Abstract
BACKGROUND:
The OxyMask (Southmedic Inc, Canada) is a new face mask for oxygen delivery that uses a small ‘diffuser’ to concentrate and direct oxygen toward the mouth and nose. The authors hypothesized that this unique design would enable the OxyMask to deliver oxygen more efficiently than a Venturi mask (Hudson RCI, USA) in patients with chronic hypoxemia.
METHODS:
Oxygen-dependent patients with chronic, stable respiratory disease were recruited to compare the OxyMask and Venturi mask in a randomized, single-blind, cross-over design. Baseline blood oxygen saturation (SaO2) was established breathing room air, followed in a random order by supplemental oxygen through the OxyMask or Venturi mask. Oxygen delivery was titrated to maintain SaO2 4% to 5% and 8% to 9% above baseline for two separate 30 min periods of stable breathing. Oxygen flow rate, partial pressure of inspired and expired oxygen (PO2) and carbon dioxide (PCO2), minute ventilation, heart rate, nasal and oral breathing, SaO2 and transcutaneous PCO2 were collected continuously. The study was repeated following alterations to the OxyMask design, which improved clearance of carbon dioxide.
RESULTS:
Thirteen patients, aged 28 to 79 years, were studied initially using the original OxyMask. Oxygen flow rate was lower, inspired PO2 was higher and expired PO2 was lower while using the OxyMask. Minute ventilation and inspired and expired PCO2 were significantly higher while using the OxyMask, whereas transcutaneous PCO2, heart rate and the ratio of nasal to oral breathing did not change significantly throughout the study. Following modification of the OxyMask, 13 additional patients, aged 18 to 79 years, were studied using the same protocol. The modified OxyMask provided a higher inspired PO2 at a lower flow rate, without evidence of carbon dioxide retention.
CONCLUSIONS:
Oxygen is delivered safely and more efficiently by the OxyMask than by the Venturi mask in stable oxygen-dependent patients.
Keywords: Chronic obstructive pulmonary disease, Hypoxemia, Oxygen masks, Oxygen therapy, Respiratory failure
Abstract
HISTORIQUE :
L’OxyMask (Southmedic Inc., Canada) est un nouveau masque facial pour l’administration d’oxygène qui utilise un petit « diffuseur » pour concentrer et diriger l’oxygène vers la bouche et le nez. Selon l’hypothèse des auteurs, cette conception originale permettrait à l’OxyMask d’administrer l’oxygène plus efficacement que le masque Venturi (Hudson RCI, É. U.) chez les patients souffrant d’hypoxémie chronique.
MÉTHODES :
Des patients atteints de maladie respiratoire chronique stable et dépendants de l’oxygénothérapie ont été recrutés afin de comparer l’OxyMask et le masque Venturi dans le cadre d’un protocole randomisé à simple insu avec permutation des groupes. La saturation du sang en oxygène (SaO2) a été établie au départ à l’air ambiant, ensuite de manière aléatoire avec des suppléments d’oxygène administrés au moyen de l’OxyMask ou du masque Venturi. L’administration d’oxygène a été ajustée de manière à maintenir la SaO2 entre 4 et 5 % et 8 et 9 % au-dessus des données de départ pendant deux périodes distinctes de 30 minutes de respiration stable. Le débit d’oxygène, la pression partielle de l’oxygène inspiré et expiré (PO2) et du gaz carbonique (PCO2), la ventilation par minute, la fréquence cardiaque, la respiration nasale et buccale, la SaO2 et la PCO2 transcutané ont été recueillis de manière continue. L’étude a été répétée après des modifications apportées au modèle de l’OxyMask qui ont amélioré l’élimination du CO2.
RÉSULTATS :
Treize patients, âgés de 28 à 79 ans, ont été examinés au départ avec l’OxyMask original. Le débit d’oxygène était plus faible, la PO2 inspirée était plus élevée et la PO2 expirée était plus faible avec l’OxyMask. La ventilation par minute et la PCO2 inspiré et expiré ont été significativement plus élevés avec l’OxyMask, tandis que la PCO2 transcutane, la fréquence cardiaque et le ratio de respiration nasale vs orale n’ont pas changé significativement au cours de l’étude. Après la modification de l’OxyMask, treize autres patients âgés de 18 à 79 ans ont été étudiés au moyen du même protocole. L’OxyMask modifié a donné lieu à une PO2 inspirée plus élevée avec un débit moindre, sans signe de rétention du CO2.
CONCLUSION :
L’oxygène est administré sans danger et plus efficacement avec l’OxyMask qu’avec le masque Venturi chez les patients dépendants de l’oxygénothérapie dont l’état est stable.
Patients with severe lung disease often require supplemental oxygen to maintain an adequate level of oxygen in the blood and adequate delivery of oxygen to vital organs (1). In patients with chronic hypoxemia, oxygen therapy is usually provided through nasal cannulae and can improve sleep and mood, increase mental alertness and stamina, enable an oxygen-dependent patient to carry out activities of daily living, and prevent pulmonary hypertension and cor pulmonale (2). In patients with acute or acute-on-chronic hypoxemia, supplemental oxygen is usually administered through a face mask. One of the commonly used, conventional face masks for oxygen delivery is the ‘Venturi’ or air-entrainment system (1).
While the Venturi mask is effective at delivering accurate oxygen concentrations (FiO2), it requires relatively high oxygen flow rates to achieve this. The OxyMask (Southmedic Inc, Canada) is a new face mask for oxygen delivery that uses a small ‘diffuser’ to concentrate and direct oxygen toward the nose and mouth, thereby delivering high concentrations of oxygen at a relatively low flow. We hypothesized that this system delivers oxygen more efficiently and more comfortably than the conventional Venturi mask. We studied this hypothesis by titrating supplemental oxygen in oxygen-dependent patients through an OxyMask and Venturi mask (Hudson RCI, USA) in a randomized, single-blind, cross-over design. Although the diffuser technology has been evaluated previously, this has predominantly been in healthy volunteers (3–5), in which the diffuser was placed in a plastic boom connected to a headset (OxyArm, Southmedic Inc). Only one previous investigation has used the OxyArm in oxygen-dependent patients (6). However, the authors did not provide information about disease severity, including pulmonary function measurements and arterial blood gases. Consequently, it is unknown how disease severity, including the presence of chronic carbon dioxide retention, impacts the effectiveness of the diffuser technology. Moreover, the diffuser has not been evaluated while placed in a face mask. These differences in patient population and mask design may limit the application of this new technology in patients with severe lung disease. Consequently, we performed a pilot study on a group of stable oxygen-dependent patients to determine if the OxyMask can deliver oxygen safely and more efficiently than the Venturi system in this patient population.
METHODS
Patient recruitment
Patients aged 18 to 80 years with chronic pulmonary disease who were using supplemental oxygen, and whose oxygen requirement was stable (ie, did not change over a 3 h period at rest) were invited to participate in the study. Patients whose oxygen requirement was unstable (ie, changed hourly) and those who could not tolerate being off supplemental oxygen for 10 min were excluded. A detailed medical history and the most recent pulmonary function test and arterial blood gas measurements were obtained for each patient enrolled in the study. The study protocol was approved by the research ethics board at St Michael’s Hospital (Toronto, Ontario), and all patients gave written informed consent to participate.
OxyMask
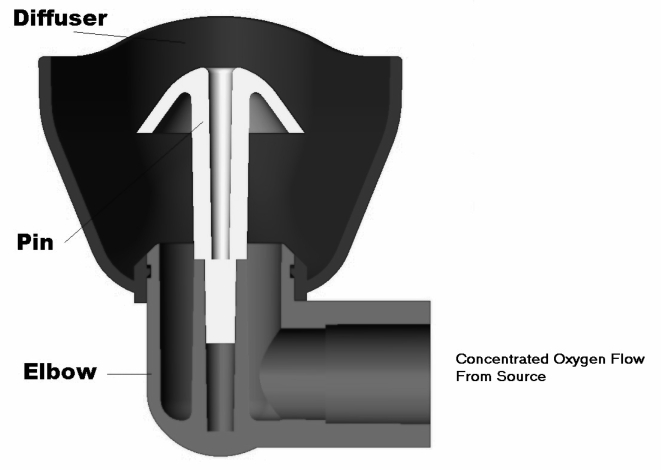
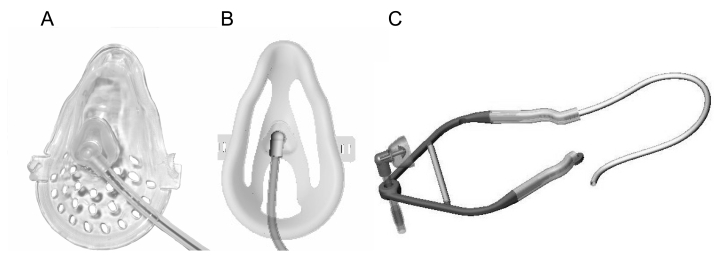
The OxyMask uses a small diffuser, comprised of a cup and pin, to concentrate and direct oxygen toward the nose and mouth (Figure 1). Oxygen diffuses out from the inlet and pin in the shape of a mushroom. During inspiration, the shape of the diffuser causes complex velocity vortexes to form, which forces oxygen into a flame-like shape toward the face. This dynamic property of the diffuser is unique to this oxygen delivery system and results in concentrated oxygen delivery during inspiration (3). The mask itself is comprised of a plastic mold, which covers the nose and mouth, and an elastic band to hold the mask in place (Figure 2A). The diffuser cup is positioned approximately 2 cm away from the nose and mouth. Two modified versions of the mask, which also employ the diffuser, combine the stability of a mask with an open oxygen delivery system, thereby reducing the likelihood for carbon dioxide retention to occur. In one modified version of the mask, the plastic mold is resected to create an open system while continuing to stabilize the diffuser cup and hold it in front of the face (Figure 2B). Another version is comprised of a rigid plastic brace in which the diffuser cup sits. An elastic band crosses the front of the brace, which allows it to rest comfortably on the chin and hold the cup in front of the face. The side arms of the brace sit below the ears and are secured by an adjustable elastic band that stretches behind the neck (Figure 2C).
Figure 1).
Cross-sectional drawing illustrating the shape of the cup that houses the pin diffuser of the OxyMask (Southmedic Inc, Canada) system. Courtesy of Southmedic Inc
Figure 2.
The OxyMask (Southmedic Inc, Canada) oxygen delivery system. A Original OxyMask; B Modified OxyMask with plastic mold resected; C Modified OxyMask comprised of brace and elastic bands. Courtesy of Southmedic Inc
Protocol
The study used a single-blind, randomized, cross-over design (Figure 3). All study measurements were performed during wakefulness in the seated, upright position. In each patient, baseline oxygen saturation (SaO2) was established after breathing room air for 10 min (washout period). Following the washout period, 5 min of baseline measurements (outlined below) were obtained breathing room air. Stable SaO2 during this 5 min period was required before proceeding. Patients then received supplemental oxygen for 60 min through either the OxyMask or Venturi mask, which were used in a random order. Oxygen delivery was titrated to maintain blood SaO2 4% to 5% (low saturation) and 8% to 9% (high saturation) above baseline, each for 30 min of stable breathing. The order of targeting ‘low saturation’ and ‘high saturation’ was also randomized. Oxygen therapy was then discontinued and another set of baseline measurements was obtained breathing room air for 5 min after a second washout period. Patients then received supplemental oxygen therapy through the remaining mask (OxyMask or Venturi) for another 60 min following the same protocol described above.
Figure 3).
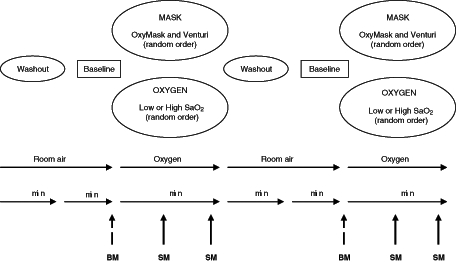
Study protocol comparing the OxyMask (Southmedic Inc, Canada) with the Venturi mask (Hudson RCI, USA). BM Baseline measurements; SaO2 Blood oxygen saturation; SM Study measurements
During all phases of the study, recordings were obtained by continuous monitoring of abdominal and chest movement (Respitrace, Ambulatory Monitoring Inc, USA); partial pressure of oxygen (PO2) (Oxigraf, USA) and partial pressure of carbon dioxide (PCO2) (Capnocheck, BCI/Smiths Medical PM Inc, USA) at the lower lip; heart rate and oximetry (Mallinckrodt/Nellcor Puritan Bennett, USA); transcutaneous PCO2 on the chest below the clavicle (Microgas, Kontron Instruments, United Kingdom); nasal and oral flow through a sensor placed on the upper lip (Ultima Dual Airflow Pressure Sensor, Braebon Medical Corporation, Canada); and oxygen flow rate (4100 Series, TCI Inc, USA) using a custom-made program (LabView 6.1, National Instruments, USA). Respitrace was calibrated to reflect tidal volume using a custom-made program (LabView 6.1) according to specified criteria (7). SaO2 was recorded from two oximeters with the probes placed on the patients’ fingers (one on each hand) to overcome any potential technical issues with the measurement, such as poor peripheral circulation. Data were collected on a breath-to-breath basis and continuous measurements of tidal volume, respiratory rate, maximum and minimum PCO2 and PO2, maximum nasal and oral flow, and mean SaO2, heart rate, transcutaneous PCO2 and oxygen flow rate were obtained. The data for each respiratory measurement during 5 min of breathing room air (baseline measurements) (Figure 3) and during the last 15 min of each experimental condition (study measurements) (Figure 3) are reported as means ± SD.
Patients were instructed to comment on what they liked and disliked about each mask and to rate the comfort of each mask on a linear scale from zero to 10. Within this scale, a rating of zero indicated the mask was ‘very uncomfortable’, five indicated it was ‘reasonably comfortable’, and a rating of 10 indicated the mask was ‘very comfortable’.
Once the first 13 patients were studied, a tendency for modest carbon dioxide retention associated with the OxyMask was noted. Consequently, the manufacturers modified the mask design (described above) to limit this tendency and the study was repeated in an additional 13 patients. Eight patients were studied using one modification (Figure 2B) and five patients were studied using the alternate modification (Figure 2C). Because both modifications were performed to address the same issue and the results with both modified masks were almost identical, the data from this second set of patients were combined. The study protocol was the same as that used for the first set of patients. Humidification was not used throughout the study.
Analysis
Mean values of tidal volume, respiratory rate and minute ventilation, minimum and maximum PCO2 and PO2, maximum nasal and oral flow, heart rate, oxyhemoglobin saturation, oxygen flow rate and transcutaneous PCO2 were calculated for each patient in each phase of the study. Mean SaO2 for each phase was determined by averaging data from both oximeters. The ratio of maximum nasal to oral breathing was calculated during baseline measurements and, in each titration phase, it was expressed as a proportion of baseline measurements. Group mean data and standard deviations were analyzed using repeated measures ANOVA and the unpaired Student’s t test (SPSS version 12.0, SPSS Inc, USA). P<0.05 was considered statistically significant.
RESULTS
Patient demographics
Thirteen patients, aged 28 to 79 years, were studied using the original OxyMask. Thirteen additional patients, aged 18 to 79 years, were studied using the modified versions of the OxyMask. Table 1 shows the patient demographic data. All patients required supplemental oxygen at rest and during exercise. Patients studied using the original and modified versions of the OxyMask had a variety of respiratory disorders, as outlined in Table 2. Table 3 shows the spirometry and arterial blood gas results. Sixteen patients (62%) had chronic hypercapnia, defined as PCO2 greater than 45 mmHg from arterial blood gas measurements on room air. There were no significant differences in patient demographics, respiratory diagnoses or pulmonary function between patients who were studied using the original OxyMask and patients who were studied using the modified masks.
TABLE 1.
Patient demographics
| Original OxyMask | Modified OxyMask | |
|---|---|---|
| Patients, n | 13 | 13 |
| Male:female | 4:9 | 5:8 |
| Age, years | 56±16 | 60±16 |
| Body mass index, kg/m2 | 35.0±12.3 | 32.7±9.2 |
| O2 requirement (rest), L/min | 2.3±1.3 | 2.5±1.2 |
| O2 requirement (exercise), L/min | 3.4±1.6 | 3.4±1.4 |
Data are presented as means ± SD unless otherwise indicated. There were no significant differences in patient demographics between those who used the original and those who used the modified OxyMask (Southmedic Inc, Canada)
TABLE 2.
Respiratory diagnosis
| Original OxyMask | Modified OxyMask | |
|---|---|---|
| COPD | 5 | 5 |
| Hypoventilation syndrome | ||
| Obesity | 1 | 1 |
| Obesity, COPD | 1 | 1 |
| Post-polio syndrome | 1 | 0 |
| Chest wall disease | ||
| Kyphoscoliosis | 1 | 1 |
| Postesophageal surgery | 1 | 0 |
| Cystic fibrosis | 2 | 1 |
| Idiopathic pulmonary fibrosis | 1 | 2 |
| Bronchiectasis | 0 | 1 |
| Pulmonary hypertension | 0 | 1 |
There were no significant differences in respiratory diagnoses between those who used the original and those who used the modified OxyMask (Southmedic Inc, Canada). COPD Chronic obstructive pulmonary disease
TABLE 3.
Pulmonary function tests
| Original OxyMask
|
Modified OxyMask
|
|||
|---|---|---|---|---|
| Measured | Predicted (%) | Measured | Predicted (%) | |
| Spirometry | ||||
| FVC, L | 1.87±0.66 | 57.38±13.20 | 1.63±0.53 | 52.33±14.06 |
| FEV1, L | 1.22±0.56 | 51.54±21.50 | 0.99±0.54 | 44.75±23.56 |
| FEV1/FVC, % | 65.06±19.29 | – | 59.7±22.5 | – |
| FEF50%, L/s | 1.38±1.23 | 42.15±34.71 | 1.40±1.82 | 46.92±64.92 |
| FEF75%, L/s | 0.40±0.32 | 25.23±18.66 | 0.35±0.34 | 23.33±21.63 |
| Vital capacity, L | 2.00±0.80 | 60.20±15.05 | 1.66±0.58 | 53.89±13.33 |
| ABG (room air) | ||||
| pH | 7.40±0.05 | 7.40±0.04 | ||
| P CO2, mmHg | 47.58±6.07 | 51.08±14.46 | ||
| P O2, mmHg | 52.75±7.56 | 51.83±8.44 | ||
| SaO2, % | 87±6 | 86±7 | ||
| HCO3–, mmol/L | 30.00±4.07 | 31.83±7.49 | ||
Data are presented as means ± SD. There were no significant differences in spirometry or arterial blood gases (ABG) between patients who used the original and those who used the modified OxyMask (Southmedic Inc, Canada). FEF50% Forced expiratory flow at 50% of vital capacity; FEF75% Forced expiratory flow at 75% of vital capacity; FEV1 Forced expiratory volume in 1 s; FVC Forced vital capacity; HCO3– Bicarbonate concentration; PCO2 Partial pressure of carbon dioxide; PO2 Partial pressure of oxygen; SaO2 Blood oxygen saturation
Mask efficiency
By study design, blood SaO2 did not differ significantly between oxygen titrations using the original OxyMask or Venturi mask (Table 4). Oxygen flow rate was significantly lower while using the OxyMask during both low and high SaO2 titrations. Oxygen flow was significantly higher for both masks during high SaO2 (P<0.001), and the difference in flow rate while using the OxyMask compared with the Venturi mask was greater during high SaO2 (P<0.001). Inspired PO2 was significantly higher and expired PO2 significantly lower while using the OxyMask compared with the Venturi mask. Inspired and expired PO2 were significantly higher during high SaO2 (P<0.001), and the difference in PO2 while using the OxyMask compared with the Venturi mask was greater during high SaO2 (P<0.05). Minute ventilation and inspired and expired PCO2 were significantly higher while using the original OxyMask than the Venturi mask. Transcutaneous PCO2, heart rate and the ratio of nasal to oral breathing did not change significantly throughout the study.
TABLE 4.
Oxygen titration – original OxyMask (Southmedic Inc, Canada)
| Low saturation
|
High saturation
|
P* | |||
|---|---|---|---|---|---|
| OxyMask | Venturi | OxyMask | Venturi | ||
| SaO2, % | 92.0±3.6 | 91.7±3.4 | 94.8±3.2 | 94.9±3.6 | NS |
| Flow, L/min | 0.9±0.3 | 4.8±1.5 | 2.1±0.9 | 12.2±3.9 | <0.001 |
| Ve, L/min | 9.1±5.0 | 7.4±4.2 | 10.6±5.9 | 8.0±4.4 | <0.05 |
| tCO2, mmHg | 51.9±8.9 | 51.4±7.6 | 51.3±9.1 | 52.4±8.0 | NS |
| PiO2, mmHg | 229.7±44.5 | 192.6±11.9 | 459.5±167.5 | 330.0±126.6 | <0.01 |
| PeO2, mmHg | 164.4±16.9 | 181.7±12.2 | 209.2±39.2 | 266.9±52.4 | <0.01 |
| PiCO2, mmHg | 3.9±1.5 | 1.6±0.9 | 3.2±0.6 | 1.4±0.8 | <0.01 |
| PeCO2, mmHg | 33.5±8.9 | 11.3±5.6 | 27.2±8.9 | 11.6±8.0 | <0.01 |
| HR, beats/min | 78±18 | 78±18 | 79±19 | 77±18 | NS |
| Nasal:oral | 1.20±0.32 | 1.01±0.26 | 1.11±0.22 | 1.07±0.26 | NS |
Data are presented as means ± SD.
OxyMask versus the Venturi mask (Hudson RCI, USA). HR Heart rate; Nasal:oral Ratio of nasal to oral breathing expressed as a proportion of the ratio at baseline; NS Not significant; PeCO2 Expired partial pressure of carbon dioxide; PeO2 Expired partial pressure of oxygen; PiCO2 Inspired partial pressure of carbon dioxide; PiO2 Inspired partial pressure of oxygen; SaO2 Blood oxygen saturation; tCO2 Transcutaneous partial pressure of carbon dioxide; Ve Minute ventilation
Similarly, the study design required that there was no difference in blood SaO2 during comparison of the modified OxyMask and the Venturi mask (Table 5). Oxygen flow rate was significantly lower while using the modified OxyMask compared with the Venturi mask. Oxygen flow was significantly higher during high SaO2 (P<0.001) and the difference in flow rate while using the modified OxyMask compared with the Venturi mask was greater during high SaO2 (P<0.001). Inspired PO2 was significantly higher and expired PO2 significantly lower while using the modified OxyMask than the Venturi mask. Inspired and expired PO2 were significantly higher during high SaO2 (P<0.001) and the difference in inspired PO2 while using the modified OxyMask compared with the Venturi mask was greater during high SaO2 (P<0.05). Although inspired PCO2 was significantly higher while using the modified OxyMask compared with the Venturi mask, the magnitude of the increase was approximately one-half that seen with the original OxyMask (Table 4). Furthermore, in contrast to what was found with the original OxyMask, minute ventilation and expired PCO2, in addition to transcutaneous PCO2, were not significantly different while using the modified OxyMask compared with the Venturi mask. Heart rate and the ratio of nasal to oral breathing did not change significantly throughout the study. Analysis of chronic hypercapnic patients alone showed similar results.
TABLE 5.
Oxygen titration – modified OxyMask (Southmedic Inc, Canada)
| Low saturation
|
High saturation
|
P* | |||
|---|---|---|---|---|---|
| OxyMask | Venturi | OxyMask | Venturi | ||
| SaO2, % | 90.6±3.3 | 90.8±3.2 | 94.8±2.3 | 95.3±2.7 | NS |
| Flow, L/min | 1.8±0.6 | 5.2±2.7 | 4.4±2.2 | 10.8±3.7 | <0.001 |
| Ve, L/min | 8.1±6.7 | 6.4±3.9 | 7.6±5.3 | 7.2±5.9 | NS |
| tCO2, mmHg | 54.5±11.0 | 54.4±11.4 | 56.0±11.6 | 55.7±11.7 | NS |
| PiO2, mmHg | 217.3±50.5 | 189.4±25.8 | 323.5±73.1 | 257.4±56.7 | <0.005 |
| PeO2, mmHg | 162.6±19.0 | 182.1±26.5 | 216.7±56.4 | 245.5±55.3 | <0.01 |
| PiCO2, mmHg | 2.4±1.6 | 1.2±0.9 | 2.4±1.8 | 1.4±0.8 | <0.05 |
| PeCO2, mmHg | 14.9±9.5 | 9.7±3.8 | 13.0±8.3 | 11.9±5.4 | NS |
| HR, beats/min | 86±16 | 85±17 | 85±16 | 83±15 | NS |
| Nasal:Oral | 1.04±0.54 | 1.10±0.69 | 0.97±0.55 | 1.01±0.58 | NS |
Data are presented as means ± SD.
OxyMask versus the Venturi mask (Hudson RCI, USA). HR Heart rate; Nasal:oral Ratio of nasal to oral breathing expressed as a proportion of the ratio at baseline; NS Not significant; PeCO2 Expired partial pressure of carbon dioxide; PeO2 Expired partial pressure of oxygen; PiCO2 Inspired partial pressure of carbon dioxide; PiO2 Inspired partial pressure of oxygen; SaO2 Blood oxygen saturation; tCO2 Transcutaneous partial pressure of carbon dioxide; Ve Minute ventilation
Mask satisfaction
There was a trend for a higher rating of mask comfort for the original OxyMask than for the Venturi mask, but this difference did not reach statistical significance (7.3±2.4 versus 5.1±2.5 [P=0.07] on the comfort scale, respectively). Similarly, ratings of mask comfort tended to be higher for the modified OxyMask than the Venturi mask, but this difference did not reach statistical significance (6.7±1.9 versus 4.9±2.4, P=0.09). Favourable comments regarding the original and modified OxyMask were that it was quiet, light, and that it fit better, was less humid and less intrusive than the Venturi mask.
DISCUSSION
Previous work has suggested that the diffuser used in the OxyMask delivers oxygen more efficiently than conventional interfaces (3). However, this study was performed using the OxyArm, in which the diffuser was placed in a plastic boom connected to a headset, and measurements were obtained in healthy volunteers (3). Subsequent work evaluating the diffuser technology used either healthy volunteers, nonoxygen-dependent patients, or patients with chronic obstructive pulmonary disease of unknown severity, and did not evaluate the diffuser while placed in a face mask (4–6,8,9). These differences in patient population and interface design may limit the application of earlier findings to patients with chronic, severe respiratory disease. We thought it was important to evaluate this before studying the usefulness of the OxyMask in a large group of patients with hypoxemic respiratory failure. Consequently, we performed a pilot study to determine whether oxygen can be delivered safely and more efficiently through the OxyMask compared with the Venturi mask in oxygen-dependent patients. To control for the effect of short-term changes in underlying respiratory disease, we chose patients who were clinically stable and made detailed measurements over a relatively short period of time. We recruited a heterogenous group of patients to determine whether our findings were consistent over a broad range of causes of oxygen dependency. Our study is the first to compare the efficiency of the OxyMask with the Venturi mask in oxygen-dependent patients.
The study demonstrated a number of interesting findings. Both the original and modified OxyMask delivered oxygen effectively to oxygen-dependent patients with severe lung disease. Target oxyhemoglobin saturation was obtained using a lower oxygen flow rate than with the conventional Venturi mask, demonstrating that it is a more efficient oxygen delivery system. Peak inspiratory PO2 was significantly higher while peak expiratory PO2 was significantly lower using the OxyMask than while using the Venturi mask. These findings demonstrate the unique functionality of the OxyMask. During inspiration, complex vortexes form as oxygen is released through the diffuser, and the concentration of oxygen is very high as it is drawn toward the nose and mouth. During expiration, oxygen diffuses away. Because of this unique function, the OxyMask does not require a reservoir to trap oxygen during expiration, nor does it require high oxygen flow rates to achieve a high FiO2. The original OxyMask did not allow adequate clearance of carbon dioxide away from the mask, as demonstrated by the rise in minute ventilation and higher PCO2. We attribute this to the fact that low oxygen flow rates and insufficient mask ventilation caused rebreathing to occur. This issue was corrected by the modifications to the OxyMask design, which employed a more open concept. Using the modified OxyMask, oxygen was delivered more efficiently, and although inspired PCO2 remained elevated, the difference to the Venturi mask was modest and it was not associated with a rise in minute ventilation or transcutaneous PCO2. Consequently, clinically significant carbon dioxide retention does not occur with the modified OxyMask, even in patients with chronic hypercapnic respiratory failure (Table 3).
The Venturi mask is commonly used for oxygen delivery, particularly in patients in whom inappropriately high FiO2 needs to be avoided (1). Oxygen is delivered at high velocity through a small orifice, and shear forces cause mixing of room air and oxygen (10). FiO2 can be adjusted using mask adaptors of different orifice sizes. The flow of gas delivered to the patient always exceeds minute ventilation, which prevents entrainment of room air around the mask and dilution of oxygen, but the oxygen flow rate requires adjustment for each orifice size (1). Delivering oxygen at flow rates exceeding minute ventilation provides a target FiO2 and also ensures adequate clearance of carbon dioxide (11). While accurate FiO2 can be obtained and varied according to patient demand using the Venturi mask, the options are limited to a specific size and number of adaptors, and increasingly high oxygen flow rates are required to deliver higher FiO2.
The physical design of the OxyMask may provide additional benefits. The size and configuration of current face masks limit their suitability for prolonged use in acute hypoxemic respiratory failure (1). Although ratings of mask comfort were similar between the OxyMask and the Venturi mask on the comfort scale, patients also reported that the OxyMask was quiet, light and relatively nonintrusive, in contrast to the Venturi mask, which patients found to be noisy, bulky and intrusive. Further innovative modifications in how the OxyMask diffuser is presented and stabilized may make it acceptable for prolonged use in hospital. The OxyMask is also simpler to use than the Venturi mask because it does not require multiple adaptors. This provides a more flexible setup, which may appeal to care givers and also reduce costs.
CONCLUSIONS
The OxyMask delivers oxygen safely and more efficiently than the Venturi mask. The tendency for carbon dioxide retention that was evident in the prototype model has been corrected by modifications to the mask design. The OxyMask provides a low-flow, open oxygen delivery system, which can deliver a broad range of FiO2 in a single setup. Further studies are required to define the clinical applications of this new technology in oxygen-dependent patients with acute and chronic respiratory failure.
Acknowledgments
The authors thank Dr Safraaz Mahamed for his assistance with the study.
Footnotes
CONFLICT OF INTEREST: Dr Patrick Hanly received financial support from Southmedic Inc to perform this study. He also received an honorarium from Southmedic Inc for attendance at a single Advisory Board meeting. Mr Jaime Beecroft has received financial support from Southmedic Inc to present the data in this article at an international scientific meeting.
REFERENCES
- 1.Heuer A, Scanlan C. Medical gas therapy. In: Wilkins R, Stoller J, editors. Egan’s Fundamentals of Respiratory Care. 8th edn. St Louis: CV Mosby; 2003. pp. 827–67. [Google Scholar]
- 2.Ryerson G, Block A. Oxygen as a drug: Clinical properties, benefits, modes, and hazards of administration. In: Burton G, Hodgkin J, Ward J, editors. Respiratory Care. 3rd edn. Philadelphia: JB Lippincott Co; 1991. pp. 19–39. [Google Scholar]
- 3.Ling E, McDonald L, Dinesen, DuVall D. The OxyArm – A new minimal contact oxygen delivery system for mouth or nose breathing. Can J Anaesth. 2002;49:297–301. doi: 10.1007/BF03020531. [DOI] [PubMed] [Google Scholar]
- 4.Paul J, Ling E, Hajgato J, McDonald L. Both the OxyArm and Capnoxygen mask provide clinically useful capnographic monitoring capability in volunteers. Can J Anaesth. 2003;50:137–42. doi: 10.1007/BF03017845. [DOI] [PubMed] [Google Scholar]
- 5.Sasaki H, Yamakage M, Iwasaki S, Mizuuchi M, Namiki A. Design of oxygen delivery systems influences both effectiveness and comfort in adult volunteers. Can J Anaesth. 2003;50:1052–5. doi: 10.1007/BF03018373. [DOI] [PubMed] [Google Scholar]
- 6.Dinesen T, McDonald L, McDonald S, DuVall D. A comparison of the OxyArm oxygen delivery device and standard nasal cannulae in chronic obstructive pulmonary disease patients. Respir Care. 2003;48:120–3. [PubMed] [Google Scholar]
- 7.Cohn M. Respiratory monitoring during sleep: Respiratory inductive plethysmography. In: Guilleminault C, editor. Sleeping and Waking Disorders: Indications and Techniques. Melo Park: Addison-Wesley Publishing Co; 1982. pp. 213–23. [Google Scholar]
- 8.Noguchi T, Shiga Y, Koga K. Use of the OxyArm in a patient suffering from trigeminal neuralgia. Can J Anaesth. 2004;51:193–4. doi: 10.1007/BF03018793. [DOI] [PubMed] [Google Scholar]
- 9.Fleischhackl R, Dorner C, Scheck T, et al. Reduction of motion sickness in prehospital trauma care. Anaesthesia. 2003;58:373–7. doi: 10.1046/j.1365-2044.2003.03082_4.x. [DOI] [PubMed] [Google Scholar]
- 10.Cohen JL, Demers RR, Saklad M. Air-entrainment oxygen masks: A performance evaluation. Respir Care. 1977;22:277–82. [PubMed] [Google Scholar]
- 11.Campbell EJ. A method of controlled oxygen administration which reduces the risk of carbon-dioxide retention. Lancet. 1960;2:12–4. doi: 10.1016/s0140-6736(60)92660-x. [DOI] [PubMed] [Google Scholar]