Abstract
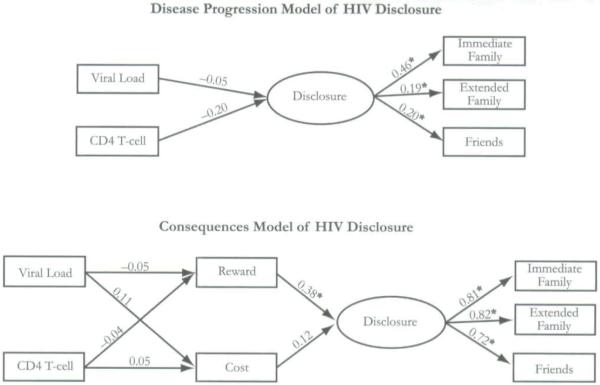
The purpose of this study was to evaluate the applicability of two theories of HIV disclosure previously tested with men. Participants included 125 HIV-positive women enrolled in a larger, longitudinal study of HIV disclosure and mental health. Structural equation modeling was used to analyze the proposed theoretical models. The disease progression model contained two single-indicator exogenous variables (disease progression) and one endogenous latent variable (disclosure).The original consequences model contained two single-indicator exogenous variables (disease progression), two single-indicator endogenous variables (consequences), and one endogenous latent variable (disclosure).The revised consequences model contained two single-indicator exogenous variables (consequences) and one endogenous latent variable (disclosure).The results of this study support the revised consequences theory and an earlier claim that disease progression may not be a direct predictor of HIV disclosure. This suggests that women may evaluate the consequences of disclosure to family and friends, particularly the reward, before the disclosure occurs.
Keywords: consequences, disclosure, disease progression, HIV-positive women
Although men constitute a majority of AIDS and HIV infection cases in the United States, the Centers for Disease Control and Prevention (CDC) reported cumulative estimates of 181,769 cases of AIDS and 73,692 cases of HIV infection in women as of December 2005 (CDC, 2005) .These figures represent significant increases of 28 percent and 83 percent, respectively, from 1999. As increasing numbers of women manage living with HIV infection and AIDS, the outlook for treatment and survival is rapidly changing. In this respect, HIV has become a disease to live with rather than to die from (Rosenberg, 1995). Nevertheless, HIV infection still presents an emotionally challenging situation for women. Several studies have demonstrated rates of clinically significant anxiety and depression ranging from 30 percent to 40 percent in women living with HIV (Kaplan, Marks, & Mertens, 1997; Miles, Burchinal, Holditch-Davis, Wasilewski, & Christian, 1997).
One strategy for women living with HIV to reduce emotional burdens is to disclose their serostatus and to access necessary social support. Rates of disclosure by women to family members, friends, and partners generally mirror those of men. In one of the first studies of disclosure among women (N = 65), Simoni et al. (1995) reported that rates of disclosure by women to friends (78 percent) surpassed all other family targets, including mothers (59 percent) and sisters (54 percent). In this study female family members were more likely than were male family members to be told. In addition, nuclear family members were more likely than were extended family to be informed. In a more recent study ot men and women (N = 331), researchers found that 85 percent of the women in the study had disclosed their HIV status to their mothers, and 86 percent had told their friends of an HIV diagnosis (Kalichman, DiMarco, Austin, Luke, & DiFonzo,2003).
Two additional studies by Sowell and colleagues (Sowell et al., 1997; Sowell, Seals, Phillips, & Julious, 2003) found similar disclosure patterns among women.The authors reported that between 65 percent (Sowell et al., 1997) and 60 percent (Sowell et al., 2003) of women reported telling both parents, whereas 22 percent and 21 percent, respectively, reported telling neither parent. Furthermore, between 51 percent (Sowell et al., 1997) and 61 percent (Sowell et al., 2003) reported telling all brothers and sisters. It is interesting to note that disclosure to close friends was reported at lower rates, with between 59 percent (Sowell et al., 1997) and 64 percent (Sowell et al., 2003) of women in their studies having reported telling all or some of their close friends.
THEORIES OF HIV DISCLOSURE
Disease Progression Theory
According to the disease progression theory, individuals disclose their HIV diagnoses as they become symptomatic. It is theorized then that as HIV progresses to AIDS, individuals can no longer keep their HIV status a secret (Babcock, 1998; Kalichman, 1998). Disease progression often results in hospitalizations and physical deterioration, which, in some cases, mandates individuals to explain their illness (Crandall & Coleman, 1992; Kalichman, 1998). Not only would hospitalization require explanation, but if death is imminent, or if individuals fear that they will need additional assistance to manage their illness, they may disclose as a means of accessing additional needed resources (Holt et al., 1998). Conversely, delaying disclosure may be a way to normalize one’s life and to protect others from pain (Babcock, 1998). The relationship between disease progression and disclosure in men has been substantiated in numerous studies that have used various indices of disease progression (Hays et al., 1993; Marks, Bundek, et al., 1992; Marks, Richardson, Ruiz, & Maldonado, 1992; Mason, Marks, Simoni, Ruiz, & Richardson, 1995).
Differences in rates of disclosure by disease progression were discovered in one study. In that study symptomatic women were least likely to disclose to sexual partners, followed by women with AIDS, and then by symptomatic women (Sowell et al., 1997). Despite medical advances for most women, disease progression is still closely hnked with variables such as viral load (CD4T-cell count) and may suggest that disclosure is a difficult event necessitating extensive personal adjustment.
Consequence Theory
The consequence theory of HIV disclosure suggests that disease progression influences disclosure through individuals’ perception of the consequences anticipated as a result of disclosure (Serovich, 2001). That is, as the disease progresses the need to evaluate the consequences of disclosure becomes more pronounced. People with HIV are likely to disclose their status to significant others and sexual partners once the rewards for disclosing outweigh the associated costs. For HIV-positive women, costs for disclosing their serostatus are potentially substantial. Sharing an HIV-positive diagnosis can provoke feelings of anxiety and threats to personal well-being. Women have reported avoiding the disclosure of their HIV-positive status because of violence (Gielen, O’Campo, Faden, & Eke, 1995; Kimberly, Serovich, & Greene, 1995), stigma,parental worrying,parental ignorance and rejection (Jenkins & Galindo, 1995; Kimberly et al.), loss of respect, and discrimination (Coleman, 1994).
Rewards or positive outcomes of disclosing are also numerous. Disclosing an HIV diagnosis can result in the acquisition of emotional, physical, and social resources. These resources may include assistance with home-related chores and errands, assistance with health and child care, housing, medical attention, and the provision of medical information. Emotional benefits include the acquisition of social support, relief from sharing a burdensome secret, and the intrinsic reward of educating or enlightening others about HIV Furthermore, disclosing one’s serostatus frees the individual from hiding complicated mediation adherence rituals from friends, family, and coworkers. Thus, indirectly, support for adhering to medical regimens may be a very significant and important reward for disclosure.
Evidence that the consequences theory is relevant comes from studies conducted by prominent disclosure and HIV theorists with male samples (for example, Derlega, Metts, Petronio.& Margulis, 1993). These authors contended that individuals who are HIV-positive contemplate the need for privacy and disclosure in determining whether to disclose an HIV-positive diagnosis (Derlega et al., 1993). Derlega and colleagues (1998) found support for this hypothesis in a qualitative study of 42 HIV-positive men and women.They concluded that the process of reducing risks and increasing benefits of disclosure results in selectivity of disclosure. That is, HIV-positive individuals disclosed to those who posed little risk, while avoiding disclosure to those who could harm them. Few investigations have been conducted on disclosure in HIV-positive women. However, in a qualitative study of African American women, Black and Miles (2002) suggested that when women were confronted with a disclosure decision, they evaluated both the risks and the benefits. That is, they suggested that women made a calculated decision (termed “calculus of disclosure”) when deciding whether to disclose.
The purpose of this study was to test two theories commonly associated with HIV-positive women’s disclosure. In this article the disease progression and consequences theories of HIV disclosure are tested to better understand the applicability of each for women. We hypothesized that the consequences model surpasses the disease progression model in explaining disclosure among HIV-positive women. Generally, research on women’s HIV disclosure has been atheoretical. Disclosure-related processes, framed theoretically, can provide guidance to interventionists, future researchers, and theorists.
METHOD
Participants and Procedures
Participants for this study included 125 HIV-positive women participating in a larger, longitudinal study of HIV disclosure and mental health. Participants were women age 18 or older with an HIV-positive or AIDS diagnosis at the time of enrollment. There were two types of recruitment sites for this study. The first were clinics associated with a large midwestern university medical center. The second were nonprofit AIDS service organizations (ASOs) in the three largest metropolitan areas of the state that deliver case management services, including social support, housing, and advocacy.
Recruitment varied only slightly depending on the site. A research nurse at the clinics provided women with a project summary sheet when they attended their regular medical appointments. Case managers at the ASOs provided women with a project summary sheet when they attended their case management appointments. In addition, flyers were posted in the waiting and interview rooms at each facility. All participation was voluntary, and refusal to participate or dropping out did not endanger or compromise participants’ treatment at any site.
Participants completed an initial interview and questionnaire to begin the study. Between each yearly wave of data collection, participants filled out a questionnaire every six months for three years. For this investigation, wave 1 data were used. Participants were paid $35 for their participation in this part of the project. Project personnel, hired for this study, conducted the interviews and assessments.
Participants were primarily African American (67.2 percent) women between the ages of 18 and 63 (M = 37.7 years, SD = 9.4) who had contracted
Disclosure-related processes, framed theoretically, can provide guidance to interventionists, future researchers, and theorists.
HIV from unsafe sexual practices (90 percent). The length of time since diagnosis ranged from one month to 19 years (M = 7.1 years, SD = 4.1).The sample was divided among partnered (34 percent), single/divorced/widowed (48 percent), and dating (18 percent). Only 22 percent of participants were employed and reported an average monthly income of $1,569. Among these women, 56 percent completed high school, 36 percent were either in college or had some college credits, and 8 percent had a college degree.
Instruments
Women completed a social network screening questionnaire to ascertain tbe extent of their available social network and the actual number of those in the social network to whom they disclosed. An adaptation of Barrera’s Arizona Social Support Interview Schedule (ASSIS) (Barrera, 1981) was used for this purpose.The ASSIS consists of a series of questions tapping seven dimensions of a social support network. For example, participants were asked who they would talk to about things that are personal and private. After the list of social network members was completed, they were asked whether they had talked with each network member in the past month about things that are personal and private. These questions were asked about getting advice, borrowing money, socializing, negative interactions, positive feedback, and physical assistance. After the interview, demographic information (that is, gender, age, and race) of each network member was obtained. In addition, participants were asked about their relationship with the network member (for example, husband, sister, aunt, or friend), length of relationship, satisfaction with relationship, physical distance or proximity (for example, live together, live within same neighborhood), frequency of contact (for example, daily or weekly), if this person knows they are HIV-positive and if so who told them.
For this project, the disclosure rate of each target group (that is, immediate family, extended family, and friends) was calculated by dividing the number of people disclosed to by the total number of people in the network. Immediate family members included parents, siblings, and spouses related by blood, marriage, or adoption. Participants reported on average three immediate family members (SD = 2.4), with an average of 69 percent of them being told of the diagnosis. Extended family members included all people related by blood, marriage, or adoption. Participants averaged one extended family member (SD = 1.5), with an average of 42 percent of them being told of the diagnosis. Participants also reported an average of three friends (SD = 3.8), with an average of 52 percent of them being told of the diagnosis. Participants were also asked about additional family members not mentioned during the ASSIS interview. For example,“You mentioned your mother, what about your father?” Participants would then report whether their father was perhaps deceased or not active in their life.
Consequences of disclosure were measured with an 18-item (Serovich,2001) instrument. Participants were asked how important each possible consequence concerning disclosure was to them when considering each specific person. Consequences were categorized into 10 reward (α = .87) and eight cost (α = .86) items. For example, fear of being blamed for contracting HIV after disclosing to that person was a negative consequence, whereas believing that disclosing would bring the relationship closer was a positive consequence.The response set ranged from 1 = not important to 5 = very important. See Table 1 for means and standard deviations.
Table 1. Means and Standard Deviations for Consequences of Disclosing HIV Status among Women.
| Rewards |
Costs |
||||
|---|---|---|---|---|---|
| Item | M | SD | Item | M | SD |
| Keep them safe from HIV | 4.23 | 1.23 | Person would lecture me | 3.57 | 1.35 |
| They had a right to know | 3.95 | 1.37 | We would fight | 3.30 | 1.61 |
| I could count on the person | 3.79 | 1.38 | Person would blame me | 3.27 | 1.50 |
| Person would be understanding | 3.72 | 1.31 | Person would be burdened | 2.96 | 1.39 |
| Be more connected | 3.40 | 1.50 | Person would be concerned | 2.76 | 1.47 |
| Would bring us closer | 3.39 | 1.52 | Relationship would get bad | 2.57 | 1.53 |
| Make the relationship better | 3.38 | 1.49 | Person would not want to be around me | 2.50 | 1.51 |
| Get emotional support | 3.33 | 1.34 | Might lose the relationship | 2.37 | 1.55 |
| Person could be prepared to assist me | 3.29 | 1.51 | |||
| I could blow off steam | 2.53 | 1.40 | |||
| Total | 3.50 | 0.96 | Total | 2.96 | 1.06 |
Note: Scale ranges from 1 = not important to 5 = very important.
Disease progression was assessed by using viral load (M = 14,911, R = 0 - 94,452, SD = 23,702) or the amount of virus detected in the blood system and CD4T-cell count (M = 527, R = 6 - 2,128, SD = 373). Both were obtained from medical records.
Analytic Procedure
Structural equation modeling (SEM) analysis with four single-indicator variables and one latent variable was used to test the proposed models predicting the relationship among disease progression, consequences, and disclosure.The data were analyzed with maximum likelihood estimation in the LISREL 8.3 Jöreskog & Sörbom, 1993) program. Chi-square statistics, root mean square error of approximation (RMSEA), comparative fit index (CFI), and goodness of fit index (GFI) were used to evaluate goodness of fit. For all tests the level of significance was set at p ≤ .05. We began by specifying the disease progression model in which disease progression is a predictor of disclosure. Then the consequences model was examined by testing the relationship among disease progression, consequences, and disclosure. It was expected that consequences of disclosure would mediate the relationship between disease progression and disclosure.
RESULTS
The data were checked for multinormality because the maximum likelihood estimation assumes that the observed variables follow a multivariate normal distribution. As a result severe violations of the multinormality assumption for variables were detected χ2 = 64.32, p ≤ .001 .Therefore, the use of normal scores was adopted to find the most appropriate transformation that would uphold the assumption. Data screening results for the variables analyzed in the study with means, standard deviations, skewness coefficients, and kurtosis coefficients are presented in Table 2.
Table 2. Descriptive Statistics for Study Variables.
| Variable | M | SD | Kurtosis | Skewness |
|---|---|---|---|---|
| Viral load | 14861.73 | 23226.14 | .95 | 1.53 |
| CD4 T-cell count | 522.49 | 355.107 | .52 | .97 |
| Reward | 3.50 | .96 | -.23 | -.63 |
| Cost | 2.90 | 1.05 | -.87 | .25 |
| Immediate family | .69 | .36 | -.82 | -.73 |
| Friends | .41 | .41 | -1.53 | .32 |
| Extended family | .42 | .44 | -1.61 | .39 |
Disease Progression Model
The disease progression model contained two single-indicator exogenous variables for disease progression and one endogenous latent variable with three indicators (see Figure 1). For this model, a covariance matrix of five variables was entered as the input matrix.Then by means of maximum Wishart likelihood iterative method, parameter estimates were calculated for paths and disturbance terms for all models.The null hypothesis for each model was that there is no significant difference between the original matrix of correlations and the reproduced correlation matrix.The RMSEA for the disease progression model was .047 (90% confidence interval [CI]: 0.00-0.17), which is considered to be a close fit but with a very large CI (RMSEA interpretive guidelines: .00 = perfect fit, between .00 and .05 = close fit, between .05 and .08 reasonable fit, and ≥, .10 = unacceptable fit) (Browne & Cudeck, 1992). The chi-square test of the model fit was nonsignificant [χ2(3) = 3.82], and the values of CFI (0.99) and GFI (0.99) indicated good fit. To indicate good fit, CFI and GFI are expected to be above 0.95 (Hu & Bentler, 1995). Although the disease progression model appeared to be an acceptable model based on the values of model fit indices, attention to the parameter estimates showed an irregularity.That is, an examination of the structural model revealed that the parameter estimates for viral load and CD4 T-cell count to disclosure were nonsignificant (β = -0.01, t = -.58; β = 0.00, t = -1.37, respectively). In addition, this model suggested that only 3 percent of the variance in disclosure could be explained by disease progression. Thus disease progression was not as predictive of disclosure of HIV status as was otherwise thought.
Figure 1. Disease Progression and Consequences Models with Standardized Parameter Estimates.
*Indicates significant path.
Consequences Model
The consequences model contained two single-indicator exogenous variables and two single-indicator endogenous variables and one endogenous latent variable with three indicators of disclosure (see Figure 1). For this model, a covariance matrix of seven variables was entered as the input matrix (see Table 3).The RMSEA for the consequences model was .060 (90% CI:0.00-0.12),which is considered a reasonable fit with a relatively smaller CI compared with that of the disease progression model. The chi-square test of the model fit was nonsignificant [χ2(10) = 14.70];the CFI = 0.97 and the GFI = 0.97. Further inspection of this structural model revealed that the path from reward to disclosure was significant (β = 0.14, t = 4.22). However,the hypothesized path from disease progression and consequences (β = -0.04, t = -0.49, for viral load ≥ reward; β = 0.09, t = 1.13, for viral load ≥ cost; β = 0.00. t = -.42, for CD4 T-cell ≥ reward; β = 0.00, t = .51, for CD4 T-cell ≥ cost) and from cost to disclosure was nonsignificant (β = 0.04, t = 1.42).This model also suggests that the dismal amount of variance in a cost consequence (1 percent) and almost nothing for a reward consequence might be explained by the disease progression indicators, whereas 16 percent of the variance in disclosure might be explained by the consequences and disease progression.This suggests that although disease progression is not a precursor to consequences, consequences (especially expected reward of disclosure) are predictive of disclosure.
Table 3. Covariance Matrix among Indicators (n = 125).
| Indicator | 1 | 2 | 3 | 4 | 4 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Viral load | 98.53 | ||||||
| 2. CD4 T-cell | -4.99 | 1.12 | |||||
| 3. Reward | -.14 | -.02 | .56 | ||||
| 4. Cost | -.02 | .08 | -.06 | .74 | |||
| 5. Immediate | -.77 | .00 | .10 | .00 | .16 | ||
| 6. Extended | -.03 | -.04 | .07 | .01 | .09 | .11 | |
| 7. Friend | -.16 | 0.01 | .08 | .04 | .06 | .04 | .16 |
Revised Consequences Model
Because disease progression did not significantly contribute to either model, the consequences model was analyzed omitting the path of disease progression to consequences (see Figure 1). The RMSEA for the revised consequences model was .026 (90% CI: 0.00-0.16), which is considered a close fit.The chi-square test was nonsignificant [χ2(3) = 3.26]; the CFI = 1.00 and the GFI = 0.99. Therefore, all fit indices consistently indicated good fit in the revised consequence model. In addition, each measured variable loaded significantly on the disclosure latent variable in the predicted manner. This model revealed that the hypothesized path from reward consequence to disclosure was significant (β = 0.14, t = 4.20), whereas the path from cost consequence to disclosure was not significant (β = 0.04, t = 1.42). In this model 15 percent of the variance in disclosure was explained by consequences, which indicates that omitting disease progression indicators did not cause a significant difference in terms of explaining disclosure.This suggests that the final model best explained that the evaluation of disclosure and perceived consequences is a precursor of disclosure.
DISCUSSION
The results of this study support an earlier claim that disease progression may not be a direct precursor of HIV disclosure (Serovich, 2001). Historically, the progression of HIV disease has been unambiguous; contracting HIV meant an early death. Because of this, many women may have experienced a pressing need to settle personal matters quickly, which necessitated disclosure. For women to conceal an HIV diagnosis from close family members and friends under these conditions would have been difficult. Currently, however, advanced therapies have changed the progression of HIV, with many women living longer, healthier, and more productive lives. Hence, with early detection and proper medical attention, disease progression may not play as pivotal a role in women’s disclosure decisions. In addition, as the general public becomes more educated and accepting of HIV infection, the potential rewards of disclosure may outweigh the potential costs.
Other plausible explanations for the lack of support for the relationship between disease progression and disclosure could be argued. First, there is considerable variability in which disease progression has been measured in earlier studies (Mansergh, Marks, & Simoni, 1995; Marks, Bundek, et al., 1992). Indices of disease progression such as symptom severity, CD4 T-cell counts, number of opportunistic infections, and time since diagnosis may not be measuring “disease progression” as previously conceptualized. In fact, it is equally plausible that what is being measured is the degree to which women experience heightened symptomatology and not health decline. Second, there may be a methodological or theoretical problem in the assumption that a woman’s medical condition at one point in time is related to the cumulative measurement of her disclosure. Future researchers should he cautious in the interpretation of such data.
The results of this study support a consequences-based model of HIV disclosure, which suggests that women may evaluate the rewards and costs of disclosure to family and friends before it occurs. Unfortunately, how this processing occurs, how rewards and costs are weighed, who is involved, and how to intervene in this process were not considered in this study and are yet to be fully understood.There may he, however, some indication of the important items to be considered by examining Table 2. For women, the most frequently reported rewards for disclosing their HIV status appeared to be other and not self-oriented. For example, priority rewards focused on the concern for other’s safety (that is, “Keep them safe from HIV,” and “They had a right to know”) rather than their own. In fact, the less frequently reported rewards for disclosure were self-oriented. These rewards focused more on the woman’s own instrumental needs (that is, “Person could be prepared to assist me”) or expressive needs (“I could blow off steam”).This is further supported by an examination of the most frequently reported costs for disclosing. Concerns about negative communications that might follow disclosure (that is,
A fuller understanding of the rewards and costs associated with disclosure could offer some insight into the consequences women consider in deciding whether to disclose their HIV status.
“Person would lecture me”) were predominant, whereas less frequently endorsed costs for disclosure were about the relationship (that is, “Person would not want to be around me,” and “Might lose the relationship”).
Although it is altruistic that women view those to whom they disclose as needing the information to either heighten their awareness of HIV or out of obligation because of familial or emotional ties, the other focus is worrisome as it might lead to a minimization of their own needs. If women approach disclosure with that attitude of “you need this information,” this could result in a false perception by others that the woman is handling her situation well. Given the high levels of reported depression in HIV-positive women (Kaplan et al., 1997; Miles et al., 1997), this is problematic. In fact, in this sample more than 62 percent of women would be considered clinically depressed with scores of more than 16 on the Center for Epidemiologic Studies Depression Scale (Radloff, 1977).
A fuller understanding of the rewards and costs associated with disclosure could offer some insight into the consequences women consider in deciding whether to disclose their HIV status. For professionals (for example, nurses, partner notification programs) this information might provide potential entry points for intervention with these women. For example, it may be helpful to direct women toward considering how both others and they could benefit from disclosure. Helping women examine both the prospective costs and rewards of disclosure may prevent women from incurring further isolation.
One limitation of this study is the relatively small sample size and the small number of indicators among suggested models that resulted in relatively wide CIs for the RMSEA values. Future researchers may consider replicating with a larger sample size and additional indicators to evaluate these models more fully. Unfortunately, garnering larger samples typically means conducting studies in larger coastal cities. Although important, these studies do not represent women living in smaller, sometimes midwestern areas who may be experiencing the social ramifications of HIV infection differently. Therefore, careful consideration should be made to avoid diminishing the results of smaller studies, inherently dismissing the voices of those who participated in them.
A second limitation of this study is the nature of the data. Interpretative caution may be required because of the cross-sectional, retrospective nature of these data. Tracking women from diagnosis to disclosure could he enlightening as it would allow monitoring of the process in real time so that objective evaluations of the process can be assessed, as opposed to relying on retrospective data. Prospective investigations of this phenomenon might offer clarity and provide a more accurate assessment. Logically, however, those kinds of studies are difficult and costly to conduct. In fact, the current study may be the best attempt to date to capture a very difficult, potentially stigmatized process occurring at a time of great discrimination, high anxiety, and emotion. Although a prospective account is most desirable, unfortunately, such data are not, and will never be, available for this particular time period.
Future researchers might consider taking a closer look at how women weigh rewards and costs, who is involved in the process, and how to intervene. Furthermore, the current study did not include a model for women’s disclosure to either children or sexual partners. Although there is considerable literature on disclosure to children, less is available on women’s disclosure to their sexual partners. Understanding what consequences are considered in this decision-making process would assist both prevention and mental health professionals. For disclosure to children, a consequences perspective may assist in translating the primarily descriptive work into a theoretically comprehensive approach for addressing disclosure.
Acknowledgments
This work was funded by National Institute of Mental Health grant R01MH62293. The authors thank all of the women who participated in this study.
REFERENCES
- Babcock JH. Involving family and significant others in acute care. In: Aronstein DM, Thompson BJ, editors. HIV and social work: A practitioner’s guide. Harrington Park Press; New York: 1998. pp. 101–108. [Google Scholar]
- Barrera M., Jr. Social support in the adjustment of pregnant adolescents: Assessment issues. In: Gottlieb BH, editor. Social networks and social support. Sage Publications; Beverly Hills. CA: 1981. pp. 69–96. [Google Scholar]
- Black B, Miles MS. Calculating the risks and benefits of disclosure in African American women who have HIV. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2002;31:688–697. doi: 10.1177/0884217502239211. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociological Methods and Research. 1992;21:230–258. [Google Scholar]
- Centers for Disease Control and Prevention . HIV/AIDS Surveillance Report. Author; Atlanta: 2005. [Google Scholar]
- Coleman C. Unpublished doctoral dissertation. University of California; Los Angeles: 1994. Coping strategies, psychological adjustment, and AIDS-related concerns of women with the human immunodeficiency virus. [Google Scholar]
- Crandall CS, Coleman R. AIDS-related stigmatization and the disruption of social relationships. Journal of Social and Personal Relationships. 1992;9:163–177. [Google Scholar]
- Derlega VJ, Lovejoy D, Winstead BA. Personal accounts of disclosing and concealing HIV-positive test results: Weighing the benefits and risks. In: Derlega VJ, Barbee A, editors. HIV infection and social interactions. Sage Publications; Newbury Park, CA: 1998. pp. 147–164. [Google Scholar]
- Derlega VJ, Metts S, Petronio S, Margulis ST. Self-disclosure. Sage Publications; Newbury Park, CA: 1993. [Google Scholar]
- Gielen AC, O’Campo P, Faden RR, Eke A. Women with HIV: Disclosure concerns and experiences; Paper presented at the HIV Infection in Women Conference; Washington, DC. 1995, February. [Google Scholar]
- Hays RB, McKusick L, Pollack L, Hilliard R, Hoff C, Coates TJ. Disclosing HIV seropositivity to significant others. AIDS. 1993;7:425–431. doi: 10.1097/00002030-199303000-00019. [DOI] [PubMed] [Google Scholar]
- Holt R, Court P, Vedhara K, Nott KH, Holmes J, Snow MH. The role of disclosure in coping with HIV infection. AIDS Care. 1998;10(1):49–60. doi: 10.1080/09540129850124578. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Evaluating model fit. In: Hoyle RH, editor. Structural equation modeling: Concepts, issues, and applications. Sage Publications; Thousand Oaks, CA: 1995. pp. 76–99. [Google Scholar]
- Jenkins SR, Galindo L. Dilemmas of disclosure of HIV+ families; Paper presented at the Third Annual NIMH Research Conference on the Role of Families in Preventing and Adapting to HIV/AIDS; Washington, DC.. 1995, July. [Google Scholar]
- Jöreskog KG, Sörbom D. LISREL 8: User’s reference guide. Scientific Software; Chicago: 1993. [Google Scholar]
- Kalichman SC. Understanding AIDS: Advances in research and treatment. 2nd ed. American Psychological Association; Washington, DC: 1998. [Google Scholar]
- Kalichman SC, DiMarco M, Austin J, Luke W, DiFonzo K. Stress, social support, and HIV-status disclosure to family and friends among HIV-positive men and women. Journal of Behavioral Medicine. 2003;26:315–332. doi: 10.1023/a:1024252926930. [DOI] [PubMed] [Google Scholar]
- Kaplan MS, Marks G, Mertens SB. Distress and coping among women with HIV infection: Preliminarly findings from a multiethnic sample. American Journal of Orthopsychiatry. 1997;67:80–91. doi: 10.1037/h0080213. [DOI] [PubMed] [Google Scholar]
- Kimberly JA, Serovich JM, Greene K. Disclosure ot HIV-positive status: Five women’s stories. Family Relations. 1995;44:316–322. [Google Scholar]
- Mansergh G, Marks G, Simoni JM. Self-disclosure of HIV infection among men who vary in time since seropositive diagnosis and symptomatic status. AIDS. 1995;9:639–644. doi: 10.1097/00002030-199506000-00017. [DOI] [PubMed] [Google Scholar]
- Marks G, Bundek NI, Richardson JL, Ruiz MS, Maldonado N, Mason HRC. Self-disclosure of HIV infection: Preliminary results from a sample of Hispanic men. Health Psychology. 1992;11:300–306. doi: 10.1037//0278-6133.11.5.300. [DOI] [PubMed] [Google Scholar]
- Marks G, Richardson JL, Ruiz MS, Maldonado N. HIV-infected men’s practices in notifying past sexual partners of infection risk. Public Health Reports. 1992;107:100–105. [PMC free article] [PubMed] [Google Scholar]
- Mason HRC, Marks G, Simoni JM, Ruiz MS, Richardson j. L. Culturally sanctioned secrets? Latino men’s nondisclosure of HIV infection to family, friends, and lovers. Health Psychology. 1995;14:6–12. doi: 10.1037//0278-6133.14.1.6. [DOI] [PubMed] [Google Scholar]
- Miles MS, Burchinal P, Holditch-Davis D, Wasilewski Y, Christian B. Personal, family, and health-related correlates of depressive symptoms in mothers with HIV. Journal of Family Psychology. 1997;11:23–34. [Google Scholar]
- Radloff LS. The CES-D Scale:A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rosenberg PS. Scope of the AIDS epidemic in the United States. Science. 1995 November 24;270:1372–1375. doi: 10.1126/science.270.5240.1372. [DOI] [PubMed] [Google Scholar]
- Serovich JM. A test of two HIV disclosure theories. AIDS Education and Prevention. 2001;13:355–364. doi: 10.1521/aeap.13.4.355.21424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Mason HRC, Marks G, Ruiz MS, Reed D, Richardson JL. Women’s self-disclosure of HIV-infection: Rates, reasons, and reaction. Journal of Consulting and Clinical Psychology. 1995;63:474–478. doi: 10.1037//0022-006x.63.3.474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sowell RL, Lowenstein A, Moneyham L, Demi A, Mizuno Y, Seals BF. Resources, stigma, and patterns of disclosure in rural women with HIV infection. Public Health Nursing. 1997;14:302–312. doi: 10.1111/j.1525-1446.1997.tb00379.x. [DOI] [PubMed] [Google Scholar]
- Sowell RL, Seals BF, Phillips KD, Julious CH. Disclosure of HIV infection: How do women decide to tell? Health Education Research Theory and Practice. 2003;18:32–44. doi: 10.1093/her/18.1.32. [DOI] [PubMed] [Google Scholar]