Abstract
This study uses a diffusion of innovations theoretical framework (Rogers, 2003) to identify organizational-level predictors of a categorical typology of substance abuse treatment centers based on naltrexone adoption. Data from the National Treatment Center Study (n=158) was used to examine the impact of socio-economic status, organizational personality, and communication behavior on adopter categorization (i.e., innovators, early adopters, early majority, late majority, or laggards). Results from the ordered logistic regression model indicate that organizations’ that did not have on-site 12-step meetings and were familiar with treatment innovations were more likely to be in a more innovative category. Organizations that learned about innovations from professional development seminars and informal conversations with external treatment providers were more likely to be in a less innovative category. Identifying and targeting the early and late majority categories of adopting organizations for better training and community linkages could help to reduce the research to practice gap.
Keywords: Innovation Adoption, Naltrexone, Categorical Typology, Organizations
1. Introduction
The use of medications to treatment alcohol and drug dependence has shown promise in several clinical trials; however, substance abuse treatment centers have been slow to integrate these evidence-based practices into their respective treatment regimens. Issues surrounding this “research to practice gap” have been widely discussed in recent years (Backer, David, & Soucy, 1995; Lamb, Greenlick, & McCarty, 1998), with significant concern that this gap will prevent new treatment practices from being delivered in substance abuse treatment centers. One promising pharmacological therapy that has not been widely adopted is naltrexone (ReVia), an opiate antagonist used in the treatment of both opiate and alcohol dependence.
The purpose of this study is to use a “diffusion of innovations” theoretical framework to identify organizational-level predictors of a categorical typology of private substance abuse treatment centers, where the categories represent varying levels of the speed with which centers adopt naltrexone. Private centers, or centers operating primarily on revenues from commercial insurers and client fees, were chosen as the unit of analysis because they are subject to managed care organizations which are calling for the use of evidenced based practices (Knudsen & Roman, 2004; Knudsen, Roman, Ducharme, & Johnson, 2005; Magura, Schildhaus, Rosenblum, & Gastfriend, 2002). Data were collected from administrators as part of the National Treatment Center Study (NTCS). It should be noted that the use of the administrator as a proxy for the organization could be an over-simplification of the organization’s beliefs, values, and practices, thereby impacting the results. However, this approach is consistent with other organizational-level studies of innovation adoption (Knudsen, Ducharme, & Roman, 2006; Oser, Staton-Tindall, & Leukefeld, 2007).
1.1. Naltrexone (Re Via)
The substance abuse treatment field has endorsed the use of naltrexone as an effective treatment choice for specific demographic populations, but only some organizations have adopted naltrexone. The development of naltrexone for the treatment of opiate dependence dates back to the 1960’s (Stine & Kosten, 1997), with approval by the Food and Drug Administration (FDA) resulting in 1984. The standard usage of naltrexone for the treatment of opiate dependence is as a post-withdrawal relapse prevention intervention, however it can also be used during the process of rapid opiate detox. As a non-specific competitive opiate antagonist, naltrexone works by binding to the mu receptor, thus hindering the activity of opiates (Kirchmayer et al., 1997). Opiate self-administration is no long rewarding in the presence of naltrexone, thus ideally reducing or eliminating the behavior. The best results with naltrexone treatment have been reported in patients whose careers depended on compliance with treatment, such as medical professionals or business executives (Ling & Wesson, 1984; Washton, Pottash, & Gold, 1984), or in patients under contingency contracting, such as prisoners or probationers (Brahen, Henderson, Capone, & Kondal, 1984).
Subsequently, this pharmacological innovation was approved for the adjunctive treatment of alcohol dependence a decade later based on two single-site randomized trials which reported that the use of naltrexone, when used in concert with psychosocial therapies, decreases cravings and reduces the risk of relapse (O’Malley et al., 1992; Volpicelli, Alterman, Hayashida, & O’Brien, 1992). However, several studies have not been able to fully replicate the results of the two initial studies (Chick et al., 2000; Volpicelli et al., 1997), and again further research emphasizes the need to increase compliance with naltrexone (Chick et al., 2000; O’Brien, Volpicelli, & Volpicelli, 1996; Oslin et al., 1999; Volpicelli et al., 1997). Moreover, naltrexone may only be an effective treatment approach for specific patient populations of motivated individuals with low to moderate levels of alcohol dependence (Anton et al., 1999; Krystal et al., 2001).
A few caveats must be noted. First, the authors are not promoting a pro-innovation bias, which would imply that an innovation should be utilized by all individuals within a social system, that the innovation should be rapidly diffused, and that it should not be re-invented (Rogers, 2003). It is important to note that the use of naltrexone is not recommended for all clients within a treatment center; however, the vast majority of private treatment facilities will have at least a few clients who could benefit from naltrexone treatment. Second, a calculated decision was made in selecting the “example” of naltrexone adoption. Naltrexone was chosen over antabuse and methadone because it is a more novel, less established alcohol and opiate treatment. Additionally, naltrexone was selected over the more recently FDA approved treatments (e.g., Buprenorphine) because it provides a sufficient timeframe to look at yearly trends of adoption.
1.2. Categorical Typology of Adopters
While previous research has examined the organizational-level predictors of naltrexone adoption using both cross-sectional data (Roman & Johnson, 2002) and longitudinal data dating back to 1984 (Oser & Roman, in press), this is the first study to examine naltrexone innovativeness, or the degree to which a substance abuse treatment organization is relatively earlier in adopting naltrexone than other adopting organizations. There is a contagion effect of the innovation diffusion process (Rai, Ravichandran, & Samaddar, 1998; Rogers, 2003). It is important to differentiate the first organizations to try a new product or service from the later adopters who wait until the vast majority of consumers have adopted because it allows for the future targeting of the correct audience of potential adopters. This is a worthy endeavor because information on how organizational characteristics affect the adoption process over time will help the substance abuse treatment field to better understand the dynamics of private organizational adoption of pharmacotherapies.
Rogers’ (2003) continuum of innovation identifies five categories within the normal curve of adoption: innovators, early adopters, early majority, late majority, and laggards. These five ideal types of adoption behaviors are exhaustive, mutually exclusive, and derived from a single classification principle. Innovators are characterized by organizational traits (e.g., stable economic position, technical expertise, and effective coping strategies) that can support their intense interest in novel ideas. Early adopters are distinguished by noteworthy social connections as well as a drive to improve their performance (DiMaggio & Powell, 1983). The early adopters often engage in cross-pollination because they are watched by other organizations and are the most likely targets of pharmaceutical company detailing (Berwick, 2003).
The early majority are defined by a deliberate motive to adopt new ideas just before the average organization adopts. According to Berwick (2003), early majority organizations in health care settings scan their local environment for innovations, are likely to observe the early adopters behavior, and primarily base their adoption decision on informal communication of local proof (rather than on scientific or theoretical foundations). The late majority, characterized by skepticism, do not adopt until just after the average organization has adopted. The late majority may experience a bandwagon pressure to adopt, fearing that non-adoption will result in sub-par performance and the inability to reap financial rewards (Abrahamson & Rosenkopf, 1993). The final category, termed the laggards, place an emphasis on traditional, normative practices. Adoption by laggards is impeded by a lack of organizational leadership, a deficient knowledge base surrounding innovations, and inadequate financial resources. Oftentimes, there is a negative connotation associated with the term “laggards” that undermines their value as traditionalist and their wisdom to use the past as a point of reference (Berwick, 2003).
1.3. Theoretical Concepts Predicting Innovativeness
This study is the first to use a diffusion of innovations theoretical framework (Rogers, 2003) to identify the organizational-level predictors of a categorical typology of substance abuse treatment centers based on naltrexone adoption. Specifically, the three organizational-level components of Socio-Economic Status, Organizational Personality, and Communication Behavior are used to predict adopter categorization.
The characteristics of adopting organizations suggest that Socio-Economic Status and innovativeness go hand in hand (Martinez, Polo, & Flavian, 1998; Rogers, 2003). The age of the organization was found to positively impact pharmacotherapy adoption behavior (Roman & Johnson, 2002). Earlier adopters have been typified as more educated, of higher socio-economic status, and larger in size (Rogers, 2003). Organizations that are innovators, as compared to laggards, employ staff with more years of formal education (Dickerson & Gentry, 1983; Greco & Fields, 1991; Martinez et al., 1998). At the macro-level, organizations may be adopting innovations in an effort to obtain or secure a higher socio-economic status. Treatment centers with higher socio-economic status are expected to acknowledge and financially compensate for the value of emotional labor that their counselors engage in. Being in a higher income bracket is positively associated with innovativeness (Dickerson & Gentry, 1983; Greco & Fields, 1991; Martinez et al., 1998).
Another characteristic that marks organizations as innovators is size (Castle, 2001; Rogers, 2003; Yan Tam, 1996). Damanpour (1987) suggests that the size effect is really the availability of slack resources within a large organization. It has also been postulated that larger organizations may receive more information regarding innovations and could possess the resources to quickly implement these techniques.
Organizational Personality, or climate, is the second component cited by Rogers (2003) as influential in predicting adopter categorization. This has been largely unexplored by researchers, which can be attributed to variability in organizational personality by industry as well as to difficulties operationalizing these concepts (Rogers, 2003). It is hypothesized that laggards will be less flexible because these organizations prefer to maintain the status quo or have more brand loyalty (Greco & Fields, 1991). In transferring this line of thought to the substance abuse treatment field, it is believed that facilities based on a 12-step ideology may be characterized by organizational inertia and may subsequently be less likely to try novel treatment techniques.
Innovations can be differentiated by the manner in which they congeal with an organization’s climate or personality. The adoption of radical innovations results in fundamental changes in the activities of an organization, whereas incremental innovations produce little departure from existing practices (Damanpour, 1991). Therefore, incremental innovations are more likely to be adopted because they result in a minimal deviation from existing practices (Dewar & Dutton, 1986). For example, this can be translated to the adoption of naltrexone in private treatment facilities because if a facility is already emphasizing the medical model of treatment, the adoption of naltrexone will be an incremental innovation.
The factors influencing the original decision to adopt may vary by innovativeness. Organizations that adopt naltrexone because of either consistency with their treatment practices or a need for an alternative to more traditional treatment are hypothesized to be more flexible facilities. The early adoption of this innovation would only been seen as an incremental, rather than radical, innovation. On the contrary, facilities that state the use of naltrexone at comparable centers is an influential factor in their decision to adopt will be less likely to be innovators. It is also hypothesized that innovators have a more favorable attitude towards science than do laggards (Rogers, 2003). Familiarity of a treatment center’s staff with other innovative pharmacotherapies can be used as a proxy measure of an organization’s attitude towards science. If the knowledge resources are already in existence, then new techniques can be easily understood and the infrastructure is already in place to encourage adoption (Dewar & Dutton, 1986; Dickerson & Gentry, 1983).
The third component that is expected to influence the adopter categorization is Communication Behavior (Rogers, 2003). Knowledge of innovations can be communicated through formal sources (i.e., scientific journals, pharmaceutical companies, provider associations) or informal sources (i.e., professional development activities and informal conversations). In addition, accreditation status and market competition may be related to communication behavior. As a result of the uncertainty related with innovation adoption, organizations may conduct a cost-benefits analysis or engage in other proactive strategies to decrease the perception of ambiguity associated with innovation adoption (e.g., environmental scanning) (Fahey & Narayanan, 1989). Seeking out external sources of information about one’s environment increases both the speed and breadth of diffusion because the potential adopter is more knowledgeable about the needs of clientele base (O’Neill, Pouder, & Buchholtz, 1998). Specific to the treatment field, environmental scanning had a positive effect on the adoption of an aggregate measure of 15 innovative treatment techniques (Knudsen & Roman, 2004).
To begin with formal sources of knowledge, the majority of health care organizations do not regularly review appropriate scientific journals, nor have they assigned as a routine job task the attendance at key scientific meetings in an effort to report back to the organization about effective treatment techniques (Berwick, 2003; Ely et al., 2002). Organizations that do engage and immerse themselves in these activities are expected to be innovators. In addition, knowledge communicated by the pharmaceutical industry plays a significant role in organizational innovativeness. This industry has harvested huge rewards by recognizing the power of face-to-face interaction “detailing” the characteristics of new drugs to physicians (Berwick, 2003). In fact, the first news of a new drug is most often learned about from pharmaceutical representatives or journal advertisements (Jones, Greenfield, & Bradley, 2001). Furthermore, involvement in provider associations and industry or trade associations widens the hospital’s environmental focus, encourages the sharing of technical knowledge, and fosters institutional legitimacy (Goes & Ho Park, 1997; Ibarra, 1993; Mohr, 1992; Thomas & Trevino, 1993).
While formal sources are an important form of communicating innovation knowledge for innovators, informal sources are the primary source of information fueling the adoption decision of laggards (Gatigon & Robertson, 1989). Informal communication with other organizations provides an opportunity to exchange technical information/resources, establish legitimacy, and provide a point of reference (Oliver, 1990; Nohria & Eccles, 1992). After an organization becomes aware of adoption in their local environment they may attempt to disseminate innovation knowledge to their own staff through professional development seminars.
Another manner in which organizations may communicate with their industry, and thereby learn of innovations in their field, is by receiving an accredited status. Accredited organizations face considerable pressure from their accrediting agencies including accountability (Griffith, Sahney, & Mohr, 1995). For organizations to obtain and maintain their accredited status by organizations such as the Joint Commission on Accreditation of Health Care Organizations (JCAHO), they must have regular reviews to examine medical records to assess the quality of care provided by hospitals and they must document evidence of quality improvement practices (Westphal, Gulati, & Shortell, 1997).
Competition is the final variable related to Communication Behavior. The presence of repeated success among innovation adopters prompts other organizations to innovate; this pattern is particularly prominent in competitive environments (Kimberly & Evanisko, 1981). Organizations share a limited pool of resources (such as potential clients) in competitive private-sector environments, and thus may seek out innovation adoption to distinguish their services and improve their market image (Castle, 2001). Market competition has been noted in the literature as a driving force towards isomorphism, and the resulting legitimacy pressures may provide an additional impetus towards innovation adoption (Abrahamson & Rosenkopf, 1993).
Additional research is needed on the diffusion of substance abuse treatment innovations due to the field’s current interest in promoting translation from research to practice. Therefore, the purpose of this paper is to explore the theoretical predictors of innovativeness, or the degree to which a substance abuse treatment facility is relatively earlier in adopting new treatment techniques, such as naltrexone, than other organizations. The purpose of this paper is two-fold. First, descriptive statistics will display the cumulative percentage of treatment centers adopting naltrexone over the course of the study, as well as describe the distribution of adopting organizations by categorical type. These descriptive statistics are used as a first step to assess Roger’s (2003) theory of a continuum of innovativeness. A categorical typology of adopters will be created based on year of naltrexone adoption using Rogers (1958) method of adopter categorization. The five categories include innovators, early adopters, early majority, late majority, and laggards. Second, ordered logistic regression will be used to predict if a treatment center will fall into a more innovative category. This type of analysis uses a causal model specification to estimate the effects of Roger’s theoretical predictors of adopter categorization including Socio-Economic Status, Organizational Personality, and Communication Behavior on the likelihood that a treatment center will be in one of the five-adopter categories.
2. Materials and Methods
2.1. Sample: National Treatment Center Study
Data for these analyses were derived from Wave III of the National Treatment Center Study (NTCS), a nationally representative study of private-sector substance abuse treatment centers that provide treatment for both alcohol and drug dependence. Additional details on the methodology can be found elsewhere (Roman & Johnson, 2002; Oser & Roman, in press).
The initial Wave I sample of data was collected between 1994 and 1996 and included 450 centers in 38 states, with a response rate of 89%. A second wave of on-site interviews was conducted with the same panel of centers in 1997-1998. Approximately 376 treatment facilities remained both open and eligible for participation. Using a split-panel design method, approximately 30 “new” treatment centers were added to the original sample. These facilities are defined as “new” in that they began offering substance abuse services after the initial sample was created in 1994. The third wave of on-site data collection for the NTCS was conducted in 2000-2001 and included 305 of the original 450 treatment centers. Approximately 111 of the original centers had experienced organizational death, 19 treatment facilities were unable to participate, and seven centers were no longer eligible for participation in the study. A split-panel design method was again employed to augment the sample size, resulting in 397 completed on-site interviews. Only data from Wave III is used in these analyses.
Inclusion criteria for the NTCS consisted of (1) receiving less than 50% of their funding from state or federal block grants and (2) offering a level of care that is at a minimum consistent with the American Society of Addiction Medicine (ASAM) standards of a structured outpatient program. The average private center reported that over half of their clients were covered by managed care (53%) and 15% of clients were self-paying.
Informed consent was obtained from program administrators. Data collection was comprised of on-site interviews conducted by trained field interviewers in 2000-2001 with the program administrators. Of the 397 participating organizations, only 158 are included in the analyses. Treatment centers were excluded if they had not adopted naltrexone (n=234) or did not provide information on the year of naltrexone adoption (n=5). For cases that were missing data on any of the continuous independent variables, mean substitution was used but this occurred in less than 15% of the sample. Client-level data was not available; therefore, it is unclear if clients are being treated with naltrexone for alcohol or opiate dependence.
2.2. Measures
The dependent variable in the ordered logit model allowed for five outcomes, taking into account innovativeness, or the year in which a substance abuse treatment facility adopted naltrexone. In accordance with Rogers’ (2003) method for creating an innovation typology, the innovativeness variable was partitioned into five categories by laying off standard deviations from the average time of adoption (1995-1996) (see Figure 1). This method of categorization of the dependent variable resulted in the following number of organizations in each of the categories including 9 innovators (6%), 14 early adopters (9%), 49 early majority (31%), 73 late majority (46%), and 13 laggards (8%).
Figure 1.
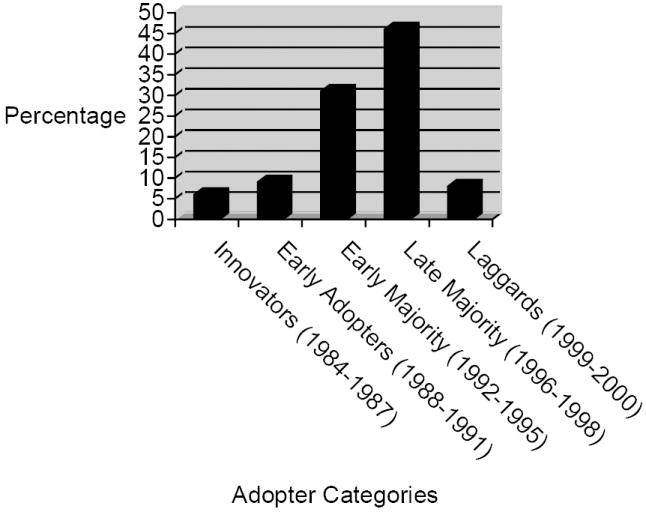
Categorical Typology of Adopting Substance Abuse Treatment Centers on the Basis of Innovativeness (n=158)
Three theoretical components were included in the ordered logit model to predict naltrexone adopter categorization including Socio-Economic Status, Organizational Personality, and Communication Behavior. First, the component of Socio-Economic Status was composed of five variables. Age was a measure of the treatment center’s age in years. Administrator education was composed of the categories of less than a Bachelor’s degree (coded 1), Bachelor’s Degree (coded 2), Master’s Degree (coded 3), and Ph.D. or M.D. (coded 4). Other variables in the socioeconomic status component included the percentage of counselors with a master’s degree or above, the mean counselor salary, and the natural log of the number of full time equivalent employees (FTEs) (appropriate because the distribution is positively skewed).
Seven measures are included in the Organizational Personality component. Two dichotomous measures assessed if the treatment center was based on a 12-step model of treatment (1 = yes; 0 = no) and if the facility held 12-step meeting on their premises (1 = yes; 0 = no). The extent to which the treatment center emphasized a medical model, ranging from a value of 0 (no emphasis) to a value of 5 (intense emphasis of the medical model), was also measured. In addition, Organizational Personality was based on three items that ask center administrators the extent to which certain factors influenced their decision to begin using naltrexone to treat qualifying clients. The factors that may have influenced naltrexone adoption included the extent to which naltrexone was consistent with the treatment centers practices/philosophy, the extent to which there was a need for an alternative to traditional treatments, and the extent to which was it used at comparable centers. Possible responses for each item ranged from 0 (no extent) to 5 (great extent). The last measure of Organizational Personality, familiarity with innovative treatments, assessed the organization’s knowledge of other innovative psychosocial and pharmacological treatment techniques including motivational enhancement therapy (MET), acupuncture, disulfiram, rapid opiate detox, LAAM, buprenorphine, methadone, and SSRI’s. An additive scale was created with possible responses ranging from a value of 0 (no familiarity of any other innovative treatments) to a value of 40 (extreme familiarity with all innovative treatments) (α = .81).
Communication Behavior was based on five items that ask center administrators to estimate the extent to which the center staff’s knowledge about innovative treatment techniques came from journal publications, materials from or contact with pharmaceutical company representatives, involvement in provider associations, informal conversations with employees of other treatment organizations, and participation in professional development seminars. Possible responses for each item ranged from a value of 0 (no extent) to a value of 5 (great extent). Centers were also distinguished by accreditation status (1 = yes; 0 = no). Finally, the extent to which a treatment center faced competition from other treatment facilities in its market area was included in the ordered logit model. Treatment center administrators were asked to rate the level of competition in their market area ranging from 1, indicating no competition, to 10, signifying intense market competition.
2.3. Analytic Strategy
Rogers’ (2003) method of categorization was employed to create categories of naltrexone adopters. To begin, the year that centers adopted naltrexone was used to graph the cumulative percentage of treatment centers adopting naltrexone. After having plotted the centers adopting naltrexone by the year of adoption as well as using two parameters of the distribution (the mean year of adoption and the standard deviation) to identify into which category they should be placed, an ordered logistic regression was performed using the five adopter categories as the dependent variable. Ordered logistic regression is the appropriate analytic method to examine Rogers’ categorical typology of naltrexone adopters and can be understood in terms of an underlying latent variable that has observed, ordered categories (Long and Freese, 2001). This model was theoretically guided to allow the dependent variable to be “cut” at four points based on the rank order of innovativeness. Ordered logit models assume proportional effects in that they estimate the (log) odds that a treatment center will fall in the “next highest” category of the dependent variable. The raw coefficients, z-scores, percent changes in odds, and the McKelvey and Zavoina R2 are reported. It should be noted that the McKelvey and Zavoina R2 is not equivalent to the R2 in an OLS model and thus should be interpreted cautiously. None of the independent variables correlated so highly as to imply multicollinearity.
3. Results
3.1. Descriptive Statistics
As displayed in Figure 2, when the cumulative percentage of adopting treatment organizations (n=158) is plotted, the result was an S-shaped curve. This was consistent with Roger’s theoretical prediction that the S-shaped adopter distribution would advance slowly at first when there are few adopters at each year. This trend was followed by a period of accelerated adoption until approximately half of the treatment facilities had adopted naltrexone. Next, the S-shaped curve increased at a gradually slower pace as fewer and fewer of the remaining treatment organizations adopt naltrexone. This S-curve of adoption had a relatively long “tail” to the left, indicating that about ten years were required before the rate of adoption started to accelerate. Table 1 displays the descriptive statistics.
Figure 2.
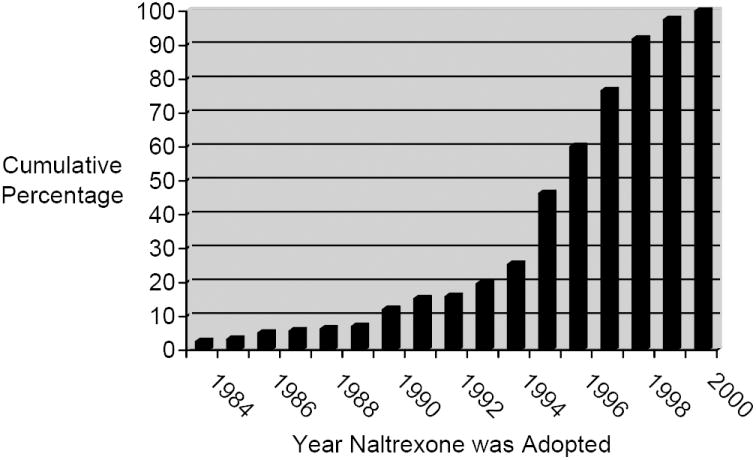
Cumulative Percentage of Naltrexone Adopting Substance Abuse Treatment Centers (n=158)
Table 1.
Descriptive Statistics of Substance Abuse Treatment Centers (n=158)
| Variable | Mean | Standard Deviation | Range |
|---|---|---|---|
| Socio-Economic Status | |||
| Age of Center | 20.53 | 13.34 | 4 – 116 |
| Administrator’s Education | 2.65 | .78 | 1 – 4 |
| % MA Counselors | 58.67 | 31.49 | 0 – 100 |
| Counselor’s Salary | 34,531.12 | 5,819.63 | 15,600 – 53,040 |
| Natural Log of FTE’s | 3.04 | 1.11 | 0 – 5.82 |
| Organization’s Personality | |||
| Based on 12-Step | .90 | .30 | 0 – 1 |
| 12-Step on Site | .85 | .35 | 0 – 1 |
| Emphasize Medical Model | 3.56 | 1.54 | 0 – 5 |
| Consistent with Treatment Philosophy | 3.25 | 1.96 | 0 – 5 |
| Need Alternative Treatment | 2.97 | 2.01 | 0 – 5 |
| Used at Comparable Centers | 1.15 | 1.59 | 0 – 5 |
| Familiar with Innovative Treatments | 25.25 | 6.92 | 11 – 40 |
| Communication Behavior | |||
| Learn from Journals | 3.51 | 1.11 | 0 – 5 |
| Learn from Pharmaceutical Co.’s | 2.40 | 1.56 | 0 – 5 |
| Learn from Provider Associations | 3.15 | 1.29 | 0 – 5 |
| Learn from Informal Conversations | 3.36 | 1.26 | 0 – 5 |
| Learn from Prof Development | 4.08 | .92 | 0 – 5 |
| Accredited | .87 | .34 | 0 – 1 |
| Level of Competition | 3.76 | 1.82 | 1 – 10 |
3.2. Ordered Logistic Regression
The results of the ordered logit model estimating the correlates of adopter categorization are displayed in Table 2. None of the variables in the Socioeconomic Characteristics component approached statistical significance; however, several variables in the Organizational Personality component were significant predictors of adopter categorization. Net of the effects of the other variables, centers that host 12-step meetings on their premises (b = -.89, p<.05) were 59% less likely to be in a higher innovative category than in a lower innovative category. Consistent with expectations, as treatment centers became more familiar with other psychosocial and pharmacological innovative treatments, the organizations percentage change in the odds of being more innovative (or being in a more innovative category because they had adopted naltrexone earlier) increased by 5.5%.
Table 2.
Coefficients from the Ordered Logit Model Predicting Substance Abuse Treatment Centers’ Adopter Categorization (n=158)
| b | z | % | |
|---|---|---|---|
| Socio-economic Status | |||
| Age of Center | .01 | .78 | 1.0 |
| Administrator’s Education | .05 | .22 | 4.9 |
| % MA Counselors | .00 | .29 | 0.2 |
| Counselor’s Salary | -.00 | -.25 | -0.0 |
| FTE’s | .14 | .86 | 14.5 |
| Organization’s Personality | |||
| Hold 12-Step Meeting on Premises | -.89* | -1.69 | -59.0 |
| Based on 12-Step | .20 | .36 | 22.0 |
| Emphasize Medical Model | -.07 | -.61 | -6.8 |
| Consistent with Tx Philosophy | -.02 | -.24 | -2.0 |
| Need Alternative Treatment | -.07 | -.76 | -6.4 |
| Used at Comparable Centers | -.16 | -.49 | -14.9 |
| Familiar with Innovative Tx | .05* | 2.09 | 5.5 |
| Communication Behavior | |||
| Learn from Journals | -.14 | -.92 | -13.3 |
| Learn from Pharmaceutical Co.’s | .04 | .32 | 3.8 |
| Learn from Provider Associations | -.00 | -.01 | -.1 |
| Learn from Informal Conversations | -.24* | -1.73 | -21.6 |
| Learn from Prof Development | -.41* | -2.22 | -33.3 |
| Accredited | -.20 | -.37 | -17.9 |
| Level of Competition | .02 | .13 | 1.3 |
| Ll_0 = -207.53 | |||
| Ll = -195.92 | |||
| McKelvey and Zavoina R2 = .14 | |||
Note:
b = raw coefficient
z = z-score for test of b=0
% = percent change in odds for a unit increase in x
p<.05 (one-tailed tests)
Two variables in the Communication Behavior component were significant in predicting the likelihood of being in a more innovative category. The hypothesis which suggested that innovators would have less innovation knowledge from informal sources (including face to face communication with employees of other treatment facilities and involvement in professional development seminars) than later adopters was supported. Treatment centers that said they learned about innovations from participation in professional development seminars and from informal conversations with employees of other treatment organizations were more likely to be less innovative (or be in a lower category). For instance, centers which indicated that they had learned about innovative treatment techniques from informal conversations with individuals employed at other treatment centers decreased their odds of being in a more innovative adopter category by 21.6%. In a similar fashion, it was found that organizations that relied more heavily on professional development seminars (i.e., moving from 0 (lower) to 5 (higher) on an ordinal scale) for information about innovations decreased their odds of being in a more innovative category by 33.3%.
A significant test statistic (Wolfe and Gould, 1998) provides evidence that the parallel regression assumption, or proportional odds assumption, has not been violated. This implies that the coefficients across the four equations are considered “close” to being equal (χ2 = 71.54, df (57), p<.09). 1
4. Discussion
Guided by the sociological theory on organizational innovation, this paper explored the organizational-level characteristics that impact adopter categorization in the substance abuse treatment field. The adoption of naltrexone followed the S-shaped curve model of adoption, with a relatively long time period of about 10 years until the rate of adoption began to accelerate. This largest period of growth occurred between 1994 and 1995, the time period immediately following the FDA’s approval of naltrexone for the treatment of alcohol dependence. This timeframe coincided with the publication of promising findings by O’Malley and colleagues (1992), as well as that by Volpicelli and colleagues (1992). Among adopting organizations, communication via media or informal means could be associated with naltrexone adoption. Additionally, this expansion may be the result of increased utility because naltrexone could be used to treat both alcohol and opiate dependent clients.
Using Rogers’ (2003) method of adopter categorization, facilities adopting naltrexone were partitioned into one of five categories using two parameters of the distribution, the mean and the standard deviation. Despite expectations, the ordered logistic regression demonstrated that organizational Socioeconomic Status characteristics did not have a statistically significant relationship with adopter categorization. A possible explanation for the rejection of the null hypothesis could be the operationalization of the independent variables. Several variables, such as age, education, income level, and size were taken directly from Roger’s theory, but others could have been included such as the profit margin. However, private-sector treatment organizations were reluctant to provide financial information, and as a result of missing data, these measures were not included in the analyses.
Two of the seven variables measuring Organizational Personality had a significant relationship with naltrexone innovativeness. Treatment facilities that host 12-step meetings on their premises may have been less receptive to new ideas and prefer to hew to their normative practices. The other 12-approach measure, being based on a 12-step model, was not predictive of innovativeness. Consistent with previous work (Oser & Roman, in press), it is suggested that these findings be viewed tentatively and additional studies are needed to confirm or refute the role of 12-step organizational personalities on naltrexone adoption. On the contrary, it is possible that organizations that were familiar with other innovative treatments had a greater ability to deal with scientific abstraction and may have adopted a new treatment technique on the basis of rather abstract scientific knowledge, such as information about other innovations. This relationship between the use of other innovative treatments and innovation adoption has been demonstrated in previous research (Ducharme, Knudsen, & Roman, 2006; Ducharme, Knudsen, Johnson, & Roman, 2007; Knudsen, Ducharme, & Roman, 2006; Knudsen, Ducharme, & Roman, 2007; Oser & Roman, in press). While Personality variables have not received much research attention, they were an important explanatory variable in the diffusion process.
Regarding Organizational Behavior, the hypothesis that innovators would have greater amounts of innovation knowledge from formal sources of knowledge (such as journals, pharmaceutical companies, and provider associations) was not supported by the multivariate model. Perhaps, these innovators were affiliated with research universities or have participated in clinical trials, thus gaining their innovative knowledge firsthand. However, organizations which learned about treatment innovations from participation in professional development seminars or from informal conversations with employees at other treatment facilities were more likely to be in the late majority or laggards category. According to Gatigon and Roberston (1989), external communication is a significant source of innovation knowledge during later stages of the adoption process because these organizations must first wait until others within their social system had adopted an innovation (e.g., naltrexone) before they could mimic their neighbors’ adoption practices. Furthermore, learning of others’ innovation adoption within the local milieu may facilitate in-house professional development activities to remain reputable and competitive.
Several limitations of this study need to be noted. The National Treatment Center Study used the administrator as a proxy for the organization. While this is a common practice in organizational-level research (Knudsen, Ducharme, & Roman, 2006; Lehman, Greener, & Simpson, 2002; Oser, Staton-Tindall, & Leukefeld, 2007), the use of a top executive may be an oversimplification (Rogers, 2003). Future studies could augment this approach with the use of survey research with line staff to conduct multi-level modeling or with ethnographic research. Other limitations include the lack of variables to measure type of clientele and economic stability. These measures could theoretically impact naltrexone adoption. Since the NTCS doesn’t collect client-level data, it is not possible to determine the extent to which naltrexone was used to treat alcohol dependence versus opiate dependence. Finally, only private centers were examined, thereby limiting the generalizability to other types of treatment settings such as public facilities and therapeutic communities.
The results of the multivariate model of innovativeness within private substance abuse treatment centers provide several recommendations for organizations wishing to adopt innovative pharmacotherapies, such as naltrexone. For example, it is important to note that treatment facilities based on a 12-step ideology may be less open to naltrexone adoption. Differing treatment philosophies have considerably different frames of reference that govern their rhetoric, actions, and behaviors. Accordingly, steps need to be taken to decrease cultural divergences. For example, naltrexone is a theoretically ideal pharmacotherapy, in that it is non-addictive, has a generally good side effect profile, and it is consistent with the desired outcome of abstinence held by facilities based on a 12-step disease model. Therefore, increasing awareness that some patients can benefit from pharmacotherapies is needed.
It would also be beneficial for change agents to target treatment facilities already using prescription drugs, because they possess the skills and knowledge necessary to experiment with other pharmacotherapies such as naltrexone. According to the NTCS, over 90% of the centers already use some form of prescription drugs, so the infrastructure is already present to implement pharmacological-based treatments. Berwick (2003) also suggests a strategy of investing in innovators and early adopters. However, this raises the issue of the innovativeness/needs paradox, which suggests that individuals or organizations which need the benefits of a new idea are generally the last to adopt an innovation (Rogers, 2003). This paradox serves to widen the gap and dichotomize the treatment field into the information-rich and the information-poor as a result of the prevalent tendency of innovation creators, or change agents, to ignore the hard-to-reach sub-audience of the late majority and laggards. In order to overcome this unwanted consequence, a segmentation strategy is needed in which change agents, such as addiction researchers or state substance abuse facility directors, target the faction of treatment facilities that they believe will be the last to adopt for intensified communication.
Finally, knowledge of innovations can be achieved by reading professional journals, participating in professional development activities, involvement in provider associations, informally speaking with other treatment providers, and through requesting promotional materials from pharmaceutical companies. The use of mediated communication in the form of company newsletters, videos, or magazines, may help to create an innovation-friendly environment (Meyer et al., 1997) and may be more cost efficient than other strategies.
In conclusion, the characteristics of the potential pool of innovation adopters do affect innovativeness within a sample of private substance abuse treatment centers. The organizational-level characteristics impacting the diffusion of substance abuse treatment innovations are often overlooked in the treatment literature, the majority of which focuses on the attributes of the innovation. Moreover, drug dependence is a chronic medical illness (McLellan, Lewis, O’Brien, & Kleber, 2000), and as such, dependent individuals have the right to adequate health care. Reducing the research to practice gap is an important public health and federal government endeavor. The identification of the significant organizational predictors guides the recommendations offered to the substance abuse treatment field in an effort to reduce the research to practice gap that currently exists.
Acknowledgments
This project is supported by grant R01-DA13110 (PI: Roman) and R03-DA107199 (PI: Oser) from the National Institute on Drug Abuse. Special thanks to Dr. J. Aaron Johnson for reading multiple drafts of this manuscript.
Footnotes
The parallel regression assumption, also known as the proportional odds assumption, implies that the coefficients across the four equations are considered “close” to being equal. Based on Wolfe and Gould’s (1998) “omodel” command in Stata (Long and Freese, 2001), the approximate likelihood ratio test of proportionality of odds across response categories indicated the assumption was on the verge of being violated in the present study. Thus, while Allison (1995) as well as Long and Freese (2001) caution that a violation of this assumption is commonplace, a multinomial model, which does not impose the constraint of parallel regressions, was also explored. After performing a likelihood-ratio test for independent variables in the multinomial model, it was found that several of the same variables improved the model fit including holding 12-step meetings on site, being familiar with other innovative treatments, and receiving a great deal of innovation knowledge from participation in professional development activities (p<.10). While learning about innovations from informal conversations with other treatment providers was not significant, endorsing a 12-step model did reach statistical significance. This model was marginally statistically significant (χ2 = 94.09, df (76), p<.08).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abrahamson R. Managerial fads and fashions: The diffusion and rejection of innovations. Academy of Management Review. 1991;16:586–612. [Google Scholar]
- Anton RF, Moak DH, Waid R, Latham PK, Malcolm RJ, Dias JK. Naltrexone and cognitive behavioral therapy for the treatment of outpatient alcoholics: Results of a placebo-controlled trial. American Journal of Psychiatry. 1999;156:1758–1764. doi: 10.1176/ajp.156.11.1758. [DOI] [PubMed] [Google Scholar]
- Backer TE, David SL, Soucy G, editors. Reviewing the behavioral science knowledge base on technology transfer: NIDA Research Monograph No 155. Rockville, MD: National Institute on Drug Abuse (NIDA); 1995. [PubMed] [Google Scholar]
- Berwick DM. Disseminating innovations in health care. JAMA. 2003;289(15):1969–1975. doi: 10.1001/jama.289.15.1969. [DOI] [PubMed] [Google Scholar]
- Brahen HS, Henderson RK, Capone T, Kondal N. Naltrexone treatment in a jail work release program. Journal of Clinical Psychiatry. 1984;45(9):49–52. [PubMed] [Google Scholar]
- Castle NG. Innovation in nursing homes: Which facilities are the early adopters. Gerontologist. 2001;41(2):161–172. doi: 10.1093/geront/41.2.161. [DOI] [PubMed] [Google Scholar]
- Chick JR, Anton R, Checinski K, Croop RS, Drummond DC, Farmer R, et al. A multicentre, randomized, double-blind, placebo-controlled trial of naltrexone in the treatment of alcohol dependence and abuse. Alcohol & Alcoholism. 2000;35:587–593. doi: 10.1093/alcalc/35.6.587. [DOI] [PubMed] [Google Scholar]
- Damanpour F. The adoption of technological, administrative, and ancillary innovations: Impact of organizational factors. Journal of Management. 1987;13:675–688. [Google Scholar]
- Damanpour F. Organizational innovation: A meta-analysis of effects of determinants and moderators. Academy of Management Journal. 1991;34:555–590. [Google Scholar]
- Dewar RD, Dutton JE. The adoption of radical and incremental innovations: An empirical analysis. Management Science. 1986;32:1422–1433. [Google Scholar]
- Dickerson MD, Gentry JW. Characteristics of adopters and non adopters of the home computer. Journal of Consumer Research. 1983;10:225–235. [Google Scholar]
- DiMaggio PJ, Powell WW. The iron cage revisited: Institutional isomorphism and collective rationality in organizational fields. American Sociological Review. 1983;48:147–160. [Google Scholar]
- Ducharme LJ, Knudsen HK, Roman PM. Evidence-based treatment for opiate- dependent clients: Availability, variation, and organizational correlates. The American Journal of Drug and Alcohol Abuse. 2007;32:569–576. doi: 10.1080/00952990600920417. [DOI] [PubMed] [Google Scholar]
- Ducharme LJ, Knudsen HK, Roman PM, Johnson JA. Innovation adoption in substance abuse treatment: Exposure, trialability, and the Clinical Trials Network. Journal of Substance Abuse Treatment. 2006;32:321–329. doi: 10.1016/j.jsat.2006.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ely JW, Osheroff JA, Ebell MH, Chambliss ME, Vinson DC, Stevermer JL, et al. Obstacles to answering doctors’ questions about patient care with evidence: Qualitative study. British Medical Journal. 2002;324:710–713. doi: 10.1136/bmj.324.7339.710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fahey L, Narayanan VK. Linking changes in revealed causal maps and environmental change: An empirical study. Journal of Management Studies. 1989;26(4):361–378. [Google Scholar]
- Gatignon H, Robertson TS. Technology diffusion: An empirical test of competitive effects. Journal of Marketing. 1989;53(1):35–49. [Google Scholar]
- Goes JB, Ho Park S. Interorganizational links and innovation: The case of hospital services. Academy of Management Journal. 1997;40(3):673–696. [Google Scholar]
- Greco AJ, Fields DM. Profiling early triers of service innovations: A look at interactive home video ordering services. Journal of Services Marketing. 1991;5(3):19–26. [Google Scholar]
- Griffith JR, Sahney VK, Mohr RA. Reengineering health care: Building on CQU. Ann Arbor, MI: Health Administration Press; 1995. [Google Scholar]
- Ibarra H. Network centrality, power, and innovation involvement: Determinants of technical and administrative roles. Academy of Management Journal. 1993;36(3):471–501. [Google Scholar]
- Jones MI, Greenfield SM, Bradley CP. Prescribing new drugs: Qualitative study of influences on consultants and general practitioners. British Medical Journal. 2001;323:378–381. doi: 10.1136/bmj.323.7309.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimberly JR, Evanisko MJ. Organizational innovation: The influence of individual, organizational, and contextual factors on hospital adoption of technological and administrative innovations. Academy of Management Journal. 1981;24:689–713. [PubMed] [Google Scholar]
- Kirchmayer U, Davoli M, Verster AD, Amato L, Ferri M, Perucci CA. A systematic review on the efficacy of naltrexone maintenance treatment in opiod dependence. Addiction. 1997;97:1241–1249. doi: 10.1046/j.1360-0443.2002.00217.x. [DOI] [PubMed] [Google Scholar]
- Knudsen HK, Roman PM. Modeling the use of innovations in private treatment organizations: The role of absorptive capacity. Journal of Substance Abuse Treatment. 2004;26:353–361. doi: 10.1016/s0740-5472(03)00158-2. [DOI] [PubMed] [Google Scholar]
- Knudsen HK, Roman PM, Ducharme LJ, Johnson JA. Organizational predictors of pharmacological innovation adoption: The case of disulfiram. Journal of Drug Issues. 2005;35:559–574. [Google Scholar]
- Knudsen HK, Ducharme LJ, Roman PM. Early adoption of buprenorphine in substance abuse treatment centers: Data from the private and public sectors. Journal of Substance Abuse Treatment. 2006;30:363–373. doi: 10.1016/j.jsat.2006.03.013. [DOI] [PubMed] [Google Scholar]
- Knudsen HK, Ducharme LJ, Roman PM. The adoption of medications in substance abuse treatment: Associations with organizational characteristics and technology clusters. Drug and Alcohol Dependence. 2007;87:164–174. doi: 10.1016/j.drugalcdep.2006.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krystal JH, Cramer JA, Krol WF, Kirk GF, Rosenheck RA. Naltrexone in the treatment of alcohol dependence. New England Journal of Medicine. 2001;345(24):1734–1739. doi: 10.1056/NEJMoa011127. [DOI] [PubMed] [Google Scholar]
- Lamb S, Greenlick MR, McCarty D, editors. Bridging the gap between practice and research: Forging partnerships with community-based drug and alcohol treatment. Washington, DC: National Academy Press; 1998. [PubMed] [Google Scholar]
- Lehman WEK, Greener JM, Simpson DD. Assessing organizational readiness for change. Journal of Substance Abuse Treatment. 2002;22:197–209. doi: 10.1016/s0740-5472(02)00233-7. [DOI] [PubMed] [Google Scholar]
- Ling W, Wesson DR. Naltrexone treatment for addicted health care professionals: A collaborative private practice experience. Journal of Clinical Psychiatry. 1984;45(9):46–48. [PubMed] [Google Scholar]
- Long JS, Freese J. Regression models for categorical dependent variables using Stata. College Station, TX: Stata Press Publication; 2001. [Google Scholar]
- Magura S, Schildhaus S, Rosenblum A, Gastfriend D. Substance user treatment program quality: Selected topics. Substance Use and Misuse. 2002;37:1185–1214. doi: 10.1081/ja-120004179. [DOI] [PubMed] [Google Scholar]
- Martinez E, Polo Y, Flavian C. The acceptance and diffusion of new consumer durables: differences between first and last adopters. Journal of Consumer Marketing. 1998;15(4):323–334. [Google Scholar]
- McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1698–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- Meyer M, Johnson JD, Ethington C. Contrasting attributes of preventive health innovations. Journal of Communication. 1997;47(2):112–131. [Google Scholar]
- Mohr R. An institutional perspective on rational myths and organizational change in health care. Medical Care Reviews. 1992;49:233–255. doi: 10.1177/002570879204900205. [DOI] [PubMed] [Google Scholar]
- Nohria N, Eccles RG. Networks and organizations. Boston: Harvard Business School Press; 1992. [Google Scholar]
- O’Brien CP, Volpicelli LA, Volpicelli JR. Naltrexone in the treatment of alcoholism: A clinical review. Alcohol: An International Biomedical Journal. 1996;13(1):35–39. doi: 10.1016/0741-8329(95)02038-1. [DOI] [PubMed] [Google Scholar]
- Oliver C. Determinants of interorganizational relationships: Integration and future directions. Academy of Management Review. 1990;15:241–265. [Google Scholar]
- O’Malley SS, Jaffe A, Chang G, Schottenfeld RS, Meyer RE, Rounsaville BJ. Naltrexone and coping skills therapy for alcohol dependence: A controlled study. Archives of General Psychiatry. 1992;49:881–887. doi: 10.1001/archpsyc.1992.01820110045007. [DOI] [PubMed] [Google Scholar]
- O’Neill HM, Pouder RW, Buchholtz AK. Patterns in the diffusion of strategies across organizations: Insights from the innovation diffusion literature. Academy of Management Review. 1998;23(1):98–114. [Google Scholar]
- Oser CB, Roman PM. Organizational-level predictors of adoption across time: Naltrexone in private addiction treatment centers. Journal of Studies on Alcohol and Drugs. doi: 10.15288/jsad.2007.68.852. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oser C, Staton Tindall M, Leukefeld C. HIV/AIDS testing in correctional agencies and community treatment programs: The impact of internal organizational structure. Journal of Substance Abuse Treatment. 2007;32:301–310. doi: 10.1016/j.jsat.2006.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oslin DW, Pettinati HM, Volpicelli JR, Wolf AL, Kampman KM, O’Brien CP. The effects of naltrexone on alcohol and cocaine use in dually addicted patients. Journal of Substance Abuse Treatment. 1999;16(2):163–167. doi: 10.1016/s0740-5472(98)00039-7. [DOI] [PubMed] [Google Scholar]
- Rai A, Ravichandran T, Samaddar S. How to anticipate the internet’s global diffusion. Communications of the ACM. 1998;41(10):97–106. [Google Scholar]
- Rogers EM. Categorizing the adopters of agricultural practices. Rural Sociology. 1958;23(4):346–354. [Google Scholar]
- Rogers EM. Diffusion of innovations. 5. New York: The Free Press; 2003. [Google Scholar]
- Roman PM, Johnson JA. Adoption and implementation of new technologies in substance abuse treatment. Journal of Substance Abuse Treatment. 2002;22:1–8. doi: 10.1016/s0740-5472(02)00241-6. [DOI] [PubMed] [Google Scholar]
- Stine SM, Kosten TR. New treatments for opiate dependence. New York: The Guilford Press; 1997. [Google Scholar]
- Thomas JB, Trevino LK. Information processing in strategic alliance building: A multiple-case approach. Journal of Management Studies. 1993;30:779–814. [Google Scholar]
- Volpicelli JR, Alterman AI, Hayashida M, O’Brien CP. Naltrexone in the treatment of alcohol dependence. Archives of General Psychiatry. 1992;49:876–880. doi: 10.1001/archpsyc.1992.01820110040006. [DOI] [PubMed] [Google Scholar]
- Volpicelli JR, Rhines KC, Rhines JS, Volpicelli LA, Alterman AI, O’Brien CP. Naltrexone and alcohol dependence. Archives of General Psychiatry. 1997;54:737–742. doi: 10.1001/archpsyc.1997.01830200071010. [DOI] [PubMed] [Google Scholar]
- Washton AM, Pottash AC, Gold MA. Naltrexone in addicted business executives and physicians. Journal of Clinical Psychiatry. 1984;45(9):39–41. [PubMed] [Google Scholar]
- Westphal JD, Gulati R, Shortell SM. Customization or conformity? An institutional and network perspective on the content and consequences of TQM adoption. Administrative Science Quarterly. 1997;42:366–394. [Google Scholar]
- Wolfe R, Gould W. An approximate likelihood-ratio test for ordinal response models. Stata Technical Bulletin. 1998;42:24–27. [Google Scholar]
- Yan Tam K. Dynamic price elasticity and the diffusion of mainframe computing. Journal of Management Information System. 1996;13(2):163–183. [Google Scholar]


