Abstract
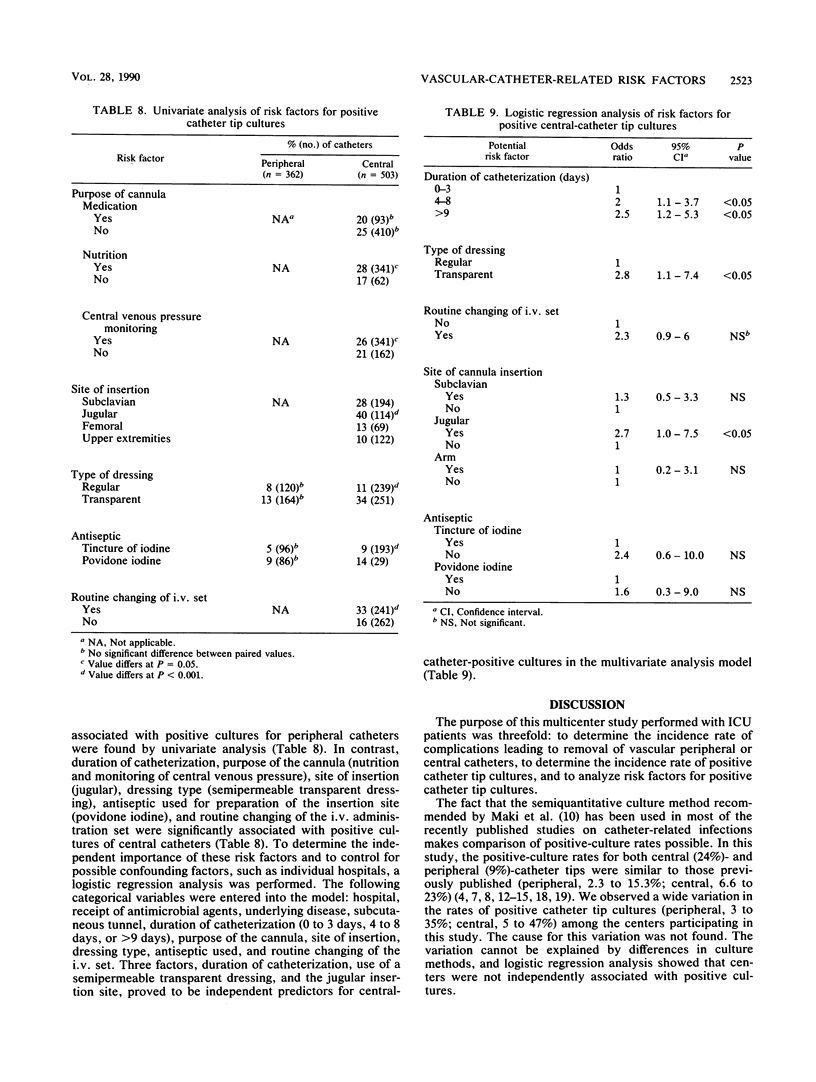
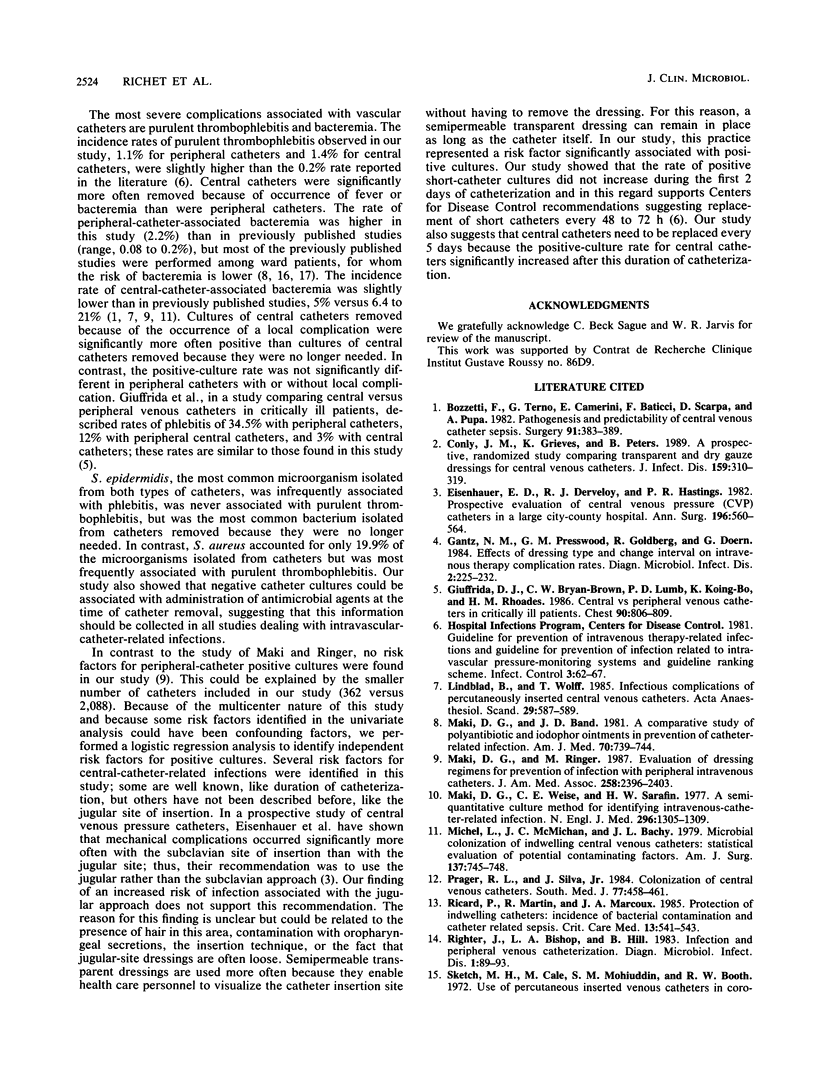
To determine the incidence rate of complications associated with vascular catheters in intensive care unit patients and to analyze risk factors for a positive vascular culture, we performed a multicenter study of intensive care unit patients at eight French hospitals. During the study period, 865 intravenous catheters were inserted in 566 patients; 362 (41.8%) were peripheral catheters, and 503 (58.2%) were central catheters. Local complications (i.e., infiltration) occurred significantly more often with peripheral than with central catheters (P less than 0.001); in contrast, fever and bacteremia were significantly more often associated with central than with peripheral catheters (P less than 0.01 and P less than 0.05, respectively). The culture of the vascular-catheter tip was positive for 24% of central catheters (32 of 1,000 catheters days) and for 9% of peripheral catheters (21 of 1,000 catheters days). Staphylococcus epidermidis was the most common microorganism isolated from both peripheral and central catheters, followed by Staphylococcus aureus and Pseudomonas aeruginosa. No significant risk factor associated with positive cultures for peripheral catheters was found by univariate analysis. In contrast, the purpose of the cannula (nutrition and monitoring of central venous pressure), the insertion site (jugular), the dressing type (semipermeable transparent dressing), the antiseptic used to prepare the insertion site (povidone iodine), and routine changing of the intravenous administration set were significantly associated with positive cultures of central catheters. Three factors, duration of catheterization, use of a semipermeable transparent dressing, and the jugular insertion site, were found to be independently associated with positive cultures of central catheters by multivariate analysis.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bozzetti F., Terno G., Camerini E., Baticci F., Scarpa D., Pupa A. Pathogenesis and predictability of central venous catheter sepsis. Surgery. 1982 Apr;91(4):383–389. [PubMed] [Google Scholar]
- Conly J. M., Grieves K., Peters B. A prospective, randomized study comparing transparent and dry gauze dressings for central venous catheters. J Infect Dis. 1989 Feb;159(2):310–319. doi: 10.1093/infdis/159.2.310. [DOI] [PubMed] [Google Scholar]
- Eisenhauer E. D., Derveloy R. J., Hastings P. R. Prospective evaluation of central venous pressure (CVP) catheters in a large city-county hospital. Ann Surg. 1982 Nov;196(5):560–564. doi: 10.1097/00000658-198211000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giuffrida D. J., Bryan-Brown C. W., Lumb P. D., Kwun K. B., Rhoades H. M. Central vs peripheral venous catheters in critically ill patients. Chest. 1986 Dec;90(6):806–809. doi: 10.1378/chest.90.6.806. [DOI] [PubMed] [Google Scholar]
- Lindblad B., Wolff T. Infectious complications of percutaneously inserted central venous catheters. Acta Anaesthesiol Scand. 1985 Aug;29(6):587–589. doi: 10.1111/j.1399-6576.1985.tb02259.x. [DOI] [PubMed] [Google Scholar]
- Maki D. G., Band J. D. A comparative study of polyantibiotic and iodophor ointments in prevention of vascular catheter-related infection. Am J Med. 1981 Mar;70(3):739–744. doi: 10.1016/0002-9343(81)90605-7. [DOI] [PubMed] [Google Scholar]
- Maki D. G., Ringer M. Evaluation of dressing regimens for prevention of infection with peripheral intravenous catheters. Gauze, a transparent polyurethane dressing, and an iodophor-transparent dressing. JAMA. 1987 Nov 6;258(17):2396–2403. [PubMed] [Google Scholar]
- Maki D. G., Weise C. E., Sarafin H. W. A semiquantitative culture method for identifying intravenous-catheter-related infection. N Engl J Med. 1977 Jun 9;296(23):1305–1309. doi: 10.1056/NEJM197706092962301. [DOI] [PubMed] [Google Scholar]
- Michel L., McMichan J. C., Bachy J. L. Microbial colonization of indwelling central venous catheters: statistical evaluation of potential contaminating factors. Am J Surg. 1979 Jun;137(6):745–748. doi: 10.1016/0002-9610(79)90085-0. [DOI] [PubMed] [Google Scholar]
- Prager R. L., Silva J., Jr Colonization of central venous catheters. South Med J. 1984 Apr;77(4):458–461. doi: 10.1097/00007611-198404000-00012. [DOI] [PubMed] [Google Scholar]
- Ricard P., Martin R., Marcoux J. A. Protection of indwelling vascular catheters: incidence of bacterial contamination and catheter-related sepsis. Crit Care Med. 1985 Jul;13(7):541–543. doi: 10.1097/00003246-198507000-00006. [DOI] [PubMed] [Google Scholar]
- Righter J., Bishop L. A., Hill B. Infection and peripheral venous catheterization. Diagn Microbiol Infect Dis. 1983 Jun;1(2):89–93. doi: 10.1016/0732-8893(83)90037-8. [DOI] [PubMed] [Google Scholar]
- Sketch M. H., Cale M., Mohiuddin S. M., Booth R. W. Use of percutaneously inserted venous catheters in coronary care units. Chest. 1972 Dec;62(6):684–689. doi: 10.1378/chest.62.6.684. [DOI] [PubMed] [Google Scholar]
- Tager I. B., Ginsberg M. B., Ellis S. E., Walsh N. E., Dupont I., Simchen E., Faich G. A. An epidemiologic study of the risks associated with peripheral intravenous catheters. Am J Epidemiol. 1983 Dec;118(6):839–851. doi: 10.1093/oxfordjournals.aje.a113702. [DOI] [PubMed] [Google Scholar]
- Tomford J. W., Hershey C. O., McLaren C. E., Porter D. K., Cohen D. I. Intravenous therapy team and peripheral venous catheter-associated complications. A prospective controlled study. Arch Intern Med. 1984 Jun;144(6):1191–1194. [PubMed] [Google Scholar]
- Tully J. L., Friedland G. H., Baldini L. M., Goldmann D. A. Complications of intravenous therapy with steel needles and Teflon catheters. A comparative study. Am J Med. 1981 Mar;70(3):702–706. doi: 10.1016/0002-9343(81)90600-8. [DOI] [PubMed] [Google Scholar]
- Wilkins E. G., Manning D., Roberts C., Davidson D. C. Quantitative bacteriology of peripheral venous cannulae in neonates. J Hosp Infect. 1985 Jun;6(2):209–217. [PubMed] [Google Scholar]


