Abstract
Although much has been written about the utility of applying Sameroff and Chandler's transactional perspective to the study of child psychopathology, relatively few researchers have used such an approach to trace the emergence of child problem behavior from infancy to adolescence. Using a sample of 289 male toddlers from predominantly low-income families, the current study examined associations between various forms of early child disruptive behavior, subsequent trajectories of maternal depressive symptoms over the course of 8 years, and adolescent problem behavior. Results indicated that early child noncompliance was the most robust predictor of more chronic and elevated trajectories of maternal depression, which in turn discriminated teacher and youth reports of adolescent antisocial behavior but not internalizing symptoms. The findings were consistent with transactional perspectives of developmental psychopathology that have emphasized the dynamic interplay between child and parent characteristics.
Depression is a prevalent mental health illness, affecting approximately 18% to 27% of the population at some point in their lives (Kringlen, Torgenson, & Cramer, 2001; Weissman & Myers, 1978). Investigations across a number of countries have consistently found that depression affects women disproportionately (Nolen-Hoeksema, 1987; Weissman & Klerman, 1977); lifetime and point prevalence of major depression are twice as high for women compared to men (e.g., lifetime: 10−25% vs. 5−12% among women and men, respectively; Kringlen et al., 2001). Even at a subclinical level, these symptoms can cause distress or impairment in family, work, and social situations (Farmer, McGuffin, & Williams, 2002).
A number of explanations have been proposed to account for the gender discrepancy in rates of depression. Although there is some support for the contribution of biological and hormonal factors that put women at greater risk for depression than men, thus far a specific biological mechanism that translates into this gender disparity has yet to be identified (Bebbington, 1996; Nolen-Hoeksema & Keita, 2003). Instead, research has found that factors related to social conditions may increase women's vulnerability to depression (Bebbington, 1996; Nolen-Hoeksema, 1987, 1990; Nolen-Hoeksema & Keita, 2003). In addition, women show higher rates of engaging in cognitive and interpersonal styles that are associated with depression (e.g., rumination, negative attributional style, a strong affiliative relational style, and high levels of self-evaluative concerns; Cyranowski, Frank, Young, & Shear, 2000; Nolen-Hoeksema, 1991; Ruble, Greulich, Pomerantz, & Gochberg, 1993).
One factor that may contribute to higher rates of depressive symptoms in females, specifically mothers, is the stress related to child rearing, particularly for mothers from lower socioeconomic strata with young children. Research has found that women who have a child under age 6, live in poverty or are of low socioeconomic status (SES) and lack a supportive social network are at increased risk for experiencing depressive symptoms (Brown & Harris, 1978; Lewinsohn, Hoberman, & Rosenbaum, 1988).
Maternal Depression and Child Adjustment
Throughout this paper, the term maternal depression will be used to describe both mothers who have met clinical criteria for unipolar depression and those who obtained elevated scores on inventories of depressive symptoms. In both cases, associations have been documented with parental functioning and child outcomes (Cummings, Keller, & Davies, 2005; Farmer et al., 2002). When individual studies are reviewed, the term maternal depressive symptoms will be used when depression was quantified by elevated scores on an inventory of depressive symptoms and clinical depression will refer to studies that used diagnostic criteria.
In addition to the deleterious effects of depression on women, research has found that children are affected by their mother's depression. Associations between maternal depression and child outcomes, including child adjustment, emotional well-being, and problem behavior, are well documented. Mothers who are high in depressive symptoms or diagnosed with clinical depression may not only pass along a genetic vulnerability for mood disorders but also parent in ways that can place children at risk for a range of problems (Cummings & Davies, 1994; Downey & Coyne, 1990; Gelfand & Teti, 1990; Zahn-Waxler, Iannotti, Cummings, & Denham, 1990). For example, Zahn-Waxler et al. (1990) and others (Shaw & Bell, 1993) have noted that depressed individuals are typically negative, critical, unresponsive, helpless, and passive toward others, including their children. Furthermore, in at-risk young children, parenting practices characterized by unresponsiveness and hostility have been consistently linked to the development of behavior problems during both the preschool (Shaw, Keenan, & Vondra, 1994; Shaw et al., 2006) and school-age periods (Renken, Egeland, Marvinney, Mangelsdorf, & Sroufe, 1989).
Prior research has found associations between maternal depression and multiple domains of child adjustment across developmental periods. Although researchers have studied children of depressed mothers in both narrowly defined developmental periods and across broad age spans (Goodman & Gotlib, 1999), disruptions may manifest differently depending on the developmental task typically accomplished at each age (Elgar, McGrath, Waschbusch, Stewart, & Curtis, 2004; Gelfand & Teti, 1990). Both LaRoche (1989) and Beardslee (1986) assert that early infancy and adolescence are periods of particular vulnerability, as maternal depression may interfere with the ability of an infant to form an attachment relationship and of an adolescent to form an autonomous identity.
Maternal depression has been linked to a number of child outcomes during infancy and early childhood, including observer and maternal report of elevated fussiness and more difficult temperaments (Cutrona & Troutman, 1986; Whiffen & Gotlib, 1989), lower scores on measures of mental and motor development (Cogill, Caplan, Alexandra, Robson, & Kumar, 1986; Murray, Fiori-Cowley, Hooper, & Cooper, 1996; Sharp et al., 1995), insecure attachments as assessed by independent observers (Campbell et al., 2004; Lyons-Ruth, Zoll, Connell, & Grunebaum, 1986; Murray, 1992), higher rates of parent-reported behavior problems (Ghodsian, Zajicek, & Wolkind, 1984; Marchand, Hock, & Widaman, 2002; Shaw et al., 1994), and avoidance and withdrawal in their interactions as assessed by parents, teachers, and independent raters (Alpern & Lyons-Ruth, 1993; Cohn, Matias, Tronick, Connell, & Lyons-Ruth, 1986; Field et al., 1988).
Studies of outcomes for school-aged children and adolescents of depressed mothers have documented associations between maternal depression and maternal and teacher reports of children's low social competence and adaptive functioning (Luoma et al., 2001), higher rates of externalizing problems and more serious forms of antisocial behaviors as assessed by parent, teacher, and self-report (Hay, Pawlby, Angold, Harold, & Sharp, 2003; Munson, McMahon, & Spieker, 2001; Owens & Shaw, 2003), poor adjustment and lower levels of self-esteem as reported by parents and teachers (Cummings et al., 2005; Wilkins et al., 2004), teacher reports of academic and behavior problems at school (Sinclair & Murray, 1998), and elevated rates of internalizing behaviors, especially depression (Cummings et al., 2005; Hammen & Brennan, 2003; Leve, Kim, & Pears, 2005).
Reciprocal Associations Between Child and Mother
Despite the wealth of existing literature that documents associations between maternal depression and child outcomes, there are few studies that examine how child characteristics and behaviors may contribute to and exacerbate mother's depressive symptoms. Coyne's interpersonal model of depression describes how depressed adults elicit negative reactions from others that intensify their unhappiness and negativity in a cycle of mutual distress (Coyne, Kahn, & Gotlib, 1987). Nelson, Hammen, Brennan, and Ullman (2003) speculate that maternal depression may create dysfunctions in the early parent–child relationship and elicit problems in the child, which would, in turn, maintain negative maternal attitudes. In support of these reciprocal effects, studies have documented higher rates of maternal depressive symptoms in clinic-referred versus normal children (Brown, Borden, Clingerman, & Jenkins, 1988; Fergusson, Lynskey, & Horwood, 1993) and in mothers whose children have more behavioral or emotional problems (Civic & Holt, 2000). However, the majority of studies have used cross-sectional rather than longitudinal designs, and the perceived methodological difficulties to testing reciprocal pathways have resulted in limited empirical findings (Sameroff & MacKenzie, 2003).
Another methodological limitation of prior research is that few have addressed the possibility that children's behaviors may affect maternal depression as early as infancy, and that mothers likely experienced elevated rates of depressive symptoms prior to the onset of their children's behavior problems. Some research has focused on how infant characteristics, including temperament and interaction style with adults, may elicit or maintain particular parental behaviors. For example, Field et al. (1988) found that when infants of depressed mothers interacted with nondepressed adults in avoidant and unresponsive ways, these nondepressed adults began to exhibit depressed-like manners in these interactions. Crockenberg (1981) found that easygoing children were more impervious to their mother's behavior than were irritable children. Downey and Coyne (1990) speculated that this imperviousness “may impede the development of the reciprocal pattern of negativity often seen in the interactions of depressed mothers and their children” (p. 68). Other studies have found that behavior problems and irritability in infants are associated with the continuation of maternal clinical depression (Ghodsian et al., 1984) and the onset of postpartum depression (Murray, Stanley, Hooper, King, & Fiori-Cowley, 1996).
In a study utilizing an experimental design, Pelham et al. (1997) had married couples and single mothers interact with 5- to 12-year-old boys who were trained to behave in either a normal or defiant manner. While waiting to have a second interaction with the same boy, the adults completed questionnaires, including one assessing depressive symptoms. Those who had interacted with the defiant boys reported significantly higher levels of depressive symptoms than those interacting with nondefiant children. The experimental design addressed the bias inherent in having depressed mothers report on their child's behavior, as some researchers contend that negative cognitive styles and associated family dysfunction may lead depressed mothers to negatively distort their perceptions of their children's behaviors (Boyle & Pickles, 1997; Fergusson et al., 1993). Specifically, informants with higher levels of depression have been found to overestimate behavior problems, perceptions that may contribute to negative caregiving interactions (Goodman & Gotlib, 1999).
Another study examined whether individual differences in initial child behavior and child frontal asymmetry (i.e., EEG) were associated with changes in maternal report of depressive symptoms one year later (Forbes et al., 2006). Results indicated that mothers whose 3- to 9-year-old children had either below-average affect regulation and/or right frontal EEG asymmetry reported increased depressive symptoms 1 year later.
Although these findings are consistent with a reciprocal effects model of maternal depressive symptoms across a number of ages, it is possible that such effects are particularly prominent in early childhood. In particular, the “terrible twos” have been identified as a period of high parental dissatisfaction relative to the first year (Fagot & Kavanagh, 1993), when children's increasing mobility coupled with continued cognitive limitations in their ability to grasp important principles (e.g., gravity, electricity, consequences of physical aggression on others) increase the stresses and challenges of caregiving on maternal well-being (Shaw, Bell, & Gilliom, 2000; Zahn-Waxler et al., 1990). Thus, results from the extant literature suggest that child characteristics may be associated with maintenance and increases in maternal depressive symptoms, particularly in early childhood.
Chronicity and Severity of Maternal Depressive Symptoms
Another limitation of the existing research on maternal depression and its relation to child outcomes is the inability to partition chronicity and severity of maternal depressive symptoms from one another, factors that may help to explain discrepant findings in the field (Campbell et al., 2004). In general, studies that have included measurements of severity and/or chronicity of depressive symptoms have shown that more severe and chronic levels are associated with higher levels of children's depression, anxiety, and externalizing problems (Hammen & Brennan, 2003; Keller et al., 1986; Warner, Mufson, & Weissman, 1995). Brennan et al. (2000) found children whose mothers had experienced both chronic and severe depressive symptoms demonstrated significantly more behavior problems than children whose mothers had only chronic or severe depressive symptoms. In contrast, Rutter (1990) has suggested that children may be better able to understand and accept more severe parental pathology and find less severe symptoms to be more arbitrary and disturbing. In support of this, Hammen and Brennan (2003) found that the effects of maternal depression were not linear, with youth depression decreasing for exposure to moderate and severe maternal, clinical depression.
Research Questions
In the current study, we sought to advance our understanding of reciprocal influences on maternal depressive symptoms and subsequent risk of child problem behavior. First, we used a semiparametric modeling technique (Nagin, 2005) to identify developmental trajectories of maternal depressive symptoms during an 8.5-year span among a group of predominantly low-income mothers and their toddler-age sons. We are unaware of any existing studies that have traced trajectories of depressive symptoms among a sample of low-income mothers from early to middle childhood. Based on the high recurrence rates of depression (i.e., at least 60% of individuals who have one depressive episode will have another, 70% with two episodes will have a third, and 90% with three episodes will have a fourth, according to the American Psychiatric Association [APA], 2000), we hypothesized that there would be at least one persistent low depressive symptom group and at least one persistent high group in addition to two or three moderate trajectory groups.
Second, and following up the work of Pelham et al. (1997) and Forbes et al. (2006), we sought to address whether child characteristics, observed prior to the assessment of maternal depression trajectories, would discriminate trajectory group membership. Based on the existing literature, we predicted that children showing higher levels of observed irritability, aggression, and/or noncompliance would be more likely to have mothers demonstrating more severe and chronic trajectories of depressive symptoms. We chose to restrict our measurement of child behaviors perceived by parents to be aversive (e.g., noncompliance, aggression) to the beginning of the toddler period (i.e., at 18 months), a time identified as challenging for parents in general, and in particular, for parents from lower SES due to fewer social and economic resources. Third, we assessed long-term child outcomes associated with different types of maternal depression trajectories, examining youth and teacher reports of youth externalizing and internalizing symptoms between the ages of 11 and 13. We predicted that more persistent and severe trajectories of maternal depressive symptoms would be associated with higher levels of boys’ internalizing and externalizing symptoms during early adolescence.
Method
Participants
Subjects were recruited from the Allegheny County Women, Infants and Children (WIC) program in the Pittsburgh Metropolitan area (Shaw et al., 1998). The sample was restricted to boys because of the larger study's primary goal, to examine antecedents of antisocial behavior. Out of 421 families approached at WIC sites, 310 participated in the first assessment when the boys were 18 months old. At the time of recruitment, all families met the income requirements for WIC and had a child between 6 and 17 months of age. At the initial assessment, mothers ranged in age from 17 to 43 years, with a mean age of 28. Fifty-five percent of the sample was European American, 40.5% African American, 5% biracial, and 4% other (e.g., Hispanic, Asian). Sixty-four percent of mothers were married or living together, 28% were single, 7% were divorced, and 1% identified as “other.” There were an average of 2.67 children living in the household, with a range of one to seven children (SD = 0.939). Mean per capita family income was $236 per month (SD = 143; range = 29.3−1,000), with a mean Hollingshead SES score of 23.3, indicative of a working class sample. The study retention rate was relatively high, with 275 families (88.7% of the original sample of 310) participating in the age 10, 11, or 12 assessments.
Of the original 310 families recruited for participation in the study, 289 met criterion to be included in analyses by having maternal depression data for at least three time points. Families were excluded when the primary caregiver who completed the Beck Depression Inventory (BDI; Beck, Ward, Mendelson, Mock, & Erbaugh, 1961) changed and remained different during the course of the study; however, if a different person completed the Beck at just one or two time points, those families were retained and the data from the second primary caregiver were not used. This subsample was not significantly different from the original sample on maternal education, F (312) = 3.64, p < .10, family income, F (310) = 0.09, ns, maternal age, F (310) = 0.19, ns, or SES, F (313) = 0.38, ns.
Procedures
Mothers and target children were seen when the children were ages 1.5, 2, 3.5, 5, 5.5, 6, 8, 10, 11, and 12 years. Data were collected in the laboratory (ages 1.5, 2, 3.5, 6, and 11 years) and/or at home (ages 2, 5, 5.5, 8, 10, and 12 years). In addition, teacher data were collected by mail when the children were 10 through 13 years old. At the age 1.5 assessment, observations of the parent–child dyad were completed and coded for instances of noncompliance, aggression, and infant irritability. Demographic variables, including income, social status, and number of children in the household, were collected in the age 1.5 interview with the primary caregiver. Finally, mothers completed the BDI at all time points.
Measures
Aggression
Child aggressive behavior was coded in the laboratory during selected structured tasks during the 18-month assessment. Tasks were chosen to vary in stress level (e.g., Strange Situation vs. free play) and aggression was coded during a clean-up task, a no-toys task, two 5-min free play periods, and during two segments of the Strange Situation. The total coding time was 23 min. Codes, developed by Keenan and Shaw (1994), included aggression directed toward the mother or examiner (throwing toys at mother and/or examiner, hitting or kicking mother and/or examiner) and aggression directed toward toys or objects in the observation room. Counts of aggression were collapsed across situations and types to generate a total summary score of seconds the child showed aggression. Coders were trained and supervised undergraduate students who were unaware of any information about the families or research hypotheses. Interrater reliabilities, using kappas, were at or above 85% for all five aggression codes based on a random sampling of 10% of the tapes coded by each rater. In addition to calculating reliability for initial tapes, reliability was checked at 6-month intervals.
Noncompliance
Noncompliance was coded during a 5-min clean-up task at the 18-month assessment based on a molecular system developed by Martin (1981). Noncompliant behaviors included walking away, passive noncompliance, changing the task, and struggling or resisting. As different forms of noncompliance were highly correlated (i.e., r > .90), they were aggregated into a composite. The final score indicated how many seconds the child demonstrated various forms of noncompliance. A separate team of undergraduates was trained to code noncompliance versus aggression. The kappa for the final composite of noncompliance score was .71 based on 10% of the tapes coded by each rater.
Infant irritability
Irritability was assessed across all observational tasks administered at the 18-month assessment, including a free play, a clean-up task (Matas, Arend, & Sroufe, 1978), a no-toys task (Smith & Pederson, 1988), three teaching tasks (Martin, 1981), and throughout the entire Strange Situation (Ainsworth & Wittig, 1969), resulting in approximately 1 hr of coded observation. Coders recorded the duration of infants’ fussing or crying; a percentage was generated by dividing this by the length of observation. The same coders completed 5-point global ratings of the amount and intensity of the infant's fussing and crying as well as a global rating for infant difficulty (Owens, Shaw, & Vondra, 1998). Interrater agreement in the form of weighted kappas was calculated across 22 randomly selected cases and ranged from .77 to .96, with a mean of .87. Scores for percent of time spent fussing and crying, global amount and intensity of fussing and crying, and global difficulty were standardized and summed into an observed irritability score, with a reliability coefficient α of .91.
BDI
Mothers completed the BDI (Beck, Ward, Mendelson, Mock, & Erbaugh, 1961), a widely used measure of depressive states, at all assessments (e.g., children's ages 1.5, 2, 3.5, 5, 5.5, 6, 8, 10, 11, and 12 years). This measure is appropriate for both measuring intensity of depressive symptoms in psychiatric populations and detecting depressive symptoms in normal populations. Respondents rate the intensity of 21 depressive symptoms on a 0 (no symptomatology) to 3 (severe symptomatology) scale, and a score is derived by summing these ratings. Reliability and external validity of the BDI are high (Beck, Steer, & Garbin, 1988). In this sample, the reliability of the BDI ranged from .82 to .89, with an average Cronbach α of .86 across all 10 time points. Descriptive statistics for the total BDI scores at all assessments are presented in Table 1.
Table 1.
Descriptive statistics for BDI total score at all assessments
| Child's Age (years) | N | Mean | SD |
|---|---|---|---|
| 1.5 | 281 | 8.95 | 6.82 |
| 2 | 285 | 7.55 | 6.16 |
| 3.5 | 267 | 7.08 | 6.65 |
| 5 | 265 | 7.91 | 6.77 |
| 5.5 | 201 | 7.39 | 6.69 |
| 6 | 244 | 6.86 | 6.35 |
| 8 | 237 | 6.50 | 6.99 |
| 10 | 230 | 6.70 | 6.93 |
| 11 | 223 | 6.96 | 6.74 |
| 12 | 218 | 6.67 | 6.30 |
Note: BDI, Beck depression Inventory (Beck et al., 1988).
Self-Reported Delinquency (SRD)
Youth completed the SRD measure at ages 11 and 12 (Elliot, Huizinga, & Ageton, 1985). This is a questionnaire that assesses the context and frequency of offending and examines overt, covert, destructive, and nondestructive offenses. Self-reported measures of delinquency have been shown to have strong psychometric properties, with test–retest reliabilities ranging from .75 to .98 and internal consistency as from .65 to .92 (Krueger et al., 1994). The SRD is considered to be a highly respected self-report assessment of delinquency with good psychometric properties. In our sample, a composite score was used by summing the number of delinquent acts committed, with internal consistencies of .88 at age 11 and .84 at age 12. To minimize missing data, when data were available only at age 11 or at age 12, the total score from that age was used. If data were obtained at both time points, a composite score was derived by averaging the two scores.
Teacher Report Form (TRF)
Classroom teachers completed the TRF (Achenbach, 1991) when the children were ages 11 through 13. The TRF is a widely used measure of child problem behavior consisting of 115 items that has adequate internal consistency and reliability (Achenbach, 1991). For purposes of the present study, we used two broadband factors: the 36-item internalizing and 34-item externalizing factors. In this sample, internal consistencies were uniformly high from ages 11 to 13 (internalizing factor range = .86−.89, externalizing factor range = .92−.97). When data were available for only one age (n = 106), it was used as the final score. For participants with TRF scores available on two (n = 94) or three (n = 5) assessments, scores were averaged across available time points.
Analysis plan
Group-based trajectory modeling
In the first step of the current study, we used a semiparametric, group-based approach (Nagin, 2005) to model the trajectory of depressive symptoms among mothers from when their sons were ages 1.5 to 10 years of age (Figure 1). The method is designed to identify clusters of individuals who share common pathways. This method may be particularly relevant for examining maternal depressive symptoms because it addresses such issues as course, timing, and severity of symptoms, which have been helpful in explaining discrepant findings in relation to child outcomes (Campbell et al., 2004). In addition, this method is designed to handle data that are missing completely at random; when data are missing, the equations in the base model are adapted to accommodate missing observations and the sample size count is adjusted so as not to include missing observations (Nagin, 2005). As a result, this method is useful for longitudinal data analysis, allowing the researcher to retain individuals with incomplete assessment histories.
Figure 1.
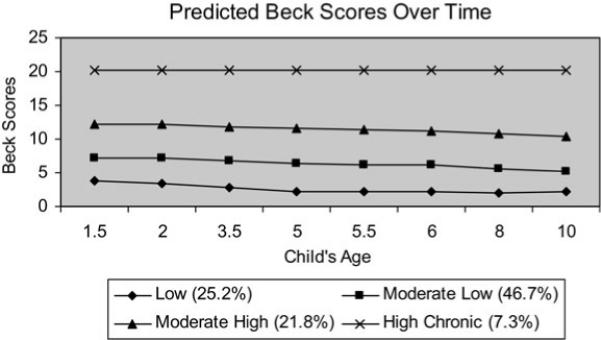
Trajectories of maternal depressive symptoms from ages 1.5 to 10.
Technically, the group-based trajectory model is an example of a finite mixture or latent class model. A polynomial function is used to model the relationship between an attribute (e.g., maternal depressive symptoms) and age or time (Nagin, 1999, 2005; Nagin & Tremblay, 1999). The models were estimated with a specialized SAS-based procedure called “Proc Traj” which is described in Jones, Nagin, and Roeder (2001) and Jones and Nagin (2007). A censored normal model was fitted to the data. Censored normal models are used not only in group-based models, but in conventional single-group models that use psychometric scale data where a significant number of participants cluster at the scale maximum or minimum. In this analysis, there were a significant number of mothers who exhibited no or few depressive symptoms, resulting in a cluster of data at the scale minimum. By formally accounting for this censoring in the specification of the likelihood function, the censored normal model provides consistent estimates of the parameters of the polynomial relationship that describe the trajectory equations for each group. A more comprehensive discussion of the technical details of this approach can be found elsewhere (Nagin, 1999, 2005; Nagin & Tremblay, 1999).
In selecting the optimal trajectory group model, the Bayesian information criteria (BIC) is typically used to identify the best fit in both number and shape of groups (D'Unger, Land, McCall, & Nagin, 1998). Following the recommendation of Kass and Rafferty (1995), model selection is guided by the objective of maximizing the BIC score. The model generates posterior probabilities of group membership, which estimates each individual's probability of belonging to each of the trajectory groups. Individuals are assigned to the group with the largest posterior probability estimate.
Risk factor and outcome analysis
Once the trajectories were established, we sought to address two core questions. First, what are the child effects on mothers’ depression trajectories? Second, how do mothers’ depression trajectories predict chidren's outcomes? To examine these questions, we first conducted exploratory analyses of variance (ANOVAs) to determine if there were early child behaviors that showed differences among mothers who had been assigned to different depression trajectory groups based on their posterior probabilities of group membership. Having identified candidate risk factors for trajectory group membership, we then estimated a generalized group-based model in which probability of trajectory group membership varied as a function of these risk and protective factors. As described in Nagin (2005), a multinomial logit function is used to specify this probability function. By estimating a generalized model in which probability of trajectory group membership is conditional on individual characteristics and the trajectories themselves are jointly estimated, we avoid biases in statistical tests due to classification error in trajectory group membership. Finally, an analysis of covariance (ANCOVA) was conducted to examine if trajectory group status was associated with child adjustment outcomes at ages 11, 12, and 13 after accounting for the effects of child noncompliance assessed at 18 months.
Results
Identification of trajectories
The first step was to model trajectories of maternal depressive symptoms from the time the children were 1.5 to 10 years of age. Various models were examined with regard to the characteristics and number of trajectory groups (see Table 2). As BIC scores generally improve as more groups are added, and this occurred in the current study, BIC scores were not the only criterion used for model selection (Nagin, 2005). Despite improved BIC scores, both the five and six group models resulted in subdividing already modest-size groups with higher levels of maternal depressive symptoms into smaller groups that were not substantively different from one another; thus, the four group model emerged as the best fitting and most parsimonious model.
Table 2.
Model fit indices
| No. of Groups | BIC (N = 2010) | BIC (N = 289) |
|---|---|---|
| 2 | −6051.68 | −6043.92 |
| 3 | −5939.25 | −5927.61 |
| 4 | −5922.20 | −5906.69 |
| 5 | −5906.03 | −5886.64 |
| 6 | −5897.97 | −5874.69 |
Note: BIC, Bayesian information criterion.
Groups 1 and 2, comprising the majority of the sample, demonstrated BDI scores suggestive of minimal depressive symptomatology (Beck et al., 1988). Group 1, which we term “low,” consisted of 25.2% (n = 73) of the sample who endorsed very few depressive symptoms across all time points (M = 2.0 across the eight time points). Group 2, which we term “moderate low,” included 45.7% (n = 132) of the sample and was characterized by a consistent pattern of moderately low depressive symptoms (M = 6.25 across eight time points). Group 3 included 21.8% (n = 63) mothers, which we term “moderate high.” This group consistently had BDI scores in the moderate depression range (M = 11.75 across all time points), with a slight decrease over time (M = 13.05 at age 1.5 versus M = 10.82 at age 10). Group 4, which included 7.3% (n = 21) of the sample, is termed the “high chronic group,” with scores suggestive of moderate to severe levels of depression at all time points (M = 20.55 across assessments).
The average posterior probability for each group was calculated to confirm the adequacy of the final four-group model. Posterior probabilities measure a specific individual's likelihood of belonging to each of the model's trajectory groups (Nagin, 2005). As shown in Table 3, for all four groups the average posterior probabilities fell well above the lower recommended threshold for assignment of .7 (Nagin, 2005). The range in the current sample was .83 (moderate low group) to .97 (high chronic group). In addition, we found that the model met three other indicators of model adequacy recommended in Nagin (2005): a close correspondence between each group's estimated probability and the proportion of individuals actually classified to the group on the basis of the maximum posterior probability assignment rule, reasonably tight confidence intervals on group membership probabilities, and high odds of correct group classification relative to chance.
Table 3.
Diagnostic statistics for judging model selection
| Group | Ave. Post. Prob. | Propor. Assigned to Each Group | Estim. Using Model |
|---|---|---|---|
| 1 (low) | .89 | .25 | .27 |
| 2 (moderate low) | .83 | .46 | .43 |
| 3 (moderate high) | .87 | .22 | .22 |
| 4 (high chronic) | .97 | .07 | .07 |
Risk factors for depression trajectory membership
The next step was to examine child characteristics that may be associated with the trajectory group membership of mother's depressive symptoms. A series of exploratory ANOVAs was computed to examine the associations between trajectory group membership and individual child risk factors (see Table 4). Each child risk factor examined, including observed noncompliance, aggression, and infant irritability, showed significant associations with maternal depression group status; however, findings were not uniformly in the expected direction, particularly for infant irritability where the moderate low group showed the highest levels and aggression where the high chronic group had the lowest levels. Post hoc tests indicated that for noncompliance, children of mothers in the high chronic group were found to have significantly higher BDI scores than children of mothers in the low group, F (1, 215) = 11.14, p = .001, with p < .008 cutoff for significance using Bonferroni adjustment. For infant irritability, the moderate low group had significantly higher BDI scores than the low group, F (1, 278) = 8.29, p = .004. There were no significant, post hoc contrasts among groups for aggression.
Table 4.
ANOVA of 18-month child risk factors by trajectory group
| Group | N | Aggression | Infant Irritabil. | Noncompl. |
|---|---|---|---|---|
| L | 70 | .08 | −.88ML | −.34HC |
| ML | 131 | −.16 | .60L | .07 |
| MH | 62 | .20 | −.13 | .03 |
| HC | 19 | −.20 | .31 | .63L |
| F | 2.81, df = 259 | 2.86, df = 281 | 4.31, df = 218 | |
| p | .04 | .04 | <.01 |
Note: ANOVA, analysis of variance; L, low; ML, moderate low; HC, high chronic; MH, moderate high. Superscript letters reflect significant differences between other groups in that column. Maximum N values are reported for each group, but actual N values vary by data available for each child risk factor.
Next, we sought to examine the unique contribution of all three child variables in distinguishing trajectory group membership. We retained all three child variables in this multivariate logit analysis because the results of the ANOVAs found that each child factor showed differences in means by maternal depression trajectory groups. In this analysis, all groups were first compared to the low group using a multivariate logit analysis (Table 5), and then all other pairs of trajectory groups were contrasted using Wald tests of equality (Table 6). As low SES and income may increase the risk of the onset and persistence of depression (Lorant et al., 2003), both variables were also entered into each logit equation and then subjected to Wald tests. Number of children in the household was also entered as a covariate, to control for the effects of family size on depression in this sample of economically depressed women. When all risk factors were entered in the model, only noncompliance consistently distinguished depression group membership, with greater child noncompliant behavior associated with higher levels of maternal depression. Noncompliance distinguished between the low group and both the moderate low and high chronic groups (B = 0.50 and 1.21, p = .02 and p < .001, respectively) and gave some indication of distinguishing between the low and moderate high groups (B = 0.46, p = .05). Noncompliance also distinguished between the moderate low and high chronic groups and the moderate high and high chronic groups in the expected direction (χ2 = 4.29 for moderate low and high chronic groups, p < .05, χ2 = 3.85 for comparison between moderate high and high chronic groups, p = .05). Family income significantly distinguished between the low and high chronic groups (B = 0.00, p < .05) and showed some indication of distinguishing the high chronic from the moderate low (χ2 = 3.87, p < .05) and from the moderate high groups (χ2 = 3.26, p < .10). In all cases, family income was significantly lower in the high chronic group. Child aggression showed some indication of discriminating trajectory group membership in only one comparison; aggression was higher for children in the moderate high group than the moderate low group (χ2 = 3.79, p = .05). Within a multivariate framework, infant irritability, family SES, and number of children in household were not found to distinguish between any pairs of trajectory groups.
Table 5.
Multivariate logit analysis for predicting trajectory group membership with each group compared to low
| Low Vs. Moderate Low |
Low Vs. Moderate High |
Low Vs. High Chronic |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Predictor Variables | B | Wald Test | p | B | Wald Test | p | B | Wald Test | p |
| Family income | 0.00 | 0.28 | .60 | 0.00 | 0.00 | .14 | 0.00 | 4.43 | .04 |
| SES | 0.01 | 0.09 | .77 | 0.00 | 0.01 | .92 | 0.07 | 2.18 | .14 |
| No. of children in home | −0.01 | 0.00 | .97 | 0.09 | 0.14 | .71 | 0.41 | 1.54 | .22 |
| Aggression | −0.24 | 1.16 | .28 | 0.19 | 0.70 | .40 | −0.33 | 0.50 | .48 |
| Noncompliance | 0.50 | 5.68 | .02 | 0.46 | 3.80 | .05 | 1.21 | 12.25 | .00 |
| Infant irritability | 0.10 | 3.30 | .07 | 0.05 | 0.57 | .45 | −0.02 | 0.03 | .86 |
Note: SES, socioeconomic status.
Table 6.
Wald tests of equality and comparisons of regression coefficients in all pairs of trajectory groups
| Moderate Low Vs. Moderate High |
Moderate Low Vs. High Chronic |
Moderate High Vs. High Chronic |
||||
|---|---|---|---|---|---|---|
| Predictor Variables | Wald-Based χ2 | p | Wald-Based χ2 | p | Wald-Based χ2 | p |
| Family income | 0.00 | .95 | 3.87 | .05 | 3.26 | .07 |
| SES | 0.690 | .41 | 1.57 | .21 | 2.76 | .10 |
| No. of children in home | 0.44 | .51 | 1.79 | .18 | 0.55 | .46 |
| Aggression | 3.79 | .05 | 0.00 | .99 | 1.49 | .22 |
| Noncompliance | 0.02 | .90 | 4.29 | .04 | 3.85 | .05 |
| Infant irritability | 0.57 | .45 | 1.16 | .28 | 0.23 | .63 |
Note: SES, socioeconomic status.
Outcome analysis: Youth externalizing and internalizing problems during early adolescence
Our final goal was to evaluate whether maternal depression trajectory group membership predicted boys’ later externalizing symptoms, as measured by both TRF and self-reported SRD, and internalizing symptoms, as measured by the TRF. We conducted an ANCOVA to examine differences in boys’ reports of antisocial activities (i.e., SRD) and teacher reports of externalizing and internalizing symptoms by maternal depression trajectory group after controlling for 18-month child noncompliance. We then examined Bonferroni post hoc tests to look at the differences in outcomes among the maternal depression trajectory groups.
There was a significant effect of trajectory group status on boys’ self-reported delinquent behavior when controlling for 18-month non-compliance, F (4, 169) = 5.79, p < .001 (see Table 7). Post hoc tests indicated that self-reported delinquency in the moderate high group was significantly higher than in the low and moderate low groups (moderate high, M = 5.87; low, M = 2.48; moderate low, M = 3.31; ps < .01 for both comparisons).
Table 7.
Descriptive statistics for self-reported delinquency at ages 11 and 12
| Group | N | Mean | SD |
|---|---|---|---|
| 1 (low) | 46 | 2.16MH | 2.16 |
| 2 (moderate low) | 75 | 3.31MH | 3.36 |
| 3 (moderate high) | 38 | 5.87L,ML | 4.57 |
| 4 (high chronic) | 15 | 3.73 | 3.57 |
Note: L, low; MH, moderate high; ML, moderate low; HC, high chronic. Superscript letters reflect significant differences between the groups in the same column.
For teacher reports using the TRF, the ANCOVA found significant effects for externalizing, F (4, 158) = 3.81, p < .01, but not internalizing, F (4, 158) = 1.80, p = .131, outcomes after controlling for 18-month noncompliance (see Table 8). Post hoc tests indicated that teachers rated boys of mothers in the moderate high group to have significantly higher externalizing symptoms than boys of mothers in the low and moderate low groups (moderate high, M = 18.20; low, M = 9.55; moderate low, M = 10.85; ps < .01 for both comparisons). The externalizing scores among boys in the moderate high group were similar to the mean of a sample of clinic-referred boys, indicating that the level of externalizing behaviors for this group was elevated compared to a normal population (M = 15.7, SD = 12.4 for clinic-referred boys age 6−11, M = 18.1, SD = 13.6 for clinic-referred boys aged 12−18; Achenbach & Rescorla, 2001). In all three outcome analyses, 18-month noncompliance was not significantly related to youth outcomes (ps = .39−.71).
Table 8.
Descriptive statistics for Teacher Report Form outcomes at ages 11−13
| Mean |
|||
|---|---|---|---|
| Group | N | Externalizing | Internalizing |
| 1 (low) | 45 | 9.64MH | 5.21 |
| 2 (moderate low) | 69 | 10.81MH | 5.87 |
| 3 (moderate high) | 33 | 18.20L,ML | 8.20 |
| 4 (high chronic) | 12 | 12.33 | 4.96 |
Note: L, low; MH, moderate high; ML, moderate low; HC, high chronic. Superscript letters reflect significant differences between the groups in the same column.
Discussion
This study sought to examine early child predictors of trajectories of maternal depressive symptoms followed over an 8.5-year period and youth outcomes in early adolescence associated with these trajectory groups. The trajectory analysis showed four relatively stable groups of maternal depressive symptoms, including low, moderate low, moderate high, and high chronic groups. Although the majority of the sample (71%) fell in either the low or moderate low groups, 63 mothers (21.8%) showed a consistent pattern of moderately high levels of depressive symptoms, and an additional 21 mothers (7.3%) demonstrated severe levels of depressive symptoms across all time points. The findings for the two persistently high groups are consistent with previous studies suggesting that for a subset of adult women, high levels of depressive symptoms tend to be recurrent and chronic (Belsher & Costello, 1988; Keller, 2003; Kennedy, Abbott, & Paykel, 2003; Monroe & Harkness, 2005). When different types of observed aversive child behaviors were examined at 18 months within a multivariate framework, child noncompliance was the most robust predictor of maternal depression trajectory group; higher levels of child noncompliance were consistently associated with more persistent and higher levels of maternal depressive symptoms. Finally, examining the role of maternal depression in predicting youth outcomes in adolescence, we found that both youth and teacher reports of antisocial behavior were more prevalent for boys whose mothers were in the moderate high trajectory group, with no such difference found for internalizing problems.
These results are consistent with transactional perspectives of developmental psychopathology that have emphasized the dynamic interplay between child and parenting characteristics, and subsequent increased risk for child maladjustment (Bell, 1968; Patterson, 1982; Sameroff & Chandler, 1975). Accordingly, disruptive child behavior in the toddler period was associated with increased risk for persistence of moderate to high levels of maternal depressive symptoms, which in turn, was associated with increased risk of boys’ and teacher reports of adolescent antisocial behavior. Regarding child effects on maternal depressive symptoms, although we do not wish to advocate that early forms of disruptive child behavior are a primary cause of maternal depression, the findings do suggest that aversive child behaviors might merit consideration as one of a constellation of intrapersonal (e.g., rumination) and interpersonal (e.g., social support) factors previously found to affect the course of depression (e.g., Bebbington, 1996; Nolen-Hoeksema, 1991). Of course, without reports of maternal depression during their child's infancy or the prenatal period, it also remains unclear how early maternal depressive symptoms might have been associated with irritability, noncompliance, or aggression at 18 months. As there is no correct “starting point” in capturing the genesis of reciprocal effects between mothers and their children, this study should be considered only a representative “slice” of a transactional process. Nonetheless, as previous literature has placed little emphasis on how child factors might have an impact on the course of maternal depression after the first 12 months of life (Forbes et al., 2006; Gelfand, Teti, & Fox, 1992; Murray, Stanley, et al., 1996), the findings suggest child disruptive behavior might be an informative risk factor to assess among mothers showing high levels of depressive symptoms. It is somewhat surprising that child effects are not considered more heavily in assessing risk of maternal depression for families with toddler-age children based on the high levels of oppositional and defiant behaviors exhibited during the “terrible twos” (Shaw & Bell, 1993).
Noncompliance as a child risk factor
We found noncompliance to be the most consistent predictor of maternal trajectory group status, with child aggression and infant irritability showing few or no significant effects when examined within a multivariate framework. In studies of preschool and school-aged hyperactive children, many of whom exhibit high rates of noncompliance, noncompliant and oppositional behaviors in children have been found to create substantial distress for parents (Barkley, Karlsson, & Pollard, 1985; Fischer, 1990; McKee, Harvey, Danforth, Ulaszek, & Friedman, 2004). In addition, in interactions with hyperactive and noncompliant children, parents display more disapproval, are more negative and reprimanding, use more physical punishment, and are less responsive (Danforth, Barkley, & Stokes, 1991; Fischer, 1990; Johnston, 1996; Johnston & Mash, 2001; Woodward, Taylor, & Dowdney, 1998).
It is somewhat surprising that aggression and infant irritability were not as strongly associated with maternal depression trajectory group status as noncompliance. However, noncompliance occurs with greater frequency than aggression and severe bouts of irritability during the toddler period, as reflected by the greater frequencies of these behaviors within our structured laboratory assessments. Thus, we suspect that oppositional and defiant child behaviors are likely to have a greater cumulative effect on parental mood than less frequent incidences of physical aggression or less intense bouts of irritability during the second year. The timing of our assessment might have also affected the magnitude of effect for irritability, as previous research has shown irritability to be a correlate of elevated maternal depressive symptoms during the first year of life before children begin displaying increased levels of aggressive and noncompliant behavior (Gelfand et al., 1992; Murray, Stanley, et al., 1996).
Outcome analysis
Consistent with the extant literature, we found that higher levels of maternal depressive symptoms were significantly associated with externalizing and antisocial youth outcomes at ages 11−13 (Munson et al., 2001; Owens & Shaw, 2003; Zahn-Waxler et al., 1990). Variance attributed to maternal depression trajectory group in relation to later externalizing behaviors remained significant after accounting for early child noncompliance. In contrast to previous research, we did not find a relationship between maternal depressive symptoms and youth internalizing behaviors. This may, in part, be due to the use of teacher report for internalizing symptoms. Other studies have found that teacher reports of child internalizing (but not externalizing) behaviors tend to have lower levels of cross-informant agreement when compared to self- and parent report, especially in early adolescence (Glaser, Kronsnoble, & Forkner, 1997; Stanger & Lewis, 1993). This discrepancy also may reflect true variation in children's behaviors across settings and/or limited opportunities for teachers to observe internalizing symptoms compared to externalizing symptoms, which are more observable (Stanger & Lewis, 1993).
Although sons of mothers with high chronic trajectories of depressive symptoms showed somewhat higher levels of youth- and teacher-reported antisocial behavior in early adolescence, it was only the sons of mothers in the moderate high group who consistently demonstrated significantly higher levels of antisocial outcomes when compared to boys whose mothers had low and moderate rates of depressive symptoms. Although somewhat paradoxical, this finding is consistent with a model posited by Rutter (1990), who has suggested that children with chronically depressed parents may be less impaired than those with chronic but more moderate symptomatology. Accordingly, Rutter has suggested that offspring of mothers who are chronically depressed are better able to understand their parents as “ill” and as a result, may learn to rely more heavily on others and themselves to develop adaptive coping skills and better social functioning (Rutter, 1981, 1990). Furthermore, other people in the child's life (friends, extended family, teachers, relatives) may be more likely to offer support to children whose mothers are chronically depressed, thus serving a protective role. In contrast, when parents show a less severe, albeit a persistent and moderate course of symptoms, children and others in their lives may continue to expect mothers to be the primary source of support and model for developing emotion regulation skills. Rutter's theory provides a possible explanation for our findings; however, to our knowledge, the current findings and the Hammen and Brennan (2003) study are the first empirical demonstrations of this phenomenon. An alternate explanation is that the mothers in the high chronic depression group were less involved in parenting their sons, resulting in lower levels of conflict and other negative parent–child interactions that have been found to contribute to externalizing outcomes.
Limitations
There are a few significant methodological limitations to the study. First, participants were primarily low-income European and African American boys living in an urban setting. There is research to support there may be gender differences in how children are affected by maternal depression. For example, Leve et al. (2005) found that the association between maternal depressive symptoms and later outcomes vary by gender, with elevated maternal depressive symptoms uniquely predicting increases in internalizing symptoms for girls and increases in boy's externalizing symptoms only when impulsivity was low. This may help explain our findings as to why maternal depression was significantly associated with externalizing but not internalizing symptoms for this all-male sample. Similarly, it is not clear if these results would have been replicated for children living in rural or suburban contexts. Thus, we recommend that future work in this area be conducted on boys and girls from diverse socioeconomic strata and ethnic backgrounds to replicate or disconfirm our results.
In the current study, we cannot rule out the role of possible “third variables” at 18 months or during the age period from ages 1.5 to 10 when maternal depressive symptoms were measured. Incorporating measurement of other child (e.g., inhibitory control), parent (e.g., caregiving quality), or contextual (e.g., neighborhood quality) factors might provide additional insight into the underlying mechanisms by which reciprocal and transactional associations emerge. Although the primary goal of this paper was to examine early child factors on patterns of maternal depression and subsequent associations with adolescent outcomes, a more intensive examination of transactional processes underlying ongoing associations between child behavior and maternal depressive symptoms during the preschool and school-age periods is clearly warranted.
Clinical implications
The results of this study are consistent with the robust finding in existing literature that higher levels of maternal depressive symptoms are associated with poor outcomes in children. This finding coupled with our finding that maternal depressive symptoms were relatively stable over time and related to serious antisocial behavior in early adolescence suggest that identification and early preventive interventions are indicated (Olds, 2002; Shaw, Dishion, Supplee, Gardner, & Arnds, 2006). In addition, the finding that child noncompliance was associated with higher and more persistent trajectories of maternal depressive symptoms suggests that the behavior of children and parents and the quality of their interaction should be a focus of interventions for children and mothers with young children. Finally, if future studies continue to find that children of mothers with chronic depression are less impaired than children whose mothers are moderately depressed (but may not reach clinical criteria), we should try to identify factors in these children's lives (e.g., external support systems, internal coping skills) that have allowed them to achieve normative levels of externalizing and internalizing problems. This information could be a powerful tool for clinicians working with children of depressed mothers.
In sum, these findings provide novel information about child factors associated with trajectories of maternal depression, and suggest that such trajectories in turn, are quite predictive of boys’ later adolescent antisocial behavior. This study has several methodological strengths. The trajectory modeling analysis used in this research allowed us to make a distinction between the two groups of mothers showing the highest levels of depressive symptoms. If these mothers had been grouped together, we would have overlooked the differences found in the outcomes between sons of mothers with moderate high and high chronic depressive symptoms. Another methodological strength of this study is that neither the associations between early child behavior and maternal depression nor between maternal depression and later child behavior can be accounted for by shared informant bias. The child's initial behavior was assessed using observational data, maternal reports were used to evaluate depressive symptoms, and youth and teacher reports were used to evaluate externalizing and internalizing problems. Finally, this study used data collected over an 11.5-year span from an at-risk sample with a relatively high retention rate. This provided a unique opportunity to examine a transactional process in a sample of mothers who generally showed above average rates of depressive symptoms and boys who exhibited elevated rates of disruptive behaviors as toddlers and adolescents.
Acknowledgments
The research reported in this paper was supported by National Institute of Mental Health Grants MH 46925, MH 50907, and MH 01666 (to D.S.S.). We are grateful to the staff of the Pitt Mother & Child Project for their years of service and to our study families for making the research possible. We also thank Dr. Bob Jones for his helpful comments and assistance on this manuscript.
References
- Achenbach TM. Manual for the Child Behavior Checklist/4−18 and 1991 profile. University of Vermont, Department of Psychiatry; Burlington, VT: 1991. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA school-age forms and profiles. University of Vermont, Research Center for Children, Youth, & Families; Burlington, VT: 2001. [Google Scholar]
- Ainsworth MS, Wittig BA. Attachment and exploratory behavior of one-year olds in a strange situation. In: Foss BM, editor. Determinants of infant behavior. Vol. 4. Methuen; London: 1969. pp. 111–136. [Google Scholar]
- Alpern L, Lyons-Ruth K. Preschool children at social risk: Chronicity and timing of maternal depressive symptoms and child behavior problems at school and at home. Development and Psychopathology. 1993;5:371–387. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 2000. text. rev. [Google Scholar]
- Barkley RA, Karlsson J, Pollard S. Effects of age on the mother–child interactions of ADD-H and normal boys. Journal of Abnormal Child Psychology. 1985;13:631–637. doi: 10.1007/BF00923146. [DOI] [PubMed] [Google Scholar]
- Beardslee WR. The need for the study of adaptation in the children of parents with affective disorders. In: Rutter M, Izard CE, Read PB, editors. Depression in young people. Guilford Press; New York: 1986. pp. 189–204. [Google Scholar]
- Bebbington P. The origins of sex differences in depressive disorder: Bridging the gap. International Review of Psychiatry. 1996;8:295–332. [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Bell RQ. A reinterpretation of the direction of effects in studies of socialization. Psychological Review. 1968;75:81–95. doi: 10.1037/h0025583. [DOI] [PubMed] [Google Scholar]
- Belsher G, Costello CG. Relapse after recovery from unipolar depression: A critical review. Psychological Bulletin. 1988;104:84–96. doi: 10.1037/0033-2909.104.1.84. [DOI] [PubMed] [Google Scholar]
- Boyle MHP, Pickles AR. Influence of maternal depressive symptoms on ratings of childhood behavior. Journal of Abnormal Child Psychology. 1997;25:399–412. doi: 10.1023/a:1025737124888. [DOI] [PubMed] [Google Scholar]
- Brennan P, Hammen C, Anderson M, Bor W, Najman J, Williams GM. Chronicity, severity, and timing of maternal depressive symptoms: Relationships with child outcomes at age 5. Developmental Psychology. 2000;36:759–766. doi: 10.1037//0012-1649.36.6.759. [DOI] [PubMed] [Google Scholar]
- Brown GW, Harris T. Social origins of depression. Free Press; New York: 1978. [DOI] [PubMed] [Google Scholar]
- Brown RT, Borden KA, Clingerman SR, Jenkins P. Depression in attention-deficit-disordered and normal children and their parents. Child Psychiatry and Human Development. 1988;18:119–132. doi: 10.1007/BF00709726. [DOI] [PubMed] [Google Scholar]
- Campbell SB, Brownell CA, Hungerford A, Spieker S, Mohan R, Blessing JS. The course of maternal depressive symptoms and maternal sensitivity as predictors of attachment security at 36 months. Development and Psychopathology. 2004;16:231–252. doi: 10.1017/s0954579404044499. [DOI] [PubMed] [Google Scholar]
- Civic D, Holt VL. Maternal depressive symptoms and child behavior problems in a nationally representative normal birthweight sample. Maternal and Child Health Journal. 2000;4:215–221. doi: 10.1023/a:1026667720478. [DOI] [PubMed] [Google Scholar]
- Cohn JF, Matias R, Tronick EZ, Connell D, Lyons-Ruth D. Face-to-face interactions of depressed mothers and their infants. New Directions for Child and Adolescent Development. 1986;34:31–45. doi: 10.1002/cd.23219863405. [DOI] [PubMed] [Google Scholar]
- Cogill S, Caplan H, Alexandra H, Robson K, Kumar R. Impact of postnatal depression on cognitive development in young children. British Medical Journal. 1986;292:1165–1167. doi: 10.1136/bmj.292.6529.1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyne J, Kahn J, Gotlib I. Depression. In: Jacob T, editor. Family interaction and psychopathology: Theories, methods, and findings. Plenum Press; New York: 1987. pp. 509–533. [Google Scholar]
- Crockenberg SB. Infant irritability, mother responsiveness, and social influences on the security of mother-infant attachment. Child Development. 1981;52:857–865. [PubMed] [Google Scholar]
- Cummings EM, Davies PT. Maternal depression and child development. Journal of Child Psychology and Psychiatry. 1994;35:73–112. doi: 10.1111/j.1469-7610.1994.tb01133.x. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Keller PS, Davies PT. Towards a family process model of maternal and paternal depressive symptoms: Exploring multiple relations with child and family functioning. Journal of Child Psychology and Psychiatry. 2005;46:479–489. doi: 10.1111/j.1469-7610.2004.00368.x. [DOI] [PubMed] [Google Scholar]
- Cutrona DE, Troutman BR. Social support, infant temperament, and parenting self-efficacy: A mediational model of postpartum depression. Child Development. 1986;57:1507–1518. [PubMed] [Google Scholar]
- Cyranowski JM, Frank E, Young E, Shear K. Adolescent onset of the gender difference in lifetime rates of major depression: A theoretical model. Archives of General Psychiatry. 2000;57:21–27. doi: 10.1001/archpsyc.57.1.21. [DOI] [PubMed] [Google Scholar]
- Danforth JS, Barkley RA, Stokes TF. Observations of parent–child interactions with hyperactive children: Research and clinical implications. Clinical Psychology Review. 1991;11:703–727. [Google Scholar]
- Downey G, Coyne JC. Children of depressed parents: An integrative review. Psychological Bulletin. 1990;108:50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- D'Unger A, Land K, McCall P, Nagin D. How many latent classes of delinquent/criminal careers? Results from mixed Poisson regression analyses of the London, Philadelphia, and Racine cohort studies. American Journal of Sociology. 1998;103:1593–1630. [Google Scholar]
- Elgar FJ, McGrath PJ, Waschbusch DA, Stewart SH, Curtis LJ. Mutual influences on maternal depression and child adjustment problems. Clinical Psychology Review. 2004;24:441–459. doi: 10.1016/j.cpr.2004.02.002. [DOI] [PubMed] [Google Scholar]
- Elliot DS, Huizinga D, Ageton SS. Explaining delinquency and drug use. Sage; Thousand Oaks, CA: 1985. [Google Scholar]
- Fagot BI, Kavanagh K. Parenting during the second year: Effects of children's age, sex, and attachment classification. Child Development. 1993;64:258–271. doi: 10.1111/j.1467-8624.1993.tb02908.x. [DOI] [PubMed] [Google Scholar]
- Farmer A, McGuffin P, Williams J. Measuring psychopathology. Oxford University Press; Oxford: 2002. [Google Scholar]
- Fergusson DM, Lynskey MT, Horwood LJ. The effect of maternal depression on maternal ratings of child behavior. Journal of Abnormal Child Psychology. 1993;21:245–269. doi: 10.1007/BF00917534. [DOI] [PubMed] [Google Scholar]
- Field T, Healy B, Goldstein S, Perry S, Bendell D, Shanberg S, et al. Infants of depressed mothers show “depressed” behaviour even with non-depressed adults. Child Development. 1988;59:1569–1579. doi: 10.1111/j.1467-8624.1988.tb03684.x. [DOI] [PubMed] [Google Scholar]
- Fischer M. Parenting stress and the child with attention deficit hyperactivity disorder. Journal of Clinical Child Psychology. 1990;19:337–346. [Google Scholar]
- Forbes EE, Shaw DS, Fox NA, Cohn JF, Silk JS, Kovacs M. Maternal depression, child frontal asymmetry, and child affective behavior as factors in child behavior problems. Journal of Child Psychology and Psychiatry. 2006;47:79–87. doi: 10.1111/j.1469-7610.2005.01442.x. [DOI] [PubMed] [Google Scholar]
- Gelfand DM, Teti DM. The effects of maternal depression on children. Clinical Psychology Review. 1990;10:320–354. [Google Scholar]
- Gelfand DM, Teti DM, Fox CR. Sources of parenting stress for depressed and nondepressed mothers of infants. Journal of Clinical Child Psychology. 1992;21:262–272. [Google Scholar]
- Ghodsian M, Zajicek E, Wolkind S. A longitudinal study of maternal depression and child behaviour problems. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1984;25:91–109. doi: 10.1111/j.1469-7610.1984.tb01721.x. [DOI] [PubMed] [Google Scholar]
- Glaser BA, Kronsnoble KM, Forkner CBW. Parents and teachers as raters of children's problem behaviors. Child and Family Behavior Therapy. 1997;19:1–13. [Google Scholar]
- Goodman SJ, Gotlib IH. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review. 1999;106:458–490. doi: 10.1037/0033-295x.106.3.458. [DOI] [PubMed] [Google Scholar]
- Hammen C, Brennan PA. Severity, chronicity, and timing of maternal depression and risk for adolescent offspring diagnoses in a community sample. Archives of General Psychiatry. 2003;60:253–258. doi: 10.1001/archpsyc.60.3.253. [DOI] [PubMed] [Google Scholar]
- Hay DF, Pawlby S, Angold A, Harold GT, Sharp D. Pathways to violence in the children of mothers who were depressed postpartum. Developmental Psychology. 2003;39:1083–1094. doi: 10.1037/0012-1649.39.6.1083. [DOI] [PubMed] [Google Scholar]
- Johnston C. Parent characteristics and parent–child interactions in families of nonproblem children and ADHD children with higher and lower levels of oppositional–defiant behavior. Journal of Abnormal Child Psychology. 1996;24:85–104. doi: 10.1007/BF01448375. [DOI] [PubMed] [Google Scholar]
- Johnston C, Mash EJ. Families of children with attention-deficit/hyperactivity disorder: Review and recommendations for future research. Clinical Child and Family Psychology Review. 2001;4:183–207. doi: 10.1023/a:1017592030434. [DOI] [PubMed] [Google Scholar]
- Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociological Methods and Research. 2007;35:542–571. [Google Scholar]
- Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociological Methods and Research. 2001;29:374–393. [Google Scholar]
- Kass RE, Raftery AE. Bayes factor. Journal of the American Statistical Association. 1995;90:773–795. [Google Scholar]
- Keenan K, Shaw D. The development of aggression in toddlers: A study of low-income families. Journal of Abnormal Child Psychology. 1994;22:53–77. doi: 10.1007/BF02169256. [DOI] [PubMed] [Google Scholar]
- Keller MB. Past, present, and future directions for defining optimal treatment outcome in depression: Remission and beyond. Journal of the American Medical Association. 2003;289:3152–3160. doi: 10.1001/jama.289.23.3152. [DOI] [PubMed] [Google Scholar]
- Keller MB, Beardslee WR, Dorer DJ, Lavori PW, Samuelson H, Kerman GR. Impact of severity and chronicity of parental affective illness on adaptive functioning and psychopathology in children. Archives of General Psychiatry. 1986;43:930–937. doi: 10.1001/archpsyc.1986.01800100020004. [DOI] [PubMed] [Google Scholar]
- Kennedy N, Abbott R, Paykel ES. Remission and recurrence of depression in the maintenance era: Long-term outcome in a Cambridge cohort. Psychological Medicine. 2003;33:827–838. doi: 10.1017/s003329170300744x. [DOI] [PubMed] [Google Scholar]
- Kringlen E, Torgersen S, Cramer V. A Norwegian psychiatric epidemiological study. American Journal of Psychiatry. 2001;158:1091–1098. doi: 10.1176/appi.ajp.158.7.1091. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Schmutte PS, Caspi A, Moffitt TE, Campbell K, Silva PA. Personality traits are linked to crime among men and women: Evidence from a birth cohort. Journal of Abnormal Psychology. 1994;103:328–338. doi: 10.1037//0021-843x.103.2.328. [DOI] [PubMed] [Google Scholar]
- LaRoche C. Children of parents with major affective disorders. The Psychiatric Clinics of North America. 1989;12:919–932. [PubMed] [Google Scholar]
- Leve LD, Kim HK, Pears KC. Childhood temperament and family environment as predictors of internalizing and externalizing trajectories from ages 5 to 17. Journal of Abnormal Child Psychology. 2005;33:505–520. doi: 10.1007/s10802-005-6734-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Hoberman HM, Rosenbaum M. A prospective study of risk factors for unipolar depression. Journal of Abnormal Psychology. 1988;97:251–264. doi: 10.1037//0021-843x.97.3.251. [DOI] [PubMed] [Google Scholar]
- Lorant V, Deliège D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: A meta-analysis. American Journal of Epidemoiology. 2003;157:98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Luoma I, Tamminen T, Kaukonen P, Laippala P, Puura K, Salmelin R, et al. Longitudinal study of maternal depressive symptoms and child well-being. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:1367–1374. doi: 10.1097/00004583-200112000-00006. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Zoll D, Connell D, Grunebaum HU. The depressed mother and her one-year-old infant: Environment, interaction, attachment and infant development. New Directions for Child and Adolescent Development. 1986;34:61–82. doi: 10.1002/cd.23219863407. [DOI] [PubMed] [Google Scholar]
- Marchand JF, Hock E, Widaman K. Mutual relations between mothers’ depressive symptoms and hostile-controlling behavior and young children's externalizing and internalizing behavior problems. Parenting: Science and Practice. 2002;2:335–353. [Google Scholar]
- Martin J. A longitudinal study of the consequences of early mother–infant interaction: A microanalytic approach. Monographs of the Society for Research in Child Development. 1981;46(3):59. [Google Scholar]
- Matas L, Arend RA, Sroufe LA. Continuity of adaptation in the second year: The relationship between quality of attachment and later competence. Child Development. 1978;49:547–556. [Google Scholar]
- McKee TE, Harvey E, Danforth JS, Ulaszek WR, Friedman JL. The relation between parental coping styles and parent–child interactions before and after treatment for children with ADHA and oppositional behavior. Journal of Clinical Child and Adolescent Psychology. 2004;33:158–168. doi: 10.1207/S15374424JCCP3301_15. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Harkness KL. Life stress, the “kindling” hypothesis, and the recurrence of depression: Considerations from a life stress perspective. Psychological Review. 2005;112:417–445. doi: 10.1037/0033-295X.112.2.417. [DOI] [PubMed] [Google Scholar]
- Munson JA, McMahon RJ, Spieker SJ. Structure and variability in the developmental trajectory of children's externalizing problems: Impact of infant attachment, maternal depressive sypmtomatology, and child sex. Development and Psychopathology. 2001;13:277–296. doi: 10.1017/s095457940100205x. [DOI] [PubMed] [Google Scholar]
- Murray L. The impact of postnatal depression on infant development. Journal of Child Psychology and Psychiatry. 1992;33:543–561. doi: 10.1111/j.1469-7610.1992.tb00890.x. [DOI] [PubMed] [Google Scholar]
- Murray L, Fiori-Cowley A, Hooper R, Cooper PJ. The impact of postnatal depression and associated adversity on early mother–infant interactions and later infant outcome. Child Development. 1996;67:2512–2516. [PubMed] [Google Scholar]
- Murray L, Stanley C, Hooper R, King F, Fiori-Cowley A. The role of infant factors in postnatal depression and mother–infant interactions. Developmental Medicine and Child Neurology. 1996;38:109–119. doi: 10.1111/j.1469-8749.1996.tb12082.x. [DOI] [PubMed] [Google Scholar]
- Nagin DS. Analyzing developmental trajectories: A semiparametric group-based approach. Psychological Methods. 1999;4:139–157. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- Nagin DS. Group-based modeling of development. Harvard University Press; Cambridge, MA: 2005. [Google Scholar]
- Nagin DS, Tremblay RE. Trajectories of boys’ physical aggression, opposition, and hyperactivity on the path to physically violent and nonviolent juvenile delinquency. Child Development. 1999;70:1181–1196. doi: 10.1111/1467-8624.00086. [DOI] [PubMed] [Google Scholar]
- Nelson DR, Hammen C, Brennan PA, Ullman JB. The impact of maternal depression on adolescent adjustment: The role of expressed emotion. Journal of Counseling and Clinical Psychology. 2003;71:935–944. doi: 10.1037/0022-006X.71.5.935. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Sex differences in unipolar depression: Evidence and theory. Psychological Bulletin. 1987;101:259–282. [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Sex differences in depression. Stanford University Press; Stanford, CA: 1990. [Google Scholar]
- Nolen-Hoeksema S. Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology. 1991;100:569–582. doi: 10.1037//0021-843x.100.4.569. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Keita GP. Women and depression: Introduction. Psychology of Women Quarterly. 2003;27:89–90. [Google Scholar]
- Olds D. Prenatal and infancy home visiting by nurses: From randomized trials to community replication. Prevention Science. 2002;3:153–172. doi: 10.1023/a:1019990432161. [DOI] [PubMed] [Google Scholar]
- Owens EB, Shaw DS. Predicting growth curves of externalizing behavior across the preschool years. Journal of Abnormal Child Psychology. 2003;31:575–590. doi: 10.1023/a:1026254005632. [DOI] [PubMed] [Google Scholar]
- Owens E, Shaw D, Vondra J. Relations between infant irritability and maternal responsiveness in low-income families. Infant Behavior & Development. 1998;21:761–778. [Google Scholar]
- Patterson G. Family coercive process. Castalia Press; Eugene, OR: 1982. [Google Scholar]
- Pelham WE, Lang AR, Atkeson B, Murphy DA, Gnagy EM, Greiner AR, et al. Effects of deviant child behavior on parental distress and alcohol consumption in laboratory interactions. Journal of Abnormal Child Psychology. 1997;25:413–424. doi: 10.1023/a:1025789108958. [DOI] [PubMed] [Google Scholar]
- Renken B, Egeland B, Marvinney D, Mangelsdorf S, Sroufe A. Early childhood antecedents of aggression and passive-withdrawal in early elementary school. Journal of Personality. 1989;57:257–281. doi: 10.1111/j.1467-6494.1989.tb00483.x. [DOI] [PubMed] [Google Scholar]
- Ruble D, Greulich F, Pomerantz M, Gochberg B. The role of gender- related processes in the development of sex differences in self-evaluation and depression. Journal of Affective Disorders. 1993;29:97–128. doi: 10.1016/0165-0327(93)90027-h. [DOI] [PubMed] [Google Scholar]
- Rutter M. Stress, coping and development: Some issues and some questions. Journal of Child Psychology and Psychiatry. 1981;22:323–256. doi: 10.1111/j.1469-7610.1981.tb00560.x. [DOI] [PubMed] [Google Scholar]
- Rutter M. Commentary: Some focus and process considerations regarding effects of parental depression on children. Developmental Psychology. 1990;26:60–67. [Google Scholar]
- Sameroff AJ, Chandler M. Reproductive risk and the continuum of caretaking casualty. In: Horowitz FD, Hetherington EM, Scarr-Salapatek S, Siegel G, editors. Review of child development research. Vol. 4. University of Chicago Press; Chicago: 1975. [Google Scholar]
- Sameroff AJ, MacKenzie MJ. Research strategies for capturing transactional models of development: The limits of the possible. Development and Psychopathology. 2003;15:613–640. doi: 10.1017/s0954579403000312. [DOI] [PubMed] [Google Scholar]
- Sharp D, Hay D, Pawlby S, Schmucher G, Allen H, Kumar R. The impact of postnatal depression on boys intellectual development. Journal of Child Psychology and Psychiatry. 1995;36:1315–1337. doi: 10.1111/j.1469-7610.1995.tb01666.x. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Bell RQ. Developmental theories of parental contributors to antisocial behavior. Journal of Abnormal Child Psychology. 1993;21:493–518. doi: 10.1007/BF00916316. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Bell RQ, Gilliom M. A truly early starter model of antisocial behavior revisited. Clinical Child and Family Psychology Review. 2000;3:155–172. doi: 10.1023/a:1009599208790. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Dishion TJ, Supplee L, Gardner F, Arnds K. Randomized trial of a family-centered approach to the prevention of early conduct problems: 2-year effects of the family check-up in early childhood. Journal of Consulting and Clinical Psychology. 2006;74:1–9. doi: 10.1037/0022-006X.74.1.1. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Keenan K, Vondra JI. The developmental precursors of antisocial behavior: Ages 1−3. Developmental Psychology. 1994;30:355–364. [Google Scholar]
- Shaw DS, Sherrill J, Huffman D, Schonberg M, Lukon J, Obrosky D, et al. Responsivity to off-spring's expression of emotion among childhood-onset depressed mothers. Journal of Clinical Child and Adolescent Psychology. 2006;35:490–503. doi: 10.1207/s15374424jccp3504_1. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Winslow EB, Owens EB, Vondra JI, Cohn JF, Bell RQ. The development of early externalizing problems among children from low-income families: A transformational perspective. Journal of Abnormal Child Psychology. 1998;26:95–107. doi: 10.1023/a:1022665704584. [DOI] [PubMed] [Google Scholar]
- Sinclair DA, Murray L. Effects of postnatal depression on children's adjustment in school. British Journal of Psychiatry. 1998;172:58–63. doi: 10.1192/bjp.172.1.58. [DOI] [PubMed] [Google Scholar]
- Smith PB, Pederson DR. Maternal sensitivity and patterns of infant–mother attachment. Child Development. 1988;59:1097–1101. doi: 10.1111/j.1467-8624.1988.tb03262.x. [DOI] [PubMed] [Google Scholar]
- Stanger C, Lewis M. Agreement among parents, teachers, and children on internalizing and externalizing behavior problems. Journal of Clinical Child Psychology. 1993;22:107–115. [Google Scholar]
- Warner V, Mufson L, Weissman MM. Off-spring at high and low risk for depression and anxiety: Mechanisms of psychiatric disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34:786–797. doi: 10.1097/00004583-199506000-00020. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Klerman GL. Sex differences in the epidemiology of depression. Archives of General Psychiatry. 1977;34:98–111. doi: 10.1001/archpsyc.1977.01770130100011. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Myers JK. Affective disorders in a US urban community. Archives of General Psychiatry. 1978;35:1304–1311. doi: 10.1001/archpsyc.1978.01770350030002. [DOI] [PubMed] [Google Scholar]
- Whiffen VE, Gotlib IH. Infants of postpartum depressed mothers: Temperament and cognitive status. Journal of Abnormal Psychology. 1989;98:274–279. doi: 10.1037//0021-843x.98.3.274. [DOI] [PubMed] [Google Scholar]
- Wilkins AJ, O'Callaghan MJ, Najman JM, Bor W, Williams GM, Shuttlewood G. Early childhood factors influencing health-related quality of life in adolescents at 13 years. Journal of Paediatrics and Child Health. 2004;40:102–109. doi: 10.1111/j.1440-1754.2004.00309.x. [DOI] [PubMed] [Google Scholar]
- Woodward L, Taylor E, Dowdney L. The parenting and family functioning of children with hyperactivity. Journal of Child Psychology and Psychiatry. 39:161–169. [PubMed] [Google Scholar]
- Zahn-Waxler C, Iannotti RJ, Cummings EM, Denham S. Antecedents of problem behaviors in children of depressed mothers. Development and Psychopathology. 1990;2:271–291. [Google Scholar]


