Abstract
Vertebral fractures are the most common osteoporotic fracture. Hip and clinical fractures are less common in black women, but there is little information on vertebral fractures. We studied 7860 white and 472 black women ≥65 yr of age enrolled in the Study of Osteoporotic Fractures. Prevalent vertebral fractures were identified from lateral spine radiographs using vertebral morphometry and defined if any vertebral height ratio was >3 SD below race-specific means for each vertebral level. Information on risk factors was obtained by questionnaire or examination. Lumbar spine, total hip, and femoral neck BMD and BMC were measured by DXA. The prevalence of vertebral fractures was 10.6% in black and 19.1% in white women. In age-adjusted logistic regression models, a 1 SD decrease in femoral neck BMD was associated with 47% increased odds of fracture in black women (OR = 1.47; 95% CI, 1.12–1.94) and 80% increased odds in white women (OR = 1.80; 95% CI, 1.68–1.94; interaction p = 0.14). The overall lower odds of fracture among black women compared with white women was independent of femoral neck BMD and other risk factors (OR = 0.51; 95% CI, 0.37–0.72). However, the prevalence of vertebral fractures increased with increasing number of risk factors in both groups. The prevalence of vertebral fractures is lower in black compared with white women but increases with age, low BMD, and number of risk factors.
Key words: osteoporosis, vertebral fracture, race/ethnicity, black, white, women
INTRODUCTION
Vertebral fractures are the hallmark of osteoporosis. They are the most common osteoporotic fracture, with prevalence estimates ranging from 10–15% among women 50–59 yr of age to 50% among women ≥85 yr of age.(1–5) About 700,000 vertebral fractures occur each year in the United States. Women with vertebral fractures experience decreased survival(6–9) and are at an increased risk of future vertebral, hip, and other nonspine fractures.(10–13) Vertebral fractures are also associated with chronic back pain, limitations with common activities of daily living, and reduced quality of life.(14,15)
The lifetime risk of any fracture in black women(16–18) is about one half that for white women, but these figures are primarily based on nonvertebral fractures. Jacobsen et al.(19) compared hospital discharge rates for vertebral fractures using the Medicare tapes in white women and black women. The greatest rate of discharge at 17.1 per 10,000 person-years was found for white women compared with 3.7 per 10,000 person-years for black women. The prevalence of vertebral fractures was probably underestimated because the study was limited to clinical vertebral fractures that were identified at hospital discharge. Clinical vertebral fractures account for ∼27% and ∼23% of all fractures in white women and black women, respectively.(20) Only about one fourth to one third of vertebral fractures are clinically recognized.(21,22) To our knowledge, no study has examined morphometrically defined vertebral fractures in black versus white women.
In this study, we examined the prevalence of radiographic vertebral fractures in 472 black women and 7860 white women ≥65 yr of age enrolled in the Study of Osteoporotic Fractures (SOF). We tested the hypothesis that low BMD will be associated with an increased likelihood of having a prevalent vertebral fracture and that the magnitude of the association will be similar in black women and white women. We examined the prevalence of vertebral fractures by age and number of risk factors in both black women and white women. Finally, we tested the hypothesis that a lower prevalence of vertebral fractures among black women will be independent of BMD and other risk factors for vertebral fractures.
MATERIALS AND METHODS
Study population
We enrolled 9704 white women into the SOF from 1986 to 1988 using population-based listings in Baltimore, MD; Minneapolis, MN; Portland, OR; and the Monongahela Valley near Pittsburgh, PA. To be eligible to participate, women had to be ≥65 yr of age and ambulatory. We excluded women who reported a bilateral hip replacement. Details of the cohort study have been published.(23) In this study, we analyzed 7860 white women who had a technically adequate hip BMD measurement at the second examination (1988–1990) and vertebral morphometry from spinal radiographs (1986–1988).
Black women were originally excluded from the SOF because of their low incidence of hip fractures. At a sixth SOF examination conducted between 1996 and 1998, we enrolled 662 black women ≥65 yr of age. Of these, 472 black women returned for a clinic visit 2 yr later (1998–2000). BMD and lateral spine films were obtained at this second visit. Race was self-declared, and only women designating themselves as black were enrolled. Because the black women were recruited later in SOF, we targeted women ⩾70 yr of age.
Bone measurements
BMC and BMD of the total hip and the femoral neck were measured by DXA using Hologic QDR 1000 and 2000 scanners (Bedford, MA, USA). Lumbar spine BMD and BMC was measured in white women using QDR 1000. For black women, we estimated lumbar spine BMD from whole body scans, and the region of interest (ROI) differs from the lumber spine ROI. Details of the measurement and densitometry quality control procedures have been published elsewhere.(24,25) In brief, a random sample of scans was reviewed by technicians at a quality control center. In addition, all scans flagged by the technicians for certain problems (such as difficulty defining bone edges) were reviewed at the quality control center. To assess longitudinal performance of the scanners, an anthropometric spine phantom was scanned daily, and a hip phantom was scanned once per week at each clinic. We calculated T-scores for the femoral neck based on race-specific reference values using the National Health and Nutrition Examination Survey (NHANES III).(26) Areal BMD measurements are based on bone length and width. Because they do not include bone depth, the measurements only partially adjust for bone size. To test whether a volumetric measurement of BMD is a better predictor of fracture occurrence, we also calculated the femoral neck bone mineral apparent density (BMAD) using the formula(27) BMC per area2 (g/cm3).
Vertebral morphometry
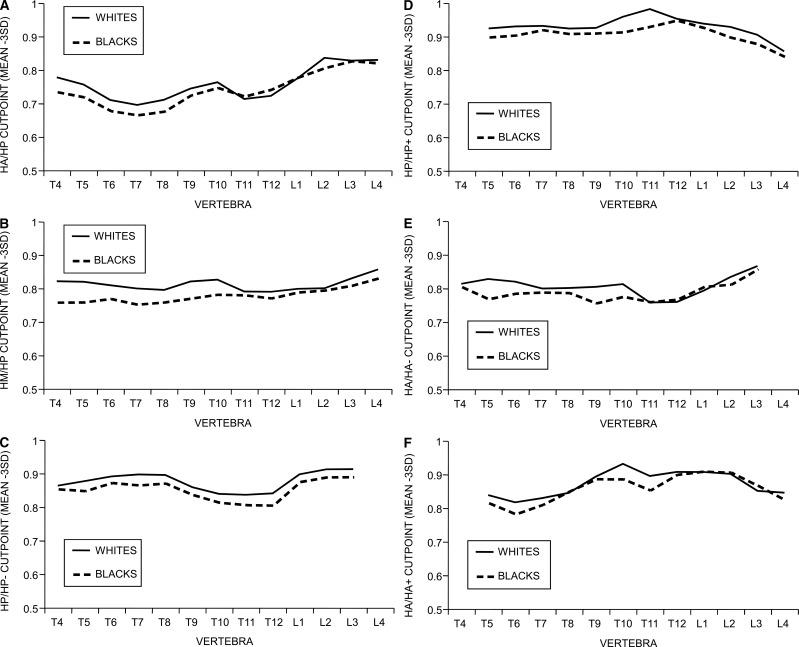
Lateral radiographs of the thoracic and lumbar spine were taken in accordance with current guidelines.(28) Quantitative vertebral morphometry was performed as previously described(29) to calculate the anterior (Ha), middle (Hm), and posterior (Hp) height for each vertebral body from T4 to L4. For white women, radiographs were first screened for probable fractures, using methods described previously(30) to reduce the number undergoing morphometric measurements. Briefly, highly trained technicians separated sets of radiographs into three groups: normal, uncertain, and probably fractured, using a binary semiquantitative grading scheme that classified women by the most abnormal vertebral level on her follow-up films. Those that were uncertain were further classified by the study radiologist as normal or probably fractured. Morphometry on paired films was performed for women classified as probably fractured. For black women, we performed morphometry an all radiographs to generate race-specific normal means and standardizations for vertebral heights and their ratios. As shown in Figs. 1A–1F, the norms for the vertebral height ratios were similar in white and black women across each vertebral level. All discrepancies between the morphometry and initial review of radiographs were adjudicated.
FIG. 1.
Mean normative vertebral height ratios for white and black women by vertebral level: (A) Ha/Hp; (B) Hm/Hp; (C) Hp/Hp−; (D) Hp/Hp+; (E) Ha/Ha−; and (F) Ha/Ha+.
Definitions of vertebral fractures
A vertebra was classified as having a prevalent fracture on the baseline radiograph if any of the following ratios were >3 SD below the trimmed normal mean(31) for that vertebral level: (Ha/Hp), (Hm/Hp), or a combination of (Hpi/Hpi±1 and Hai/Hai±1).(30) The performance of the technician triage was evaluated in a random sample of 503 women, all of whose radiographs were triaged and underwent morphometry. The sensitivity of triage for prevalent fracture, as defined in this study, was 97%.(30,32)
Other measurements
Body weight was measured using a balance beam scale and height was measured using the Harpenden stadiometer (Holtain, Crymych, UK). Body mass index (BMI) was calculated as the weight in kilograms divided by the square of height in meters. Participants were asked to stand up from a chair without using their arms five times. This was coded as able or unable; if able, time to complete the five chair stands was recorded in seconds. Grip strength (kg) was measured in both arms using a hand-held dynamometer. The average of both the right and left grip was used in the analyses. Participants also completed a questionnaire and interview that collected information on demographics, lifestyle (current smoking, alcohol use), fractures and falls history, and medical and family history. Information was obtained on whether participants walked as a form of exercise and whether they had difficulty performing any of the following instrumental activities of daily living (IADLS): walking two or three blocks, climbing up 10 steps, walking down 10 steps, preparing meals, doing heavy housework, or grocery shopping. The number of difficult activities was summed. Participants were asked to bring all prescription and over-the-counter medications to the clinic for verification of use. Dietary calcium intake was estimated using a modified Block food frequency questionnaire(33) and expressed in milligrams per day. Self-reported health status in comparison with women of the same age was reported as excellent, good, fair, poor, or very poor.
Statistical analyses
The characteristics of black women and white women who had a fracture were compared with women who did not have a fracture within race/ethnic group using t-tests for continuous variables and χ2 tests for categorical variables. We used least squared means to test whether the bone measures differed by prevalent vertebral fracture status adjusting for age. We used logistic regression models to estimate the OR of fracture and the 95% CI for each SD decrease in BMC, BMD, or BMAD. Tests for race × bone measure interactions were carried out. The SD for each site was determined from the combined cohort of women. To compare the predictive value of various measurements, we analyzed the areas under receiver operating characteristic curves using the C statistic. We initially examined the age-adjusted relationship between BMD and prevalent vertebral fracture. Because of the major effect of body weight on BMD,(34) we adjusted separately for age and body weight. Variables were included in the multivariable model if they differed by fracture status (p < 0.10) in either ethnic group. In the multivariable model, we adjusted for age, body weight, height, grip strength, uses arms to stand, walks for exercise, current calcium supplements, past and current hormone use, fracture history, health status, difficulty with ≥1 IADLS, falls in the past year, diabetes, and chronic obstructive pulmonary disease (COPD). Multivariable models were run in the combined sample with race/ethnicity coded as a dummy variable (black = 1; white = 0). We calculated the odds of having a vertebral fracture in black women compared with white women after adjusting for age, BMD, and other risk factors. If differences in BMD and risk factors contribute to ethnic differences in vertebral fractures, we would expect to see attenuation in the OR for race in analyses adjusting for these factors. Finally, we examined the prevalence of vertebral fractures by age and number of risk factors. We included the risk factors that were significant at p < 0.10 in the femoral neck multivariable BMD model. For continuous variables, women were considered to have the risk factor if they were in the lowest tertile. Risk factors included low femoral neck BMD (<0.60 g/cm2), using arms to stand, height (≤156.7 cm), health status (fair or worse), calcium supplement use, estrogen use (past or current), COPD, diabetes, and positive fracture history. χ2 tests were carried out to examine whether the prevalence of fracture differed by the number of risk factors in both white women and black women and the interaction between race and number of risk factors.
RESULTS
Overall, black women were older, had a greater body weight and BMI, were more likely to report fair, poor, or very poor health status, and were less likely to report a fracture after age 50, to walk for exercise, or to currently use calcium supplements than white women (Table 1). Use of hormone therapy did not differ by race, nor did alcohol use or smoking status. A higher proportion of black women were not able to stand from a chair without using their arms and reported difficulty with at least one IADL. Compared with white women, COPD, diabetes, and hypertension were more common among black women. A similar proportion of both races reported osteoarthritis and a history of at least one fall in the past year.
Table 1.
Characteristics of White Women and Black Women by Prevalent Vertebral Fracture Status: Mean (SD) or Percent
|
White
|
Black
|
|||
| No fracture | Fracture | No fracture | Fracture | |
| N (%) | 6360 (80.9) | 1500 (19.1) | 422 (89.4) | 50 (10.6) |
| Age (yr) | 70.9 (4.9) | 72.9 (5.6)* | 76.9 (4.8) | 78.7 (4.9)† |
| Weight (kg) | 67.7 (12.4) | 65.6 (12.0)* | 75.8 (15.6) | 68.0 (17.1)† |
| Height (cm) | 159.7 (5.9) | 158.1 (6.2)* | 157.9 (6.3) | 156.4 (5.9) |
| BMI (kg/m2) | 26.5 (4.6) | 26.2 (4.3)‡ | 30.4 (6.0) | 27.7 (6.4)† |
| Grip strength (kg) | 21.2 (4.2) | 20.4 (4.6)* | 19.7 (5.1) | 17.8 (5.3)‡ |
| Uses arms to stand (%) | 2.6 | 5.2* | 17.1 | 16.0 |
| Walk for exercise (%) | 52.8 | 50.1 | 40.5 | 36.0 |
| Alcohol (1+ drinks/last month) (%) | 29.1 | 29.0 | 28.7 | 30.0 |
| Current smoker (%) | 9.2 | 10.8 | 7.6 | 10.0 |
| Past smoker (%) | 30.3 | 28.9 | 31.7 | 40.0 |
| Dietary calcium intake (mg/d) | 718 (421) | 723 (433) | 638 (352) | 626 (430) |
| Current calcium supplement (%) | 41.3 | 50.7* | 29.0 | 29.2 |
| Current hormone use (%) | 14.5 | 13.9 | 16.1 | 11.1 |
| Past hormone use (%) | 28.9 | 25.2 | 21.2 | 26.7 |
| Health status | ||||
| Fair, poor, very poor (%) | 14.6 | 17.9† | 31.1 | 42.0 |
| Difficulty ≥ 1 IADLS | 32.3 | 37.2† | 49.3 | 56.0 |
| Any falls last 12 mo (%) | 29.1 | 31.4 | 27.1 | 38.0 |
| Fall ≥ 2 last 12 mo (%) | 10.0 | 11.3 | 9.5 | 16.0 |
| Fractures after age 50 (%) | 32.4 | 51.2* | 21.1 | 36.0‡ |
| Diabetes (%) | 6.8 | 5.5 | 16.2 | 24.0 |
| COPD (%) | 8.5 | 11.4† | 13.5 | 20.0 |
| Hypertension (%) | 37.3 | 39.3 | 64.5 | 54.0 |
| Osteoarthritis (%) | 19.6 | 19.1 | 20.0 | 30.0 |
* p < 0.0001.
† p < 0.01.
‡ p < 0.05.
Eleven percent of black women had at least one prevalent vertebral fracture compared with 19.1% of white women (Table 1). Of those with a fracture, 32% of black women compared with 40% of white women had two or more prevalent fractures. The black women who had a prevalent vertebral fracture were older and had a lower body weight, BMI, and grip strength than black women who did not have a prevalent vertebral fracture (Table 1). Compared with white women who did not have a prevalent vertebral fracture, white women who had a fracture were older, had a lower body weight and BMI, lower grip strength, were twice as likely to use their arms to stand from a chair, and were more likely to report calcium supplement use, fair/poor or very poor health status, difficulty with at least one IADL, fracture after age 50, and a history of COPD. A higher proportion of women with a vertebral fracture reported falls in the past year, but this observation was of borderline significance in whites (p = 0.07) and blacks (p = 0.10).
In both white women and black women, the mean BMD and BMC of the total hip, femoral neck, and lumbar spine and femoral neck BMAD were lower among women who had a prevalent vertebral fracture compared with women who did not have a fracture (Table 2). A higher proportion of both white (41.7%) and black women (30%) who had a fracture had a femoral neck T-score of −2.5 or less.
Table 2.
Age-Adjusted Mean BMD, BMC, or BMAD (95% CI) by Prevalent Vertebral Fracture Status in White Women and Black Women
|
White
|
Black
|
|||
| No fracture (n = 6360) | Fracture (n = 1500) | No fracture (n = 422) | Fracture (n = 50) | |
| Total hip | ||||
| BMD (g/cm2) | 0.77 (0.768, 0.774) | 0.70 (0.698, 0.711)* | 0.83 (0.82, 0.85) | 0.75 (0.71, 0.79)* |
| BMC (g) | 29.5 (29.4, 29.7) | 27.3 (27.0, 27.6)* | 29.0 (28.4, 29.5) | 26.3 (24.7, 27.9)† |
| Femoral neck | ||||
| BMD (g/cm2) | 0.66 (0.656, 0.661) | 0.61 (0.60, 0.61)* | 0.75 (0.74, 0.76) | 0.69 (0.65, 0.73)† |
| BMC (g) | 3.2 (3.19, 3.22) | 3.0 (2.9, 3.0)* | 3.9 (3.8, 3.9) | 3.6 (3.4, 3.8)‡ |
| BMAD (g/cm3) | 0.14 (0.138, 0.139) | 0.13 (0.126, 0.129)* | 0.15 (0.14, 0.15) | 0.14 (0.13, 0.15)‡ |
| Femoral neck T-score§ | ||||
| T-score (mean) | −1.71 (−1.74, −1.69) | −2.16 (−2.21, −2.11)* | −1.41 (−1.51, −1.32) | −1.81 (−2.09, −1.54)† |
| T-score > −1 | 20.6% | 9.3% | 29.6% | 18.0% |
| T-score < −1 and > −2.5 | 58.6% | 48.9% | 56.4% | 52.0% |
| T-score ≤ −2.5 | 20.8% | 41.7%* | 14.0% | 30.0%‡ |
| Lumbar spine BMD¶ | ||||
| BMD (g/cm2) | 0.87 (0.866, 0.875) | 0.80 (0.789, 0.807)* | 0.96 (0.939, 0.981) | 0.86 (0.798, 0.923)† |
| BMC (g) | 49.2 (48.86, 49.46) | 44.0 (43.32, 44.57)* | 48.2 (46.58, 49.83) | 39.2 (34.40, 44.03)* |
* p < 0.001 for no fracture vs. fracture within race.
† p < 0.01 for no fracture vs. fracture within race.
‡ p < 0.05 for no fracture vs. fracture within race.
§ Race-specific reference values used for calculation of T-scores.
¶ Lumbar spine BMD and BMC estimated from whole body scans in black women.
In white women and black women, respectively, after adjusting for age, the OR of vertebral fracture per 1 SD decrease in BMD was 1.88 (95% CI, 1.75, 2.01) and 1.85 (95% CI, 1.36, 2.52) for the total hip and 1.80 (95% CI, 1.68, 1.94) and 1.47 (95% CI, 1.12, 1.94) for the femoral neck; all increases were statistically significant (p < 0.05; Table 3). Similar associations were found for BMAD and lumbar spine BMD. The areas under receiver operating characteristic curves (AUCs) for BMD of the total hip, femoral neck, and lumbar spine were similar in white women and black women. The association between bone mass measurements and prevalent vertebral fracture did not differ by race (femoral neck BMD × race interaction, p = 0.14; BMC × race interaction, p = 0.95; BMAD × race interaction, p = 0.86). Additional adjustment for body weight and other risk factors had only a modest effect on the association between BMD and prevalent vertebral fractures in white women but resulted in greater attenuation of the OR in black women.
Table 3.
OR (95% CI) for Prevalent Vertebral Fracture for 1 SD Decrease in BMD, BMC, or BMAD: Age, Age and Body Weight, and Multivariable-Adjusted Models
|
White
|
Black
|
|||
| OR (95% CI) | AUC | OR (95% CI) | AUC | |
| Age alone* | 1.42 (1.35, 1.49) | 0.603 | 1.40 (1.07, 1.84) | 0.613 |
| Total hip BMD | ||||
| Age adjusted | 1.88 (1.75, 2.01) | 0.681 | 1.85 (1.36, 2.52) | 0.694 |
| Age and body weight | 2.08 (1.92, 2.25) | 0.689 | 1.70 (1.20, 2.41) | 0.692 |
| Multivariate† | 2.03 (1.87, 2.20) | 0.712 | 1.49 (1.00, 2.23) | 0.737 |
| Total hip BMC | ||||
| Age adjusted | 1.53 (1.43, 1.63) | 0.649 | 1.69 (1.20, 2.39) | 0.655 |
| Age and body weight | 1.69 (1.56, 1.83) | 0.655 | 1.44 (0.95, 2.18) | 0.657 |
| Multivariate† | 1.60 (1.47, 1.74) | 0.686 | 1.19 (0.75, 1.91) | 0.718 |
| Femoral neck BMD | ||||
| Age adjusted | 1.80 (1.68, 1.94) | 0.672 | 1.47 (1.12, 1.94) | 0.655 |
| Age and body weight | 1.92 (1.77, 2.08) | 0.676 | 1.32 (0.99, 1.77) | 0.659 |
| Multivariate† | 1.81 (1.67, 1.97) | 0.701 | 1.12 (0.81, 1.54) | 0.718 |
| Femoral neck BMC | ||||
| Age adjusted | 1.47 (1.38, 1.57) | 0.641 | 1.47 (1.08, 2.00) | 0.649 |
| Age and body weight | 1.49 (1.39, 1.60) | 0.642 | 1.28 (0.92, 1.78) | 0.652 |
| Multivariate† | 1.41 (1.30, 1.52) | 0.677 | 1.06 (0.73, 1.52) | 0.715 |
| Femoral neck BMAD | ||||
| Age adjusted | 1.53 (1.43, 1.65) | 0.646 | 1.50 (1.05, 2.15) | 0.658 |
| Age and body weight | 1.52 (1.41, 1.63) | 0.645 | 1.35 (0.94, 1.95) | 0.662 |
| Multivariate† | 1.49 (1.38, 1.61) | 0.682 | 1.14 (0.77, 1.69) | 0.718 |
| Lumbar spine BMD‡ | ||||
| Age adjusted | 1.78 (1.65, 1.93) | 0.660 | 1.62 (1.17, 2.24) | 0.660 |
| Age and body weight | 1.87 (1.71, 2.03) | 0.662 | 1.45 (1.03, 2.05) | 0.659 |
| Multivariate† | 1.82 (1.66, 1.99) | 0.695 | 1.23 (0.85, 1.78) | 0.708 |
| Lumbar spine BMC‡ | ||||
| Age adjusted | 1.80 (1.66, 1.96) | 0.659 | 1.74 (1.26, 2.40) | 0.672 |
| Age and body weight | 1.94 (1.77, 2.13) | 0.662 | 1.60 (1.12, 2.28) | 0.670 |
| Multivariate† | 1.86 (1.69, 2.05) | 0.692 | 1.34 (0.90, 2.00) | 0.707 |
* OR per 5-yr increase in age.
† Multivariable model includes adjustment for age, body weight, height, grip strength, uses arms to stand, walks for exercise, current calcium supplements, past and current hormone use, health status, difficulty with ≥1 IADLS, falls in past 12 mo, fracture history, diabetes, and COPD.
‡ Lumbar spine BMD and BMC estimated from whole body scans in black women.
AUC, area under receiver operating characteristic curves.
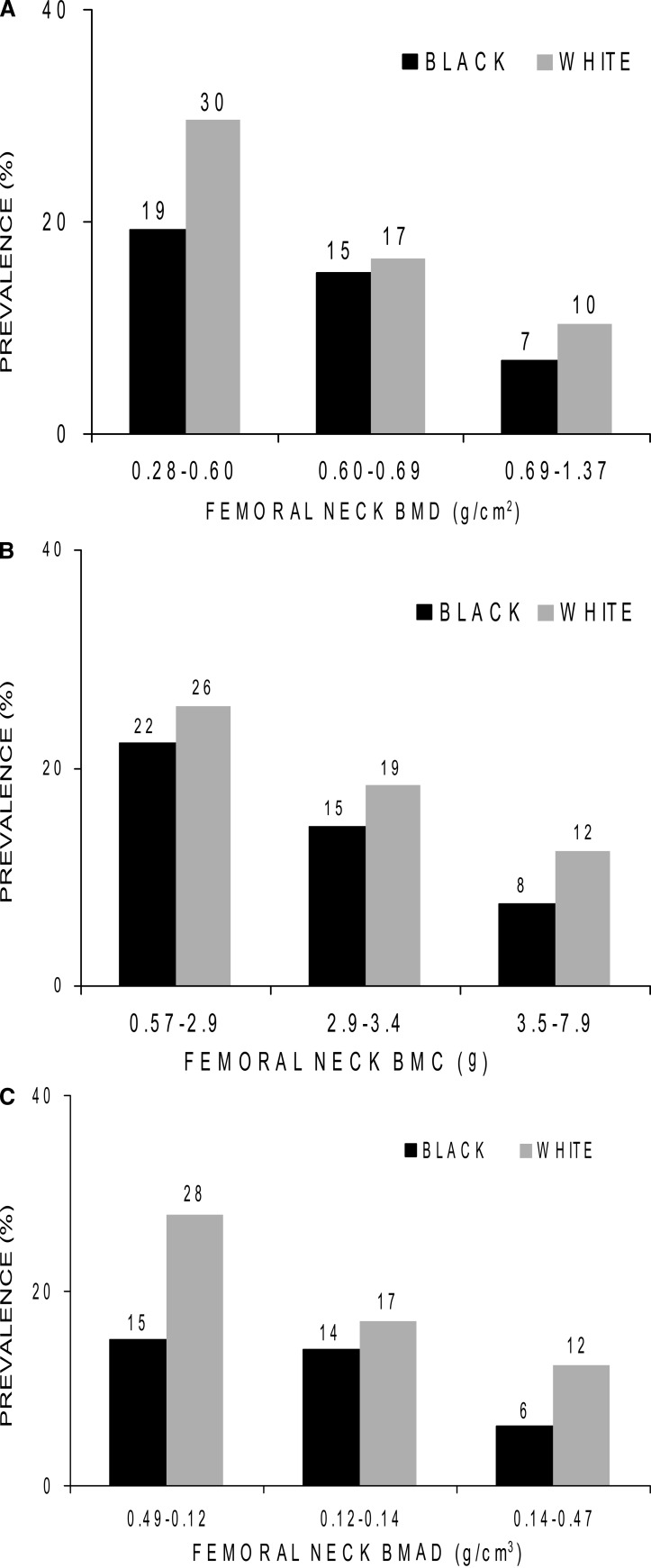
Total hip, femoral neck, and lumbar spine BMC were related to prevalent vertebral in white women but not in black women. Within each racial group, the prevalence of vertebral fractures was highest among women with the lowest tertile of femoral neck BMC, BMD, and BMAD (Fig. 2). Nevertheless, at every bone mass level, the prevalence was lower in black women.
FIG. 2.
Prevalence (%) of vertebral fractures by tertiles of femoral neck BMD, BMC, and BMAD in white women and black women.
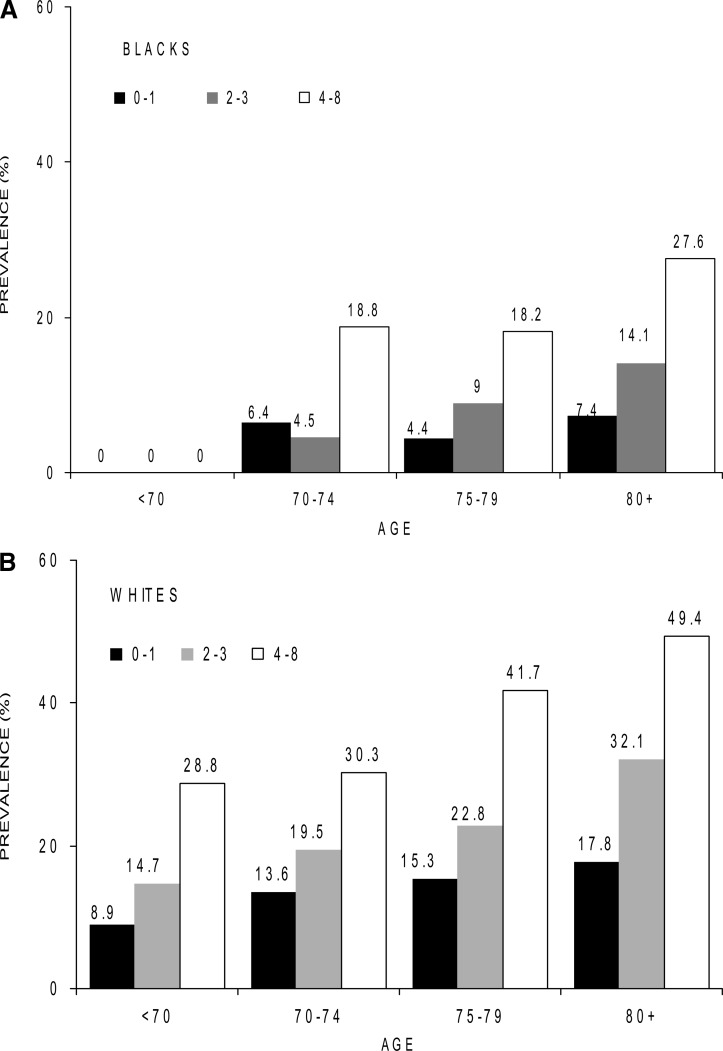
The prevalence of vertebral fracture increased with increasing age and number of risk factors in each group (Fig. 3). The prevalence of vertebral fractures was two to three times higher in women with four to eight risk factors compared with women with zero to one risk factors at every age group.
FIG. 3.
Prevalence (%) of vertebral fractures by age and the number of risk factors in white women and black women. The number of black women in each age group was as follows: <70, n = 10; 70–74, n = 146; 75–79, n = 168; and 80+, n = 120. The number of white women in each age group was as follows: <70, n = 3382; 70–74, n = 2401; 75–79, n = 1169; and 80+, n = 632. For continuous variables, the risk factor was considered present for women in the lowest tertile. Risk factors included low femoral neck BMD (<0.60 g/cm2), using arms to stand, height (≤156.7 cm), health status (fair or worse), calcium supplement use, estrogen use, COPD, diabetes, and positive fracture history.
In age-adjusted models, black women had 67% lower odds of having a vertebral fracture (Table 4). Further adjustments for femoral neck BMD and other risk factors resulted in some attenuation, but the odds of having a prevalent vertebral fracture was still ∼50% lower for black women compared with white women.
Table 4.
OR (95% CI) for Prevalent Vertebral Fracture in Black Women Compared With White Women
| Adjustments | OR (95% CI) |
| Age alone | 0.33 (0.25, 0.45) |
| Femoral neck BMD plus | |
| Age | 0.56 (0.40, 0.76) |
| Age and multivariable model | 0.51 (0.37, 0.72) |
| Femoral neck BMAD plus | |
| Age | 0.40 (0.29, 0.54) |
| Age and multivariable modela | 0.40 (0.29, 0.56) |
| Total hip BMD plus | |
| Age | 0.49 (0.36, 0.67) |
| Age and multivaribale model a | 0.45 (0.32, 0.63) |
Multivariable model = adjustment for age, body weight, height, grip strength, uses arms to stand, walks for exercise, current calcium supplements, past and current hormone use, health status, difficulty with ≥1 IADLS, fracture history, diabetes, and COPD.
DISCUSSION
The prevalence of vertebral fractures was 11% in black women compared with 19% in white women; this prevalence was 45–50% lower among black women compared with white women even after adjusting for age, BMD, and other risk factors for fracture. The lower prevalence of vertebral fractures among black women is consistent with the lower incidence of all fractures including hip fractures observed in black women.(16–18) Age-specific prevalence of vertebral fractures have been reported for European women,(35) U.S. white women,(36) Asian women in Hawaii,(37) Hiroshima,(37) Taiwan,(38) and Beijing,(39) and Latin Americans.(40) The prevalence of vertebral fractures is on average in all these groups ∼25%, >2-fold higher than we observed among black women. Despite large geographic differences in hip fracture across the world, the prevalence of vertebral fractures is actually very similar. In contrast, black women have a lower prevalence of both vertebral fractures and hip fractures.
We showed that reduced BMD of the total hip and femoral neck is associated with increased odds of having a prevalent vertebral fracture in both black women and white women. The magnitude of the association between low total hip BMD and prevalent vertebral fracture was similar in both groups. However, the association between femoral neck BMD and prevalent vertebral fractures was weaker and nonsignificant in multivariable-adjusted models in black women. The association between BMC and vertebral fractures was weaker than observed for BMD in white women and nonsignificant in black women. This may be because BMC makes no correction for bone size. These results are similar to what we observed for incident nonspine fractures.(41)
We hypothesized that if BMAD provides an accurate estimate of volumetric BMD, we may find a stronger association because BMAD would compensate for ethnic differences in bone size. However, there was no evidence that our estimate of volumetric BMD was more strongly associated with prevalent vertebral fractures than areal BMD measures of the hip. Nevertheless, we were limited to estimated volumetric BMD at the hip. We did not have volumetric measurements of the spine, and it is possible that associations with spine volumetric BMD may be stronger. We have previously shown that lumbar spine areal BMD was more strongly associated with incident vertebral fractures than hip BMD, at least in white women.(42) In this analysis, there was no evidence in either group that lumbar spine BMD was more strongly associated with vertebral fracture. We were, however, limited to estimating lumbar spine BMD in black women using whole body scans, and the region of interest is not directly comparable to the direct measure of lumbar spine BMD.
At the same BMD level, the prevalence of vertebral fracture was lower among black women. However, areal BMD measures provide little information on the material composition of bone and its structural design, two properties that determine bone strength.(43) Ethnic differences in trabecular number, thickness and connectivity, cortical thinning and porosity, periosteal apposition, and bone remodeling all likely contribute to the lower prevalence of vertebral and hip fractures in black women. Finally, the heritability of BMD is very high,(44) and it is likely that genetic factors contribute to the lower risk of vertebral fracture among black women. Greater European admixture in U.S. blacks has been associated with lower BMD.(45)
The prevalence of vertebral fractures increased with age and number of risk factors in both black women and white women. We included many risk factors for vertebral fractures but it is possible that other factors may also affect the likelihood of fracture such as sex steroid hormones,(46) inflammatory markers,(47) and vitamin D levels, although vitamin D deficiency is more common in blacks than whites.(48) Our results suggest that screening efforts should focus on older women with multiple risk factors to potentially identify women who are likely to have a prevalent vertebral fracture. Underdiagnosis of vertebral fracture is a worldwide problem.(49) Use of DXA to measure vertebral morphometry may be more cost-effective to identify women with prevalent vertebral fractures who have a high absolute risk of fracture and may be more likely to benefit from pharmacological therapy.(50) Treatment of women with asymptomatic vertebral fractures has been shown to reduce future hip and vertebral fractures(51–54) and reduce disability.(55)
Strengths of our study include our well-characterized cohort of both black and white community-dwelling women. We used standard clinical measures of BMD, state of the art vertebral morphometry, and included a number of important risk factors for fracture. There are, however, some limitations. Although we used a population-based listing for recruitment, the women were volunteers and thus may be healthier and have a lower prevalence of vertebral fracture. Women in our analytical sample were somewhat healthier than those excluded, which may also contribute to an underestimation of the prevalence of vertebral fractures. However, this healthy bias was present for both white women and black women and should not influence these comparisons. The number of black women was relatively small, especially in stratified analyses, and we had limited power to identify correlates of vertebral fractures in this group. We used a cross-sectional design, and prospective studies of risk factors for incident vertebral fractures in black women are needed. Race/ethnicity was self-declared, and we had no information on European admixture, which has been shown to range from 12% to 23% in blacks.(56) Hip BMD was measured 2 yr after the spine radiographs in the white women. Finally, we estimated lumbar spine BMD from whole body scans in the black women and directly measured BMD in the spine in white women. These measurements are not directly comparable.
In conclusion, prevalent radiographic vertebral fractures are more common among older white women compared with black women. They are associated with older age, lower BMD, and a larger number of risk factors in both black women and white women. Identification of women with multiple risk factors and appropriate treatment could reduce their fracture burden.
ACKNOWLEDGMENTS
The Study of Osteoporotic Fractures (SOF) is supported by National Institutes of Health funding. The following institutes provide support: the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) and the National Institute on Aging (NIA) under the following grant numbers: AG05407, AR35582, AG05394, AR35584, AR35583, R01 AG005407, R01 AG027576-22, 2 R01 AG005394-22A1, and 2 R01 AG027574-22A1. Additional support was provided by AR45568. The sponsor had no role in the design and conduct of the study, interpretation of the data, or in the development of the manuscript.
Footnotes
Dr Cauley has received research support from Merck, Eli Lilly, Pfizer Pharmaceuticals, and Novartis Pharmaceuticals. She has also received consulting fees from Eli Lilly and Novartis Pharmaceuticals. Dr Hochberg has received research support from the National Institutes of Health. He is a consultant for the following companies that have products related to osteoporosis and/or vertebral fractures: Amgen, GlaxoSmithKline, Merck, Novartis Pharma AG, Procter & Gamble, Roche Laboratories, and Wyeth Pharmaceuticals. Dr Nevitt receives honoraria from Eli Lilly and Wyeth for osteoarthritis-related activities. All other authors state that they have no conflicts of interest.
REFERENCES
- 1.Cooper C, O'Neill T, Silman A. The epidemiology of vertebral fractures. European Vertebral Osteoporosis Study Group. Bone. 1993;14(Suppl 1):S89–S97. doi: 10.1016/8756-3282(93)90358-h. [DOI] [PubMed] [Google Scholar]
- 2.Melton LJ., III Epidemiology of spinal osteoporosis. Spine. 1997;22(24 Suppl):2S–11S. doi: 10.1097/00007632-199712151-00002. [DOI] [PubMed] [Google Scholar]
- 3.Melton LJ, III, Kan SH, Frye MA, Wahner HW, O'Fallon WM, Riggs BL. Epidemiology of vertebral fractures in women. Am J Epidemiol. 1989;129:1000–1011. doi: 10.1093/oxfordjournals.aje.a115204. [DOI] [PubMed] [Google Scholar]
- 4.Wasnich RD. Vertebral fracture epidemiology. Bone. 1996;18(3 Suppl):179S–183S. doi: 10.1016/8756-3282(95)00499-8. [DOI] [PubMed] [Google Scholar]
- 5.Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761–1767. doi: 10.1016/S0140-6736(02)08657-9. [DOI] [PubMed] [Google Scholar]
- 6.Cauley JA, Thompson DE, Ensrud KC, Scott JC, Black D. Risk of mortality following clinical fractures. Osteoporos Int. 2000;11:556–561. doi: 10.1007/s001980070075. [DOI] [PubMed] [Google Scholar]
- 7.Kado DM, Duong T, Stone KL, Ensrud KE, Nevitt MC, Greendale GA, Cummings SR. Incident vertebral fractures and mortality in older women: A prospective study. Osteoporos Int. 2003;14:589–594. doi: 10.1007/s00198-003-1412-5. [DOI] [PubMed] [Google Scholar]
- 8.Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR. Vertebral fractures and mortality in older women: A prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med. 1999;159:1215–1220. doi: 10.1001/archinte.159.11.1215. [DOI] [PubMed] [Google Scholar]
- 9.Jalava T, Sarna S, Pylkkanen L, Mawer B, Kanis JA, Selby P, Davies M, Adams J, Francis RM, Robinson J, McCloskey E. Association between vertebral fracture and increased mortality in osteoporotic patients. J Bone Miner Res. 2003;18:1254–1260. doi: 10.1359/jbmr.2003.18.7.1254. [DOI] [PubMed] [Google Scholar]
- 10.Melton LJ, III, Atkinson EJ, Cooper C, O'Fallon WM, Riggs BL. Vertebral fractures predict subsequent fractures. Osteoporos Int. 1999;10:214–221. doi: 10.1007/s001980050218. [DOI] [PubMed] [Google Scholar]
- 11.Black DM, Arden NK, Palermo L, Pearson J, Cummings SR. Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1999;14:821–828. doi: 10.1359/jbmr.1999.14.5.821. [DOI] [PubMed] [Google Scholar]
- 12.Ross PD, Davis JW, Epstein RS, Wasnich RD. Pre-existing fractures and bone mass predict vertebral fracture incidence in women. Ann Intern Med. 1991;114:919–923. doi: 10.7326/0003-4819-114-11-919. [DOI] [PubMed] [Google Scholar]
- 13.Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, III, Berger M. Patients with prior fractures have an increased risk of future fractures: A summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15:721–739. doi: 10.1359/jbmr.2000.15.4.721. [DOI] [PubMed] [Google Scholar]
- 14.Oleksik A, Lips P, Dawson A, Minshall ME, Shen W, Cooper C, Kanis J. Health-related quality of life in postmenopausal women with low BMD with or without prevalent vertebral fractures. J Bone Miner Res. 2000;15:1384–1392. doi: 10.1359/jbmr.2000.15.7.1384. [DOI] [PubMed] [Google Scholar]
- 15.Nevitt MC, Ettinger B, Black DM, Stone K, Jamal SA, Ensrud K, Segal M, Genant HK, Cummings SR. The association of radiographically detected vertebral fractures with back pain and function: A prospective study. Ann Intern Med. 1998;128:793–800. doi: 10.7326/0003-4819-128-10-199805150-00001. [DOI] [PubMed] [Google Scholar]
- 16.Farmer ME, White LR, Brody JA, Bailey KR. Race and sex differences in hip fracture incidence. Am J Public Health. 1984;74:1374–1380. doi: 10.2105/ajph.74.12.1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baron JA, Karagas M, Barrett J, Kniffin W, Malenka D, Mayor M, Keller RB. Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology. 1996;7:612–618. doi: 10.1097/00001648-199611000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Baron JA, Barrett J, Malenka D, Fisher E, Kniffin W, Bubolz T, Tosteson T. Racial differences in fracture risk. Epidemiology. 1994;5:42–47. doi: 10.1097/00001648-199401000-00008. [DOI] [PubMed] [Google Scholar]
- 19.Jacobsen SJ, Cooper C, Gottlieb MS, Goldberg J, Yahnke DP, Melton LJ., III Hospitalization with vertebral fracture among the aged: A national population-based study, 1986-1989. Epidemiology. 1992;3:515–518. doi: 10.1097/00001648-199211000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465–475. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 21.Cooper C, Atkinson EJ, O'Fallon WM, Melton LJ., III Incidence of clinically diagnosed vertebral fractures: A population-based study in Rochester, Minnesota, 1985-1989. J Bone Miner Res. 1992;7:221–227. doi: 10.1002/jbmr.5650070214. [DOI] [PubMed] [Google Scholar]
- 22.Fink HA, Milavetz DL, Palermo L, Nevitt MC, Cauley JA, Genant HK, Black DM, Ensrud KE. What proportion of incident radiographic vertebral deformities is clinically diagnosed and vice versa. J Bone Miner Res. 2005;20:1216–1222. doi: 10.1359/JBMR.050314. [DOI] [PubMed] [Google Scholar]
- 23.Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM. Risk factors for hip fracture in white women. Study of Osteoporotic Fractures Research Group. N Engl J Med. 1995;332:767–773. doi: 10.1056/NEJM199503233321202. [DOI] [PubMed] [Google Scholar]
- 24.Ensrud KE, Palermo L, Black DM, Cauley J, Jergas M, Orwoll ES, Nevitt MC, Fox KM, Cummings SR. Hip and calcaneal bone loss increase with advancing age: Longitudinal results from the study of osteoporotic fractures. J Bone Miner Res. 1995;10:1778–1787. doi: 10.1002/jbmr.5650101122. [DOI] [PubMed] [Google Scholar]
- 25.Steiger P, Cummings SR, Black DM, Spencer NE, Genant HK. Age-related decrements in bone mineral density in women over 65. J Bone Miner Res. 1992;7:625–632. doi: 10.1002/jbmr.5650070606. [DOI] [PubMed] [Google Scholar]
- 26.Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC, Jr, Lindsay RL. Proximal femur bone mineral levels of US adults. Osteoporos Int. 1995;5:389–409. doi: 10.1007/BF01622262. [DOI] [PubMed] [Google Scholar]
- 27.Katzman DK, Bachrach LK, Carter DR, Marcus R. Clinical and anthropometric correlates of bone mineral acquisition in healthy adolescent girls. J Clin Endocrinol Metab. 1991;73:1332–1339. doi: 10.1210/jcem-73-6-1332. [DOI] [PubMed] [Google Scholar]
- 28.Kiel D. Assessing vertebral fractures. National Osteoporosis Foundation Working Group on Vertebral Fractures. J Bone Miner Res. 1995;10:518–523. doi: 10.1002/jbmr.5650100403. [DOI] [PubMed] [Google Scholar]
- 29.Nevitt MC, Cummings SR, Stone KL, Palermo L, Black DM, Bauer DC, Genant HK, Hochberg MC, Ensrud KE, Hillier TA, Cauley JA. Risk factors for a first-incident radiographic vertebral fracture in women > or = 65 years of age: The study of osteoporotic fractures. J Bone Miner Res. 2005;20:131–140. doi: 10.1359/JBMR.041003. [DOI] [PubMed] [Google Scholar]
- 30.Black DM, Palermo L, Nevitt MC, Genant HK, Epstein R, San Valentin R, Cummings SR. Comparison of methods for defining prevalent vertebral deformities: The Study of Osteoporotic Fractures. J Bone Miner Res. 1995;10:890–902. doi: 10.1002/jbmr.5650100610. [DOI] [PubMed] [Google Scholar]
- 31.Black DM, Cummings SR, Stone K, Hudes E, Palermo L, Steiger P. A new approach to defining normal vertebral dimensions. J Bone Miner Res. 1991;6:883–892. doi: 10.1002/jbmr.5650060814. [DOI] [PubMed] [Google Scholar]
- 32.Black DM, Palermo L, Nevitt MC, Genant HK, Christensen L, Cummings SR. Defining incident vertebral deformity: A prospective comparison of several approaches. The Study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1999;14:90–101. doi: 10.1359/jbmr.1999.14.1.90. [DOI] [PubMed] [Google Scholar]
- 33.Cummings SR, Block G, McHenry K, Baron RB. Evaluation of two food frequency methods of measuring dietary calcium intake. Am J Epidemiol. 1987;126:796–802. doi: 10.1093/oxfordjournals.aje.a114716. [DOI] [PubMed] [Google Scholar]
- 34.Orwoll ES, Bauer DC, Vogt TM, Fox KM. Axial bone mass in older women. Study of Osteoporotic Fractures Research Group. Ann Intern Med. 1996;124:187–196. doi: 10.7326/0003-4819-124-2-199601150-00001. [DOI] [PubMed] [Google Scholar]
- 35.O'Neill TW, Felsenberg D, Varlow J, Cooper C, Kanis JA, Silman AJ. The prevalence of vertebral deformity in european men and women: The European Vertebral Osteoporosis Study. J Bone Miner Res. 1996;11:1010–1018. doi: 10.1002/jbmr.5650110719. [DOI] [PubMed] [Google Scholar]
- 36.Davies KMSM, Heaney RP, Recker RR. Prevalence and severity of vertebral fracture: The Saunders County Bone Quality Study. Osteoporos Int. 1996;6:160–165. doi: 10.1007/BF01623941. [DOI] [PubMed] [Google Scholar]
- 37.Ross PD, Fujiwara S, Huang C, Davis JW, Epstein RS, Wasnich RD, Kodama K, Melton LJ., III Vertebral fracture prevalence in women in Hiroshima compared to Caucasians or Japanese in the US. Int J Epidemiol. 1995;24:1171–1177. doi: 10.1093/ije/24.6.1171. [DOI] [PubMed] [Google Scholar]
- 38.Tsai K, Twu S, Chieng P, Yang R, Lee T. Prevalence of vertebral fractures in chinese men and women in urban Taiwanese communities. Calcif Tissue Int. 1996;59:249–253. doi: 10.1007/s002239900118. [DOI] [PubMed] [Google Scholar]
- 39.Ling X, Cummings SR, Mingwei Q, Xihe Z, Xioashu C, Nevitt M, Stone K. Vertebral fractures in Beijing, China: The Beijing Osteoporosis Project. J Bone Miner Res. 2000;15:2019–2025. doi: 10.1359/jbmr.2000.15.10.2019. [DOI] [PubMed] [Google Scholar]
- 40.Clark P, Cons-Molina F, Ragi S, Deleze M, Haddock L, Zanchetta J, Messina D, Jaller J, Navarrete A, Salmeron J, Morales Torres J, Palermo L, Cummings S. The prevalence of vertebral fractures in Latin American women: The Latin American Vertebral Osteoporosis Study “LAVOS”. Osteoporos Int. 2006;17(Suppl 2):S130–S142. doi: 10.1007/s00198-008-0657-4. [DOI] [PubMed] [Google Scholar]
- 41.Cauley JA, Lui LY, Ensrud KE, Zmuda JM, Stone KL, Hochberg MC, Cummings SR. Bone mineral density and the risk of incident nonspinal fractures in black and white women. JAMA. 2005;293:2102–2108. doi: 10.1001/jama.293.17.2102. [DOI] [PubMed] [Google Scholar]
- 42.Cauley JA, Hochberg MC, Lui LY, Palermo L, Ensrud KE, Hillier TA, Nevitt MC, Cummings SR. Long term risk of incident vertebral fractures. JAMA. 2007;298:2761–2767. doi: 10.1001/jama.298.23.2761. [DOI] [PubMed] [Google Scholar]
- 43.Seeman E, Delmas PD. Bone quality–the material and structural basis of bone strength and fragility. N Engl J Med. 2006;354:2250–2261. doi: 10.1056/NEJMra053077. [DOI] [PubMed] [Google Scholar]
- 44.Ralston SH, de Crombrugghe B. Genetic regulation of bone mass and susceptibility to osteoporosis. Genes Dev. 2006;20:2492–2506. doi: 10.1101/gad.1449506. [DOI] [PubMed] [Google Scholar]
- 45.Shaffer JR, Kammerer CM, Reich D, McDonald G, Patterson N, Goodpaster B, Bauer DC, Li J, Newman AB, Cauley JA, Harris TB, Tylavsky F, Ferrell RE, Zmuda JM. Genetic markers for ancestry are correlated with body composition traits in older African Americans. Osteoporos Int. 2007;18:733–741. doi: 10.1007/s00198-006-0316-6. [DOI] [PubMed] [Google Scholar]
- 46.Cummings SR, Lee JS, Lui LY, Stone K, Ljung BM, Cauleys JA. Sex hormones, risk factors, and risk of estrogen receptor-positive breast cancer in older women: A long-term prospective study. Cancer Epidemiol Biomarkers Prev. 2005;14:1047–1051. doi: 10.1158/1055-9965.EPI-04-0375. [DOI] [PubMed] [Google Scholar]
- 47.Cauley JA, Danielson ME, Boudreau RM, Forrest KY, Zmuda JM, Pahor M, Tylavsky FA, Cummings SR, Harris TB, Newman AB. Inflammatory markers and incident fracture risk in older men and women: The health aging and body composition study. J Bone Miner Res. 2007;22:1088–1095. doi: 10.1359/jbmr.070409. [DOI] [PubMed] [Google Scholar]
- 48.Holick MF, Siris ES, Binkley N, Beard MK, Khan A, Katzer JT, Petruschke RA, Chen E, de Papp AE. Prevalence of Vitamin D inadequacy among postmenopausal North American women receiving osteoporosis therapy. J Clin Endocrinol Metab. 2005;90:3215–3224. doi: 10.1210/jc.2004-2364. [DOI] [PubMed] [Google Scholar]
- 49.Delmas PD, van de Langerijt L, Watts NB, Eastell R, Genant H, Grauer A, Cahall DL. Underdiagnosis of vertebral fractures is a worldwide problem: The IMPACT study. J Bone Miner Res. 2005;20:557–563. doi: 10.1359/JBMR.041214. [DOI] [PubMed] [Google Scholar]
- 50.Lewiecki EM, Laster AJ. Clinical review: Clinical applications of vertebral fracture assessment by dual-energy x-ray absorptiometry. J Clin Endocrinol Metab. 2006;91:4215–4222. doi: 10.1210/jc.2006-1178. [DOI] [PubMed] [Google Scholar]
- 51.Harris ST, Watts NB, Genant HK, McKeever CD, Hangartner T, Keller M, Chesnut CH, III, Brown J, Eriksen EF, Hoseyni MS, Axelrod DW, Miller PD. Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: A randomized controlled trial. Vertebral Efficacy With Risedronate Therapy (VERT) Study Group. JAMA. 1999;282:1344–1352. doi: 10.1001/jama.282.14.1344. [DOI] [PubMed] [Google Scholar]
- 52.Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, Marcus R, Ott SM, Torner JC, Quandt SA, Reiss TF, Ensrud KE. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet. 1996;348:1535–1541. doi: 10.1016/s0140-6736(96)07088-2. [DOI] [PubMed] [Google Scholar]
- 53.Ettinger B, Black DM, Mitlak BH, Knickerbocker RK, Nickelsen T, Genant HK, Christiansen C, Delmas PD, Zanchetta JR, Stakkestad J, Gluer CC, Krueger K, Cohen FJ, Eckert S, Ensrud KE, Avioli LV, Lips P, Cummings SR. Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: Results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. JAMA. 1999;282:637–645. doi: 10.1001/jama.282.7.637. [DOI] [PubMed] [Google Scholar]
- 54.Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, Cosman F, Lakatos P, Leung PC, Man Z, Mautalen C, Mesenbrink P, Hu H, Caminis J, Tong K, Rosario-Jansen T, Krasnow J, Hue TF, Sellmeyer D, Eriksen EF, Cummings SR. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007;356:1809–1822. doi: 10.1056/NEJMoa067312. [DOI] [PubMed] [Google Scholar]
- 55.Nevitt MC, Thompson DE, Black DM, Rubin SR, Ensrud K, Yates AJ, Cummings SR. Effect of alendronate on limited-activity days and bed-disability days caused by back pain in postmenopausal women with existing vertebral fractures. Fracture Intervention Trial Research Group. Arch Intern Med. 2000;160:77–85. doi: 10.1001/archinte.160.1.77. [DOI] [PubMed] [Google Scholar]
- 56.Parra EJ, Marcini A, Akey J, Martinson J, Batzer MA, Cooper R, Forrester T, Allison DB, Deka R, Ferrell RE, Shriver MD. Estimating African American admixture proportions by use of population-specific alleles. Am J Hum Genet. 1998;63:1839–1851. doi: 10.1086/302148. [DOI] [PMC free article] [PubMed] [Google Scholar]