Abstract
Jejunoileal bypass (JIB), popular in the 1960s and 1970s, had remarkable success in achieving weight loss by creating a surgical short bowel syndrome. Our patient had an unusual case of liver disease and provided no history of prior bariatric surgery. Later, it was recognized that he had a JIB in the 1970s, which was also responsible for the gamut of his illnesses. Patients with JIB are often not recognized, as they died of complications, or underwent reversal of their surgery or a liver-kidney transplant. Early identification with prompt reversal, and the recognition and treatment of the life-threatening consequences play a critical role in the management of such patients.
Keywords: Jejunoileal bypass, Bariatric surgery, Weight loss, Obesity, Morbid obesity
INTRODUCTION
Bariatric surgery is one of the few proven methods that cause durable weight loss. Failure of conservative means of producing permanent weight reduction in patients with morbid obesity, led to the introduction of operative approaches, such as jejunoileal bypass (JIB), which became popular in the late 1960s and early 1970s[1].
At that time, JIB was the most effective surgical intervention for achieving and maintaining weight loss. Typically, 35 centimeters of proximal jejunum was anastamosed, end-to-side or end-to-end, to the terminal 10 centimeters of ileum[2] (Figure 1). It was presumed that patients undergoing this procedure would experience continued hyperphagia, but would accomplish weight loss due to malabsorption[3]. As a result of JIB, patients whose preoperative weight was over 157 kg lost a mean of 58 kg at the end of 1 year[2].
Figure 1.

Jejunoileal bypass. A surgical short bowel syndrome created by bypassing more than 90% of the functioning small intestine.
However, JIB surgery has long been abandoned as a method of weight reduction surgery because of serious short and long-term complications. The number of patients who currently retain a jejunoileal bypass is small, as most patients have died or undergone reversal of their operation or conversion to a different bariatric procedure[3]. Recognition of previous JIB and understanding of its metabolic consequences are essential in the proper management of these patients.
CASE REPORT
A 64-year-old male was admitted on a regular basis for tense ascites (requiring serial large volume paracentesis) attributed to underlying advanced liver disease of unclear etiology. It was presumed to be the result of steatohepatitis from nonalcoholic fatty liver disease and/or chronic hepatic congestion due to decreased cardiac function.
The patient had a prior history of morbid obesity (191 kg, BMI 62) and cholecystectomy. His physical examination was remarkable for jaundice, abdominal ascites, spider angioma in the upper chest, gynecomastia and splenomegaly.
He had numerous other medical problems including multiple kidney stones with three previous lithotripsy interventions, progressive kidney disease requiring hemodialysis, a 30-year history of intermittent loose stools, arthritis, fatigue, paresthesias, progressive loss of night vision, joint pains, slurred speech, incoordination and weakness.
On further questioning, the patient and family revealed that he had “weight loss surgery” in the 1970s at another facility. However, an upper endoscopy showed an intact pylorus, which raised suspicion of possible previous JIB surgery. His archived medical records were then obtained and it revealed that the patient indeed had a jejunoileal bypass performed in 1974.
Initial laboratory evaluation is noted in Table 1. Further evaluation revealed deficiency of all fat-soluble vitamins. The markers of other causes of chronic liver disease (viral hepatitis B and C, antinuclear antibody, anti-smooth muscle antibody, anti-mitochondrial antibody, ceruloplasmin, iron and ferritin) were negative. Stool studies showed findings consistent with steatorrhea. Computed tomography imaging of his abdomen revealed nephrolithiasis, pneumatosis intestinalis, a shrunken and nodular liver with abdominal ascites, and osteopenia (Figure 2). Upper endoscopy, as in Figure 3, revealed esophageal varices, portal hypertensive gastropathy and no evidence of prior gastric bypass.
Table 1.
Laboratory investigations
| BUN/Creatinine (normal = 8-26/0.9-1.3) | 34/8.2 |
| Albumin (normal = 3.5-5.0) | 1.9 |
| Prothrombin time/INR (normal = 11.9-14.3/< 1.0) | 25.3/2.4 |
| ALT/AST (normal = 15-41/14-63) | 45/41 |
| Platelet count (normal = 140-400) | 129 |
| Serum albumin ascites gradient | 2.3 |
| Hepatitis profile (A, B, C) | Negative |
BUN: Blood urea nitrogen; INR: International normalized ratio; ALT: Alanine aminotransferase; AST: Aspartate aminotransferase.
Figure 2.
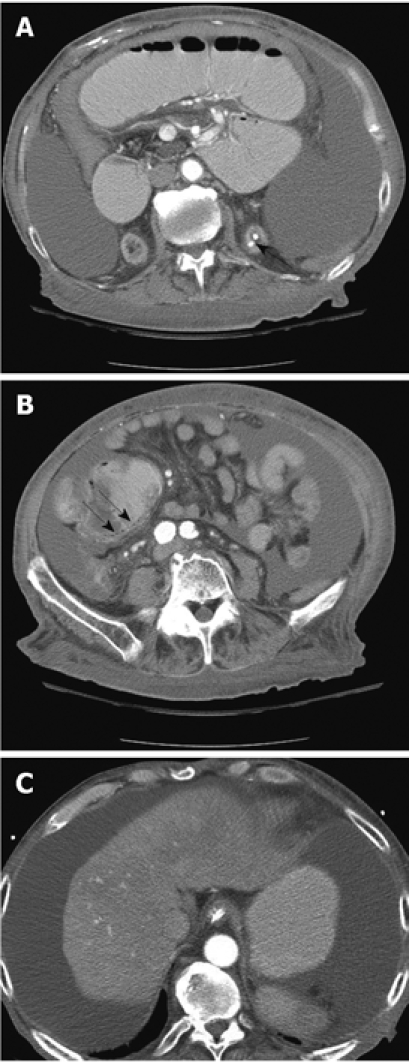
CT scan of the abdomen. showing stones in the left kidney (A, arrow), pneumatosis intestinalis (B, arrow) and shrunken nodular liver with abdominal ascites (C).
Figure 3.
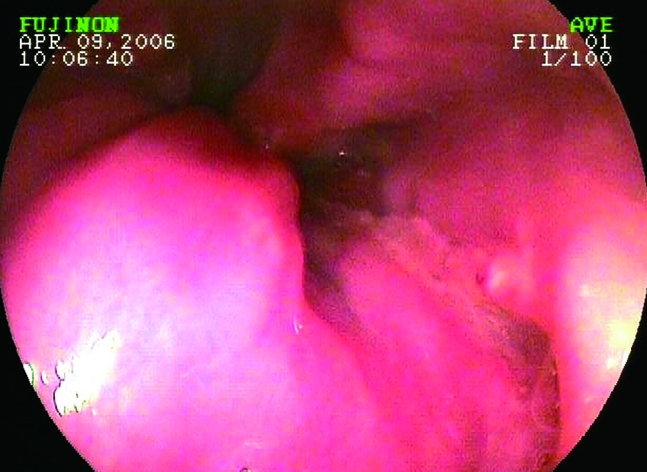
Upper endoscopy showing grade I esophageal varices, as a result of portal hypertension.
He underwent a transjugular liver biopsy that showed portal fibrosis (stage 2, grade 1) with specimen fragmentation. A repeat transjugular liver biopsy with hepatic hemodynamic measurements was performed, with a hepatic portal venous gradient at 7 mmHg (normal, 1-4 mmHg), the wedge pressure was 23 (normal, 4-13 mmHg) and the hepatic vein pressure was 16 mmHg (normal, 2-10 mmHg) - findings consistent with portal hypertension.
The patient declined reversal of JIB and did not wish evaluation for liver-kidney transplantation. He is currently being managed symptomatically by hospice care.
The complications of JIB are summarized in Table 2 above[4].
Table 2.
Complications of jejunoileal bypass
| Problem | Mechanism | Manifestations in this patient |
| Steatohepatitis Possible cirrhosis | Amino acid deficiency | Advanced liver disease with portal hypertension |
| Renal oxalosis | Excess oxalate absorption; Oxalate not bound by calcium | Multiple kidney stones and three previous lithotripsy interventions; Progressive kidney disease due to suspected oxalate nephropathy requiring lifelong hemodialysis |
| Fat soluble vitamin deficiency | Malabsorption; Steatorrhea | Serum levels: |
| Vitamin A = 17 (360-200 mg/L) | ||
| Vitamin D ≤ 10 (22-67 pg/mL) | ||
| Vitamin E = 3 (5.5-17.0 mg/L) | ||
| Vitamin K ≤ 0.03 (0.1-.2 ng/mL) | ||
| Gallstones | Bile acid loss; Mobilization of cholesterol | Previous cholecystectomy for symptomatic cholelithiasis |
| Enteritis | Bacterial overgrowth | 30 years of diarrhea and steatorrhea Pneumatosis intestinalis |
| Arthritis | Bacterial toxin; Autoimmune | Bilateral knee and shoulder pain |
| Fatigue syndrome | Vitamin deficiency; Multifactorial | Marked fatigue, bed-ridden status |
| Bypass encephalopathy | Possible deficiency; Possible D-lactic acid deficiency | Slurred speech, incoordination and weakness |
| Bypass dermatitis | Possible antigen-antibody complex (enteric bacteria) | Cutaneous urticarial rash |
CONCLUSION
Although jejunoileal bypass was effective and reliable, it was associated with severe complications such as renal failure (37%), diarrhea (29%) and consequent electrolyte imbalances, calcium oxalate nephrolithiasis (29%), liver disease (10%), fat-soluble vitamin deficiencies, malnutrition and death[5]. The most severe early complication of JIB was acute liver failure (7%)[5]. Our patient exhibited nearly all of the known metabolic complications described in the literature (Table 2).
Of the various types of bariatric procedures, JIB is particularly devastating because of its dramatic complications, and is no longer used for the management of morbid obesity. A number of studies[6–8] highlighted the high complication rates even after a decade and sometimes lifelong, difficulty maintaining satisfactory follow-up and the need for frequent revision surgery making it an unacceptable procedure performed remotely on any major scale.
Today, this procedure is a formidable diagnostic challenge because it was a surgery of the olden days (1960s and 1970s), old records may not be available and upper endoscopy may be essentially normal. Most patients have either died or had conversion to a different bariatric procedure. The importance lies in early identification based on clinical history, with prompt reversal and the recognition and treatment of the life-threatening metabolic consequences.
Footnotes
Peer reviewers: Robert JL Fraser, Associate Professor, Investigations and Procedures Unit, Repatriation General Hospital, Daw Park, Australia; Frank I Tovey, OBE, ChM, FRCS, Honorary Research Fellow, Department of Surgery, University College London, London, United Kingdom
S- Editor Tian L L- Editor Cant MR E- Editor Yin DH
References
- 1.Griffen WO Jr, Bivins BA, Bell RM. The decline and fall of the jejunoileal bypass. Surg Gynecol Obstet. 1983;157:301–308. [PubMed] [Google Scholar]
- 2.Griffen WO Jr, Young VL, Stevenson CC. A prospective comparison of gastric and jejunoileal bypass procedures for morbid obesity. Ann Surg. 1977;186:500–509. doi: 10.1097/00000658-197710000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Elder KA, Wolfe BM. Bariatric surgery: a review of procedures and outcomes. Gastroenterology. 2007;132:2253–2271. doi: 10.1053/j.gastro.2007.03.057. [DOI] [PubMed] [Google Scholar]
- 4.Faloon WW. Surgical Treatment of Morbid Obesity. In: JE Berk, WS Haubrich, MH Kaiser, JLA Roth, F Schaffner, et al., editors. Bockus Gastroenterology. Volume 5. 4th edition. W.B. Saunders Company: Philadelphia; 1985. pp. 4390–4399. [Google Scholar]
- 5.Requarth JA, Burchard KW, Colacchio TA, Stukel TA, Mott LA, Greenberg ER, Weismann RE. Long-term morbidity following jejunoileal bypass. The continuing potential need for surgical reversal. Arch Surg. 1995;130:318–325. doi: 10.1001/archsurg.1995.01430030088018. [DOI] [PubMed] [Google Scholar]
- 6.Halverson JD, Wise L, Wazna MF, Ballinger WF. Jejunoileal bypass for morbid obesity. A critical appraisal. Am J Med. 1978;64:461–475. doi: 10.1016/0002-9343(78)90233-4. [DOI] [PubMed] [Google Scholar]
- 7.Hocking MP, Duerson MC, O'Leary JP, Woodward ER. Jejunoileal bypass for morbid obesity. Late follow-up in 100 cases. N Engl J Med. 1983;308:995–999. doi: 10.1056/NEJM198304283081703. [DOI] [PubMed] [Google Scholar]
- 8.McFarland RJ, Gazet JC, Pilkington TR. A 13-year review of jejunoileal bypass. Br J Surg. 1985;72:81–87. doi: 10.1002/bjs.1800720202. [DOI] [PubMed] [Google Scholar]


