Abstract
OBJECTIVE
Chronic low-grade activation of the immune system (CLAIS) predicts type 2 diabetes via a decrease in insulin sensitivity. Our study investigated potential relationships between nuclear factor-κB (NF-κB) and c-Jun NH2-terminal kinase (JNK) pathways—two pathways proposed as the link between CLAIS and insulin resistance.
RESEARCH DESIGN AND METHODS
Adiposity (dual-energy X-ray absorptiometry), waist-to-hip ratio (WHR), and insulin sensitivity (M, hyperinsulinemic-euglycemic clamp) were measured in 22 healthy nondiabetic volunteers (aged 29 ± 11 years, body fat 28 ± 11%). NF-κB activity (DNA-binding assay) and JNK1/2 activity (phosphorylated JNK) were assessed in biopsies of the vastus lateralis muscle and subcutaneous adipose tissue and in peripheral blood mononuclear cell (PBMC) lysates.
RESULTS
NF-κB activities in PBMCs and muscle were positively associated with WHR after adjustment for age, sex, and percent body fat (both P < 0.05). NF-κB activity in PBMCs was inversely associated with M after adjustment for age, sex, percent body fat, and WHR (P = 0.02) and explained 16% of the variance of M. There were no significant relationships between NF-κB activity and M in muscle or adipose tissue (both NS). Adipose-derived JNK1/2 activity was not associated with obesity (all P> 0.1), although it was inversely related to M (r = −0.54, P < 0.05) and explained 29% of its variance. When both NF-κB and JNK1/2 were examined statistically, only JNK1/2 activity in adipose tissue was a significant determinant of insulin resistance (P = 0.02).
CONCLUSIONS
JNK1/2 activity in adipose tissue but not NF-κB activity in PBMCs is an independent determinant of insulin resistance in healthy individuals.
Chronic low-grade activation of the immune system (CLAIS) (i.e., increased plasma inflammatory markers without overt signs of inflammation) is suggested to play an etiological role in the development of type 2 diabetes. Support for this hypothesis is derived from cross-sectional (1–3) and prospective (4–7) studies demonstrating associations between elevation in markers of inflammation and obesity, insulin resistance, and/or type 2 diabetes. We provided the first prospective evidence in healthy, normal glucose tolerant individuals that CLAIS may contribute to the development of type 2 diabetes by causing a decline in insulin sensitivity (7), which has since been confirmed by two other studies (6,8). However, the exact mechanisms whereby activation of the immune system could contribute to insulin resistance are not completely understood. The nuclear factor-κB (NF-κB)/inhibitor of κB (IκB) kinase (IKK) β (7) and c-Jun NH2-terminal kinase (JNK) pathways (9) have been proposed as two possible links between activation of the immune system and the development of insulin resistance and type 2 diabetes.
NF-κB is a sequence-specific transcription factor most commonly found as a heterodimer of p65 (RelA) and p50, which induces the transcription of inflammatory genes (10,11) and other genes that may alter insulin action (12). NF-κB is maintained in the cytoplasm through interaction with inhibitory proteins, the IκBs, which are rapidly degraded upon phosphorylation by IKK. The inhibitory effect of NF-κB on insulin action is thought to be mediated by phosphorylation of serine residues of insulin receptor substrate (12). Recently, it has been shown that mice lacking IKK in peripheral blood mononuclear cells(PBMCs) are unable to translocate NF-κB, which protected them from systemic insulin resistance (13). This finding suggested for the first time that peripheral blood monocytes might be more important in the development of insulin resistance than skeletal muscle or adipose tissue.
Jun NH2-terminal kinases belong to a mitogen-activated protein kinase family that controls cell development and function by regulation of transcription by phosphorylating protein 1 complex proteins including c-Jun and JunB. There are three isoforms, with JNK1 and JNK2 being present in most cells and tissues (14). In particular, JNK1 appears to be the predominant isoform present in muscle, liver, and adipose tissues. JNK1 has been shown to interfere with insulin action in cultured cells (15); JNK activity is abnormally elevated in obesity, and an absence of JNK1 results in decreased adiposity, improved insulin sensitivity, and enhanced insulin receptor signaling in two different mouse models of obesity (9). Therefore, JNK1 is now considered an important player in the modulation of insulin action and a critical component of the pathogenesis of obesity, insulin resistance, and type 2 diabetes (9).
There is a paucity of data exploring the hypothesis that either or both of these pathways play a role in CLAIS-induced insulin resistance in humans. In particular, no study investigated these pathways in healthy individuals before they develop diabetes, which is essential with respect to etiology of insulin resistance. An association between NF-κB activation and glucose metabolism has been suggested in patients with type 2 diabetes, in whom there was a 60% reduction in the protein levels of IKKβ and a parallel elevation of NF-κB activity in skeletal muscle biopsies, which correlated with insulin resistance (16). In another study in insulin-resistant women with polycystic ovary syndrome (a condition also associated with CLAIS) NF-κB expression correlated with 2-h glucose levels (17). Furthermore, increased NF-κB activity in mononuclear cells has been shown in patients with type 2 diabetes (18,19) as well as in obese individuals (20). However, none of these studies investigated NF-κB activity in relation to direct assessment of insulin sensitivity, as measured by the hyperinsulinemic-euglycemic clamp. With regard to JNK1 activity, we have also previously shown that obese insulin-resistant humans (insulin sensitivity assessed by homeostasis model assessment [HOMA]) have increased JNK phosphorylation in skeletal muscle (21). Only one other study demonstrated that JNK1 activity in skeletal muscle was increased in obesity and type 2 diabetes and was an independent determinant of insulin resistance as measured by euglycemic clamp (22), but in that study adipose tissue and PBMCs were not examined.
Thus far, no studies have investigated the relative contribution of NF-κB and JNK pathways to development of insulin resistance in humans. Because it is likely that the relationship between CLAIS and insulin resistance can be initiated and perpetuated systemically by cross talk among insulin-sensitive tissues, i.e., adipose tissue, skeletal muscle, liver, and circulating immune cells, we sought to investigate these pathways in relation to insulin resistance in skeletal muscle, adipose tissue, and PBMCs. Therefore, we hypothesized that sustained activation of NF-κB and/or JNK1 in PBMCs and/or insulin-sensitive tissues such as skeletal muscle and subcutaneous adipose tissue contributes to development of insulin resistance in nondiabetic and otherwise healthy individuals.
RESEARCH DESIGN AND METHODS
Twenty-two volunteers (10 women) aged between 18 and 50 years underwent a rigorous protocol using standard measures of obesity and insulin resistance. Specifically, participants were nondiabetic (normal glucose tolerance or impaired glucose tolerance) according to an oral glucose tolerance test (OGTT) (World Health Organization 1999 criteria), nonsmokers at the time of the study, and healthy according to a detailed physical examination and routine blood analyses. No participants had clinical or laboratory signs of acute or chronic infection or took any medication or used illicit drugs at the time of the study. The protocol was approved by the Alfred Hospital Ethics Committee and complied with the Declaration of Helsinki 2004. All subjects provided written informed consent before participation. All participants were characterized for plasma inflammation markers, body composition, glucose tolerance, insulin action, and NF-κB and JNK1 activity in PBMCs and muscle and adipose tissue (Table 1).
TABLE 1.
Anthropometric and metabolic parameters of the study population
| All | Women | Men | |
|---|---|---|---|
| n | 22 | 10 | 12 |
| Age (years) | 29 ± 11 | 31 ± 12 | 27 ± 10 |
| Weight (kg) | 75 ± 11 | 71 ± 12 | 79 ± 9 |
| BMI (kg/m2) | 25 ± 4 | 25 ± 4 | 26 ± 4 |
| Waist circumference (cm) | 84 ± 10 | 82 ± 11 | 85 ± 10 |
| WHR | 0.85 ± 0.08 | 0.82 ± 0.07 | 0.88 ± 0.08 |
| Body fat (%) | 28 ± 11 | 36 ± 7 | 22 ± 9* |
| Fasting glucose (mmol/l) | 4.5 ± 0.5 | 4.3 ± 0.4 | 4.7 ± 0.5 |
| 2-h glucose (mmol/l) | 4.6 ± 1.3 | 4.7 ± 1.6 | 4.6 ± 1.1 |
| M(mg· kg−1· min−1) | 10.3 ± 4.4 | 10.7 ± 5.3 | 9.9 ± 3.8 |
| White blood cells (109/l) | 5.8 ± 1.0 | 5.8 ± 1.1 | 5.9 ± 1.0 |
| hsCRP (mg/l) | 1.1 ± 1.1 | 1.4 ± 1.2 | 0.9 ± 0.9 |
| MCP-1 (ng/ml) | 15.3 ± 17.5 | 10.7 ± 11.7 | 19.1 ± 20.0 |
| ALT (units/l) | 17 ± 9 | 13 ± 4 | 20 ± 10 |
| GGT (units/l) | 21 ± 14 | 16 ± 5 | 26 ± 18 |
Data are means ± SD.
*P< 0.05 male vs. female subjects.
All subjects underwent medical screening, which included history, physical examination, and basic laboratory tests (including fasting plasma lipid levels, liver function tests, urea, creatinine, and electrolyte levels, urinary illicit drug screening, an anthropometric assessment, an OGTT, and a hyperinsulinemic-euglycemic glucose clamp. Before metabolic testing, participants were asked to abstain from strenuous exercise and caffeine for 3 days. All of the metabolic testing was performed after a 12-h overnight fast.
Anthropometric measurements.
Body composition was estimated by total-body dual-energy X-ray absorptiometry (DPX-L; Lunar Radiation, Madison, WI) with calculations of percent body fat, fat mass, and fat-free mass as described previously (11). Waist and hip circumferences were measured and waist-to-hip ratio (WHR) was calculated as an index of body fat distribution.
Metabolic studies.
A 2-h 75-g OGTT was performed after a 12-h overnight fast, and glucose tolerance status was determined by World Health Organization 1999 criteria. Plasma glucose concentrations were determined by the glucose oxidase method (ELM 105; Radiometer, Copenhagen, Denmark).
Insulin action was assessed at physiological insulin concentrations during a hyperinsulinemic-euglycemic clamp. In brief, after an overnight fast, a primed continuous intravenous insulin infusion (9 mU/kg) was administered for 120 min at a constant rate of 40 mU/m2body surface area per minute (M). Plasma glucose was measured every 5 min during the clamp, and the variable infusion rate of glucose was adjusted to maintain blood glucose at a constant value of 5 mmol/l. This infusion achieved steady-state plasma insulin concentrations. The rate of total insulin-stimulated glucose disposal (M) was calculated for the last 40 min of the insulin infusions. Blood samples for analysis of inflammation markers were drawn before the start of the glucose clamp.
Muscle and adipose tissue biopsies.
Biopsies of subcutaneous adipose and vastus lateralis muscle were performed on a separate day using standard aseptic technique and local anesthesia. In brief, before a percutaneous muscle biopsy of the vastus lateralis muscle, a scalpel blade was used to make a 7-mm skin incision and to cut the fascia. A side-cutting muscle biopsy needle was passed through the incision to obtain ∼100 mg of muscle tissue. Adipose tissue was obtained by needle biopsy from the abdominal area, 1–2 cm superior to McBurney's point. After making an ∼5-mm skin incision, the needle biopsy was performed using a 50-ml plastic syringe attached to a 13-gauge aspiration needle. The muscle and adipose tissues were immediately placed in liquid nitrogen and then stored at −80°C.
Blood sample analysis.
Blood samples were drawn using standard phlebotomy techniques into sodium citrate Vacutainers for measurement of inflammatory markers. The tubes were centrifuged immediately (1,500g, 15 min, 4°C), and the plasma was stored at −80°C until analyses were performed. Monocyte chemoattractant protein-1 (MCP-1) was measured using a Beadlyte plex kit (Upstate Cell Signaling Solutions, Charlottesville, VA). Multiplexed assays were run according to the manufacturer's instructions on a Luminex 100 Bioplex machine using Luminex Pro software version 1.7 (Bio-Rad, Atherton, CA). Plasma high-sensitivity C-reactive protein (hsCRP) was measured by an immunoturbidimetric assay. Hepatic enzymes, alanine aminotransferase (ALT) and γ-glutamyltranspeptidase (GGT), were measured by NADH (without P-5′-P) andl-γ-glutamyl-3-carboxy-4-nitroanilide substrates, respectively. hsCRP and hepatic enzymes (ALT and GGT) were measured by Alfred Hospital Pathology Services using the Architect system (Abbott Diagnostics, Abbott Park, IL).
NF-κB activity measurements.
PBMCs were isolated from whole blood using Ficoll-Paque Plus density centrifugation (Amersham Biosciences, Uppsala, Sweden). The PBMC pellet was resuspended in FBS with 10% DMSO and stored at −80°C.
Nuclear extraction from PBMCs and adipose and skeletal muscle tissue was performed. Briefly, muscle and adipose tissue biopsy samples were homogenized in a 1:5 w/v ice-cold homogenization buffer (50 mmol/l Tris-HCl, pH 7.8, 10 mmol/l EDTA, pH 8.0, 100 mmol/l NaF, 2 mmol/l Na3 VO4, 1 mmol/l sodium pyrophosphate, 250 μmol/l phenylmethylsulfonyl fluoride, 10 μg/ml aprotinin, and 10 μg/ml leupeptin) with a hand-held homogenizer (Polytron-Aggregate; Kinematica, Switzerland). Samples were then rotated for 30 min, end-over-end, at 4°C, before being centrifuged (14,000g, 30 min, 4°C) to isolate the nuclear pellet. The nuclear pellet was then resuspended in 500 μl buffer A (10 mmol/l HEPES, pH 7.9, 10 mmol/l KCI, 0.1 mmol/l EDTA, 0.1 mmol/l EGTA, and 0.7% v/v IGEPAL), vortexed and centrifuged (7,000g, 1 min, room temperature), and then resuspended in 500 μl buffer B (10 mmol/l HEPES, pH 7.9, 10 mmol/l KCI, 0.1 mmol/l EDTA, and 0.1 mmol/l EGTA). Supernatant was removed, and the pellet was resuspended in 150 μl buffer C (20 mmol/l HEPES, pH 7.9, 400 mmol/l NaCl, 1 mmol/l EDTA, and 1 mmol/l EGTA), incubated on ice for 20 min, and then centrifuged (10,000g, 30 min, room temperature). The resulting supernatant was used in the NF-κB DNA-binding assay.
PBMC samples were washed in excess PBS and centrifuged (400g, 5 min, 4°C), to remove residual FBS and DMSO. The supernatant was discarded, and the pellets were resuspended in 100 μl triple detergent buffer (50 mmol/l Tris-HCl, pH 8.0, 150 mmol/l NaCl, 0.02% NaN3, 0.1% SDS, 100 μg/ml phenylmethylsulfonyl fluoride, 1 μg/ml aprotinin, 1% Nonidet P-40, and 0.5% sodium deoxycholate, in Milli-Q H2 O). These were then sonicated for 1 min and centrifuged (400g, 3 min, 4°C). The resulting supernatant was used in the NF-κB assay. The protein concentration of all protein isolates was determined using the bicinchoninic acid protein assay (Pierce, Rockford, IL), performed according to the manufacturer's instructions.
The TransAM NFκB DNA-binding activity assay (Active Motif, Carlsbad, CA) was used to detect and quantify NF-κB transcription factor activation, specifically of the p65 subunit. Nuclear extracts obtained from muscle (1 μg protein/well) and adipose tissue (5 μg protein/well) biopsies and PBMC (30 μg protein/well) samples were analyzed for their binding capacity to an NF-κB consensus sequence in labeled DNA in a 96-well plate format. The assays were performed according to the manufacturer's instructions, and absorbance was measured on a Victor3V Multilabel plate reader (PerkinElmer, Wellesley, MA). Results are expressed as nanograms of p65 activity per microgram of protein.
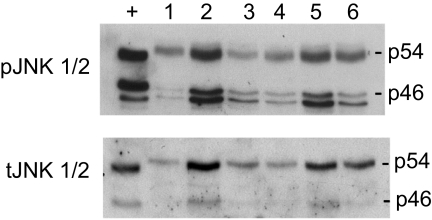
JNK1/2 activity measurements.
Phosphorylation of JNK ([Thr183/Tyr185 ]/total JNK) was used as a surrogate for JNK1/2 activity as described previously (21). PBMC, subcutaneous adipose tissue, and skeletal muscle samples were homogenized, and protein concentrations were determined. Total protein (40 μg) was separated by SDS-PAGE and blotted onto a polyvinylidene fluoride membrane. Blots were performed for phosphorylated JNK (1:1,000) and total JNK (1:1,000) using antibodies from Cell Signaling Technologies. Bands were visualized using a Bio-Rad anti-rabbit IgG horseradish peroxidase (1:4,000) conjugated antibody and ECL solution (Sigma) and developed on film. Bands were quantified using Quantity One Imaging software. JNK1/2 activity in muscle and adipose tissue was available for only 18 individuals because insufficient tissue was available for analyses.
Real-time analysis (RT-PCR).
Gene expression of the p65 subunit of NF-κB and IκBα in PBMCs was assessed by real-time quantitative RT-PCR, performed using the TaqMan system based on real-time detection of accumulated fluorescence (ABI Prism 7700 sequence detection system; PE Biosystems, Foster City, CA) as described previously (23). Briefly, 4 μg total RNA was isolated from PBMCs with TRIzol according to the manufacturer's instructions (Gibco BRL, Grand Island, NY). The resulting RNA was used to synthesize cDNA with a Superscript First Strand synthesis system (Gibco BRL). To control for variation in the amount of DNA available for PCR in the different samples, gene expression was normalized simultaneously (by multiplexing) in relation to the expression of the housekeeping gene 18S rRNA (18S rRNA TaqMan Control Reagent kit) as an endogenous control. Primers and TaqMan probes for the proteins described above were constructed with the help of Primer Express (PerkinElmer) (for sequences, see Table 2) and fluorescence for each cycle was quantitatively analyzed by an ABI Prism 7700 sequence detection system. Results are expressed as arbitrary units, related to minor groove binding (MGB) probe sample fluorescence, corrected to endogenous 18S expression.
TABLE 2.
Real-time RT-PCR probes and primers used for amplification of NF-κB p65 and IκBα in PBMCs
| Target | Probe | Forward primer 5′–3′ | Reverse primer 5′–3′ |
|---|---|---|---|
| NF-κB p65 | 6-FAM AGCTCAAGATCTGCCG | CTCATCCCATCTTTGACAATCGT | TGCACCTTGTCACACAGTAGGAA |
| IκBα | 6-FAM CTTCCAGAACAACCTGC | AGGGAGACCTGGCCTTCCT | TTCTGGCTGGTTGGTGATCA |
Statistical analysis.
Statistical analyses were performed using SAS Jump statistics software (SAS Institute, Cary, NC). Results are given as means ± SD (unless indicated otherwise). The values for inflammatory markers and M were logarithmically transformed before analysis to approximate normal distributions.
The relationships between inflammatory markers, NF-κB, JNK1/2, and anthropometric and metabolic variables were examined by calculating Pearson correlation coefficients, and P values were corrected for multiple comparisons (Benjamini-Hochberg procedure). Multiple linear regression models and partial correlations were used to examine the relationships after adjustment for covariates. Stepwise regression was used to determine a relative contribution of each of the variables to the model. Differences between men and women were assessed by unpaired Student's t test. Statistical significance was assumed when P < 0.05.
Our correlation tests are sufficiently sensitive at α = 0.05 with a power of 1 − β = 0.80 for two-sided correlations at r = 0.53 and for one-sided correlations at r = 0.48 (n = 22, degrees of freedom = 20). Because inflammation markers are known to be positively associated with obesity and negatively with insulin sensitivity, the one-sided calculation is most relevant to the current analyses. Post hoc statistical power calculations for the multiple regression models of our main findings, which all had R2>0.6, give power estimates greater than 0.90 for up to five independent variables in the model at α = 0.05.
RESULTS
The anthropometric and metabolic characteristics of the whole study population are summarized inTable 1. All subjects were deemed healthy according to their physical examination, were normotensive with normal lipid profile, full blood count, plasma CRP levels, liver function tests (Table 1), and renal function (estimated glomerular filtration rate >60 ml/min per m2), and therefore subclinical inflammation was ruled out. Women had higher percent body fat and HDL cholesterol levels, but there were no other sex differences seen among any of the other anthropometric and metabolic variables.
Relationship between NF-κB and JNK1/2 activity.
NF-κB activity in PBMCs was positively associated with NF-κB activity in the skeletal muscle (r = 0.68, P = 0.0004) but not in adipose tissue (r = −0.17, P = 0.4). JNK1/2 activity in PBMCs was not related to JNK1/2 activity in skeletal muscle (r = −0.14, P = 0.6) or subcutaneous adipose tissue (r = −0.34, P = 0.2). In addition, no relationship between JNK1/2 activity and NF-κB activity was identified in any of the tissues studied (all P> 0.2).
Relationship of NF-κB and JNK1/2 to inflammation markers.
White blood cell count (r = 0.39, P < 0.05) and plasma levels of MCP-1 (r = 0.63, P < 0.05) were each associated with NF-κB activity in PBMCs but not with NF-κB activity in the skeletal muscle or subcutaneous adipose tissue (Table 3). Plasma hsCRP (Table 3) was not related to NF-κB activity in any of the tissues investigated and did not correlate with insulin sensitivity (r = 0.20, P = 0.4). JNK1/2 activity was not associated with any of these markers of inflammation (P> 0.1).
TABLE 3.
Pearson correlation coefficients between NF-κB and JNK1/2 activity in PBMCs and muscle and adipose tissue with anthropometric and metabolic variables
| NF-κB |
JNK1/2 |
|||||
|---|---|---|---|---|---|---|
| PBMCs | Muscle | Adipose tissue | PBMCs | Muscle | Adipose tissue | |
| Age | −0.16 | −0.11 | 0.35 | −0.009 | −0.09 | 0.01 |
| % body fat | 0.20 | −0.09 | 0.21 | −0.14 | −0.12 | 0.07 |
| Waist | 0.17 | 0.29 | 0.08 | 0.06 | −0.29 | 0.32 |
| WHR | 0.48* | 0.68* | 0.03 | 0.14 | −0.40 | 0.04 |
| M | −0.46* | −0.29 | −0.15 | −0.08 | 0.23 | −0.54* |
| WBC | 0.39 | 0.20 | 0.18 | 0.13 | −0.20 | 0.04 |
| hsCRP | 0.11 | 0.13 | −0.03 | −0.41 | 0.39 | −0.002 |
| MCP-1 | 0.63* | 0.36 | 0.21 | 0.02 | 0.03 | 0.21 |
*P< 0.05. WBC, white blood cell count.
Relationship of NF-κB and JNK1/2 to obesity.
NF-κB activity in either PBMCs or skeletal muscle was not associated with an overall measure of obesity, percent body fat (Table 3,Fig. 1). NF-κB activity in subcutaneous adipose tissue also was not related to any of the anthropometric variables. Furthermore, the gene expression of IκBα and NF-κB (p65) in PBMC did not correlate with any of the anthropometric or metabolic parameters or NF-κB activity in PBMCs (data not shown). However, we found that NF-κB activity in both PBMCs and skeletal muscle was positively associated with WHR (r = 0.48, P = 0.02; r = 0.68, P = 0.003) (Table 3,Fig. 1) before and after adjustment for age and sex (both P < 0.05). This association persisted after additional adjustment for percent body fat (both P < 0.05). Tissue JNK1/2 activity was not related to any measures of obesity (both P> 0.1) (Table 3).
FIG. 1.
NF-κB p65 activity in PBMCs and central obesity, insulin sensitivity, and JNK1 activity in subcutaneous adipose tissue and insulin sensitivity. A: NF-κB p65 activity in PBMCs and WHR. B: NF-κB p65 activity in PBMCs and total body fat. C: NF-κB p65 activity in PBMCs and M. D: JNK1/2 activity and insulin sensitivity (M).
Relationship of NF-κB and JNK1/2 to insulin sensitivity.
NF-κB activity in PBMCs was inversely associated with insulin sensitivity before (r = −0.46, P = 0.03) (Table 3) and after adjustment for age, sex, percent body fat, and WHR (P = 0.02). In stepwise regression, elevated NF-κB activity in PBMCs explained 16% of the variance in the model after adjustment for the variables stated above. NF-κB activity in skeletal muscle and adipose tissue were not associated with insulin sensitivity (both P > 0.1).
JNK1/2 activity in the adipose tissue was related to insulin sensitivity (r = −0.54, P < 0.05) (Fig. 2) before and after adjustment for age, sex, percent body fat, and WHR (P = 0.04). In stepwise regression with age, sex, percent body fat, and WHR, JNK1/2 activity in adipose tissue explained the 29% variance in insulin sensitivity (P = 0.02). When both JNK1/2 in adipose tissue and NF-κB activity in PBMCs were entered in the same model, only JNK1/2 activity in adipose tissue remained a significant determinant of insulin sensitivity, explaining 29% (P = 0.02), whereas percent body fat contributed 21% (P = 0.02) and sex 10% (P = 0.07). When forced into this model, NF-κB activity in PBMCs explained only 4% of the variance in insulin sensitivity (P = 0.1). JNK1/2 activity in PBMCs and muscle was not associated with any measures of obesity or glucose metabolism (all P> 0.2). Exclusion of the two subjects with impaired glucose metabolism (one with impaired glucose tolerance and one with impaired fasting glucose) did not significantly alter the correlations presented.
FIG. 2.
Representative immunoblots of human adipose tissue (n = 6) probed for total JNK (tJNK) and phosphorylated JNK (pJNK, Thr183/Tyr185).
DISCUSSION
In the present study, we showed for the first time that, among healthy, nondiabetic individuals, both NF-κB activity in PBMCs and JNK1/2 activity in subcutaneous adipose tissue were important determinants of insulin resistance and explained 16 and 29%, respectively, of its variance after adjustment for appropriate covariates. Moreover, NF-κB activity in both PBMCs and skeletal muscle was also associated with central obesity.
The cross-sectional relationships between NF-κB activity in PBMCs and adiposity were consistent with previous findings in obese patients in whom NF-κB activity in PBMCs was elevated (20,24) and correlated with BMI (20,25). We added to the current evidence by showing this relationship across a wide range of adiposity. We also provided more precise measures of overall adiposity, specifically percent body fat by dual-energy X-ray absorptiometry as opposed to BMI, but, interestingly, our study showed that NF-κB activity in PBMCs was specifically associated with central obesity but not overall adiposity (measured as total percent body fat or BMI), perhaps because we have studied participants with a wide range of adiposity as opposed to only morbidly obese patients. In the above-mentioned studies (20,24), the relationship between central adiposity and NF-κB activity was not investigated. It is well established that central adiposity is a stronger predictor than overall adiposity of insulin resistance and progression to type 2 diabetes than overall adiposity and is likely to be responsible for the proinflammatory phenotype seen in these conditions (26–31). Thus, our additional findings showed for the first time a relationship between NF-κB activity in skeletal muscle and central obesity, suggesting that activation of the NF-κB/IκB pathway in muscle may contribute to a local inflammatory environment due to lipid accumulation and contributing to insulin resistance.
In accordance with two other studies (20,24), we also found a relationship between increased NF-κB activity in PBMCs and insulin resistance. In contrast to these studies, which used a calculated HOMA as a proxy for insulin resistance, we examined insulin resistance directly using the standard hyperinsulinemic-euglycemic clamp. Moreover, we showed that the relationship between NF-κB activity in PBMCs and insulin resistance is independent of the degree of obesity and explained 16% of variance in insulin resistance after adjustment for age, sex, percent body fat, and WHR. Although previous studies have shown that NF-κB activation in skeletal muscle is related to insulin resistance in obese humans (20,24), this was not seen in our study in nondiabetic healthy individuals. Our data are consistent with rodent studies in which overexpression of the p65 subunit of NF-κB in skeletal muscle had no effect on insulin resistance as measured by glucose clamp (32). In our study, we also found no relationship between activation of NF-κB in adipose tissue and any of the anthropometric or metabolic parameters. Animal models of type 2 diabetes have demonstrated an association between insulin resistance and elevated levels of the activator of NF-κB, IKKβ, at the gene level, in perigonadal but not in mesenteric adipose tissue (33). Gene levels of the inhibitor of NF-κB (IκBα) have also been associated with central adiposity in obese elderly women (34). Both of these studies (33,34), however, examined only gene expression as opposed to activity. The absence of an association between NF-κB activity in adipose tissue and anthropometric or metabolic parameters in the present study could also be due to differences in the populations examined. Both of the previously reported studies described the relationship in obese and insulin-resistant animals/populations (33,34), whereas our study was conducted in a healthy population.
Interestingly, NF-κB activity in PBMCs was associated with circulating MCP-1 levels but not with CRP. MCP-1 is one of the many downstream cytokine targets of the key proinflammatory transcription factor, NF-κB. MCP-1 is known to recruit white blood cells to the site of inflammation and therefore may be considered an important driver and perpetuator of NF-κB activation and inflammation (35). NF-κB activity in PBMCs and adipose tissue have been shown previously to correlate with the gene (20,34) and protein (20) expression of interleukin-6, macrophage inhibitory factor, and hsCRP in obese individuals. In our study, however, plasma levels of CRP were not associated with either NF-κB activity or insulin sensitivity probably because of the low plasma levels of CRP (all values within normal range) in our healthy nondiabetic population. Therefore, NF-κB may be a more sensitive early marker of inflammation than CRP in healthy individuals. We have made the novel observation that NF-κB activity in PBMCs is an important determinant of both central adiposity and insulin resistance. Interestingly, Arkan et al. (13) demonstrated that mice lacking IKK in PBMCs, which makes them unable to activate the NF-κB/IκB pathway, are protected from systemic insulin resistance. Our data demonstrated this relationship for the first time in humans.
To date, JNK1/2 activity has only been associated with obesity in animal models of obesity and diabetes (9). In this study, we showed that JNK1/2 activity in PBMCs, skeletal muscle, and subcutaneous adipose tissue was not associated with any measure of obesity in humans. Importantly, in the current study we also showed that JNK1/2 activity in subcutaneous adipose tissue was associated with insulin resistance, independently of age, sex, percent body fat, and WHR and explained 29% of the variance in insulin resistance after adjustment for these covariates. In this study, we have made the novel observation that when both NF-κB activity in PBMCs and JNK1/2 activity in subcutaneous adipose tissue are included in this model, only JNK1/2 activity was a significant determinant of insulin resistance, suggesting not only that these pathways are codependent but also that JNK1/2 activity is an independent and therefore potentially more important determinant of insulin resistance in nondiabetic, otherwise healthy individuals. JNK activity in skeletal muscle has been shown to be associated with insulin resistance in obese and diabetic subjects (22). We have also shown previously that obese insulin-resistant humans (insulin sensitivity assessed by HOMA) have increased JNK1/2 phosphorylation in skeletal muscle (21). In our present study, however, we did not see a relationship between JNK1/2 activity in skeletal muscle and insulin resistance, most likely because of our different study population, i.e., healthy nondiabetic individuals versus obese, type 2 diabetic subjects. Adipose tissue JNK activity was not examined in either of these previous studies (21,22), so we cannot compare our results in this regard. It could be hypothesized that different inflammatory pathways may be important in the initiation of insulin resistance as opposed to when diabetes has already developed. In our study, tissue JNK1/2 activity was not associated with circulating inflammatory makers, suggesting that tissue-specific inflammation and activation of JNK are enough to cause insulin resistance.
Our study has several limitations. First, because of the cross-sectional nature of the study, we cannot delineate the cause and effect relationships between JNK and NF-κB activity and insulin resistance. Second, the sample size is small, and, hence, the results should be interpreted with caution. However, the strength of the correlations and their robustness in various adjusted models attests to the validity of our findings. Third, standard imaging methods such as computed tomography or magnetic resonance imaging would have provided a better assessment of central adiposity than waist circumference.
In conclusion, we have demonstrated that elevated NF-κB activity in PBMCs and JNK1/2 activity in subcutaneous adipose tissue are both important determinants of insulin resistance in a healthy nondiabetic population. Moreover, we show that JNK1/2 activity in adipose tissue but not NF-κB activity in PBMC is an independent determinant of insulin resistance in this population. Further investigation is warranted to determine the mechanisms by which changes in NF-κB and JNK1/2 activity contribute to the development of type 2 diabetes in humans.
Acknowledgments
This work was supported by the National Health and Medical Research Council of Australia (Project, Fellowship and Centre for Clinical Research Excellence grants).
This work was also supported by the Bennelong Foundation and Pfizer Cardiovascular Lipid Research grants. No other potential conflicts of interest relevant to this article were reported.
We thank all volunteers for their participation in the study. We are grateful for the medical supervision of Stephen Duffy and the technical expertise of Kirsten Howlett, Melissa Formosa, Dona Onan, Brian Drew, Anna Gasser, Alaina Natoli, and Sally Penfold.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Pickup JC, Crook MA: Is type II diabetes mellitus a disease of the innate immune system? Diabetologia 1998; 41: 1241– 1248 [DOI] [PubMed] [Google Scholar]
- 2.Vozarova B, Stefan N, Hanson R, Lindsay RS, Bogardus C, Tataranni PA, Metz C, Bucala R: Plasma concentrations of macrophage migration inhibitory factor are elevated in Pima Indians compared to Caucasians and are associated with insulin resistance. Diabetologia 2002; 45: 1739– 1741 [DOI] [PubMed] [Google Scholar]
- 3.Vozarova B, Fernandez-Real JM, Knowler WC, Gallart L, Hanson RL, Gruber JD, Ricart W, Vendrell J, Richart C, Tataranni PA, Wolford JK: The interleukin-6 (−174) G/C promoter polymorphism is associated with type-2 diabetes mellitus in Native Americans and Caucasians. Hum Genet 2003; 112: 409– 413 [DOI] [PubMed] [Google Scholar]
- 4.Schmidt MI, Duncan BB, Sharrett AR, Lindberg G, Savage PJ, Offenbacher S, Azambuja MI, Tracy RP, Heiss G: Markers of inflammation and prediction of diabetes mellitus in adults (Atherosclerosis Risk in Communities study): a cohort study. Lancet 1999; 353: 1649– 1652 [DOI] [PubMed] [Google Scholar]
- 5.Freeman DJ, Norrie J, Caslake MJ, Gaw A, Ford I, Lowe GD, O'Reilly DS, Packard CJ, Sattar N: C-reactive protein is an independent predictor of risk for the development of diabetes in the West of Scotland Coronary Prevention Study. Diabetes 2002; 51: 1596– 1600 [DOI] [PubMed] [Google Scholar]
- 6.Festa A, D'Agostino R, Jr, Tracy RP, Haffner SM: Elevated levels of acute-phase proteins and plasminogen activator inhibitor-1 predict the development of type 2 diabetes: the insulin resistance atherosclerosis study. Diabetes 2002; 51: 1131– 1137 [DOI] [PubMed] [Google Scholar]
- 7.Vozarova B, Weyer C, Lindsay RS, Pratley RE, Bogardus C, Tataranni PA: High white blood cell count is associated with a worsening of insulin sensitivity and predicts the development of type 2 diabetes. Diabetes 2002; 51: 455– 461 [DOI] [PubMed] [Google Scholar]
- 8.Chen J, Wildman RP, Hamm LL, Muntner P, Reynolds K, Whelton PK, He J: Association between inflammation and insulin resistance in U.S. nondiabetic adults: results from the Third National Health and Nutrition Examination Survey. Diabetes Care 2004; 27: 2960– 2965 [DOI] [PubMed] [Google Scholar]
- 9.Hirosumi J, Tuncman G, Chang L, Gorgun CZ, Uysal KT, Maeda K, Karin M, Hotamisligil GS: A central role for JNK in obesity and insulin resistance. Nature 2002; 420: 333– 336 [DOI] [PubMed] [Google Scholar]
- 10.Sha WC: Regulation of immune responses by NF-κ B/Rel transcription factor. J Exp Med 1998; 187: 143– 146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jacque E, Tchenio T, Piton G, Romeo PH, Baud V: RelA repression of RelB activity induces selective gene activation downstream of TNF receptors. Proc Natl Acad Sci USA 2005; 102: 14635– 14640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shoelson SE, Lee J, Goldfine AB: Inflammation and insulin resistance. J Clin Invest 2006; 116: 1793– 1801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arkan MC, Hevener AL, Greten FR, Maeda S, Li ZW, Long JM, Wynshaw-Boris A, Poli G, Olefsky J, Karin M: IKK-β links inflammation to obesity-induced insulin resistance. Nat Med 2005; 11: 191– 198 [DOI] [PubMed] [Google Scholar]
- 14.Davis RJ: Signal transduction by the JNK group of MAP kinases. Cell 2000; 103: 239– 252 [DOI] [PubMed] [Google Scholar]
- 15.Aguirre V, Uchida T, Yenush L, Davis R, White MF: The c-Jun NH2-terminal kinase promotes insulin resistance during association with insulin receptor substrate-1 and phosphorylation of Ser307. J Biol Chem 2000; 275: 9047– 9054 [DOI] [PubMed] [Google Scholar]
- 16.Sriwijitkamol A, Christ-Roberts C, Berria R, Eagan P, Pratipanawatr T, DeFronzo RA, Mandarino LJ, Musi N: Reduced skeletal muscle inhibitor of κBβ content is associated with insulin resistance in subjects with type 2 diabetes: reversal by exercise training. Diabetes 2006; 55: 760– 767 [DOI] [PubMed] [Google Scholar]
- 17.Gonzalez F, Rote NS, Minium J, Kirwan JP: Increased activation of nuclear factor κB triggers inflammation and insulin resistance in polycystic ovary syndrome. J Clin Endocrinol Metab 2006; 91: 1508– 1512 [DOI] [PubMed] [Google Scholar]
- 18.Hofmann MA, Schiekofer S, Kanitz M, Klevesath MS, Joswig M, Lee V, Morcos M, Tritschler H, Ziegler R, Wahl P, Bierhaus A, Nawroth PP: Insufficient glycemic control increases nuclear factor-κB binding activity in peripheral blood mononuclear cells isolated from patients with type 1 diabetes. Diabetes Care 1998; 21: 1310– 1316 [DOI] [PubMed] [Google Scholar]
- 19.Adaikalakoteswari A, Rema M, Mohan V, Balasubramanyam M: Oxidative DNA damage and augmentation of poly(ADP-ribose) polymerase/nuclear factor-κB signaling in patients with type 2 diabetes and microangiopathy. Int J Biochem Cell Biol 2007; 39: 1673– 1684 [DOI] [PubMed] [Google Scholar]
- 20.Ghanim H, Aljada A, Hofmeyer D, Syed T, Mohanty P, Dandona P: Circulating mononuclear cells in the obese are in a proinflammatory state. Circulation 2004; 110: 1564– 1571 [DOI] [PubMed] [Google Scholar]
- 21.Chung J, Nguyen A-K, Henstridge DC, Holmes AG, Chan MHS, Mesa JL, Lancaster GI, Southgate RJ, Bruce CR, Duffy SJ, Horvath I, Mestril R, Watt MJ, Hooper PL, Kingwell BA, Vigh L, Hevener A, Febbraio MA: HSP72 protects against obesity-induced insulin resistance. Proc Natl Acad Sci USA 2008; 105: 1739– 1744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bandyopadhyay GK, Yu JG, Ofrecio J, Olefsky JM: Increased p85/55/50 expression and decreased phosphatidylinositol 3-kinase activity in insulin-resistant human skeletal muscle. Diabetes 2005; 54: 2351– 2359 [DOI] [PubMed] [Google Scholar]
- 23.Thomas MC, Tikellis C, Burns WM, Bialkowski K, Cao Z, Coughlan MT, Jandeleit-Dahm K, Cooper ME, Forbes JM: Interactions between renin angiotensin system and advanced glycation in the kidney. J Am Soc Nephrol 2005; 16: 2976– 2984 [DOI] [PubMed] [Google Scholar]
- 24.Dandona P, Aljada A, Mohanty P, Ghanim H, Hamouda W, Assian E, Ahmad S: Insulin inhibits intranuclear nuclear factor κB and stimulates IκB in mononuclear cells in obese subjects: evidence for an anti-inflammatory effect? J Clin Endocrinol Metab 2001; 86: 3257– 3265 [DOI] [PubMed] [Google Scholar]
- 25.Ghanim H, Aljada A, Daoud N, Deopurkar R, Chaudhuri A, Dandona P: Role of inflammatory mediators in the suppression of insulin receptor phosphorylation in circulating mononuclear cells of obese subjects. Diabetologia 2007; 50: 278– 285 [DOI] [PubMed] [Google Scholar]
- 26.Montague CT, O'Rahilly S: The perils of portliness: causes and consequences of visceral adiposity. Diabetes 2000; 49: 883– 888 [DOI] [PubMed] [Google Scholar]
- 27.Kabir M, Catalano KJ, Ananthnarayan S, Kim SP, Van Citters GW, Dea MK, Bergman RN: Molecular evidence supporting the portal theory: a causative link between visceral adiposity and hepatic insulin resistance. Am J Physiol Endocrinol Metab 2005; 288: E454– E461 [DOI] [PubMed] [Google Scholar]
- 28.Shen W, Punyanitya M, Chen J, Gallagher D, Albu J, Pi-Sunyer X, Lewis CE, Grunfeld C, Heshka S, Heymsfield SB: Waist circumference correlates with metabolic syndrome indicators better than percentage fat. Obesity (Silver Spring) 2006; 14: 727– 736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Manios Y, Moschonis G, Kourlaba G, Bouloubasi Z, Grammatikaki E, Spyridaki A, Hatzis C, Kafatos A, Fragiadakis GA: Prevalence and independent predictors of insulin resistance in children from Crete, Greece: the Children Study. Diabet Med 2008; 25: 65– 72 [DOI] [PubMed] [Google Scholar]
- 30.Onat A, Uyarel H, Hergenc G, Karabulut A, Albayrak S, Can G: Determinants and definition of abdominal obesity as related to risk of diabetes, metabolic syndrome and coronary disease in Turkish men: a prospective cohort study. Atherosclerosis 2007; 191: 182– 190 [DOI] [PubMed] [Google Scholar]
- 31.Toscani M, Migliavacca R, Sisson de Castro JA, Spritzer PM: Estimation of truncal adiposity using waist circumference or the sum of trunk skinfolds: a pilot study for insulin resistance screening in hirsute patients with or without polycystic ovary syndrome. Metabolism 2007; 56: 992– 997 [DOI] [PubMed] [Google Scholar]
- 32.Polkinghorne E, Lau Q, Cooney GJ, Kraegen EW, Cleasby ME: Local activation of the IκK-NF-κB pathway in muscle does not cause insulin resistance. Am J Physiol Endocrinol Metab 2008; 294: E316– E325 [DOI] [PubMed] [Google Scholar]
- 33.Bradley RL, Jeon JY, Liu FF, Maratos-Flier E: Voluntary exercise improves insulin sensitivity and adipose tissue inflammation in diet-induced obese mice. Am J Physiol Endocrinol Metab 2008; 295: E586– E594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zamboni M, Di Francesco V, Garbin U, Fratta Pasini A, Mazzali G, Stranieri C, Zoico E, Fantin F, Bosello O, Cominacini L: Adiponectin gene expression and adipocyte NF-κB transcriptional activity in elderly overweight and obese women: inter-relationships with fat distribution, hs-CRP, leptin and insulin resistance. Int J Obes (Lond) 2007; 31: 1104– 1109 [DOI] [PubMed] [Google Scholar]
- 35.Shoelson SE, Herrero L, Naaz A: Obesity, inflammation, and insulin resistance. Gastroenterology 2007; 132: 2169– 2180 [DOI] [PubMed] [Google Scholar]