Abstract
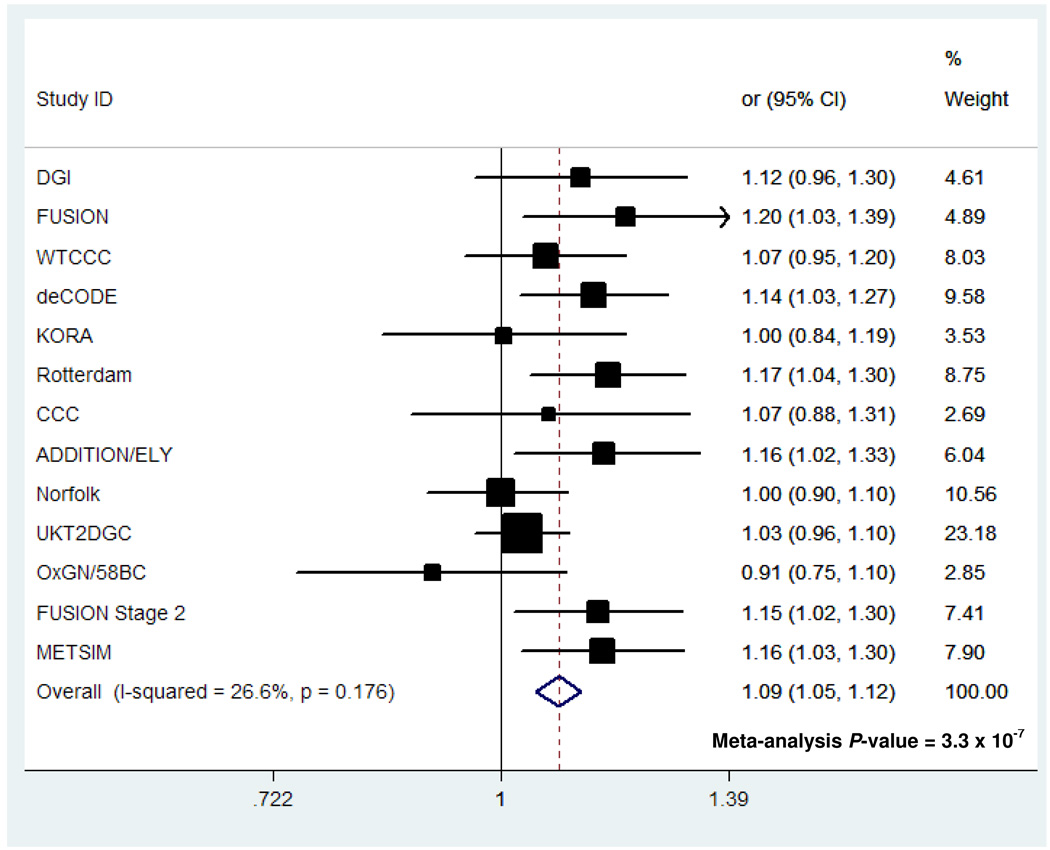
To identify novel genetic loci associated with fasting glucose concentrations, we examined the leading association signals in 10 genome-wide association scans involving a total of 36,610 individuals of European descent. Variants in the gene encoding the melatonin receptor 1B (MTNR1B) were consistently associated with fasting glucose across all ten studies. The strongest signal was observed at rs10830963, where each G-allele (frequency 0.30 in HapMap CEU) was associated with an increase of 0.07 (95%CI 0.06–0.08) mmol/L in fasting glucose levels (P=3.2×10−50) and reduced beta-cell function as measured by homeostasis model assessment (HOMA-B, P=1.1×10−15). The same allele was associated with an increased risk of type 2 diabetes (odds ratio = 1.09 (1.05–1.12), per G allele P=3.3×10−7) in a meta-analysis of thirteen case-control studies totalling 18,236 cases and 64,453 controls. Our analyses also confirm previous associations of fasting glucose with variants at the G6PC2 (rs560887, P=1.1×10−57) and GCK (rs4607517, P=1.0×10−25) loci.
Blood and plasma fasting glucose (FG) levels are usually tightly regulated within a narrow physiologic range by a feedback mechanism that targets a particular FG set point for each individual1,2. Disruption of normal glucose homeostasis and substantial elevations of FG are hallmarks of type 2 diabetes (T2D) and typically result from sustained reduction in pancreatic beta-cell function and insulin secretion.
However, even within healthy, non-diabetic populations there is substantial variation in FG levels. Approximately one-third of this variation is genetic3, but little of this heritability has been explained. There is growing evidence to suggest that common variants contributing to variation in FG are largely distinct from those associated with major disruptions of beta-cell function that predispose to T2D. Common sequence variants in the glucokinase (GCK) promoter4–6, and around genes encoding the islet specific glucose-6-phosphatase (G6PC2)5,6 and the glucokinase regulatory protein (GCKR)7–9 have each been associated with individual variation in FG levels, but have, at best, weak effects on T2D risk8,10. Furthermore, though there are now over 15 genetic loci strongly associated with the risk of T2D7,10–14, none shows compelling evidence for association with FG in the two genome-wide association scans (GWAS) so far reported5,6.
MAGIC (the Meta-Analyses of Glucose and Insulin-related traits Consortium) represents a collaborative effort to combine data from multiple GWAS to identify additional loci that impact on glycaemic and metabolic traits. Our genetic studies of FG levels originally coalesced into four distinct consortia: (i) European Network for Genetic and Genomic Epidemiology (ENGAGE), combining data from deCODE, Northern Finland Birth Cohort 1966 (NFBC1966), Netherlands Twins Register/Netherlands Study of Depression and Anxiety (NTR/NESDA), and the Rotterdam Study; (ii) Genetics of Energy Metabolism (GEM), a meta-analysis of the Lausanne (CoLaus) and TwinsUK scans; (iii) DFS, involving the Diabetes Genetics Initiative (DGI), Finland-United States Investigation of NIDDM Genetics (FUSION) and SardiNIA scans; and (iv) the Framingham Heart Study (FHS). Details of the ten component studies (n=1,233–6,479) are provided in Supplementary Table 1.
As a prelude to more extensive data-sharing, the four consortia initially exchanged the identities of between 10 and 20 SNPs prominently associated with FG in their individual, interim, meta-analyses (n=6,479–12,389: Supplementary Table 2). Comparison of these signals revealed three loci with consistent effects on FG detected in multiple studies. Two of these represented the previously reported signals in G6PC2 and GCK. In addition, all four groups independently generated evidence for an association between FG and SNPs around the MTNR1B (melatonin receptor 1B) locus (ENGAGE [rs1387153] P=2.2 × 10−17; GEM [rs10830963] P=7.4 × 10−11; DFS [rs10830963] P=2.5 × 10−7; FHS [rs11020107] P=5.8 × 10−4, for the most strongly associated SNP exchanged from each analysis). The association signals at all three loci were confirmed on formal meta-analysis including results from all 10 studies, after exclusion of individuals with known diabetes (rs560887 [G6PC2], P=1.1 × 10−57; rs4607517 [GCK], P=1.0 × 10−25; rs10830963 [MTNR1B], P=3.2 × 10−50) (Table 1, Supplementary table 3). Subsequent efforts to harmonize additional aspects of data analysis strategies (including the additional exclusion, where necessary, of individuals with FG measures >7mmol/l) had only a marginal impact on estimates of significance and effect size (Supplementary Table 4).
Table 1. Associatest SNPs across all ten studies for three fasting glucose loci (MTNR1B, G6PC2 and GCK).
FG levels (mmol/L) are reported untransformed and unadjusted for covariates. Effect of the risk allele and SE were calculated using untransformed FG values. P-values are reported for the additive genetic model with study-specific transformation of FG values, adjusted for gender and age).
| Study sample | N | G allele Frequency | Mean level of FG*** per genotype (SD), mmol/L | Per_allele effect (SE), mmol/L | P-value | ||
|---|---|---|---|---|---|---|---|
| CC | CG | GG | |||||
| CoLaus | 5,000 | 0.32 | 5.36 (0.71) | 5.46 (0.80) | 5.54 (0.81) | 0.094 (0.016) | 1.9 × 10−9 |
| deCODE | 6,240 | 0.27 | 5.29 (0.71) | 5.39 (0.71) | 5.44 (0.71) | 0.086 (0.016) | 9.2 × 10−8 |
| DGI | 1,455 | 0.31 | 5.29 (0.54) | 5.32 (0.53) | 5.39 (0.60) | 0.042 (0.022) | 0.054 |
| Framingham* | 6,479 | 0.28 | 5.16 (0.48) | 5.21 (0.48) | 5.26 (0.46) | 0.050 (0.012) | 2.2 × 10−13 |
| FUSION | 1,233 | 0.33 | 5.28 (0.49) | 5.33 (0.47) | 5.40 (0.44) | 0.057 (0.016) | 5.8 × 10−4 |
| NFBC1966 | 4,245 | 0.34 | 5.63 (0.46) | 5.70 (0.49) | 5.80 (0.46) | 0.079 (0.012) | 1.7 × 10−11 |
| NTR/NESDA | 3,166 | 0.27 | 5.22 (0.64) | 5.26 (0.62) | 5.38 (0.63) | 0.062 (0.019) | 1.2 × 10−3 |
| Rotterdam | 2,058 | 0.28 | 5.58 (0.81) | 5.75 (0.91) | 5.83 (1.03) | 0.145 (0.029) | 7.9 × 10−7 |
| Sardinia | 4,108 | 0.20 | 5.62 (0.89) | 5.68 (0.89) | 5.76 (0.89) | 0.070 (0.019) | 3.2 × 10−4 |
| TwinsUK** | 1,828 | 0.30 | 4.58 (0.65) | 4.67 (0.50) | 4.74 (0.57) | 0.084 (0.032) | 7.9 × 10−3 |
| rs10830963 (MTNR1B) | Meta-analysis | 0.072 (0.005) | 3.2 × 10−50 | ||||
| rs560887 (G6PC2) | Meta-analysis | 0.064 (0.004) | 1.1 × 10−57 | ||||
| rs4607517 (GCK) | Meta-analysis | 0.062 (0.007) | 1.0 × 10−25 | ||||
In Framingham study, mean FG values for the imputed SNPs are reported for proxies: rs560887 (proxy = rs573225, r2=0.96); rs4607517 (proxy = rs1799884, r2=1); rs10830963 (proxy = rs7936247, r2=0.59)
In the TwinsUK study, mean FG values per genotype are estimated for a subset of unrelated individuals only
FG levels in NFBC1966 and SardiNIA were measured in whole blood; in other samples measures were conducted on plasma samples. Values in the table are corrected to plasma FG using a correction factor of 1.13
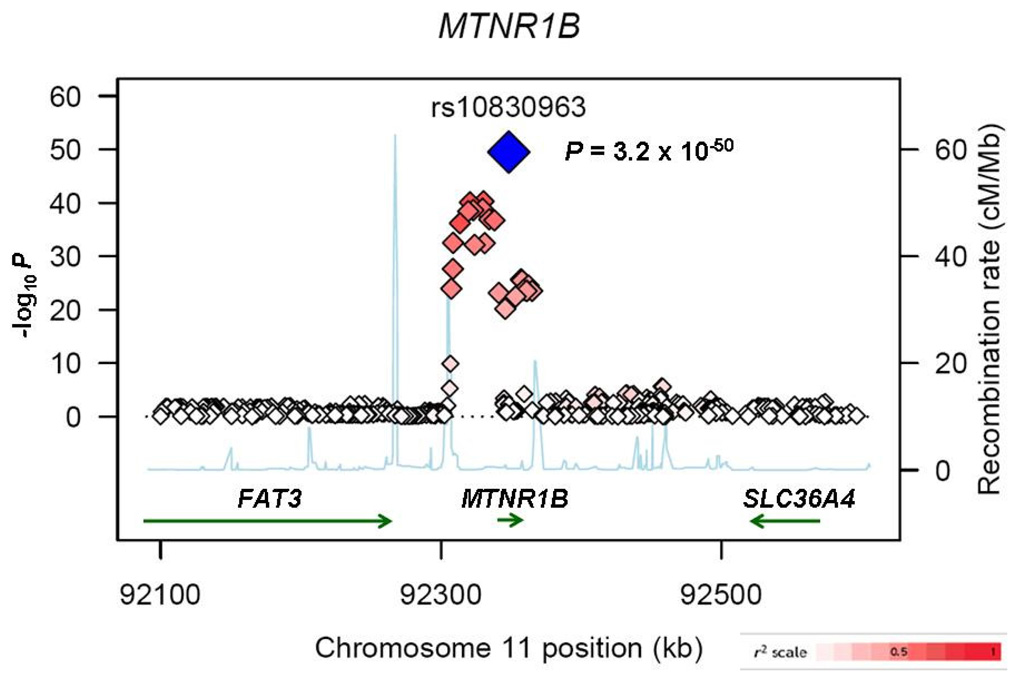
We attempted to refine the location of the MTNR1B association signal by extending the meta-analysis to all SNPs (genotyped and imputed from the HapMap) within the 1Mb region flanking the gene (n=35,812; 981 SNPs). In all, 30 genotyped and imputed SNPs showed compelling evidence for association with FG (P<10−8). The strongest signal was detected at rs10830963: the minor (G) allele (frequency 0.30 in HapMap CEU15) at this SNP was associated with a per-allele increase of 0.07 (95%CI 0.06–0.08) mmol/L in FG (P=3.2 × 10−50). Consistent evidence for association at rs10830963 was observed in all 10 component GWAS, irrespective of whether this SNP was genotyped or imputed, and the genotyping platform (Table 1, Supplementary Table 1). Repeat meta-analysis within the region after conditioning on rs10830963 revealed no additional independent signals of association (Supplementary Note).
The strength of the association between rs10830963 and FG was unchanged after adjustment for body mass index (Supplementary Table 4). Analyses of fasting insulin levels as well as indices of beta-cell function (HOMA-B) and insulin sensitivity (HOMA-IR) estimated by the homeostasis model assessment16 were possible in ~24,000 participants from the 10 studies. These established that the glucose-raising allele at rs10830963 was associated with reduced beta-cell function (P=1.1 × 10−15), with no appreciable effect on fasting insulin or insulin sensitivity (Supplementary Table 5, Supplementary Note).
To determine the impact of variants within MTNR1B on T2D risk, we performed a large-scale meta-analysis of thirteen T2D case-control samples (18,236 T2D cases, 64,453 controls; corresponding to an effective sample size of 21,179 unrelated cases and 21,179 unrelated controls). We combined data from the deCODE13, Rotterdam17, KORA18, FUSION Stage 211 and METSIM10 studies and from several case-control samples from the UK10 with publicly-available data from the DIAGRAM consortium (which itself aggregates GWA data from the WTCCC, DGI and FUSION scans)10 (Supplementary Note). We found strong evidence that the minor G-allele of rs10830963 was associated with increased risk of T2D (odds ratio=1.09 [1.05–1.12], P=3.3 × 10−7) (Supplementary Table 6 and Figure 2). The possibility that the FG association might reflect the inclusion within the cross-sectional study samples of subjects with undiagnosed T2D can be discounted given that exclusion of those with either known diabetes, or a FG exceeding 7mmol/l had little impact on the strength of the association signal (Table 1, Supplementary Table 4). Although the association with T2D does not, despite large-scale replication efforts, reach the 5×10−8 threshold consistent with “genome-wide significance”15, it seems highly probable, given the strong impact of this variant on beta-cell function (Supplementary Table 5), that this is a genuine effect.
Figure 2. Association of rs10830963 with type 2 diabetes (T2D) in thirteen case-control studies.
The analyses we performed interrogate only a minority of common sequence variants in a given region – it is likely that the causal variant for this locus is yet to be identified. The SNP with the strongest statistical evidence so far, rs10830963, maps within the single 11.5 kb intron of MTNR1B but does not appear to disrupt consensus transcription factor binding or cryptic alternative splice sites. The association signal is bounded by recombination hotspots defining a ~60kb interval within which all our strongly associated SNPs lie and the causal variant is likely to reside. This interval contains the entire coding region of MTNR1B. The only other nearby genes (the coding regions of which lie well outside this 60kb region) are SLC36A4 and FAT3, neither of which are compelling candidates. SLC36A4 encodes a proton/amino acid transmembrane transporter moderately similar to Rattus norvegicus lysosomal amino acid transporter 1, while FAT3 encodes a cadherin family member which is the human homolog of the Drosophila melanogaster FAT tumour suppressor gene. Ultimately, detailed fine-mapping and functional analyses will be required to define the causal allele(s) and to confirm that this effect is mediated through altered function or expression of MTNR1B.
As well as exploring this novel signal, the size of the MAGIC data-set allowed us to examine the G6PC2 and GCK regions in greater detail than has previously been possible. In the G6PC2 region, rs560887, within intron 3 of the gene, remained the strongest signal whether or not imputed data were included (P=1.1 × 10−57 across all 10 studies: Supplementary Figure 1). This is the same SNP reported in one recent paper,5 and in substantial LD (r2=0.72 in HapMap CEU) with the lead SNP (rs563694) identified in a second6. In the GCK region, rs4607517, which lies 6.6 kb upstream of the gene, was the most strongly-associated SNP (P=1.0 × 10−25) (Supplementary Figure 1, Table 1). This SNP is also in strong LD (r2 = 1 in HapMap CEU) with the GCK promoter SNP (rs1799884) that was featured in previous reports4. Repeat meta-analysis after conditioning on the respective lead SNPs revealed no additional independent association signals at either locus (Supplementary Note).
As with MTNR1B, the magnitudes of the FG associations for both these signals were unchanged after adjustment for BMI (Supplementary Table 4). Glucose-raising alleles at GCK and G6PC2 were associated with reduced beta-cell function (rs4607517A, P=9.8 × 10−6; rs560887C, P=1.2 × 10−26) (Supplementary Table 5, Supplementary Note). However, in line with previous reports4,9, neither signal was strongly associated with T2D in the large-scale meta-analysis: in fact, the glucose-raising allele at G6PC2 was weakly associated with reduced T2D risk (rs4607517A, per-allele OR 1.05 [1.00–1.10], P=0.031; rs560887C, 0.93 [0.89–0.97], P=0.0017) (Supplementary Table 6).
We found no influence of the non-coding lead SNPs rs10830963, rs560887 or rs4607517 on gene expression of MTNR1B, SLC36A4, FAT3, G6PC2 or GCK in genome-wide expression QTL datasets from lymphocyte derived cell lines19,20, cerebral cortex21, or liver22, and no evidence for epistatic effects among the three lead SNPs was observed (P-2 way interactions > 0.19 in each of the 7 studies including only unrelated individuals; interactions were not examined in the other 3 studies).
MTNR1B encodes one of two known human melatonin receptors23. Although this is the first study to implicate genetic variation in MTNR1B in the regulation of FG levels and predisposition to T2D, this relationship is biologically credible. As well as being highly-expressed in the brain, retina and elsewhere24, MTNR1B is transcribed in human islets and rodent insulinoma cell lines25 and the translated receptor is thought to mediate the inhibitory effect of melatonin on insulin secretion26. Melatonin release is characterized by marked circadian variability and these inhibitory effects on insulin secretion may contribute to the entrainment of circadian patterns of insulin release27. There is substantial evidence in human and rodent studies linking disturbances of circadian rhythmicity to metabolic conditions including diabetes28,29 and over-expression of melatonin receptors has been observed in islets from patients with T2D as compared to non-diabetic controls30. Taken together, these findings suggest that the association with raised FG and T2D may be driven by variants which augment expression and/or activity of islet melatonin receptors.
Our findings bring the number of common variant loci influencing FG levels to four, three of which were detected in the present study. Variants in GCKR have a smaller effect size than the others7,9 and the present study design (based on exchange of a limited number of prominent signals between component groups) was not well-powered to detect these. However, subsequent meta-analysis of GCKR variant data across all 10 study samples confirms the association with FG (rs780094, P=8.5 × 10−9) (Supplementary Table 4). The total variance in FG presently attributable to these four signals is 1.5%, indicating that additional loci remain to be found3. In comparison with GCK and G6PC2, variants in MTNR1B appear to have a more marked effect on risk of T2D, the effect size being comparable in magnitude (OR=1.09 [1.05–1.12]) to several other T2D-susceptibility genes recently identified in GWAS10. Thus, whilst the physiological regulation of FG set point and the pathological decline in beta-cell function which characterizes common forms of T2D generally appear to involve different processes, the MTNR1B finding suggests that this is not always the case. Not only can the study of diabetes-related quantitative traits provide an important path to the identification of additional T2D susceptibility loci, but there may also be opportunities for useful therapeutic overlap.
Supplementary Material
Figure 1. Regional plot of fasting glucose association results for the MTNR1B locus across 10 MAGIC GWAS.
Meta-analysis -log10 P-values are plotted as a function of genomic position (NCBI Build 35). The SNP with the strongest signal (rs10830963) is denoted by a blue diamond. Estimated recombination rates (from HapMap) are plotted to reflect the local linkage disequilibrium structure around associated SNPs and proxies (according to a white-to-red scale from r2=0 to r2=1; based on pair-wise r2 values from HapMap CEU). Gene annotations were taken from the University of California-Santa Cruz genome browser.
Acknowledgements
The authors would like to thank the many colleagues who contributed to collection and phenotypic characterization of the clinical samples, as well as genotyping and analysis of the GWA data. They would also like to acknowledge those who agreed to participate in these studies. Major funding for the work described in this paper comes from Academy of Finland (124243); the Administration of Lanusei, Ilbono, Arzana and Elini (Sardinia, Italy); American Diabetes Association (1-05-RA-140); the Center for Inherited Disease Research; Clinical Research Institute (HUCH); Diabetes UK; the European Bioinformatics Institute; the European Commission (contracts LSHM-CT-2006-037197, LSHM-CT-2003-503041. QLK6- CT-2002-02629, QLG2-CT-2002-01254, HEALTH-F4-2007-201413, LSHG-CT-2004-512066, QLRT-2001-01254, LSHG-CT-2004-518153); the Faculty of Biology and Medicine of Lausanne; Finnish Diabetes Research Foundation; Folkhalsan Research Foundation; Foundation of the NIH (GAIN initiative); German Federal Ministry of Education and Research; German Federal Ministry of Health and Social Security; German National Genome Research Network; GlaxoSmithKline; GSF-National Research Center for Environment and Health; LMUinnovativ; Ministry of Science and Research of the State North-Rhine Westphalia; Municipality of Rotterdam; NIH (HG-02651, HL-084729, HL-087679, HC-25195, DK-078616, DK-080140, DK-065978, RR-163736, MH059160, DK069922, DA-021519, DK-062370, DK-072193, NHGRI intramural project HG-000024; and the Intramural Program of the National Institute on Aging); the UK National Institute for Health Research (Oxford Biomedical Research Centre and Guys and St. Thomas’ Biomedical Research Centre); the Netherlands Ministry of Education, Culture and Science; the Netherlands Ministry of Health, Welfare and Sports; Novartis; NWO (904-61-090, 904-61-193, 480-04-004, 400-05-717); NWOGenomics; NWOInvestments; Research Institute for Diseases in the Elderly (RIDE); Sigrid Juselius Foundation; Spinozapremie; Swedish Research Council (349-2006-237); UK Medical Research Council (G0500539, G0000649, G016121); UK National Health Services Research and Development; the Wellcome Trust (including intramural support for the Wellcome Trust Sanger Institute, GR069224, Strategic Awards 076113 and 083948, Biomedical Collections Grant GR072960); and ZonMw (10-000-1002). A full list of acknowledgements is provided in the supplementary note.
Reference List
- 1.Xiang AH, et al. Coordinate changes in plasma glucose and pancreatic beta-cell function in Latino women at high risk for type 2 diabetes. Diabetes. 2006;55:1074–1079. doi: 10.2337/diabetes.55.04.06.db05-1109. [DOI] [PubMed] [Google Scholar]
- 2.Mason CC, Hanson RL, Knowler WC. Progression to type 2 diabetes characterized by moderate then rapid glucose increases. Diabetes. 2007;56:2054–2061. doi: 10.2337/db07-0053. [DOI] [PubMed] [Google Scholar]
- 3.Watanabe RM, et al. Familiality of quantitative metabolic traits in Finnish families with non-insulin-dependent diabetes mellitus. Finland-United States Investigation of NIDDM Genetics (FUSION) Study investigators. Hum.Hered. 1999;49:159–168. doi: 10.1159/000022865. [DOI] [PubMed] [Google Scholar]
- 4.Weedon MN, et al. A common haplotype of the glucokinase gene alters fasting glucose and birth weight: association in six studies and population-genetics analyses. Am.J.Hum.Genet. 2006;79:991–1001. doi: 10.1086/509517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bouatia-Naji N, et al. A polymorphism within the G6PC2 gene is associated with fasting plasma glucose levels. Science. 2008;320:1085–1088. doi: 10.1126/science.1156849. [DOI] [PubMed] [Google Scholar]
- 6.Chen WM, et al. Variations in the G6PC2/ABCB11 genomic region are associated with fasting glucose levels. J Clin Invest. 2008;118:2620–2628. doi: 10.1172/JCI34566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saxena R, et al. Genome-wide association analysis identifies loci for type 2 diabetes and triglyceride levels. Science. 2007;316:1331–1336. doi: 10.1126/science.1142358. [DOI] [PubMed] [Google Scholar]
- 8.Vaxillaire M, et al. Impact of common type 2 diabetes risk polymorphisms in the DESIR prospective study. Diabetes. 2008;57:244–254. doi: 10.2337/db07-0615. [DOI] [PubMed] [Google Scholar]
- 9.Orho-Melander M, et al. A Common Missense Variant in the Glucokinase Regulatory Protein Gene (GCKR) Is Associated with Increased Plasma Triglyceride and C-Reactive Protein but Lower Fasting Glucose Concentrations. Diabetes. 2008 Aug 4; doi: 10.2337/db08-0516. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zeggini E, et al. Meta-analysis of genome-wide association data and large-scale replication identifies additional susceptibility loci for type 2 diabetes. Nat.Genet. 2008;40:638–645. doi: 10.1038/ng.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scott LJ, et al. A genome-wide association study of type 2 diabetes in Finns detects multiple susceptibility variants. Science. 2007;316:1341–1345. doi: 10.1126/science.1142382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sladek R, et al. A genome-wide association study identifies novel risk loci for type 2 diabetes. Nature. 2007;445:881–885. doi: 10.1038/nature05616. [DOI] [PubMed] [Google Scholar]
- 13.Steinthorsdottir V, et al. A variant in CDKAL1 influences insulin response and risk of type 2 diabetes. Nat.Genet. 2007;39:770–775. doi: 10.1038/ng2043. [DOI] [PubMed] [Google Scholar]
- 14.Zeggini E, et al. Replication of genome-wide association signals in UK samples reveals risk loci for type 2 diabetes. Science. 2007;316:1336–1341. doi: 10.1126/science.1142364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.A haplotype map of the human genome. Nature. 2005;437:1299–1320. doi: 10.1038/nature04226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matthews DR, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 17.Hofman A, et al. The Rotterdam Study: objectives and design update. Eur J Epidemiol. 2007;22:819–829. doi: 10.1007/s10654-007-9199-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Herder C, et al. Variants of the PPARG, IGF2BP2, CDKAL1, HHEX, and TCF7L2 Genes Confer Risk of Type 2 Diabetes Independently of BMI in the German KORA Studies. Horm Metab Res. 2008 doi: 10.1055/s-2008-1078730. [DOI] [PubMed] [Google Scholar]
- 19.Dixon AL, et al. A genome-wide association study of global gene expression. Nat.Genet. 2007;39:1202–1207. doi: 10.1038/ng2109. [DOI] [PubMed] [Google Scholar]
- 20.Stranger BE, et al. Population genomics of human gene expression. Nat.Genet. 2007;39:1217–1224. doi: 10.1038/ng2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Myers AJ, et al. A survey of genetic human cortical gene expression. Nat.Genet. 2007;39:1494–1499. doi: 10.1038/ng.2007.16. [DOI] [PubMed] [Google Scholar]
- 22.Schadt EE, et al. Mapping the Genetic Architecture of Gene Expression in Human Liver. PLoS.Biol. 2008;6:e107. doi: 10.1371/journal.pbio.0060107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reppert SM, et al. Molecular characterization of a second melatonin receptor expressed in human retina and brain: the Mel1b melatonin receptor. Proc.Natl.Acad.Sci.U.S.A. 1995;92:8734–8738. doi: 10.1073/pnas.92.19.8734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Su AI, et al. Large-scale analysis of the human and mouse transcriptomes. Proc Natl Acad Sci U S A. 2002;99:4465–4470. doi: 10.1073/pnas.012025199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ramracheya RD, et al. Function and expression of melatonin receptors on human pancreatic islets. J.Pineal Res. 2008;44:273–279. doi: 10.1111/j.1600-079X.2007.00523.x. [DOI] [PubMed] [Google Scholar]
- 26.Stumpf I, Muhlbauer E, Peschke E. Involvement of the cGMP pathway in mediating the insulin-inhibitory effect of melatonin in pancreatic beta-cells. J.Pineal Res. 2008 doi: 10.1111/j.1600-079X.2008.00593.x. [DOI] [PubMed] [Google Scholar]
- 27.Boden G, Ruiz J, Urbain JL, Chen X. Evidence for a circadian rhythm of insulin secretion. Am.J.Physiol. 1996;271:E246–E252. doi: 10.1152/ajpendo.1996.271.2.E246. [DOI] [PubMed] [Google Scholar]
- 28.Spiegel K, Leproult R, Van CE. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–1439. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- 29.Turek FW, et al. Obesity and metabolic syndrome in circadian Clock mutant mice. Science. 2005;308:1043–1045. doi: 10.1126/science.1108750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peschke E, et al. Melatonin and type 2 diabetes - a possible link? J.Pineal Res. 2007;42:350–358. doi: 10.1111/j.1600-079X.2007.00426.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.