Abstract
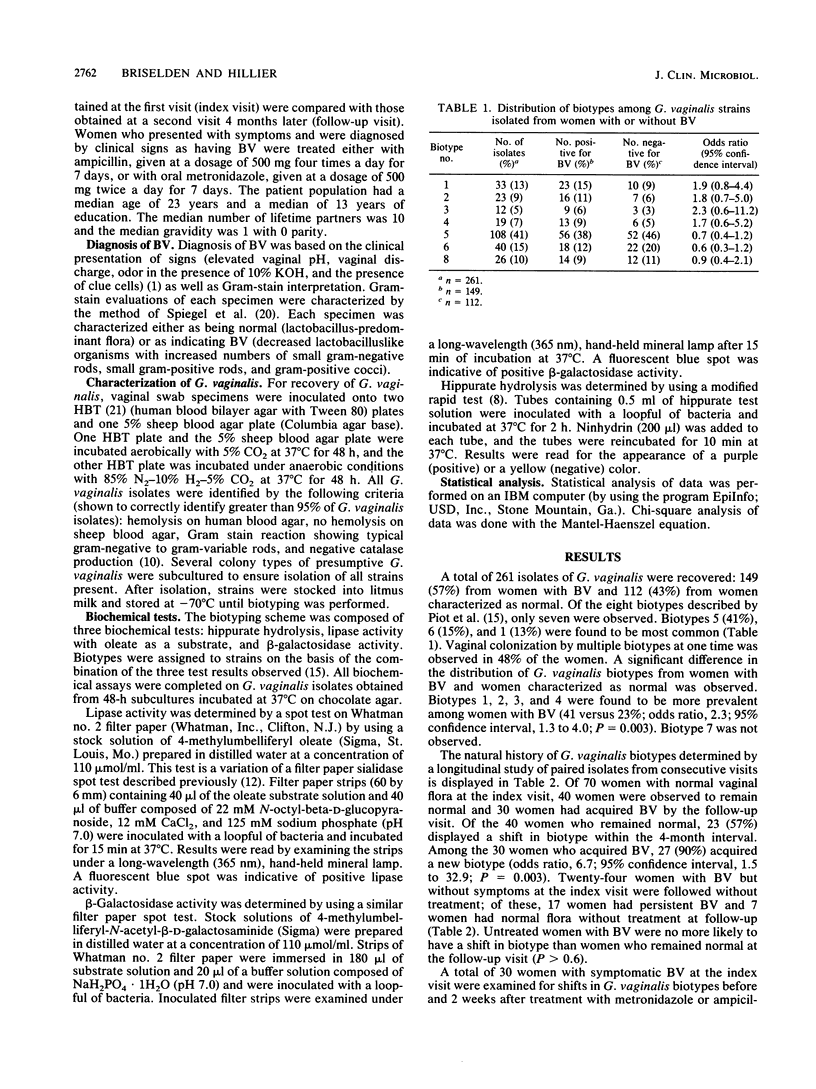
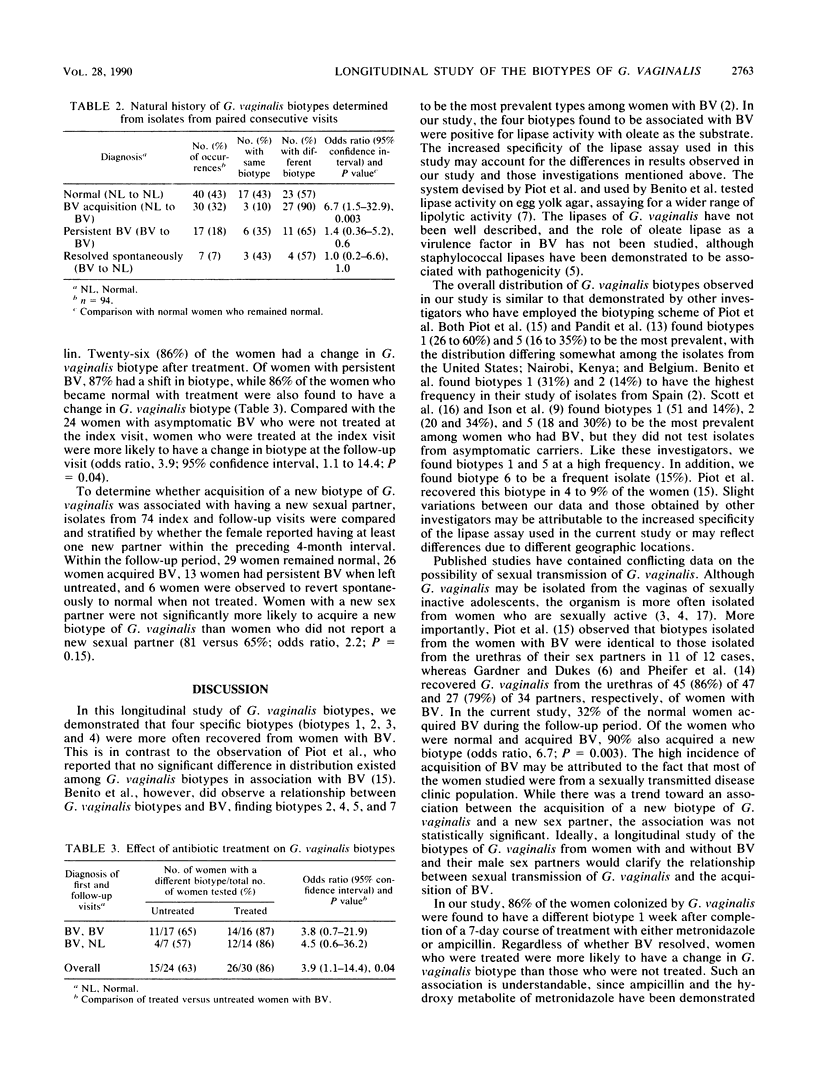
Gardnerella vaginalis is the predominant vaginal microorganism in women with bacterial vaginosis. However, this organism is also frequently isolated from women without signs or symptoms of vaginitis. Earlier studies have not revealed whether certain biotypes of G. vaginalis are more often associated with bacterial vaginosis or are more common in women who acquire bacterial vaginosis. We used a typing scheme based on tests for beta-galactosidase, hippurate hydrolysis, and lipase, using oleate as a substrate. Of 261 strains tested, the distribution of biotypes observed was as follows: 1, 13%; 2, 9%; 3, 5%; 4, 7%; 5, 41%; 6, 15%; and 8, 10%. Biotype 7 was not observed. The distributions of biotypes from women with and without bacterial vaginosis were found to be significantly different, with the lipase-positive biotypes (biotypes 1, 2, 3, and 4) being more predominant in women with vaginosis (41 versus 23%, P = 0.003). Of 40 women with normal vaginal flora at the index visit who remained normal at follow-up, 23 (57%) acquired a new biotype of G. vaginalis. By comparison, 90% of the 30 women who developed bacterial vaginosis acquired a new biotype of G. vaginalis (P = 0.003). Women with bacterial vaginosis at the index visit who were not treated were no more likely than normal women to have a shift in G. vaginalis biotype. However, 86% of the 30 women with bacterial vaginosis who were treated with an antibiotic at the index visit acquired a different biotype (P = 0.04 compared with the value for untreated women) regardless of treatment success. A trend toward the acquisition of a new biotype was observed among women who had contact with a new sexual partner (81 versus 65%, P = 0.15). These data demonstrate that the lipase-positive isolates of G. vaginalis are associated with bacterial vaginosis. Women who acquire bacterial vaginosis are more likely to have a shift in biotype than women who had normal flora at he follow-up, suggesting that the G. vaginalis isolates recovered from women who develop bacterial vaginosis represent newly acquired strains rather than overgrowth of previously colonizing biotypes.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Amsel R., Totten P. A., Spiegel C. A., Chen K. C., Eschenbach D., Holmes K. K. Nonspecific vaginitis. Diagnostic criteria and microbial and epidemiologic associations. Am J Med. 1983 Jan;74(1):14–22. doi: 10.1016/0002-9343(83)91112-9. [DOI] [PubMed] [Google Scholar]
- Benito R., Vazquez J. A., Berron S., Fenoll A., Saez-Neito J. A. A modified scheme for biotyping Gardnerella vaginalis. J Med Microbiol. 1986 Jun;21(4):357–359. doi: 10.1099/00222615-21-4-357. [DOI] [PubMed] [Google Scholar]
- Bump R. C., Buesching W. J., 3rd Bacterial vaginosis in virginal and sexually active adolescent females: evidence against exclusive sexual transmission. Am J Obstet Gynecol. 1988 Apr;158(4):935–939. doi: 10.1016/0002-9378(88)90097-x. [DOI] [PubMed] [Google Scholar]
- Bump R. C., Sachs L. A., Buesching W. J., 3rd Sexually transmissible infectious agents in sexually active and virginal asymptomatic adolescent girls. Pediatrics. 1986 Apr;77(4):488–494. [PubMed] [Google Scholar]
- GARDNER H. L., DUKES C. D. Haemophilus vaginalis vaginitis: a newly defined specific infection previously classified non-specific vaginitis. Am J Obstet Gynecol. 1955 May;69(5):962–976. [PubMed] [Google Scholar]
- Hillier S., Krohn M. A., Watts D. H., Wolner-Hanssen P., Eschenbach D. Microbiologic efficacy of intravaginal clindamycin cream for the treatment of bacterial vaginosis. Obstet Gynecol. 1990 Sep;76(3 Pt 1):407–413. [PubMed] [Google Scholar]
- Hwang M. N., Ederer G. M. Rapid hippurate hydrolysis method for presumptive identification of group B streptococci. J Clin Microbiol. 1975 Jan;1(1):114–115. doi: 10.1128/jcm.1.1.114-115.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ison C. A., Harvey D. G., Tanna A., Easmon C. S. Development and evaluation of scheme for serotyping Gardnerella vaginalis. Genitourin Med. 1987 Jun;63(3):196–201. doi: 10.1136/sti.63.3.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lien E. A., Hillier S. L. Evaluation of the enhanced rapid identification method for Gardnerella vaginalis. J Clin Microbiol. 1989 Mar;27(3):566–567. doi: 10.1128/jcm.27.3.566-567.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormack W. M., Hayes C. H., Rosner B., Evrard J. R., Crockett V. A., Alpert S., Zinner S. H. Vaginal colonization with Corynebacterium vaginale (Haemophilus vaginalis). J Infect Dis. 1977 Dec;136(6):740–745. doi: 10.1093/infdis/136.6.740. [DOI] [PubMed] [Google Scholar]
- Moncla B. J., Braham P., Hillier S. L. Sialidase (neuraminidase) activity among gram-negative anaerobic and capnophilic bacteria. J Clin Microbiol. 1990 Mar;28(3):422–425. doi: 10.1128/jcm.28.3.422-425.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandit D. V., Barve S. M., Deodhar L. P. Biotypes of Gardnerella vaginalis isolated from non-specific vaginitis patients in Bombay. Indian J Med Res. 1989 Nov;89:435–438. [PubMed] [Google Scholar]
- Pheifer T. A., Forsyth P. S., Durfee M. A., Pollock H. M., Holmes K. K. Nonspecific vaginitis: role of Haemophilus vaginalis and treatment with metronidazole. N Engl J Med. 1978 Jun 29;298(26):1429–1434. doi: 10.1056/NEJM197806292982601. [DOI] [PubMed] [Google Scholar]
- Piot P., Van Dyck E., Peeters M., Hale J., Totten P. A., Holmes K. K. Biotypes of Gardnerella vaginalis. J Clin Microbiol. 1984 Oct;20(4):677–679. doi: 10.1128/jcm.20.4.677-679.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott T. G., Smyth C. J., Keane C. T. In vitro adhesiveness and biotype of Gardnerella vaginalis strains in relation to the occurrence of clue cells in vaginal discharges. Genitourin Med. 1987 Feb;63(1):47–53. doi: 10.1136/sti.63.1.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shafer M. A., Sweet R. L., Ohm-Smith M. J., Shalwitz J., Beck A., Schachter J. Microbiology of the lower genital tract in postmenarchal adolescent girls: differences by sexual activity, contraception, and presence of nonspecific vaginitis. J Pediatr. 1985 Dec;107(6):974–981. doi: 10.1016/s0022-3476(85)80208-0. [DOI] [PubMed] [Google Scholar]
- Shanker S., Toohey M., Munro R. In vitro activity of seventeen antimicrobial agents against Gardnerella vaginalis. Eur J Clin Microbiol. 1982 Oct;1(5):298–300. doi: 10.1007/BF02019975. [DOI] [PubMed] [Google Scholar]
- Spiegel C. A., Amsel R., Eschenbach D., Schoenknecht F., Holmes K. K. Anaerobic bacteria in nonspecific vaginitis. N Engl J Med. 1980 Sep 11;303(11):601–607. doi: 10.1056/NEJM198009113031102. [DOI] [PubMed] [Google Scholar]
- Spiegel C. A., Amsel R., Holmes K. K. Diagnosis of bacterial vaginosis by direct gram stain of vaginal fluid. J Clin Microbiol. 1983 Jul;18(1):170–177. doi: 10.1128/jcm.18.1.170-177.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Totten P. A., Amsel R., Hale J., Piot P., Holmes K. K. Selective differential human blood bilayer media for isolation of Gardnerella (Haemophilus) vaginalis. J Clin Microbiol. 1982 Jan;15(1):141–147. doi: 10.1128/jcm.15.1.141-147.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]


