Introduction
Bulimia nervosa (BN) is a common eating disorder (Hudson, Hiripi, Pope, & Kessler, 2007) which carries medical, social, and functional burdens (Crow & Peterson, 2003). A number of treatments have been developed which show some benefit, including cognitive behavioral therapy (CBT), interpersonal therapy and numerous pharmacotherapies (Shapiro, et al., 2007). Psychotherapeutic treatments have generally shown better response rates than pharmacotherapies, but there are a number of strategic challenges in providing these therapies. It is uncommon for patients to receive these specific treatments from therapists trained in their use. This appears to be due to several factors, including the limited number of specialty centers for eating disorders; limited numbers of psychology training programs that include these treatments; and limited numbers of therapists who receive training in these treatments (Mussell, et al., 2000). As a result, previous research suggest that individuals presenting for BN have usually not received an adequate trial of empirically supported psychotherapy for BN (Crow, Mussell, Peterson, Knopke, & Mitchell, 1999).
One option to consider to improve dissemination of these treatment is by strengthening training efforts. Another potential strategy is to provide such treatments via telemedicine. This approach has several potential benefits. First, it would make treatment from specialized eating disorder centers available in broad geographic areas. Second, it would allow for more efficient and specialized training and supervision of therapists. Finally, it is possible that treatment provided in this way could be more effective and less costly than alternatives (for example, compared to face-to-face therapy, there could advantages in time and travel cost). Limited work to date examining costs in telepsychiatry suggests this may be true (Harley, 2006; O'Reilly, et al., 2007)
The goal of this analysis was to examine the cost effectiveness of CBT delivered via telemedicine versus face-to-face treatment with individuals with BN.
Methods
The treatment study from which this analysis was drawn is described in detail elsewhere (Mitchell, et al., 2008). In brief, the study was conducted at nine regional sites in eastern North Dakota and northwestern Minnesota; sites were 46 to 194 miles from the coordinating center. Participants were women with a DSM-IV (American Psychiatric Association, 1994) diagnosis of BN (purging or non-purging subtype) or eating disorder not otherwise specified fulfilling at least one of the following: (1) DSM-IV criteria for BN except binge eating/purging at a minimum frequency of once per week; or (2) DSM-IV criteria for BN with only subjective binge eating episodes. Subjects were excluded for weight less than 85% of ideal body weight; recent change in prescribed psychotropic medication (in the past six weeks); prior treatment with at least eight sessions of CBT; substance abuse in the past six months; pregnancy; significant medical illness that would jeopardize study participation; significant suicidal risk as assessed by the investigators; active psychosis; or a current or prior diagnosis of schizophrenia or bipolar illness.
Treatment in this study involved CBT using a manual-based CBT that has been studied widely (Agras, et al., 2000; Fairburn, Marcus, & Wilson, 1993; Fairburn, et al., 1995). Twenty sessions were conducted over a 16 week period. Treatment was face-to-face (FTF-CBT) or via telemedicine. In the telemedicine condition (TV-CBT) treatment was provided using a telemedicine system linking the regional health care system facilities using T1 lines. Therapy was provided by doctoral level psychologist who received weekly supervision. Therapy sessions were audiotaped with random review of therapy tapes for adherence. Assessments included the Eating Disorder Examination (Fairburn & Cooper, 1993); and the Structured Clinical Interview for DSM-IV (First, 1995). Approval was obtained from the Institutional Review Board prior to initiation of the study.
Cost Effective Analysis
A societal perspective was chosen for this cost effective analysis. Cost of treatment and travel time both for therapists and subjects were calculated. In this study, the health care utilization recorded was study related treatment including initial evaluation, laboratory evaluation and psychotherapy visits. In addition, costs were calculated for time and fuel costs for travel to and from sessions, both for therapists and subjects. Unit costs were derived from the Center for Medicare and Medicaid Services website (www.cms.hhs.gov). Effectiveness was defined as abstinence at the end of one year follow-up using data from the EDE.
Costs were compared by calculating cost effectiveness ratios, in which the total cost for all subjects in an arm was divided by the number of abstinent subjects (at end of follow-up) in that arm to yield a cost per abstinent subject. Bootstrapping for 10,000 iterations was conducted in order to address measurement error. In order to address error in assumptions, sensitivity analyses were conducted.
Results
The clinical and demographic characteristics of the sample by treatment arm are shown in Table 1. A total of 128 subjects were randomized, 66 to FTF-CBT and 62 to TV-CBT. At 12 month follow-up, abstinence from binge eating and purging by last observation carried forward was 28.8% in the FTF-CBT group and 22.6% in the TV-CBT group.
Table 1.
Subject Demographic and Clinical Characteristics
| Treatment Group | ||
|---|---|---|
| Characteristic | FTF-CBT (n=66) |
TV-CBT (n=62) |
| Age, years (mean ± SD) | 29.6 ± 10.9 | 28.4 ± 10.4 |
| Body mass index, kg/m (mean ± SD) | 23.3 ± 5.0 | 23.5 ± 5.4 |
| Female (n, %) | 64 (97.0%) | 62 (100%) |
| Caucasian (n, %) | 62 (93.9%) | 61 (98.4%) |
| Post high school education (n, %) | 55 (83.3%) | 56 (90.3%) |
| Baseline Objective binge episodes previous 28 days1 (mean ± SD, median) | 21.9 ± 27.3 (11.5) | 19.1 ± 24.7 (14.5) |
| Baseline Vomiting episodes previous 28 days2 (mean ± SD, median) | 31.3 ± 34.3 (24.0) | 28.5 ± 28.3 (24.0) |
| Current diagnosis | ||
| Bulimia nervosa (n, %) | 38 (57.6%) | 33 (53.2%) |
| Eating disorders not otherwise specified (n, %) | 28 (42.4%) | 29 (46.8%) |
| Abstinence at follow-up (n, %) | 18 (27.3%) | 16 (25.8%) |
Binge-eating episode frequency reported as “too great to calculate” (n = 1) recoded to maximum reported value (132)
Vomiting episode frequency reported as “too great to calculate” (n = 3) recoded to maximum reported value (132)
The total cost by arm is shown in Table 2, CBT charges (and in FTF-CBT, therapist travel) represented the largest sources of cost. In addition, the average number of sessions attended by subject and the average travel time by arm for both subjects and therapists are shown in Table 2. Cost effectiveness ratios expressed as cost per abstinent subjects are also found in Table 3. Bootstrapping results are shown in Figure 1. These indicate that in 78.9% of iterations, TV-CBT was less effective but also less costly than FTF-CBT, while in 21.1% TV-CBT was both more effective and less costly.
Table 2.
Mean Costs per Subject by Treatment Arm
| FTF-CBT | TV-CBT | |
|---|---|---|
| Total Costs | $2,684.38 | $1,648.48 |
| Evaluation and laboratory | $151.59 | $151.59 |
| CBT | $1,131.33 | $1,342.47 |
| Subject Travel | $173.89 | $101.97 |
| Gasoline | $89.44 | $52.45 |
| Therapist Travel | $1,138.14 | $0.00 |
FTF-CBT = Face-to-Face CBT
TV-CBT = CBT via telemedicine
| Notes: | 1. Costs are in 2005 US dollars | ||
| 2. Mean # of sessions: | FTF-CBT: | 13.4 (50.71) | |
| TV-CBT: | 14.2 (50.60) | ||
| 3. Mean one way subject travel time | FTF-CBT: | 14 minutes | |
| TV-CBT: | 8 minutes |
Table 3.
Cost Effectiveness and Sensitivity Analyses by Arm
| FTF-CBT | TV-CBT | |
|---|---|---|
| Cost per Abstinent Subject | $9,324.68 | $7,300.40 |
| Sensitivity Analyses | ||
| Full price1 | $10,938.53 | $9,507.57 |
| 2008 gasoline price2 | $9,763.81 | $7,628.56 |
| Built-in videocam3 | $9,324.68 | $6,586.78 |
FTF-CBT = Face-to-Face
CBT TV-CBT = CBT via telemedicine
Assumes $120/hr CBT cost
Assumes January 2008 US gas price of $3.21
Assumes TV-CBT delivered via built-in videocam in home computer.
Figure 1.
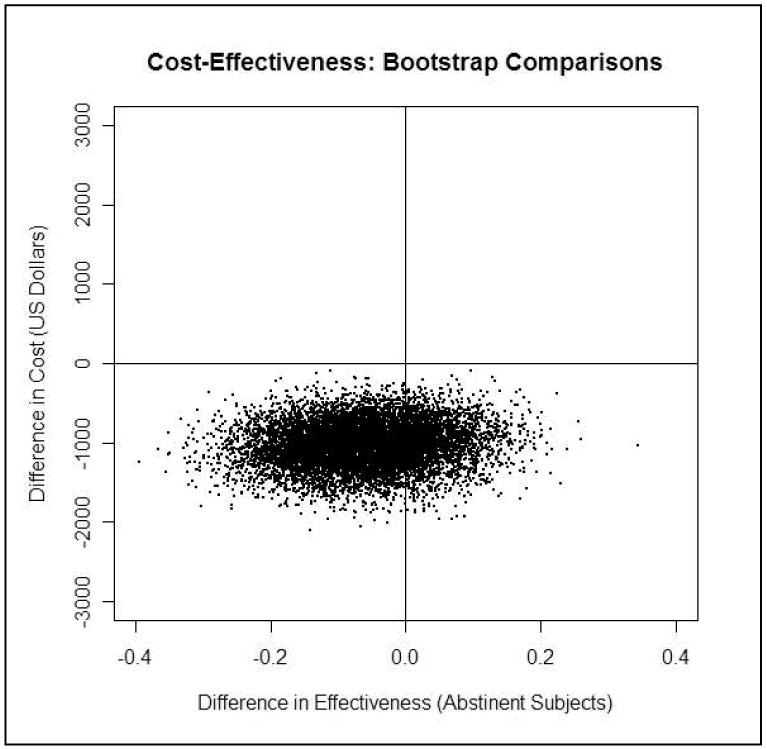
Bootstrapping Analysis
Note: Bootstrapping results yield a distribution of points in four potential quadrants with four conditions. 1. upper right: Greater cost and greater effectiveness; 2. lower left: lower cost but lower effectiveness; 3. upper left: greater cost but lower effectiveness; or 4. lower right: lower costs and greater effectiveness. The first two conditions represent potentially interesting tradeoffs. The third condition (higher costs/lower effectiveness) is not an appealing one. The final condition (where the treatment of interest is more effective and costs less) is referred to as a condition of dominance.
Sensitivity analysis was conducted to test three assumptions. First, given that unit costs came from CMS, an alternative assumption where full clinical prices were paid for treatment was examined. Second, given that prices were calculated in 2005 dollars, the travel component of costs reflects US gasoline prices of $2.27 per gallon (Energy Information Administration, Washington, D.C. USA). Thus, sensitivity analysis was done assuming February 2008 average US gasoline prices of $3.21 per gallon. Third, cost in the TV-CBT arm included a per session charge for the telemedicine connection. However, video cameras of increasingly high quality are frequently incorporated in personal computers. These could be used at no cost, and would represent an alternative mechanism for treatment delivery; therefore, sensitivity analysis was conducted in which no charges were included for the telemedicine component. The results of these analyses are shown in Table 3. These analyses revealed limited changes to cost effectiveness ratios, and the relationship of cost per abstinent subject between FTF-CBT and TV-CBT appeared fundamentally unaltered.
Discussion
In this study, CBT delivered face-to-face and CBT delivered via telemedicine had similar efficacy, but TV-CBT was associated with a lower cost per abstinent subject. The results of bootstrapping generally supported this conclusion; in most bootstrapped samples, TV-CBT was somewhat less effective but also cost substantially less. Differences in costs between the two treatments were largely accounted for by therapist travel costs; other costs related to treatment were similar between the two conditions. Cost per abstinent subject was relatively insensitive to costs of fuel as well as to costs associated with telemedicine.
These results support limited prior work in other disorders suggesting that telepsychiatry is effective and can be less costly (Harley, 2006; O'Reilly, et al., 2007). Such a telemedicine approach may be particularly well-suited to the treatment of eating disorders, given the limited number of specialized centers, the relative prominence of specialized psychotherapies in the array of affective treatments available, and the rarity with which those therapies are currently provided. In particular, telepsychiatry might be employed in a stepped care approach to treatment. Since much of the cost differential was accounted for by travel time, this approach may be more suited to rural areas then urban areas. In addition, such an approach would presume an excess capacity of specialized therapists, which may not be the case in all centers.
The study has a number of strengths, including the rigor with which therapy and structured assessment were provided. In addition, studies of telemedicine by their nature may be more generalizable and less subject to geographic idiosyncrasies than more traditional types of treatment. Another strength of this study is the inclusion of both individuals who met full criteria for BN as well as those with EDNOS with subsyndromal BN. There are also limitations to consider, particularly to the cost assessments. In this study, a full accounting of costs was not available. It would have been ideal to have information on hospitalizations, other medical utilization, and medication use, but this intensity of costs collection was not conducted here. Additionally, more extensive measures of societal perspective costs would be ideal but results of these were not available (and for eating disorders, remain undeveloped).
In summary, this study suggests that provision of CBT for BN via telemedicine may be more cost effective than face-to-face treatment when provided over a large geographic area. This alternative strategy for the delivery of highly specialized treatment holds promise in the area of eating disorders and might be similarly applicable to other types of psychopathology.
Acknowledgments
Supported in part by K02 MH 65911, P30 DK 60456 and (R01 MH 058820).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agras WS, Crow SJ, Halmi KA, Mitchell JE, Wilson GT, Kraemer HC. Outcome predictors for the cognitive behavior treatment of bulimia nervosa: Data from a multisite study. Am J Psychiatry. 2000;157(8):1302–1308. doi: 10.1176/appi.ajp.157.8.1302. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Crow S, Mussell MP, Peterson C, Knopke A, Mitchell J. Prior treatment received by patients with bulimia nervosa. Int J Eat Disord. 1999;25(1):39–44. doi: 10.1002/(sici)1098-108x(199901)25:1<39::aid-eat5>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- Crow SJ, Peterson CB, editors. The economic and social burden of eating disorders. Vol. 6. New York: Wiley and Sons; 2003. [Google Scholar]
- Fairburn CG, Cooper Z, editors. Binge eating, nature, assessment and treatment. New York: Guilford Press; 1993. [Google Scholar]
- Fairburn CG, Marcus MD, Wilson GT, editors. Cognitive-behavioral therapy for binge eating and bulimia nervosa: A comprehensive treatment manual. New York: Guilford Press; 1993. [Google Scholar]
- Fairburn CG, Norman PA, Welch SL, O'Connor ME, Doll HA, Peveler RC. A prospective study of outcome in bulimia nervosa and the long-term effects of three psychological treatments. Arch Gen Psychiatry. 1995;52(4):304–312. doi: 10.1001/archpsyc.1995.03950160054010. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for dsm-iv axis i disorders. Patient edition (scid-p, version 2. New York: New York State Psychiatric Institute, Biometrics Research; 1995. [Google Scholar]
- Harley J. Economic evaluation of a tertiary telepsychiatry service to an island. J Telemed Telecare. 2006;12(7):354–357. doi: 10.1258/135763306778682378. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the national comorbidity survey replication. Biol Psychiatry. 2006 doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell JE, Crosby RD, Wonderlich SA, Crow S, Lancaster K, Simonich H, et al. A randomized trial comparing the efficacy of cognitive-behavioral therapy for bulimia nervosa delivered via telemedicine versus face-to-face. Behav Res Ther. 2008;46(5):581–592. doi: 10.1016/j.brat.2008.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mussell MP, Crosby RD, Crow SJ, Knopke AJ, Peterson CB, Wonderlich SA, et al. Utilization of empirically supported psychotherapy treatments for individuals with eating disorders: A survey of psychologists. International Journal of Eating Disorders. 2000;27(2):230–237. doi: 10.1002/(sici)1098-108x(200003)27:2<230::aid-eat11>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- O'Reilly R, Bishop J, Maddox K, Hutchinson L, Fisman M, Takhar J. Is telepsychiatry equivalent to face-to-face psychiatry? Results from a randomized controlled equivalence trial. Psychiatr Serv. 2007;58(6):836–843. doi: 10.1176/ps.2007.58.6.836. [DOI] [PubMed] [Google Scholar]
- Shapiro JR, Berkman ND, Brownley KA, Sedway JA, Lohr KN, Bulik CM. Bulimia nervosa treatment: A systematic review of randomized controlled trials. Int J Eat Disord. 2007;40(4):321–336. doi: 10.1002/eat.20372. [DOI] [PubMed] [Google Scholar]


