Abstract
Objective
The objective of this study was to gather descriptive information concerning the clinical outcomes of patients with cervical and lumbar radiculopathy treated with a nonsurgical, chiropractic treatment protocol in combination with other interventions.
Methods
This is a retrospective review of 162 patients with a working diagnosis of radiculopathy who met the inclusion criteria (312 consecutive patients were screened to obtain the 162 cases). Data reviewed were collected initially, during, and at the end of active treatment. The treatment protocol included chiropractic manipulation, neuromobilization, and exercise stabilization. Pain intensity was measured using the numerical pain rating scale.
Results
Of the 162 cases reviewed, 85.5% had resolution of their primary subjective radicular complaints. The treatment trial was 9 (mean) treatment sessions. The number of days between the first treatment date and the first symptom improvement was 4.2 days (mean). The change in numeric pain scale between initial and final score was 4.2 (median). There were 10 unresolved cases referred for epidural steroid injection, 10 unresolved cases referred for further medication management, and 3 cases referred for and underwent surgery.
Conclusion
The conservative management strategy we reviewed in our sample produced favorable outcomes for most of the patients with radiculopathy. The strategy appears to be safe. Randomized clinical trials are needed to separate treatment effectiveness from the natural history of radiculopathy.
Key indexing terms: Radiculopathy; Manipulation, chiropractic; Exercise therapy; Musculoskeletal system; Delivery of health care, Integrated
Introduction
Little is known about effective treatments for radiculopathy. Consequently, effective management strategies need to be reported and analyzed. Historically, little progress has been made in defining optimal treatment strategies because both surgical and nonsurgical approaches are commonplace.1,2 Useful information is lacking in regard to identifying what nonsurgical and noninvasive treatment approaches are most effective. Noninvasive treatments that follow a standardized approach, in which every patient follows a similar treatment protocol, need to be analyzed to determine if these are as effective as an approach that is individualized.
The optimal frequency and duration of nonsurgical treatment have not been properly assessed or correlated along with objective information necessary to determine when nonsurgical treatment needs to be discontinued. Because there are no clear data as to the natural history of this disorder (ie, how often a spontaneous resolution of the symptoms occurs), treatment outcomes must be analyzed with caution.
Murphy et al3,4 published a conservative treatment protocol that has reported effectiveness. Their nonsurgical, noninvasive treatment approach revolved around spinal manipulation, neuromobilization, and spinal stabilization exercises. Using the noninvasive approach of Murphy et al3,4, this review reports on the outcome of 162 consecutive patients with radiculopathy gathered retrospectively between April 2006 and April 2007 in a hospital outpatient setting.
Methods
This is a retrospective review of 162 consecutive acute and chronic patients diagnosed with an initial “working diagnosis” of either upper extremity or lower extremity radiculopathy between April 30, 2006, and April 30, 2007. Data were extracted from patient medical records backward in time. Three hundred twelve consecutive patients were screened to obtain the 162 cases. Institutional Review Board approval (PeaceHealth Medical Group Institutional Review Board study 07-040) was obtained. Advanced imaging and/or electromyogram (EMG) was used but not required of all participants. Inclusion and exclusion criteria are listed in Fig 1.
Fig 1.
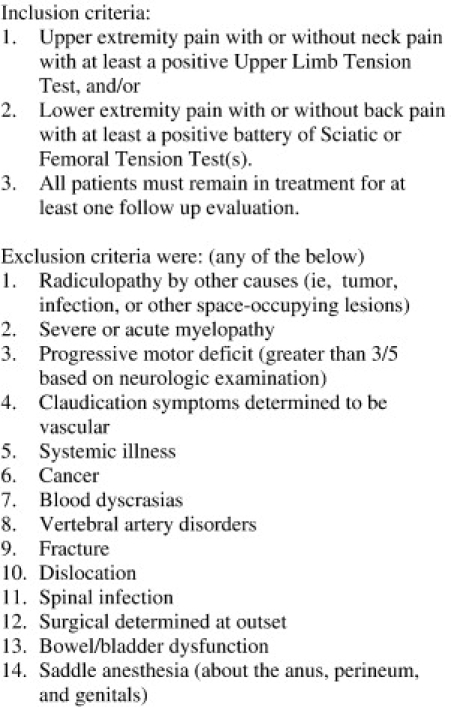
Inclusion/exclusion criteria.
A primary outcome measure was the numerical pain scale (scale 0-10). This was completed initially and at every follow-up treatment session. Other data gathered included age, sex, current and past medical history including comorbid conditions, duration of symptoms, primary diagnosis, secondary diagnosis, rheumatologic or orthopedic conditions affecting the spine, magnetic resonance imaging (MRI) findings, computed tomographic or plain film findings or EMG, history of surgery, types of previous treatments applied, medications, and complications to any treatment. These data were gathered as part of the usual patient management process.
Each patient was examined with orthopedic tests to verify the specific nerve root involved in the radiculopathy, namely, sciatic, femoral, median, radial, or ulnar. A standard chart note was recorded on every treatment visit. This included the subjective patient pain intensity including location with description as weak, ache, dull, sharp, pins/needles, numbness, burning, stabbing, or other.
Cervical objective data (median, radial, ulnar) collected included the ongoing findings of the upper limb tension test (shoulder abduction angle recorded), Spurling test A, cervical distraction, and cervical rotation. Lumbar sciatic objective data included lumbar flexion (standing tension angle recorded) and passive hip flexion (sciatic tension angle recorded). Lumbar femoral objective data included lumbar flexion (standing tension angle recorded) and passive hip extension (femoral tension angle recorded). Palpatory tenderness included comparative testing between right vs left; anterior/medial scalene, cervical/lumbar spine segments, sacroiliac, and sciatic notch regions.
Interventions on all patients included chiropractic manipulation, neuromobilization, and stabilization exercises directed by a doctor of chiropractic who was board certified in chiropractic rehabilitation with 30 years of practice experience. Although the frequency and duration of care were determined on an individual basis, each patient was generally treated 2 to 3 times per week until radicular recovery or discharge. Each patient was followed every visit to monitor home exercise progression and further activity and to address questions or uncertainty.
Chiropractic manipulation was performed on all patients. Joint dysfunction was determined by palpation demonstrating abnormal resistance to springing of the joint, reactivity of the underlying musculature, and/or the patient's report of pain. In selected cases, radiographic biomechanical analysis was performed to determine deviations from neutral to position the patient for manipulation and centration stabilization procedures that center the cervical and lumbar spine in the frontal and sagittal plane.
In cases of lumbar spine radiculopathy, distraction manipulation (DM), a low-velocity technique, and a secondary high-velocity low-amplitude (HVLA) manipulation technique were used. The maneuvers were always delivered in a direction that did not cause peripheralization of the pain. Distraction manipulation was performed on a flexion-distraction table with the patient prone using a stomach pillow to position the patient in mild lumbar semiflexion. Distraction manipulation motions included flexion, extension, and lateral flexion in the direction of spinal centration (centering) only. There was no rotation performed, with extension motion limited from semiflexion to neutral. In the HVLA technique, the lumbar spine deviation from neutral (translation or lateral flexion) was performed using a drop table in the side-lying position so that there would be no introduction of rotation to the HVLA technique.
In cases of cervical spine radiculopathy, low-velocity manipulation technique, namely, DM and motion palpation technique, was used.
Motion palpation technique5 is a diagnostic technique used by the health care provider to locate and treat joint dysfunction within the spinal column and extremities. The maneuvers were always delivered in a direction that did not cause peripheralization of the pain that consisted predominantly of cervical lateral flexion and cervical translation.
Neuromobilization was used as a manual- and exercise-oriented method that is theorized to mobilize nerve roots that are suspected to be the source of nerve root pain. It was performed on nerve roots that were suspected through examination to exhibit neural tension signs. With this method, tension was gently applied to the involved nerve roots that caused mild “pulling” but no pain during in-office treatment; and a low-amplitude repetitive movement was introduced in the direction of perceived neural tension for at-home exercise. The specific procedures for each neuromobilization pattern are described in Fig 2. The complete pattern can be performed on any adjusting table, but particularly one with cervical/lumbar motion that accommodates cervical/lumbar passive motion during the specific neuromobilization procedure.
Fig 2.
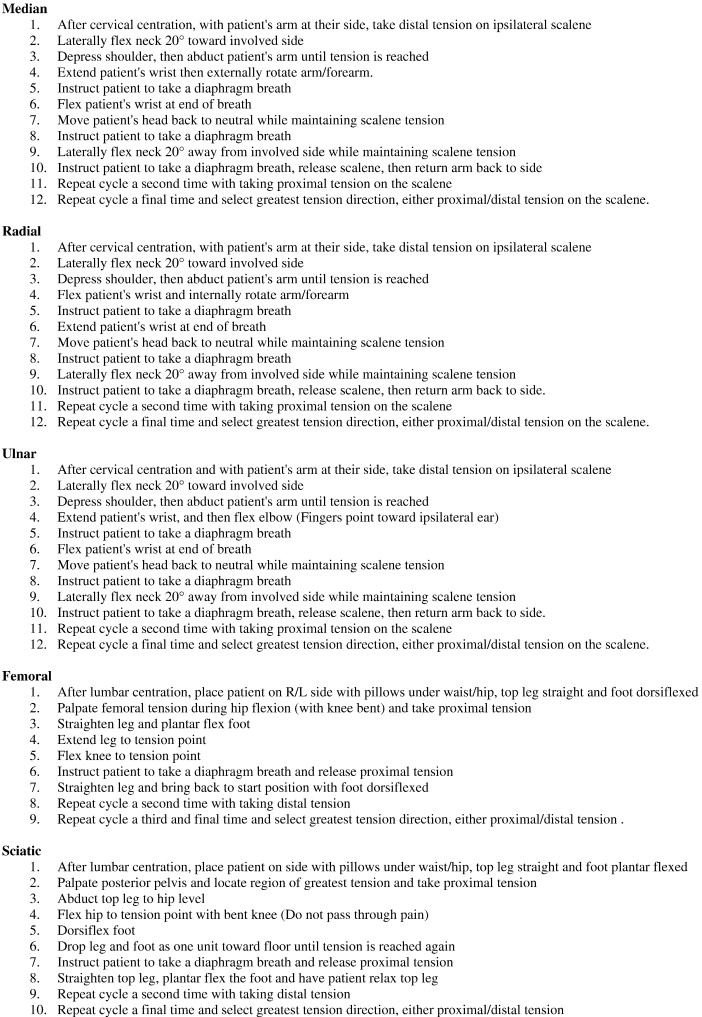
Neuromobilization procedures.
All patients were given the same series of stabilization exercises for home performance. The spine stabilization procedures used were progressive, meaning beginning procedures were performed before intermediate and advanced procedures. The patient was given a handout (Fig 3) of each actual procedure along with a DVD of the procedures to be performed. Each patient demonstrated the assigned procedure correctly before they left the office. Each patient on subsequent visits was required to demonstrate satisfactory “pain-free” performance of beginning procedures before they were allowed to advance to the intermediate and advanced procedures. The cervical and lumbar spine stabilization progressions used are listed in Figs 4 and 5.
Fig 3.
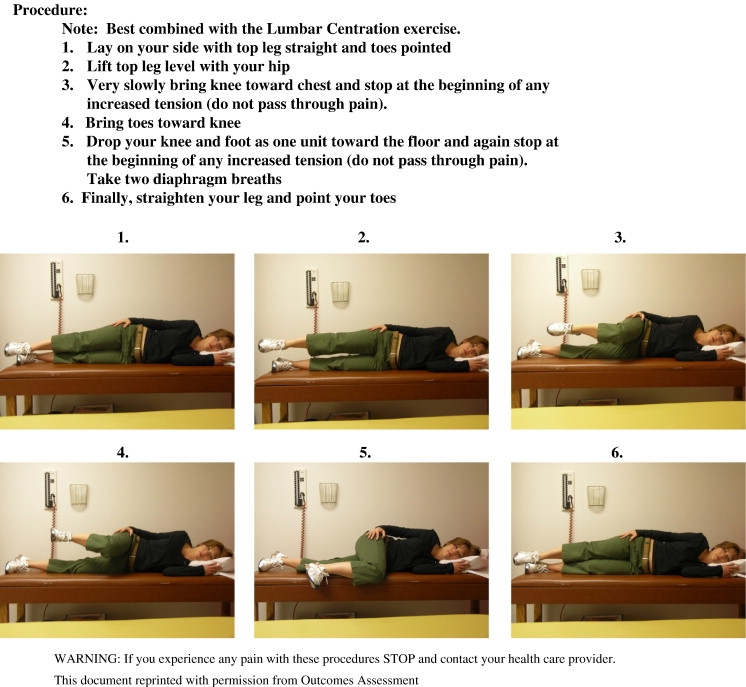
Sciatic neuromobilization.
Fig 4.
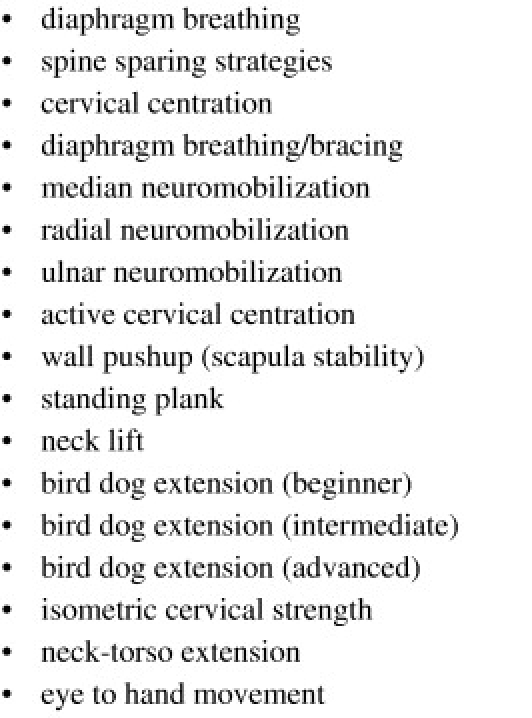
Cervical stabilization progressions.
Fig 5.
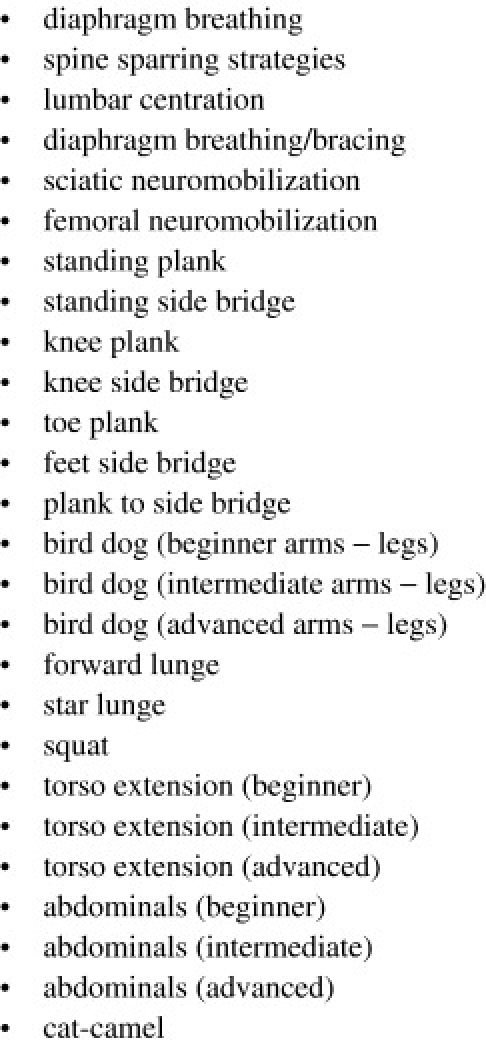
Back stabilization progressions.
Additional procedures used as needed per patient included ice massage during acute presentation demonstrating cervical or lumbar effusion, Graston instrument soft tissue technique, and custom orthotics (ArchFitters, Gresham, OR).
Results
Initial characteristics and beginning/ending data of the cases reviewed are presented in Table 1 with descriptive statistics including mean, median, standard deviation, and range. These include age, pain scores, number of treatments, and days to decreased pain. Of the 162 consecutive patients reviewed, 99 were female and 63 were male. Upper extremity symptoms were seen in 61 cases and lower extremity in 108 cases, with 7 of these cases demonstrating both.
Table 1.
Patient data
| Variable | Mean | Median | SD | Range |
|---|---|---|---|---|
| Age (Total) | 47.9 | 48 | 15.7 | 16-81 |
| Age (Female) | 49.1 | 51 | 16.4 | 16-81 |
| Age (Male) | 46.5 | 46 | 14.2 | 18-79 |
| Total Treatment No. | 9.0 | 8 | 5.1 | 1-23 |
| Pain (Initial) | 5.8 | 6 | 2.0 | |
| Pain (Ending) | 2.1 | 2 | 2.1 | |
| Pain (Initial to Ending Change) | 4.2 | 4 | 5.8 | |
| Days to Decreased Pain | 4.2 | 3 | 3.5 |
Of the 162 total cases, 85.8% resolved their significant subjective radicular complaints; and the patients were discharged from active treatment. The treatment trial was 9 (mean) treatment sessions, ranging from 1 to 23 visits and lasting between 2 and 86 days. The number of days between the first treatment date and the first symptom improvement was 4.2 (mean) days, with a range (standard deviation) of 0.78 to 7.7 day(s). The initial numerical pain rating scale score (median) was 5.8, with a final score of 2.1 (median). The pain change between initial and final score was 4.2 (median).
Of the 162 total cases, acute and chronic presentations were represented. Sixty-seven (41.36%) were classified as “acute,” meaning their symptom duration was less than 3 months. Ninety-five (58.64%) were classified as “chronic,” meaning their symptom duration was greater than 3 months. Ninety-one percent of acute presentations resolved with a treatment trial (mean) of 6.2 sessions, ranging from 1 to 20 visits. Eighty-one percent of chronic presentations resolved with a treatment trial of 8.6 (mean) sessions, ranging from 1 to 23 visits.
There were 10 unresolved cases referred for epidural steroid injection as a result of the nonsurgical treatment not resolving the radicular complaints. Of the 162 total cases, these represent 6.17%. Three of these 10 cases experienced no symptom improvement with the nonsurgical treatment. Seven cases experienced minimal to moderate improvement before referral. The treatment trial ranged from 4 to 22 visits.
There were 10 unresolved cases referred for medication management as a result of the nonsurgical treatment not resolving the radicular complaints. Of the 162 total cases, these represent 6.17%. Four of these 10 cases experienced no symptom improvement with the nonsurgical treatment. Six cases experienced minimal to moderate improvement before referral. The treatment trial ranged from 3 to 25 visits.
Three unresolved cases were referred for and underwent surgery. Of the 162 total cases, these represent 1.85%. All 3 cases showed no symptom improvement before referral. The treatment trial ranged from 2 to 7 visits, lasting between 9 and 17 days. The MRI on each of these cases demonstrated a significant disk extrusion.
There was 1 case that was scheduled for cervical spine surgery before initial evaluation. The case elected a trial of 30 days of nonsurgical treatment that resolved the complaints.
There were no major complications in any patient. Short-term increase in discomfort after manipulation, mobilization, and/or exercise was common; however, rarely did increased symptoms relative to any treatment persist beyond a few days.
Incidentally noted, with the cervical radiculopathy cases, there was a consistent increase in the shoulder abduction angle during the upper limb tension test in cases that resolved. Whereas it was common for the first test to provoke active symptoms as early as 20° to 30° of shoulder abduction, with treatment, follow-up testing increased to the maximum of patient abduction capacity without provoking symptoms. Similarly, there was a common finding of the Spurling test A, cervical distraction, and cervical rotation when positive progressing to negative testing results.
Incidentally noted, with lumbar radiculopathy cases, there was a consistent increase in active lumbar flexion (standing tension angle), passive hip flexion (sciatic tension angle), and passive hip extension (femoral tension angle) in cases that resolved. Similarly, there was a common finding of the straight leg raise, Braggard, slump, and femoral nerve stretch tests when positive progressing to negative testing in cases that resolved. Comparative palpatory tenderness testing between right vs left, anterior/medial scalene, sacroiliac, and sciatic notch regions commonly decreased or resolved in cases where the radicular complaints resolved.
Most of the cases that resolved their radiculopathy complaint completed up to 50% of the stabilization procedures. It was noted that very seldom did it require completion of all the stabilization procedures listed above.
Discussion
Radiculopathy refers to those subjects with signs and symptoms related to dysfunction of the spinal nerve root(s).6 It is a disorder that is painful, often disabling, and with limited information on the prevalence and incidence. In acute radiculopathy, Murphy7 reports that the pain comes primarily from inflammation and compression, whereas in chronic radiculopathy, pain more often comes as a result of fibrosis. Disk herniation and lateral canal stenosis are the most common causes of radiculopathy. Disk herniation involves herniation of disk material into the intervertebral foramen. Lateral canal stenosis involves encroachment on the intervertebral foramen from osteophytes from the vertebral body or zygopophyseal joint and/or ligament flavum hypertrophy. In both cases, nerve root pain with dysfunction can occur. In addition, central canal stenosis may cause bilateral radiculopathy.
In regard to cervical radiculopathy,8 the seventh cervical nerve root, between C6 and C7 (60%), and the sixth cervical nerve root, between C5 and C6 (25%), are the most commonly affected. With lumbar radiculopathy, L4, L5, and S1 are the most commonly affected nerve roots.9
The diagnostic criteria for radiculopathy7 are unclear. Some suggest that radiculopathy is a diagnosis based upon clinical impression that should be confirmed by advanced testing, such as diagnostic imaging or electrophysiology studies.10 However, there is no criterion standard for the diagnosis of radiculopathy, as clinical, radiological, and electrophysiological testing all have inherent limitations.11 The dilemma in actual fact stems from the false-positive rate associated with imaging and the false-negative rate associated with electrophysiological testing.10 Given that the establishment of a criterion standard is pivotal to diagnostic accuracy, this is no minor issue.
Asymptomatic radiological abnormalities are commonly seen with advanced imaging studies.12 It is accepted that the diagnostic accuracy of specialized imaging is limited, especially with regard to foraminal nerve root impingement.13 Unlike electrodiagnostic testing, imaging cannot distinguish noncompressive from compressive etiologies, such as inflammation.10 As a result, nerve root pain can be present in the absence of visible compression.14 Thus, Rubinstein10 proposes that the optimal diagnostic criterion standard should combine the findings of MRI with electrodiagnostic testing.
Advanced diagnostic testing however can be expensive and, in the case of nerve conduction studies, may be intrusive and/or painful. Clearly, there is a need for a cost-effective, accurate, and noninvasive manner for the health care provider to confirm his diagnostic impression and to determine whether the patient can be adequately treated in the primary care setting.
For the cervical spine, Rubinstein10 reports that, when consistent with the history and other physical findings, a positive Spurling, neck traction, neck distraction, or Valsalva (given their high specificity) test result might be indicative of a cervical radiculopathy, whereas a negative upper limb tension test result (given its high sensitivity) might be used to rule it out.
Recently, Wainner15 reported that the following cluster of cervical tests has a 90 % posttest probability that the patient has cervical radiculopathy when results of all 4 tests are positive: upper-limb tension test A, Spurling test A, distraction test, and cervical rotation (<60° on ipsilateral side).
Fig 6 provides cervical orthopedic test procedures and determination of positive findings according to Cleland.16
Fig 6.
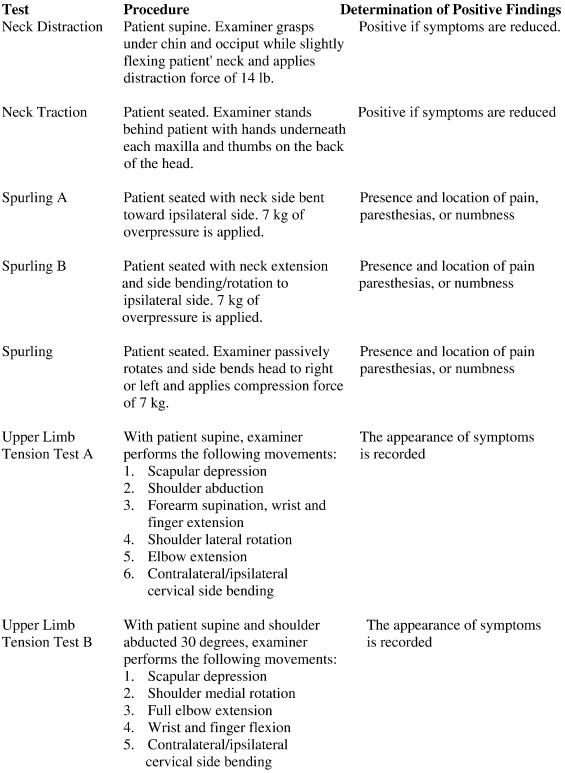
Cervical orthopedic tests.
For the sciatic nerve of the lumbar spine, Murphy7 reports that the straight leg raise has good sensitivity but poor specificity. In contrast, the well leg raise has good specificity but poor sensitivity. The suggested battery of tests for sciatic radiculopathy would include the following: straight leg raise, well leg raise, Braggard dorsiflexion, and slump test. For the femoral nerve, the femoral nerve traction test17 is used. The prone femoral nerve stretch tests and side-lying slump tests are then used as a battery of tests to confirm femoral involvement.18 Fig 7 provides the slump and side-lying slump orthopedic test procedures and determination of positive findings according to Liebenson.18
Fig 7.
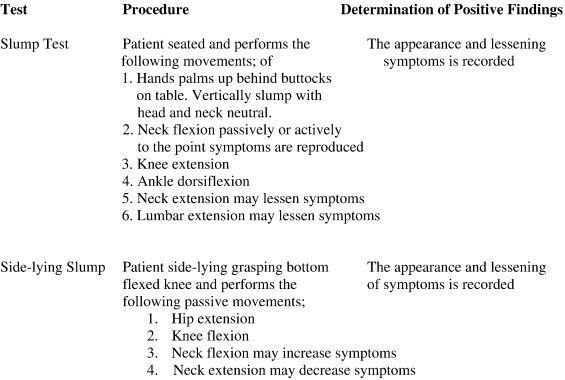
Slump orthopedic tests.
Cleland16 reports that the best clinical cluster of lumbar tests with calculated positive and negative likelihood ratios for lumbar radiculopathy include:
-
•
contralateral straight leg raise (+7.2/−.61) (well leg raise)
-
•
patellar (+7.14/−.54) and Achilles (+4.7/−.59) reflex
-
•
hip flexors weakness (+4.35/−.36)
-
•
extensor hallucis longus weakness (+4.9/−.52)
-
•
reflex/weakness/sensory all positive (+4.0/−.90)
The choice between surgical and nonsurgical treatment options remains unclear because both surgical and nonsurgical approaches are commonplace. Recently, Thomas et al1 assessed the health-related quality of life after lumbar disk protrusion causing radiculopathy, as measured by the North American Spine Society neurogenic symptoms score, treated with either microdiskectomy or nonsurgical care. One-year findings demonstrated similar improvement in both treatment groups and as such were not meaningfully associated with the treatment received. Generally, nonsurgical treatment measures are attempted before invasive procedures. However, in regard to nonsurgical care, current clinical practice guidelines afford practitioners a wide spectrum of nonoperative care options, making this treatment arm difficult to standardize.
This current study is useful in that it assesses the outcome of a nonsurgical treatment approach in a hospital outpatient environment. The results of this study suggest that the combination of manipulation, neuromobilization, and stabilization exercise may be useful for patients with radiculopathy. Clinicians should consider these results when faced with decision making for individual patients.
This study does not allow one to draw conclusions about the optimum number of treatments for patients with radiculopathy. However, these patients were treated an average of 9 times. This may help the treating clinician in decision making regarding how long to continue to treat a patient with radiculopathy using this approach. This study does not support the use of a uniform number of visits automatically provided for all patients without regard for individual patient needs. It must be noted that a relatively wide range of treatments visits (eg, 1-23) was seen in this study, suggesting that individual differences in patient responses to treatment exist that necessitate greater or fewer than the mean number of treatments. Nonetheless, with a standard deviation of 5.1, these patients required between 3 and 14 visits.
According to Workers Compensation Research Institute,19 lumbar radiculopathy complaints cost New York workers compensation an average per claim of $9847.00 and cervical radiculopathy $11,191.00 per claim. With our mean treatment number to resolve radiculopathy (costs less than $1500.00), it is clearly less expensive than customary treatment costs in New York.
This study demonstrated a decrease in the numeric rating scale within 8 days. If this is not seen, it may suggest the need for a surgical consultation. In addition, a change of 2 points on the NRS is generally considered to be the threshold for clinically meaningful improvement.20 The change (median) between initial and final score in this study was 4.2. Thus, if a minimum improvement of 2 points on the NRS is not seen, further nonsurgical treatment may not be appropriate.
It is difficult to compare the results presented here with those of other studies on nonsurgical management of patients with radiculopathy owing to difference in design, outcome measurement, and selection criteria. Interesting to note, in this study, there was no emphasis on “end-range loading” passive/active exercise techniques. This study however used neutral spine stabilization.
Controversy exists over the use of manipulation in patients with radiculopathy. It has been stated that this treatment is contraindicated in the presence of a herniated disk.21 No major complication was seen in any of these patients. The data presented here would continue to suggest that manipulation, when applied by properly trained and experience practitioners, is potentially a safe option for patients with radiculopathy.
Radiographic biomechanical analysis was performed on all patients to determine deviations from neutral to position the patient for manipulation and neuromobilization procedures. Fig 8 demonstrates the lower extremity neuromobilization positions used that were based upon the radiographic findings noted. Randomized clinical trials are needed to document any actual improved outcomes with this use.
Fig 8.
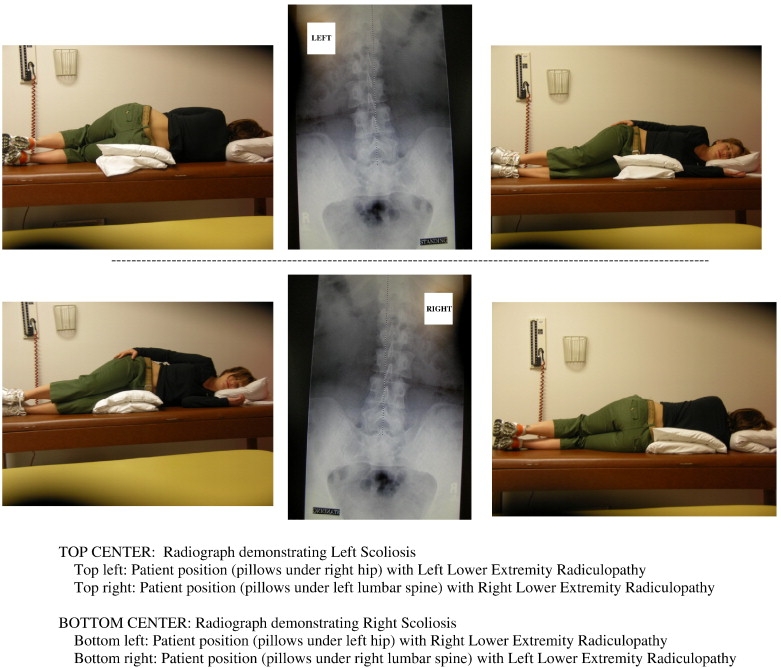
Neuromobilization positions with lumbar centration.
There are several important limitations to this study. It is not a randomized controlled trial; thus, interpretation of the results must be made with caution. The natural history of radiculopathy is generally thought to be favorable; however, data on untreated patients with this disorder are lacking. Because of this scarcity of natural history data and because the current study did not involve an untreated or placebo control group and there was no long-term follow-up, there is no way to compare the outcomes reported here with those in the untreated situation. Numerical pain rating has 1 major setback in terms of validity, which is that indeterminate factors such as patient mood, attitude, central and/or peripheral sensitization, and other biopsychosocial factors can play a role in pain reporting. Palpation of restricted spinal segments has been repeatedly shown to have relatively weak intra-/interexaminer reliability. It is possible that only one of the treatments discussed or any combination of the treatments produced the positive results seen.
Conclusion
The current study supports the notion that chiropractic management and nonsurgical measures are a viable alternative to surgery in patients with radiculopathy. Randomized controlled trials are called for to further assess this nonsurgical approach compared with untreated controls and surgical treatments.
References
- 1.Thomas K.D., Fisher C.G., Boyd M., Bishop P., Wing P., Dvorak M. Outcome evaluation of surgical and nonsurgical management of lumbar disc protrusion causing radiculopathy. Spine. 2007;32:1414–1422. doi: 10.1097/BRS.0b013e318060a5d1. [DOI] [PubMed] [Google Scholar]
- 2.Heckmann J.G., Lang C.J.G., Zobelein I., Laumer R., Druschky A., Neundorfer B. Herniated cervical intervertebral discs with radiculopathy: an outcome study of conservatively or surgically treated patients. J Spinal Disord. 1999;12:396–401. [PubMed] [Google Scholar]
- 3.Murphy D.R., Hurwitz E.L., Gregory A.A., Clary R. A nonsurgical approach to the management of patients with cervical radiculopathy: a prospective observational cohort study. J Manipulative Physiol Ther. 2006;29:279–287. doi: 10.1016/j.jmpt.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 4.Murphy D.R., Hurwitz E.L., Gregory A.A., Clary R. A non-surgical approach to the management of lumbar spinal stenosis: a prospective observational cohort study. BMC Musculoskelet Disord. 2006;7:16. doi: 10.1186/1471-2474-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Faye L.J. Motion Palpation Institute; Cincinnati, OH: 1989. Motion palpation & chiropractic technique. [Google Scholar]
- 6.Radhakrishnan K., Litchy W.J., O'Fallon W.M., Kurland L.T. Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain. 1994;117(Pt 2):325–335. doi: 10.1093/brain/117.2.325. [DOI] [PubMed] [Google Scholar]
- 7.Murphy D.R. 2007. Pathology, diagnosis, and treatment of lumbar radiculopathy. FCER Clinical Teleconference; May 31. Norwalk IA. [Google Scholar]
- 8.Ahlgren B.D., Garfin S.R. Cervical radiculopathy. Orthop Clin North Am. 1996;27(2):253–263. [PubMed] [Google Scholar]
- 9.Karppinen J., Malmivaara A., Tervonen O. Severity of symptoms and signs in relation to magnetic resonance imaging findings among sciatic patients. Spine. 2001;26(7):E149–E154. doi: 10.1097/00007632-200104010-00015. [DOI] [PubMed] [Google Scholar]
- 10.Rubinstein S.M., Pool J.J.M., van Tulder M.W., Riphagen I.I., de Vet H.C.W. A systematic review of the diagnostic accuracy of provocative tests of the neck for diagnosing cervical radiculopathy. Eur Spine J. 2007;16:307–319. doi: 10.1007/s00586-006-0225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tong H.C., Haig A.J., Yamakawa K. The Spurling test and cervical radiculopathy. Spine. 2002;27(2):156–159. doi: 10.1097/00007632-200201150-00007. [DOI] [PubMed] [Google Scholar]
- 12.Boden S.D., McCowin P.R., Davis D.O. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;27(8):1178–1184. [PubMed] [Google Scholar]
- 13.Birchall D., Connelly D., Walker L., Hall K. Evaluation of magnetic resonance myelography in the investigation of cervical spondylotic radiculopathy. Br J Radiol. 2003;76(908):525–531. doi: 10.1259/bjr/99259611. [DOI] [PubMed] [Google Scholar]
- 14.Saal J.S. The role of inflammation in lumbar pain. Spine. 1995;20(16):1821–1827. doi: 10.1097/00007632-199508150-00013. [DOI] [PubMed] [Google Scholar]
- 15.Wainner R.S., Fritz J.M., Irrgang J.J., Boninger M.L., Delitto A., Allison S. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine. 2003;28:52–62. doi: 10.1097/00007632-200301010-00014. [DOI] [PubMed] [Google Scholar]
- 16.Cleland J. Orthopaedic clinical examination. MediMedia, Inc; Amsterdam, The Netherlands: 2005. p. 189. [Google Scholar]
- 17.Morris C.E. Low back syndromes. McGraw-Hill; Philadelphia: 2006. p. 324. [Google Scholar]
- 18.Liebenson C. Rehabilitation of the spine. Lippincott Williams & Wilkins 2007. p. 467,472-3.
- 19.Workers Compensation Research Institute. WCRI flash report, July 2007, OSBM 978-1-934224-61-8.
- 20.Ostelo R.W., Deyo R.A., Stratford P. Interpreting change scores for pain and functional status in low back pain. Spine. 2008;33:90–94. doi: 10.1097/BRS.0b013e31815e3a10. [DOI] [PubMed] [Google Scholar]
- 21.Rogers C., Joshi A., Dreyfuss P. Cervical intrinsic disc pain and radiculopathy. In: Malanga G.A., editor. Cervical flexion-extension/whiplash injuries vol. 12: 2. Spine: state of the art reviews. 1998. pp. 323–356. [Google Scholar]


