 8.1 ± 23.8 | .03 |
| Social functioning | 58.9 ± 24.7 (T); 49.4 ± 26.7 (C) | 24.4 ± 25.8 | 13.2 ± 20.3 | .15 |
| Role emotional | 46.0 ± 40.1 (T); 50.8 ± 45.9 (C) | −35.0 ± 39.7 | −3.7 ± 39.4 | .03 |
| Mental health | 65.3 ± 18.9 (T); 60.6 ± 21.9 (C) | 14.2 ± 15.4 | 6.7 ± 25.2 | .27 |
| Physical component summary | 41.9 ± 8.3 (T); 42.7 ± 6.7 (C) | 2.9 ± 6.8 | −1.6 ± 9.2 | .09 |
| Mental component summary | 41.6 ± 8.6 (T); 39.4 ± 6.9 (C) | 4.9 ± 7.9 | 4.0 ± 9.1 | .76 |
Note: ERC = enhanced respite control; PT = polarity therapy.
Five outcome measures for the PT group were statistically significant. Eight outcome measures showed changes in a positive direction. The only measure on which the ERC group had a better outcome than the PT group was for the SF-36 role-emotional subscale (p = .03). The SF-36 subscale role emotional refers to “problems with work or other daily activities as a result of emotional problems” (Ware, 2000). It is possible that the role-emotional domain had a slightly better result in the respite group because the activities for the majority of the respite participants were group oriented in contrast to the dyadic relationship between therapist and intervention participant.
The multivariate analysis (Table 4) confirmed the statistically significant treatment differences in outcome variables noted earlier (p < .05 for all) and did not add any new significant outcome variables. Further, and more importantly, the mean treatment difference changed very little in any of the multivariate models from that noted in Tables 2 and 3. These confirmatory results from the multivariate analysis suggest that it is the difference in treatments and not an extraneous factor that led to the observed better outcomes with PT than with ERC.
Table 4.
Univariate and Multivariate Regression Analysis of Selected Outcome Variables (change, Week 9 − Week 1) in Relation to Treatment Effect
| Outcome | Treatment effecta | SE | p Value | Adjusted treatment effecta | SE | p Value |
| Perceived Stress Scale | −5.8 | 2.3 | .014 | −5.7 | 1.9 | .006 |
| Center for Epidemiological Studies–Depression | −6.0 | 2.9 | .045 | −6.4 | 2.5 | .015 |
| SF-36 | ||||||
| Bodily pain | 19.3 | 7.7 | .016 | 15.7 | 7.0 | .03 |
| General health | 17.4 | 6.5 | .011 | 17.1 | 5.4 | .003 |
| Vitality | 16.9 | 7.7 | .034 | 20.4 | 6.2 | .002 |
| Social functioning | 11.2 | 7.6 | .15 | 16.6 | 7.0 | .023 |
| Role emotional | −31.3 | 12.9 | .02 | −35.4 | 9.8 | .001 |
Note: a“Treatment effect” is the unadjusted regression coefficient of the treatment variable. “Adjusted treatment effect” is the coefficient of treatment from the multivariate model including treatment and potential confounding variables (see text). The baseline value of the outcome variable is the only adjustment variable included for all models, except Salish/non-Salish membership is also included for the SF-36 role-emotional outcome.
No serious adverse events were reported during the intervention or at the final physical examination. Two people reported mild muscle soreness following PT sessions.
Discussion
This randomized clinical trial compared PT, a biofield/touch therapy, with an ERC for the reduction of stress in AI dementia caregivers. The primary outcome variable, perceived stress, along with depression and pain showed a statistically significant reduction in the PT group compared with the ERC group, and general health and vitality increased significantly in PT participants compared with ERC participants. Thus, PT is an effective intervention for highly stressed AI caregivers.
In addition to the significant treatment findings, this investigation provides information about AI caregivers living in the Pacific Northwest. At baseline, almost half of the participants had PSSs greater than or equal to 20, which places them at the top of the range of perceived stress reported in other caregiving studies (de Vugt et al., 2005; Kiecolt-Glaser, Dura, Speicher, Trask, & Glaser, 1991). Almost 70% of participants scored above 16 on the CES-D, indicating significant levels of depressive symptoms. Baseline SF-36 scores were worse than those for the general population and were similar to the norms for individuals diagnosed with depressive disorder (Ware, 2000). Sleep was also significantly disrupted; the mean scores at baseline were nearly twice the cutoff score for “normal” sleep (Buysse et al., 1989). Finally, this sample reported high levels of chronic illness. At the baseline assessment, 57% of participants reported chronic headaches, 57% had arthritis, 47% had chronic heartburn, 40% had heart palpitations (those with heart disease were excluded from the study), 29% smoked cigarettes, 29% had hypertension, 21% had asthma, and 12% had early stage diabetes mellitus.
As noted earlier, stress, depression, fatigue, sleep problems, and poor health are the frequently cited problems of dementia caregivers. For AI caregivers, they appear even more common. Furthermore, these problems may filter down to the care recipient, leading to decreased capacity for continued caregiving and consequent institutionalization. Culturally acceptable caregiver interventions, such as PT, that reduce stress, depression, and pain and improve health and vitality are urgently needed.
There is a growing body of literature on the relationships between social stress (Pearlin, Schieman, Fazio, & Meersman, 2005), including discrimination based on ethnicity, socioeconomic status, and poor health outcomes (Seeman et al., 2004). Scharlach and colleagues (2006) found that AI caregivers felt that their caregiving experience was affected by experiences such as discrimination, poverty, and isolation. These experiences negatively influenced their willingness to access caregiver services. For urban and rural AIs, caregiver stress co-occurs within a social and cultural backdrop of historical trauma and intergenerational grief arising from the colonization experience. Memory and awareness of historical trauma are evident in the daily consciousness of many AIs (Jervis, 2006). Exposure to interpersonal violence and accidental trauma, which in this sample was high, is widely believed to be the sequelae of historical trauma and intergenerational grief (Evans-Campbell, 2008). Interaction between the stress of caregiving and the ongoing social stress among many AIs is an important area for future study.
Recruitment and retention are challenging in AI populations (Buchwald et al., 2006), older minorities (Levkoff & Sanchez, 2003), and minority dementia caregivers (Gallagher-Thompson, Solano, Coon, & Arean, 2003). AI populations are often small and separated by great geographical distances. Research is widely distrusted among AIs (Oberly & Macedo, 2004). In this study, we observed obstacles to recruitment and retention including significant time constraints due to multiple role responsibilities, lack of systematic diagnosis of dementia, and a small subject pool made smaller by exclusion criteria that included two major diseases common in this population: diabetic neuropathy and heart disease.
Results of this study illuminate health vulnerabilities among AI dementia caregivers and point the way to providing appropriate supports. Tribal medicine services are increasingly recognizing the role of CAM and traditional medicine services in the health care of AI communities—this study suggests that PT is an effective CAM for reducing stress (and thereby potentially improving health and well-being) of AI family caregivers. In the United States, there are more than 90,000 board-certified massage therapists, many of whom practice or can be trained in biofield touch therapy methods such as PT; thus, there already exists a cadre of potential care providers. In addition, the specific PT protocol used in this study is straightforward and easily taught to laypersons; thus, it may provide a low-cost, culturally acceptable, effective strategy for stress reduction in AI caregivers.
In the current study, we attempted to equalize social contact between the PT and ERC conditions. PT is not a social treatment per se. It is a form of bodywork or manual therapy with a focus on the human energy field. Yet, it is possible that the weekly contact with the same therapist and the feeling of empathy and care that typically accompany therapeutic touch could result in a more positive response compared with the less intense contact provided in the respite condition. Future studies are needed to compare PT to other, more intensive caregiver interventions to determine whether therapeutic touch is more beneficial than one-on-one counseling or caregiver education and support. One of the limitations of this study is that only two assessment points were collected. Future studies might address the duration of effects at different assessment points.
AIs and Alaskan Natives are a very diverse population, and healing traditions vary from place to place. Thus, the use of therapeutic touch may not be acceptable to all individuals, and additional types of caregiver support for AI caregivers should be explored. What remains certain, however, is that there is a great need for culturally appropriate, low-cost, accessible support services for AI caregivers of individuals with dementia and that this need will continue to grow in the future.
Funding
Primary funding for this research was provided by National Institutes of Health, National Center for Complementary and Alternative Medicine (NIH-NCCAM) Grant R21-AT001627 to Dr. Korn. Research Supplements to Promote Diversity in Health-Related Research supporting Dr. Gomez-Beloz and Ms. Waters were provided by the NIH-NCCAM through two separate grants: R21 AT001627. Dr. Logsdon received support from National Institute on Aging grant P50-AG05136. Additional financial support was provided by the Assured Home Health and Hospice, Centralia, Washington and the Lewis-Mason-Thurston Area Agencies on Aging, Olympia, Washington.
Acknowledgments
The authors thank Anastasia Brencick, Henry Cagey, Candace Chaney, Tracey Dickerson, Gene Hamilton, Trish Hinman, Stephen J. Korn, Natalie Metz, Connie McCloud, Rollin McCraty, Pamela Morton, Amy Robertson, David Robinson, Mary Ann Schwenka, Annie Wall, and Keith Zang for their contributions to the success of this study.
References
- American Polarity Therapy Association. Foundations of polarity therapy: Professionalism standards for practice and code of ethics. Boulder, CO: Author; 1996. [Google Scholar]
- Beals J, Welty TK, Mitchell CM, Rhoades DA, Yeh J, Henderson JA, et al. Different factor loadings for SF36: The Strong Heart Study and the National Survey of Functional Health Status. Journal of Clinical Epidemiology. 2006;59:208–215. doi: 10.1016/j.jclinepi.2005.07.010. [DOI] [PubMed] [Google Scholar]
- Belle SH, Burgio L, Burns R, Coon D, Czaja SJ, Gallagher-Thompson D, et al. Enhancing the quality of life of dementia caregivers from different ethnic or racial groups: A randomized, controlled trial. Annals of Internal Medicine. 2006;145:727–738. doi: 10.7326/0003-4819-145-10-200611210-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA. Confirmatory factor analysis of the Penn State Worry Questionnaire: Multiple factors or method effects? Behavior Research and Therapy. 2003;41:1411–1426. doi: 10.1016/s0005-7967(03)00059-7. [DOI] [PubMed] [Google Scholar]
- Buchwald D, Beals J, Manson SM. Use of traditional health practices among Native Americans in a primary care setting. Medical Care. 2000;12:1191–1199. doi: 10.1097/00005650-200012000-00006. [DOI] [PubMed] [Google Scholar]
- Buchwald D, Mendoza-Jenkins V, Croy C, McGough H, Bezdek M, Spicer P. Attitudes of urban American Indians and Alaska Natives regarding participation in research. Journal of General Internal Medicine. 2006;21:648–651. doi: 10.1111/j.1525-1497.2006.00449.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgio L, Corcoran M, Lichstein KL, Nichols L, Czaja S, Gallagher-Thompson D, et al. Judging outcomes in psychosocial interventions for dementia caregivers: The problem of treatment implementation. Gerontologist. 2001;41:481–489. doi: 10.1093/geront/41.4.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Cheung CK, Wyman JF, Halcon LL. Use of complementary and alternative therapies in community-dwelling older adults. Journal of Alternative and Complementary Medicine. 2007;13:997–1006. doi: 10.1089/acm.2007.0527. [DOI] [PubMed] [Google Scholar]
- Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The social psychology of health. Newbury Park, CA: Sage; 1988. pp. 31–67. [Google Scholar]
- Covinsky KE, Newcomer R, Fox P, Wood J, Sands L, Dane K, et al. Patient and caregiver characteristics associated with depression in caregivers of patients with dementia. Journal of General Internal Medicine. 2003;18:1006–1014. doi: 10.1111/j.1525-1497.2003.30103.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health and Human Services, Office for American Indian Alaskan Native and Native Hawaiian Programs. Native elder population, 1990 (based on Bureau of the Census Count) Washington, DC: US Administration on Aging; 1997. [Google Scholar]
- de Vugt M, Nicolson N, Aalten P, Lousberg R, Jille J, Verhey FR. Behavioral problems in dementia patients and salivary cortisol patterns in caregivers. Journal of Neuropsychiatry Clinical Neurosciences. 2005;17:201–207. doi: 10.1176/jnp.17.2.201. [DOI] [PubMed] [Google Scholar]
- Dilworth-Anderson P, Williams IC, Gibson BE. Issues of race, ethnicity, and culture in caregiving research: A 20-year review (1980–2000) Gerontologist. 2002;42:237–272. doi: 10.1093/geront/42.2.237. [DOI] [PubMed] [Google Scholar]
- Evans-Campbell T. Historical trauma in American Indian/Native Alaska communities: A multilevel framework for exploring impacts on individuals, families, and communities. Journal of Interpersonal Violence. 2008;23:316–338. doi: 10.1177/0886260507312290. [DOI] [PubMed] [Google Scholar]
- Gallagher-Thompson D, Solano N, Coon D, Arean P. Recruitment and retention of Latino dementia family caregivers. Gerontologist. 2003;43:45–51. doi: 10.1093/geront/43.1.45. [DOI] [PubMed] [Google Scholar]
- Goins RT, Moss M, Buchwald D, Guralnik JM. Disability among older American Indians and Alaska Natives: An analysis of the 2000 Census public use microdata sample. Gerontologist. 2007;47:690–696. doi: 10.1093/geront/47.5.690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsiao A, Wong MD, Goldstein MS, Yu H, Anderson RM, Brown ER, et al. Variation in complementary and alternative medicine (CAM) use across racial/ethnic groups and the development of ethnic-specific measures of CAM use. Journal of Alternative and Complementary Medicine. 2006;12:281–290. doi: 10.1089/acm.2006.12.281. [DOI] [PubMed] [Google Scholar]
- Jervis LL, Beals J, Croy CD, Klein SA, Manson SM, AI-SUPERPFP Team Historical consciousness among two American Indian tribes. American Behavioral Scientist. 2006;50:526–549. [Google Scholar]
- Jervis LL, Jackson MY, Manson SM. Need for, availability of, and barriers to the provision of long-term care services for older American Indians. Journal of Cross-Cultural Gerontology. 2002;17:295–311. doi: 10.1023/a:1023027102700. [DOI] [PubMed] [Google Scholar]
- Jervis LL, Manson SM. American Indians/Alaska Natives and dementia. Alzheimer Disease and Associated Disorders. 2002;16(Suppl. 2):S89–S95. doi: 10.1097/00002093-200200002-00011. [DOI] [PubMed] [Google Scholar]
- Jilek WG. Indian healing: Shamanic ceremonialism in the Pacific Northwest today. Blaine, WA: Hancock House; 1982. [Google Scholar]
- John R, Hennessy CH, Dyeson TB, Garrett MD. Toward the conceptualization and measurement of caregiver burden among Pueblo Indian family caregivers. Gerontologist. 2001;41:210–219. doi: 10.1093/geront/41.2.210. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Dura JR, Speicher CE, Trask OJ, Glaser R. Spousal caregivers of dementia victims: Longitudinal changes in immunity and health. Psychosomatic Medicine. 1991;53:345–362. doi: 10.1097/00006842-199107000-00001. [DOI] [PubMed] [Google Scholar]
- Kim EJ, Buschmann MT. The effect of expressive physical touch on patients with dementia. International Journal of Nursing Studies. 1999;36:235–243. doi: 10.1016/s0020-7489(99)00019-x. [DOI] [PubMed] [Google Scholar]
- Korn L. Polarity therapy. In: Novey DW, editor. Clinician's complete reference to complementary and alternative medicine. Philadelphia: Mosby; 2000. pp. 423–434. [Google Scholar]
- Korn L, Loytomaki S, Hinman T, Rÿser R. Polarity therapy protocol for dementia caregivers—Part 2. Journal of Bodywork and Movement Therapies. 2007;11:244–259. [Google Scholar]
- Korn L, Rÿser R. Designing a polarity therapy protocol: Bridging holistic, cultural and biomedical models of research. Journal of Bodywork and Movement Therapies. 2007;11:129–140. [Google Scholar]
- Lee MS, Yang KK, Hoh HJ, Kim HW, Ryo IT, Lee HS. Qi therapy as an intervention to reduce chronic pain and to enhance mood in elderly subjects: A pilot study. American Journal of Chinese Medicine. 2001;29:237–245. doi: 10.1142/S0192415X01000277. [DOI] [PubMed] [Google Scholar]
- Levkoff S, Sanchez H. Lessons learned about minority recruitment and retention from the centers on minority aging and health promotion. Gerontologist. 2003;43:18–26. doi: 10.1093/geront/43.1.18. [DOI] [PubMed] [Google Scholar]
- Li J, Cowden LG, King JD, Briles DA, Schroeder HW, Stevens AB, et al. Effects of chronic stress and interleukin-10 gene polymorphisms on antibody response to tetanus vaccine in family caregivers of patients with Alzheimer's disease. Psychosomatic Medicine. 2007;9:551–559. doi: 10.1097/PSY.0b013e3180cc2c61. [DOI] [PubMed] [Google Scholar]
- Logsdon RG, Gibbons LE, McCurry SM, Teri L. Assessing quality of life in older adults with cognitive impairment. Psychosomatic Medicine. 2002;64:510–519. doi: 10.1097/00006842-200205000-00016. [DOI] [PubMed] [Google Scholar]
- Logsdon RG, Gibbons LE, McCurry SM, Teri L. Assessing changes in quality of life in Alzheimer's disease. In: Vellas B, Grundman M, Feldman H, Fitten LJ, Winblad B, Giacobini E, editors. Research and practice in Alzheimer's disease and cognitive decline. (Vol. 10. New York: Springer; 2005. pp. 221–225. [Google Scholar]
- MacDonald G. Massage as a respite intervention for primary caregivers. American Journal of Hospital and Palliative Care. 1998;15:43–47. doi: 10.1177/104990919801500109. [DOI] [PubMed] [Google Scholar]
- Manson SM, Beals J, Klein SA, Croy CD AI-SUPERPFP Team. Social epidemiology of trauma among 2 American Indian reservation populations. American Journal of Public Health. 2005;95:851–859. doi: 10.2105/AJPH.2004.054171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behavioral Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Mittelman MS, Ferris SH, Steinberg G, Shulman E, Mackell JA, Ambinder A, et al. An intervention that delays institutionalization of Alzheimer's disease patients: Treatment of spouse-caregivers. Gerontologist. 1993;33:730–740. doi: 10.1093/geront/33.6.730. [DOI] [PubMed] [Google Scholar]
- Oberly J, Macedo J. The R word in Indian country: Culturally appropriate commercial tobacco-use research strategies. Health Promotion Practice. 2004;5:355–361. doi: 10.1177/1524839904267391. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Schieman S, Fazio E, Meersman S. Stress, health, and the life course: Some conceptual specifications. Journal of Health and Social Behavior. 2005;46:205–219. doi: 10.1177/002214650504600206. [DOI] [PubMed] [Google Scholar]
- Pierce B. The use of biofield therapies in cancer care. Clinical Journal of Oncology Nursing. 2007;11:253–258. doi: 10.1188/07.CJON.253-258. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Roscoe J, Matteson SE, Mustian KM, Padmanaban D, Morrow GR. Treatment of radiotherapy-induced fatigue through a nonpharmacological approach. Integrative Cancer Therapies. 2005;4:8–13. doi: 10.1177/1534735404273726. [DOI] [PubMed] [Google Scholar]
- Rÿser RC. Observations on self and knowing. In: Wautischer H, editor. Tribal epistemologies. Aldershot, UK: Ashgate; 1998. pp. 17–29. [Google Scholar]
- Scharlach AE, Kellam R, Ong N, Baskin A, Goldstein C, Fox P. Cultural attitudes and caregiver service use: Lessons from focus groups with racially and ethnically diverse family caregivers. Journal of Gerontological Social Work. 2006;47:133–155. doi: 10.1300/J083v47n01_09. [DOI] [PubMed] [Google Scholar]
- Schulz RC, Beach SR. Caregiving as a risk factor for mortality: The Caregiver Health Effects Study. Journal of the American Medical Association. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Crimmins E, Huang MH, Singer B, Bucur A, Gruenewald T, et al. Cumulative biological risk and socio-economic differences in mortality: MacArthur studies of successful aging. Social Science & Medicine. 2004;58:1985–1997. doi: 10.1016/S0277-9536(03)00402-7. [DOI] [PubMed] [Google Scholar]
- Smith M, Stallings MN, Mariner S, Burrall M. Benefits of massage therapy for hospitalized patients: A descriptive and qualitative evaluation. Alternative Therapies in Health and Medicine. 1999;5:64–71. [PubMed] [Google Scholar]
- Somervell PD, Beals J, et al. Criterion validity of the Center for Epidemiologic Studies Depression Scale in a population sample from an American Indian village. Psychiatry Research. 1993;47:255–266. doi: 10.1016/0165-1781(93)90083-s. [DOI] [PubMed] [Google Scholar]
- Stone R. Sebastopol, CA: CRCS; 1986. Polarity therapy: The complete collected works on this revolutionary healing art by the originator of the system. [Google Scholar]
- Wardell DW, Engebretson J. Biological correlates of Reiki touch healing. Journal of Advanced Nursing. 2001;33:439–445. doi: 10.1046/j.1365-2648.2001.01691.x. [DOI] [PubMed] [Google Scholar]
- Ware JE. SF-36 Health survey update. Spine. 2000;25:3130–3139. doi: 10.1097/00007632-200012150-00008. [DOI] [PubMed] [Google Scholar]
- World Health Organization. WHO legal status of traditional medicine and complementary alternative medicine. Geneva, Switzerland: Author; 2001. [Google Scholar]