Abstract
California’s IMPACT program provides all its enrollees with health insurance and social service resources. We hypothesized that racial/ethnic disparities in access to care might be attenuated among men served by this program. Our objective was to evaluate racial/ethnic differences in health services utilization and patient-reported health care outcomes among disadvantaged men in a prostate cancer public-assistance program, and to identify modifiable factors that might explain persistent disparities in this health care setting. We performed a retrospective cohort study of 357 low-income men enrolled in IMPACT from 2001 through 2005. We evaluated realized access to care with two health services utilization measures: (1) use of emergency department care without hospitalization and, (2) frequency of prostate-specific antigen testing. We also measured two patient-experience outcomes: (1) satisfaction with care received from IMPACT, and (2) confidence in IMPACT care providers. We observed significant bivariate associations between race/ethnicity and patient-experience outcomes (p<0.05), but not utilization measures. In multivariable models, Hispanic men were more likely than white men to report complete satisfaction with health care received in IMPACT (adjusted OR=5.15, 95% CI 1.17-22.6); however, the association between race/ethnicity and satisfaction was not statistically significant (p=0.11). Language preference and self-efficacy in patient-physician interactions are potentially-modifiable predictors of patient-experience outcomes. We observed no racial/ethnic disparities in health services utilization among disadvantaged men served by a disease-specific public assistance program. The greater satisfaction and confidence among Hispanic men are explained by modifiable variables that suggest avenues for improvement.
Keywords: Prostate cancer, Low-income, Uninsured, Race/ethnicity, Disparities, Public assistance, self-efficacy
Introduction
Access to health care reflects not only the potential for entry into the health care system, but also the consumption of services and associated outcomes. Adequate access requires more than a guarantee of payment for services; even with generous benefits, individuals must navigate non-financial barriers.[1-3] Among these are minority status[1,3,4]; environmental factors[5]; health behaviors [6]; acculturation, language, and citizenship[7-9]; provider proximity[10]; available safety-net services[5]; and the absence of a usual source of care[11].
In this context, differential access to care has been proposed as an important determinant of racial/ethnic disparities in prostate cancer screening, treatment, morbidity and mortality.[1,12-14] This is supported by empirical data demonstrating that African-American men with prostate cancer are more likely than whites to be uninsured; to receive their usual medical care in a public clinic or emergency department; and to see different clinicians on subsequent prostate cancer-related visits.[12] Likewise, discrepancies in accessibility and continuity of medical care may explain the lower use and awareness of prostate specific antigen (PSA) testing among Hispanic men in the United States;[15,16] it remains unknown whether access or continuity issues mediate the greater dissatisfaction with prostate cancer treatment decisions among Hispanic men.[17]
California’s IMPACT (Improving Access, Counseling and Treatment for Californians with Prostate Cancer) program seeks to reduce disparities by addressing financial and non-financial impediments to accessing prostate cancer care. Initiated in 2001, IMPACT provides free and comprehensive prostate cancer treatment to uninsured men with incomes under 200% of the Federal Poverty Level. This coverage enables the receipt of previously unattainable medical care. In addition to insurance benefits, each IMPACT enrollee is assigned a primary cancer care provider in his community and to a clinical care coordinator who provides case management and system advocacy. Jointly, the treating physician and clinical care coordinator serve as a usual source of care. Program architects supplemented the insurance benefit with an enabling set of social service resources designed to eliminate residual access barriers. These resources include counseling and interpreter services; culturally-competent, literacy-sensitive educational materials; transportation assistance; food security; and housing referrals. Accordingly, the population served by IMPACT provides a “laboratory” for studying access to care in a public-assistance program that provides health insurance, as well as resources aimed at dismantling non-financial barriers.
In the current study, we evaluated the extent of racial/ethnic disparities in health services utilization (i.e., realized access to prostate cancer care) and patient-reported health care outcomes (e.g., patient satisfaction) among IMPACT enrollees, who are provided with insurance coverage, a usual source of cancer care, and broad psychosocial benefits. Moreover, we sought to identify potentially mutable factors that might explain any observed racial/ethnic disparities.
Methods
Analytic framework and hypotheses
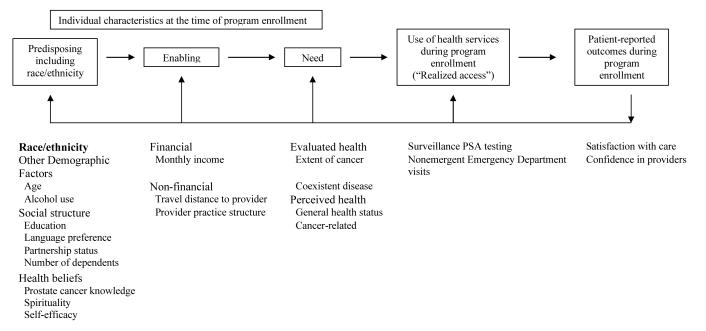
Our conceptual model emanates from the Behavioral Model of Health Services Utilization (Figure 1).[18] The Behavioral Model proposes that utilization (reflecting realized access to care) is determined by predisposing characteristics of individuals and their environments (i.e., predisposing characteristics); factors that enable or impede utilization (i.e., enabling characteristics); and perceived and/or evaluated need for health services (i.e., need characteristics). Utilization, in turn, influences biological and psychosocial outcomes. Moreover, the model is dynamic with health outcomes “feeding back” to influence predisposition to use medical services (including health behaviors), enabling resources, need for care, and utilization.[18] (Figure 1)
Figure 1. Analytic framework.
Application of the Behavioral Model to men enrolled in California’s IMPACT program
Predisposing characteristics exist before a patient’s perception of illness and predict utilization of health services. These include demographic traits, social structure, and health beliefs.[18,19] Enabling factors include personal or environmental resources that facilitate or hinder health care utilization.[18,19] Need variables include both self-assessed (i.e., perceived) and medically-determined (i.e., evaluated) measures of illness severity, including its functional consequences.[18,19]
Racial and/or ethnic minority status is a predisposing characteristic that is consistently associated with less-frequent receipt of necessary health services and adverse health outcomes.[2,3,12,14,15,20] Such disparities often reflect racial/ethnic differences in the distribution of enabling resources (e.g., medical insurance).[1,21] IMPACT provides all enrollees with an equivalent package of enabling resources including disease-specific health insurance; usual source of care; counseling and interpreter services; culturally-competent, literacy-sensitive educational materials; transportation assistance; food security; and housing referrals. Accordingly, we hypothesized that racial/ethnic disparities would be attenuated in this population. We tested this hypothesis by examining racial/ethnic differences in health services utilization and patient outcomes (e.g., satisfaction with care), adjusting for other predisposing, enabling and need factors.
We measured race/ethnicity and other predisposing, enabling, and need variables at the time of program admission. We then assessed health services utilization and patient experiences with care received. In the event that we observed racial/ethnic disparities in utilization or patient experiences, we decided a priori to perform additional analyses evaluating the degree to which other measured (and potentially modifiable) variables explain observed associations with race/ethnicity.
Study sample
IMPACT eligibility requirements include California residency, biopsy-proven prostate cancer, lack of health insurance, and a household income at or below 200% of the Federal Poverty Level. Enrollees are invited to participate in an independent research study. The University of California, Los Angeles Human Subjects Committee approved all consent and data collection protocols, and all are HIPAA compliant.
Consenting participants complete a questionnaire at three points — upon enrollment, after 6 months of program participation, and at disenrollment. The questionnaire includes validated instruments that measure health status, health behaviors, health-related quality of life (HRQOL), self-efficacy in patient-physician interactions, prostate cancer knowledge, and satisfaction with care.
From IMPACT’s inception in 2001 through June 30, 2005, 638 men enrolled in the clinical program. Among these, 437 (68% of clinical program participants) consented to participate in the study and completed a questionnaire at enrollment (“enrollment questionnaire”); 357 and 256 study participants, respectively, completed questionnaires at approximately 6 months after enrollment (“follow-up questionnaire”) and upon program exit. Our analytic sample included all men who completed enrollment and follow-up questionnaires.
Measures
Predisposing variables
We measured predisposing characteristics at the time of program enrollment. In addition to self-reported race/ethnicity, we measured age and alcohol use; four social structural variables (educational attainment, language preference, partnership status, and number of dependents); and three health belief domains (self-efficacy, spirituality, prostate cancer knowledge) (Appendix 1).
We measured self-efficacy [22] in patient-physician interactions (perceived self-efficacy in obtaining medical information and physicians’ attention to medical concerns) with the five-item Perceived Efficacy in Patient-Physician Interactions Questionnaire (PEPPI).[23] The PEPPI is a valid and reliable self-reported measure of self-efficacy in interacting with physicians. Responses are summed, with higher scores reflecting higher self-efficacy. We refer to this measure generically as “self-efficacy.”
We assessed spirituality using the Functional Assessment of Chronic Illness Therapy — Spiritual Well-Being (FACIT-Sp),[24] a self-reported 12-item scale that measures harmony, peacefulness, and a sense of strength and comfort from one’s faith.[24] FACIT-Sp scores range from 0 to 48, with higher scores reflecting greater spirituality.
We evaluated participants’ prostate cancer knowledge using a 14-item, self-administered, true-false questionnaire.[25] Collectively, the items assess knowledge domains of prostate location, function, nutrition, treatment outcomes, and treatment side effects.
Enabling variables
In the Behavioral Model, enabling factors are resources and/or behaviors that facilitate or impede the use of health services.[18] For the current study, we considered IMPACT enrollees to have equal insurance, a usual source of care, and equivalent program-related social service resources. We additionally measured one financial (any vs no monthly income) and two non-financial (travel distance to primary provider, public vs private ownership of primary provider practice) enabling factors. We determined travel distance (number of miles from a patient’s home address to his usual IMPACT provider’s primary office) using web-based mapping software. We empirically defined travel distance as ≤10 or >10 miles.[10] We specified primary IMPACT provider practice structure as either public (county hospital) or private (academic or community private practice).[26]
Need-related variables
We measured perceived need based on self-reported general health status and cancer-related symptoms and distress. For general health status, we used the RAND Medical Outcomes Study Short Form-12 (SF-12, version 2).[27] This 12-item adaptation of the RAND 36-Item Health Survey quantifies HRQOL in two composite scores, the Physical (PCS) and Mental (MCS) Component Summary scales. The scales are transformed to a normative score with a population mean of 50 and standard deviation of 10.
We used McCorkle and Young’s Symptoms and Degrees of Distress in Patients with Cancer Scale (SDS) to measure the degree of distress perceived by patients for cancer-related symptoms.[28] The 10 item responses are summed, with higher scores indicating more distress.
For each subject in the analytic cohort, we reviewed the IMPACT clinical database to ascertain the date of diagnosis, clinical parameters at enrollment (e.g., PSA level, Gleason score), and treatment information. We estimated evaluated need for prostate cancer services based on the extent of each subject’s tumor at the time of program enrollment. Using established clinical and pathological variables, we assigned each patient to 1 of 4 cancer severity categories: (1) localized; (2) regional; (3) metastatic; (4) recurrent following primary therapy.[29] We collapsed the latter two categories for multivariable analyses. We specified each patient’s burden of coexistent illness— measured by the Charlson Comorbidity Index—as an additional measure of evaluated need.[30]
Health services utilization and patient-experience outcome variables
We defined utilization measures that (1) broadly assessed adequacy of realized access to necessary prostate cancer care during program enrollment, and (2) were applicable to all members of our clinically-heterogeneous cohort. In this context, we constructed two health services utilization variables (measured over the entire period of program enrollment): (1) use of emergency department (ED) care without subsequent hospitalization; and (2) frequency of surveillance PSA testing. We refer to these as the “nonemergent ED utilization” and “PSA testing” measures, respectively; collectively, we refer to these two variables as “utilization measures.” In our conceptual model, the utilization measures reflect realized access to care in the IMPACT program (Figure 1).
Even in the advanced stages of disease, patients with good continuity of ambulatory prostate cancer care should rarely require ED visits for nonemergent indications. We therefore defined men who had one or more ED visits—without hospitalization—as having inadequate access to care during program enrollment.[31] This utilization measure has been employed previously to evaluate access to care for other chronic medical conditions.[31]
The second utilization measure reflects use of PSA as a surveillance test following prostate cancer diagnosis and/or treatment. Although IMPACT enrollees are heterogeneous with respect to factors determining the optimal PSA-testing interval, prostate cancer patients with good access to care undergo surveillance PSA testing at least every 6 months.[32] We therefore determined the proportion of 6-month enrollment intervals during which each patient received a PSA test (allowing a 1-month window for scheduling fluctuations). Based on the distribution of the PSA testing variable, we empirically (and a priori) defined men with PSA tests in >60% of eligible 6-month intervals (72% of sample) as having adequate access to IMPACT services.
We retrospectively ascertained data for the utilization measures from IMPACT’s electronic clinical records. Two authors (DCM, SS) used an algorithm to determine the dates for all PSA tests and the occurrence (or absence) of nonemergent ED utilization during the entire period of program enrollment. Inter-rater agreement for PSA test dates exceeded 80% in a 10% validation sample.
We also defined two patient-experience outcomes: satisfaction with care received from IMPACT and confidence in IMPACT health care providers. We refer to these as the “satisfaction” and “confidence” outcomes, respectively; collectively, we refer to these as “patient-experience outcomes.”
We measured the satisfaction and confidence outcomes based on responses to the following items in the 6-month follow-up questionnaire: (1) “I am satisfied with the health care I have been receiving;” and (2) “I have an extraordinary amount of confidence in the health care providers I have been seeing.” As an introduction to each item, participants received the following written instructions: “Please respond to the following about the health care services you received from IMPACT during the past 3 months, on a scale from 1 to 6, where 1 is definitely yes and 6 is definitely no.”
Based on the distribution of responses for the patient-experience outcomes, we empirically classified patients answering “definitely yes” as completely satisfied (confident) and all others as incompletely satisfied (confident) (Appendix 1).
Statistical analyses
We performed bivariate analyses to identify associations between race/ethnicity and utilization measures or patient-experience outcomes. Likewise, we evaluated bivariate associations for other measured predisposing, enabling, and need variables. We assessed statistical significance using chi-square (categorical variables) and t-tests (continuous variables).
Guided by the bivariate results, we fit multivariable logistic regression models to identify predisposing, enabling, and/or need variables independently associated with health services utilization and/or patient experience in IMPACT. We included in these “fully-adjusted models” all predisposing (including race/ethnicity), enabling, and need variables that had at least marginal bivariate associations (p<0.30) with utilization measures and/or patient-experience outcomes.
Because significant bivariate associations (p<0.05) between race/ethnicity and patient-experience outcomes disappeared in the fully-adjusted models, we performed a series of sensitivity analyses to identify potential explanatory variables for the effect of race/ethnicity on patient perceptions of care (Appendix 2). In the fully-adjusted models, we noted mild collinearity between perceived need variables; we did not exclude these from the final models. All statistical testing was two-sided, completed using computerized software (SAS v9.1, SAS Institute, Cary, NC), and carried out at the 5% significance level.
Results
Our analytic sample includes 357 men who completed enrollment and follow-up questionnaires (82% of study participants)
Two-thirds were ≤65 years old at enrollment; two-thirds had PSA values <10 ng/mL; half had Gleason scores ≤6; and half had clinically-localized cancers. Median duration of program enrollment was 18.7 months (range 3.7–42.9 months). The sample was 55% Hispanic, 17% African-American, and 22% Non-Hispanic white (Table 1). During program enrollment, 18% of men had nonemergent ED utilization and 28% had inadequate surveillance PSA testing. At a median of 8 months after enrollment (the average time from enrollment to completion of the follow-up questionnaire), 22% and 33%, respectively, reported incomplete satisfaction with health care provided and incomplete confidence in their IMPACT provider(s). Table 1 also presents the distribution of other predisposing, enabling, and need variables.
Table 1.
Bivariate associations between predisposing, enabling and need variables and measures of health services utilization, satisfaction with care provided in IMPACT, and confidence in IMPACT provider
| Utilization Measures (“Realized access”) | Patient-experience Outcomes | ||||
|---|---|---|---|---|---|
| n (%) | No non-emergent ED visits (%) |
Adequate surveillance PSA testing (%) |
Completely satisfied with health care provided by IMPACT (%) |
Complete confidence in IMPACT health care providers (%) |
|
| OVERALL | 357 | 81.8 | 71.6 | 77.9 | 66.9 |
|
| |||||
| PRIMARY COVARIATE | |||||
|
| |||||
| Self-reported race/ethnicity | ** | * | * | ||
|
|
|||||
| Non-hispanic, White | 79 (22.1) | 84.8 | 80.6 | 67.1 | 56.2 |
|
| |||||
| Hispanic | 195 (54.6) | 84.1 | 77.4 | 84.3 | 73.8 |
|
| |||||
| African-American | 61 (17.1) | 72.1 | 72.2 | 76.5 | 64.7 |
|
| |||||
| Other | 22 (6.2) | 77.3 | 84.2 | 66.7 | 52.4 |
|
| |||||
|
OTHER PREDISPOSING
VARIABLES |
|||||
|
| |||||
| Age at enrollment | ** | * | |||
|
|
|||||
| < 50 years | 9 (2.5) | 55.6 | 100.0 | 60.0 | 60.0 |
|
| |||||
| 50-59 years | 83 (23.2) | 85.5 | 73.0 | 78.9 | 67.6 |
|
| |||||
| 60-65 years | 147 (41.2) | 81.0 | 85.8 | 76.5 | 62.9 |
|
| |||||
| 66-70 years | 80 (22.4) | 83.8 | 70.3 | 78.1 | 72.6 |
|
| |||||
| > 70 years | 38 (10.7) | 79.0 | 69.4 | 83.3 | 69.4 |
|
| |||||
|
Alcohol use as reported at the time of program enrollment a |
** | ||||
|
|
|||||
| 0-1 drink/day | 288 (81.3) | 81.1 | 80.1 | 77.0 | 65.7 |
|
| |||||
| ≥ 2 drinks/day | 66 (18.7) | 83.2 | 71.3 | 80.5 | 70.1 |
|
| |||||
|
Self-reported educational attainment b |
* | * | |||
|
| |||||
| Less than high school | 153 (44.1) | 81.7 | 76.6 | 85.9 | 75.4 |
|
| |||||
| High school graduate | 71 (20.5) | 80.3 | 74.6 | 80.7 | 67.7 |
|
| |||||
| Some college | 123 (35.4) | 81.3 | 80.4 | 66.4 | 55.8 |
|
| |||||
|
Self-reported language
Preference |
** | * | * | ||
|
|
|||||
| English | 190 (53.2) | 79.0 | 78.8 | 71.8 | 57.7 |
|
| |||||
| Non-English | 167 (46.8) | 85.0 | 76.1 | 85.0 | 77.6 |
|
| |||||
|
Self-reported partnership status c |
* | ** | * | ||
|
|
|||||
| Partnered | 254 (71.4) | 81.5 | 80.5 | 80.5 | 71.0 |
|
| |||||
| Not partnered | 102 (28.6) | 82.4 | 69.9 | 70.9 | 55.8 |
|
| |||||
| Number of dependents | ** | ** | * | ||
|
| |||||
| 0 | 181 (50.7) | 78.5 | 74.3 | 73.1 | 59.6 |
|
| |||||
| 1 | 133 (37.3) | 87.2 | 80.6 | 82.6 | 72.7 |
|
| |||||
| ≥ 2 | 43 (12.0) | 79.1 | 82.1 | 82.5 | 77.5 |
|
| |||||
|
IMPACT Prostate Cancer Knowledge Scale score at enrollment d |
|||||
|
| |||||
| Lowest quartile (0-7) | 76 (22.5) | 82.9 | 73.3 | 82.8 | 71.9 |
|
| |||||
| Top three quartiles (8-14) | 262 (77.5) | 82.1 | 78.2 | 77.0 | 65.7 |
|
| |||||
|
Functional Assessment of Chronic Illness Therapy — Spiritual Well-Being Scale (FACIT-Sp) score at enrollment |
** | ** | * | ||
|
|
|||||
| Lowest quartile (4-33.8) | 91 (25.5) | 80.2 | 75.7 | 72.2 | 54.4 |
|
| |||||
| Top three quartiles (34-48) | 266 (74.5) | 82.3 | 78.2 | 79.8 | 71.0 |
|
| |||||
|
Perceived Efficacy in Patient-Physician Interactions (PEPPI) scale score at enrollment e |
* | * | |||
|
|
|||||
| Lowest tercile (5-20) | 112 (34.3) | 83.0 | 78.4 | 65.3 | 48.0 |
|
| |||||
| Middle tercile (21-24) | 84 (25.7) | 82.1 | 75.7 | 77.2 | 67.1 |
|
| |||||
| Highest tercile (25) | 131 (40.1) | 79.4 | 77.3 | 90.0 | 83.3 |
|
| |||||
| ENABLING VARIABLES | |||||
|
| |||||
|
Self-reported personal
Monthly income |
* | ||||
|
|
|||||
| None | 88 (24.6) | 83.0 | 80.7 | 76.6 | 67.8 |
|
| |||||
| Any | 269 (75.4) | 81.4 | 68.4 | 82.1 | 64.1 |
|
| |||||
|
Travel distance to primary
IMPACT provider (via existing roadways) |
** | ||||
|
| |||||
| ≤ 10 miles | 226 (63.3) | 80.1 | 77.4 | 81.1 | 66.7 |
|
| |||||
| > 10 miles | 131 (36.7) | 84.7 | 77.9 | 72.4 | 67.2 |
|
| |||||
|
Practice setting of primary
IMPACT provider |
* | ||||
|
|
|||||
| Academic or community Private practice |
152 (42.6) | 82.9 | 83.5 | 77.6 | 68.7 |
|
| |||||
| Public (County) hospital | 205 (57.4) | 81.0 | 73.3 | 78.1 | 65.6 |
|
| |||||
| NEED VARIABLES | |||||
|
| |||||
| Evaluated need | |||||
|
| |||||
|
Extent of cancer at enrollment f |
* | * | ** | ||
|
|
|||||
| Localized | 195 (55.4) | 86.2 | 76.1 | 79.8 | 68.2 |
|
| |||||
| Regional | 80 (22.7) | 85.0 | 67.2 | 83.6 | 71.2 |
|
| |||||
| Metastatic | 65 (18.5) | 67.7 | 91.2 | 67.2 | 63.8 |
|
| |||||
| Recurrent cancer following Primary therapy |
12 (3.4) | 75.0 | 83.3 | 72.7 | 45.5 |
|
| |||||
|
Charlson Comorbidity Index score g |
|||||
|
|
|||||
| 0-1 | 248 (74.7) | 80.7 | 78.9 | 79.6 | 67.7 |
|
| |||||
| ≥ 2 | 84 (25.3) | 86.9 | 78.2 | 71.8 | 65.4 |
|
| |||||
| Perceived need | |||||
|
| |||||
| General health status |
Overall
sample mean (SD) |
Mean score
among cases with outcome |
Mean score among
cases with outcome |
Mean score among cases
with outcome |
Mean score among cases
with outcome |
|
| |||||
| RAND SF-12 Physical Component Summary score (potential range 0-100) h |
45.7 (11.6) | 46.1 (11.6) †† | 46.4 (11.3) †† | 45.9 (11.8) | 46.3 (11.6) |
|
| |||||
| RAND SF-12 Mental Component Summary score (potential range 0-100) i |
42.7 (7.9) | 43.1 (7.7) †† | 42.8 (8.0) | 43.3 (7.6) †† | 43.7 (7.3) † |
|
| |||||
|
Cancer-related symptoms
and distress |
|||||
|
| |||||
| Symptoms and Degrees of Distress in Patients with Cancer Scale (SDSS) (potential range 10-50) j |
19.9 (7.1) | 19.6 (6.9) †† | 19.9 (7.3) | 18.8 (6.8) † | 18.7 (6.9) † |
3 cases with missing data for alcohol use
10 cases with missing data for education
1 case with missing data for partnership status
19 cases with missing data for IMPACT prostate cancer knowledge scale score at enrollment
30 cases with missing data for PEPPI (self-efficacy) score at enrollment
5 cases with missing data for extent of cancer at the time of program enrollment
25 cases with missing data for Charlson Index score
14 cases with missing data for SF-12 PCS score at the time of program enrollment
14 cases with missing data for SF-12 MCS score at the time of program enrollment
27 cases with missing data for symptoms and distress at the time of program enrollment
p<0.05, χ2 test of general association
p<0.30, χ2 test of general association
Values for cases with outcome specified by column heading significantly different those for cases without specified outcome (p<0.05), two-sample t-test. For the statistically significant comparisons, the values for the comparison groups are as follows: Mean RAND SF-12 Mental Component Summary score for men reporting incomplete confidence in IMPACT health care providers = 41.0; Mean Symptoms and Degrees of Distress in Patients with Cancer Scale score for men reporting incomplete satisfaction with health care provided by IMPACT = 22.6; Mean Symptoms and Degrees of Distress in Patients with Cancer Scale score for men reporting incomplete confidence in IMPACT health care providers = 21.6
p-values <0.30 for cases with outcome specified by column heading, two-sample t-test.
We observed significant bivariate associations between race/ethnicity and patient-experience outcomes (p<0.05), but not utilization measures (Table 1). This reflects the finding that more Hispanic and African-American men than white men reported complete satisfaction with health care received in IMPACT and complete confidence in their IMPACT provider(s).
Table 2 summarizes results from the fully-adjusted multivariable models. We observed no independent associations between race/ethnicity and utilization measures. Non-partnered men (adjusted odds ratio (OR) = 0.49, 95% CI 0.25–0.97), and those consuming 2 or more alcoholic drinks daily (adjusted OR= 0.44, 95% CI 0.22–0.87), were less likely to receive adequate surveillance PSA testing. Conversely, those with metastatic or recurrent cancer were more likely to access surveillance PSA tests regularly (adjusted OR=4.20, 95% CI 1.59–11.1). None of the predisposing, enabling, or need variables was independently associated with nonemergent ED utilization (Table 2).
Table 2.
Multivariable associations with measures of health services utilization, satisfaction with care provided in IMPACT, and confidence in IMPACT provider
| Characteristics | Utilization Measures (“Realized access”) | Patient-experience Outcomes | ||
|---|---|---|---|---|
| No non-emergent ED visits |
Adequate surveillance PSA testing |
Completely satisfied with health care provided by IMPACT |
Complete confidence in IMPACT health care providers |
|
| PRIMARY COVARIATE | ||||
|
| ||||
| Self-reported race/ethnicity | ||||
|
|
||||
| Non-hispanic, White | 1.00 | 1.00 | 1.00 | 1.00 |
|
| ||||
| Hispanic | 0.65 (0.19-2.23) | 0.90 (0.36-2.27) | 5.15 (1.17-22.6) | 0.83 (0.29-2.37) |
|
| ||||
| African-American | 0.43 (0.16-1.13) | 0.74 (0.28-2.01) | 1.54 (0.51-4.62) | 0.85 (0.34-2.14) |
|
| ||||
| Other | 1.03 (0.23-4.62) | 2.24 (0.37-13.72) | 0.60 (0.16-2.22) | 0.61 (0.17-2.13) |
|
| ||||
|
OTHER PREDISPOSING
VARIABLES |
||||
|
| ||||
| Age at enrollment | ||||
|
|
||||
| < 60 years | 1.0 | 1.0 | 1.0 | 1.0 |
|
| ||||
| 60-69 years | 0.51 (0.22-1.20) | 2.23 (0.90-5.55) | 0.85 (0.37-1.98) | 0.75 (0.35-1.60) |
|
| ||||
| 70-79 years | 0.63 (0.26-1.52) | 0.92 (0.42-2.03) | 1.29 (0.52-3.24) | 1.03 (0.47-2.24) |
|
| ||||
| > 80 years | 0.48 (0.14-1.58) | 1.00 (0.32-3.16) | 1.26 (0.35-4.57) | 0.67 (0.23-1.96) |
|
| ||||
|
Alcohol use as reported at
the time of program enrollment |
* | |||
|
|
||||
| 0-1 drink/day | — | 1.00 | — | — |
|
| ||||
| ≥ 2 drinks/day | — | 0.44 (0.22-0.87) | — | — |
|
| ||||
|
Self-reported educational
attainment |
||||
|
|
||||
| Less than high school | — | — | 2.13 (0.88-5.18) | 1.89 (0.89-4.03) |
|
| ||||
| High school graduate | — | — | 1.60 (0.63-4.07) | 1.45 (0.65-3.22) |
|
| ||||
| Some college | — | — | 1.00 | 1.00 |
|
| ||||
|
Self-reported language
preference |
||||
|
|
||||
| English | 1.00 | — | 1.00 | 1.00 |
|
| ||||
| Non-English | 1.61 (0.52-5.00) | — | 0.30 (0.06-1.39) | 1.39 (0.48-4.03) |
|
| ||||
|
Self-reported partnership
status |
* | |||
|
|
||||
| Partnered | — | 1.00 | 1.00 | 1.00 |
|
| ||||
| Not partnered | — | 0.49 (0.25-0.97) | 0.88 (0.38-2.06) | 0.66 (0.32-1.36) |
|
| ||||
| Number of dependents | ||||
|
|
||||
| 0 | 1.00 | — | 1.00 | 1.00 |
|
| ||||
| 1 | 1.72 (0.79-3.72) | — | 0.96 (0.41-2.25) | 1.12 (0.55-2.28) |
|
| ||||
| ≥ 2 | 0.66 (0.24-1.78) | — | 1.22 (0.33-4.47) | 2.43 (0.75-7.88) |
|
| ||||
|
Functional Assessment of Chronic Illness Therapy — Spiritual Well-Being Scale (FACIT-Sp) score at enrollment |
||||
|
|
||||
| Lowest quartile (4-33.8) | — | — | 1.60 (0.69-3.69) | 1.23 (0.60-2.51) |
|
| ||||
| Top three quartiles (34-48) | — | — | 1.00 | 1.00 |
|
| ||||
|
Perceived Efficacy in
Patient-Physician Interactions (PEPPI) scale score at enrollment e |
* | * | ||
|
|
||||
| Lowest tercile (5-20) | — | — | 0.30 (0.13-0.70) | 0.24 (0.12-0.48) |
|
| ||||
| Middle tercile (21-24) | — | — | 0.48 (0.20-1.17) | 0.47 (0.22-0.98) |
|
| ||||
| Highest tercile (25) | — | — | 1.00 | 1.00 |
|
| ||||
| ENABLING VARIABLES | ||||
|
| ||||
|
Self-reported personal
monthly income |
||||
|
|
||||
| None | — | 1.00 | — | — |
|
| ||||
| Any | — | 0.54 (0.25-1.15) | — | — |
|
| ||||
|
Travel distance to primary
IMPACT provider (via existing roadways) |
||||
|
|
||||
| ≤ 10 miles | 1.00 | — | 1.00 | — |
|
| ||||
| > 10 miles | 0.83 (0.43-1.60) | — | 0.69 (0.35-1.37) | — |
|
| ||||
|
Practice setting of primary
IMPACT provider |
||||
|
|
||||
| Academic or community private practice |
— | 1.00 | — | — |
|
| ||||
| Public (County) hospital | — | 0.56 (0.28-1.12) | — | — |
|
| ||||
| NEED VARIABLES | ||||
|
| ||||
| Evaluated need | ||||
|
| ||||
|
Extent of cancer at
enrollment |
* | |||
|
|
||||
| Localized | 1.00 | 1.00 | 1.00 | — |
|
| ||||
| Regional | 1.01 (0.44-2.35) | 0.78 (0.36-1.66) | 1.31 (0.55-3.14) | — |
|
| ||||
| Metastatic or recurrent cancer following primary therapy |
0.47 (0.22-0.98) | 4.20 (1.59-11.1) | 0.46 (0.21-1.02) | — |
|
| ||||
|
Charlson Comorbidity Index
Score |
||||
|
|
||||
| 0-1 | 1.00 | — | 1.00 | — |
|
| ||||
| ≥ 2 | 1.78 (0.83-3.82) | — | 0.64 (0.31-1.32) | — |
|
| ||||
| Perceived need | ||||
|
| ||||
| General health status | ||||
|
|
||||
| RAND SF-12 Physical Component Summary score |
1.00 (0.97-1.04) | 1.02 (1.00-1.05) | — | — |
|
| ||||
| RAND SF-12 Mental Component Summary score |
1.03 (0.99-1.07) | — | 1.03 (0.98-1.07) | 1.04 (1.00-1.08) |
|
| ||||
|
Cancer-related symptoms
and distress |
* | |||
|
|
||||
| Symptoms and Degrees of Distress in Patients with Cancer Scale (SDSS) |
1.00 (0.95-1.05) | — | 0.94 (0.89-0.99) | 0.97 (0.93-1.02) |
p<0.05 for overall variable effect in multivariable models
Hispanic men were more likely than white men to report complete satisfaction with health care received in IMPACT (adjusted OR=5.15, 95% CI 1.17–22.6); however, the overall association between race/ethnicity and satisfaction was not statistically significant (p=0.11). Likewise, multivariable analysis did not reveal a significant association between race/ethnicity and confidence in IMPACT provider(s) (Table 2).
Self-efficacy was independently associated with both patient-experience outcomes (Table 2). Compared with men with the highest self-efficacy, those with the lowest had 70% (adjusted OR= 0.30, 95% CI 0.13–0.70) lower odds of being completely satisfied with their care and 76% (adjusted OR=0.24, 95% CI 0.12–0.48) lower odds of being completely confident in their provider. We observed a small—but significant—inverse association between cancer-related symptoms and distress and satisfaction with care (adjusted OR=0.94, 95% CI 0.89–0.99) (Table 2).
In sensitivity analyses, we identified 2 potentially-modifiable explanatory variables for the associations between race/ethnicity and patient-experience outcomes (Table 3): language preference and self-efficacy. The higher levels of satisfaction among Hispanic men were consistent across language preference categories (data not shown); conversely, the higher levels of confidence among Hispanic men were concentrated among those who preferred Spanish (77% vs 54%).
Table 3.
Sensitivity analyses to identify explanatory variables for associations between race/ethnicity and patient-experience outcomes†
| Model | Self-reported race/ethnicity ‡ | Odds ratio for complete satisfaction with health care provided in IMPACT (95% CI) |
Odds ratio for complete confidence in IMPACT provider (95% CI) |
|---|---|---|---|
| * | * | ||
| Unadjusted models | Hispanic | 2.83 (1.43 – 5.57) | 2.07 (1.14 -3.75) |
| (Appendix 2, Models 2.1 and 2.2) | African-American | 1.59 (0.66 – 3.82) | 1.27 (0.58– 2.76) |
| Other race/ethnicity | 0.66 (0.22 – 2.00) | 0.73( 0.24- 2.16) | |
| Fully-adjusted models a | Hispanic | 5.15 (1.17-22.5) | 0.83 (0.29-2.37) |
| (Appendix 2, Models 2.3 and 2.4) | African-American | 1.54 (0.51-4.62) | 0.85 (0.34-2.14) |
| Other race/ethnicity | 0.60 (0.16-2.22) | 0.61 (0.17-2.13) | |
|
Models evaluating classes of
explanatory or intervening variables |
|||
|
Adjusting only for predisposing variables included in fully-adjusted models b |
Hispanic | 3.22 (0.80 – 12.9) | 0.73 (0.26– 2.06) |
| (Appendix 2, Models 2.5 and 2.6) | African-American | 1.07 (0.40 – 2.85) | 0.76 (0.31- 1.87) |
| Other race/ethnicity | 0.48 (0.14 – 1.67) | 0.57 (0.16- 1.98) | |
| * | |||
|
Adjusting only for enabling variables included in fully-adjusted models c |
Hispanic | 2.68 (1.35 – 5.34) | N/A |
| (Appendix 2, Model 2.7) | African-American | 1.51 (0.62 – 3.66) | N/A |
| Other race/ethnicity | 0.66 (0.22 – 2.00) | N/A | |
| * | * | ||
|
Adjusting only for need-related variables included in fully-adjusted models d |
Hispanic | 3.50 (1.69 – 7.24) | 2.15 (1.16- 3.97) |
| (Appendix 2, Models 2.8 and 2.9) | African-American | 2.23 (0.85 – 5.86) | 1.39 (0.61- 3.14) |
| Other race/ethnicity | 0.74 (0.23 – 2.41) | 0.76 (0.25- 2.32) | |
|
Models evaluating specific (individual) explanatory variables § |
|||
| Adjusting only for educational | Hispanic | 2.06 (0.94– 4.48) | 1.41 (0.71 -2.80) |
| attainment | |||
| (Appendix 2, Models 2.12 and 2.13) | African-American | 1.33 (0.53 – 3.31) | 1.01 (0.45- 2.28) |
| Other race/ethnicity | 0.65 (0.21-1.99) | 0.70 (0.23- 2.12) | |
|
Adjusting only for language
preference |
Hispanic | 3.24 (0.86 – 12.1) | 0.86 (0.34- 2.18) |
| (Appendix 2, Models 2.14 and 2.15) | African-American | 1.59 (0.66 – 3.82) | 1.27 (0.58- 2.76) |
| Other race/ethnicity | 0.66 (0.22 – 2.00) | 0.72 (.0.24- 2.16) | |
| * | |||
|
Adjusting only for partnership
status |
Hispanic | 2.66 (1.32 – 5.35) | 1.79 (0.96- 3.31) |
| (Appendix 2, Models 2.16 and 2.17) | African-American | 1.55 (0.64 – 3.73) | 1.19 (0.54- 2.62) |
| Other race/ethnicity | 0.64 (0.21 – 1.95) | 0.67 (0.22– 2.02) | |
| * | |||
|
Adjusting only for number of
dependents |
Hispanic | 2.60 (1.30 – 5.23) | 1.76 (0.95- 3.25) |
| (Appendix 2, Models 2.18 and 2.19) | African-American | 1.63 (0.67 – 3.94) | 1.32 (0.60- 2.91) |
| Other race/ethnicity | 0.64 (0.21 – 1.96) | 0.65 (0.21- 2.00) | |
| * | |||
| Adjusting only for spirituality | Hispanic | 2.63 (1.31 – 5.27) | 1.78 (0.96- 3.30) |
| (Appendix 2, Models 2.20 and 2.21) | African-American | 1.50 (0.62 – 3.64) | 1.12 (0.51- 2.47) |
| Other race/ethnicity | 0.61 (0.20 – 1.88) | 0.62 (0.20- 1.87) | |
| * | |||
| Adjusting only for self-efficacy | Hispanic | 2.17 (1.08 – 4.39) | 1.55 (0.83- 2.93) |
| (Appendix 2, Models 2.22 and 2.23) | African-American | 1.23 (0.39 – 4.05) | 0.91 (0.40- 2.07) |
| Other race/ethnicity | 0.58 (0.18 – 1.86) | 0.65 (0.20- 2.06) |
satisfaction model adjusts for age at enrollment, educational attainment, language preference, partnership status, number of dependants, spirituality, self-efficacy, travel distance, extent of cancer, Charlson comorbidity index score, general mental health status, and cancer-related symptoms and distress (each of these variables was at least marginally associated (p<0.30) with satisfaction in bivariate analyses); confidence model adjusts for age at enrollment, educational attainment, language preference, partnership status, number of dependants, spirituality, self-efficacy, general mental health status, and cancer-related symptoms and distress (each of these variables was at least marginally associated (p<0.30) with confidence in bivariate analyses)
satisfaction model adjusts for age at enrollment, educational attainment, language preference, partnership status, number of dependants, spirituality, and self-efficacy; confidence model adjusts for age at enrollment, educational attainment, language preference, partnership status, number of dependants, spirituality, self-efficacy
satisfaction model adjusts for travel distance; confidence model: no enabling variables were marginally associated (p<0.30) with confidence in bivariate analyses
satisfaction model adjusts for extent of cancer, Charlson comorbidity index score, general mental health status, and cancer-related symptoms and distress; confidence model adjusts for general mental health status, and cancer-related symptoms and distress
Results for explanatory variables are presented in bold font.
Reference group = non-Hispanic, whites
When adjustment for an individual variable rendered the association with race/ethnicity non-statistically significant, we defined that variable as an explanatory variable for the association between race/ethnicity and the outcome variable (either satisfaction or confidence). Results for potential explanatory variables are presented in bold font. Data for models adjusting only for age (Appendix 2, Models 2.10 and 2.11) not shown
p< 0.05 for association between race/ethnicity and outcome variable, adjusting for all other variables in a given model (i.e., p-value for the type III race effect)
Our principal findings did not change in analyses that used alternative specifications for the PSA testing and self-efficacy variables.
Discussion
Our principal finding is that prostate cancer health services utilization (i.e., realized access to medical care) is equitable across the diverse racial and ethnic groups served by IMPACT. That the relatively small proportion of men with nonemergent ED visits and inadequate PSA testing did not vary by race/ethnicity may reflect IMPACT’s provision of both financial and non-financial enabling resources. Namely, insurance coverage alone is a necessary but insufficient solution to racial and ethnic disparities in health care utilization and outcomes.[1-3,33,34] Accordingly, the absence of racial/ethnic disparities in realized access among IMPACT participants suggests that furnishing non-insurance-related social services—including a usual source of care, case management, educational resources, and transportation assistance—facilitates racially-equitable health services utilization.
This appealing conclusion is tempered, however, by the absence of a control group. Without this, we cannot determine whether—and to what extent—racial disparities in utilization exist among disadvantaged prostate cancer patients who are not IMPACT-eligible. Nonetheless, existing literature identifies reduced access and continuity as determinants of racial inequities in prostate cancer care;[12] therefore, the absence of utilization disparities among men served by IMPACT is a promising observation that motivates further evaluation of whether public assistance programs that address both financial and non-financial access barriers can ameliorate racial disparities in access to medical care.
Our second principal finding is that, unlike utilization measures, patient-reported outcomes did vary across racial/ethnic groups. Notably, the favorable experience for Hispanic men is explained, in part, by very high satisfaction among Hispanic men who prefer Spanish. To the extent that language preference serves as a proxy for acculturation [7,35], this contrasts with prior research documenting greater dissatisfaction with interpersonal aspects of health care among less-acculturated Latinos in the US.[36,37]
One explanation for this paradox is that IMPACT’s case management, interpreter services, and language-concordant educational materials mitigate the communication deficits that generally yield lower satisfaction among less-acculturated Hispanics.[37,38] In fact, a primary role of IMPACT’s clinical care coordinators is to ensure that enrollees receive adequate answers to their questions, explanations of interventions, and ongoing reassurance and support. Likewise, liberal access to interpreter services and Spanish-language educational materials facilitates clear communication and may also contribute to exceptionally high satisfaction among Spanish-speaking Hispanic men.[8,37]
Alternatively, the greater satisfaction among less-acculturated Hispanic men may reflect differences in expectations. That is, given historical difficulties navigating the US health care system, Spanish-speaking men may have lower expectations. [20] If Spanish-speaking Hispanics had more pessimistic perspectives at enrollment, then they may have had fewer unmet expectations—thus improving satisfaction.[39]
Hispanic men also reported greater confidence in their providers. Like satisfaction, adjusting for language preference partially explained this association, likely because of the confidence-building effects of case management, interpreter services, and language-concordant educational materials.
This finding was also explained by the observation that whites and African-Americans with lower self-efficacy tended to have less confidence in their providers than did Hispanics with similar levels of self-efficacy. Interventions to improve self-efficacy may, therefore, reduce disparities in prostate cancer patient experience outcomes.[40] The feasibility of this approach is supported by interventions that have yielded better patient-physician communication[23], improved glycemic control among diabetics[41], more successful weight loss and smoking cessation programs[42,43], and more informed prostate cancer screening behavior.[44]
Given their tendency to be dissatisfied with prostate cancer treatment decisions,[17] it is encouraging that Hispanic men reported the highest levels of satisfaction and confidence with care provided in IMPACT. The needs of this often difficult-to-reach population appear to be met by the program. While this finding supports the benefits of public programs aimed at improving access for vulnerable populations, further research is needed to fully clarify whether the more favorable outcomes among Hispanics reflect a beneficial effect of program resources, differential expectations for medical care, or both.
Our study has several limitations. First, as is often the case with publicly-funded programs, IMPACT sustained several large budget cuts that forced reductions in the number of enrollees, two prolonged enrollment suspensions, and staffing reductions. The budget cuts also decreased reimbursement, leading many providers to terminate participation. Despite these structural changes, our data provide important context for future studies evaluating the access-related consequences of disease-specific, public assistance programs.
Second, our results are susceptible to omitted-variable bias because we did not measure a number of individual (e.g., mental illness, drug abuse) and contextual (e.g. social networks) variables that may influence access to care among vulnerable populations. Thirds, our patient-experience outcomes and several predictor variables were limited by potential self-report bias. Finally, these data might not be generalizable to prostate cancer patients who were not part of the IMPACT program.
We observed no racial/ethnic disparities in health services utilization among disadvantaged men enrolled in a prostate cancer public-assistance program. The greater satisfaction and confidence among Hispanic men are explained by modifiable predisposing variables, including Spanish language preference and self-efficacy in patient-physician interactions, suggesting possible avenues for correcting the disparities. Future research is needed to characterize more fully the degree to which public-assistance programs provide equitable access to care for individuals and populations who find the US health care system otherwise inaccessible.
References
- 1.Mandelblatt JS, Yabroff KR, Kerner JF. Equitable access to cancer services: A review of barriers to quality care. Cancer. 1999;86:2378–2390. [PubMed] [Google Scholar]
- 2.Institute of Medicine of the National Academies . Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. National Academies Press; Washington D.C.: 2003. [PubMed] [Google Scholar]
- 3.Lurie N, Dubowitz T. Health disparities and access to health. JAMA. 2007;297:1118–1121. doi: 10.1001/jama.297.10.1118. [DOI] [PubMed] [Google Scholar]
- 4.Eisenberg JM, Power EJ. Transforming insurance coverage into quality health care: voltage drops from potential to delivered quality. JAMA. 2000;284:2100–2107. doi: 10.1001/jama.284.16.2100. [DOI] [PubMed] [Google Scholar]
- 5.Davidson PL, Andersen RM, Wyn R, et al. A framework for evaluating safety-net and other community-level factors on access for low-income populations. Inquiry. 2004;41:21–38. doi: 10.5034/inquiryjrnl_41.1.21. [DOI] [PubMed] [Google Scholar]
- 6.Call KT, McAlpine DD, Johnson PJ, et al. Barriers to care among American Indians in public health care programs. Med Care. 2006;44:595–600. doi: 10.1097/01.mlr.0000215901.37144.94. [DOI] [PubMed] [Google Scholar]
- 7.Echeverria SE, Carrasquillo O. The roles of citizenship status, acculturation, and health insurance in breast and cervical cancer screening among immigrant women. Med Care. 2006;44:788–92. doi: 10.1097/01.mlr.0000215863.24214.41. [DOI] [PubMed] [Google Scholar]
- 8.Flores G. Language barriers to health care in the United States. New Engl J Med. 2006;355:229–231. doi: 10.1056/NEJMp058316. [DOI] [PubMed] [Google Scholar]
- 9.De Alba I, Hubbell FA, McMullin JM, et al. Impact of U.S. citizenship status on cancer screening among immigrant women. J Gen Intern Med. 2005;20:290–296. doi: 10.1111/j.1525-1497.2005.40158.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schroen AT, Brenin DR, Kelly MD, et al. Impact of Patient Distance to Radiation Therapy on Mastectomy Use in Early-Stage Breast Cancer Patients. J Clin Oncol. 2005;23:7074–7080. doi: 10.1200/JCO.2005.06.032. [DOI] [PubMed] [Google Scholar]
- 11.Sox CM, Swartz K, Burstin HR, et al. Insurance or a regular physician: which is the most powerful predictor of health care? Am J Public Health. 1998;88:364–70. doi: 10.2105/ajph.88.3.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Talcott JA, Spain P, Clark JA, et al. Hidden barriers between knowledge and behavior: the North Carolina prostate cancer screening and treatment experience. Cancer. 2007;109:1599–1606. doi: 10.1002/cncr.22583. [DOI] [PubMed] [Google Scholar]
- 13.Underwood W, De Monner S, Ubel P, et al. Racial/ethnic disparities in the treatment of localized/regional prostate cancer. J Urol. 2004;171:1504–1507. doi: 10.1097/01.ju.0000118907.64125.e0. [DOI] [PubMed] [Google Scholar]
- 14.Hoffman RM, Gilliland FD, Eley JW, et al. Racial and ethnic differences in advanced-stage prostate cancer: the Prostate Cancer Outcomes Study. J Natl Cancer Inst. 2001;93:388–395. doi: 10.1093/jnci/93.5.388. [DOI] [PubMed] [Google Scholar]
- 15.McFall SL. Use and awareness of prostate specific antigen tests and race/ethnicity. J Urol. 2007;177:1475–1480. doi: 10.1016/j.juro.2006.11.096. [DOI] [PubMed] [Google Scholar]
- 16.Spencer BA, Babey SH, Etzioni DA, et al. A population-based survey of prostate-specific antigen testing among California men at higher risk for prostate carcinoma. Cancer. 2006;106:765–774. doi: 10.1002/cncr.21673. [DOI] [PubMed] [Google Scholar]
- 17.Hoffman RM, Hunt WC, Gilliland FD, et al. Patient satisfaction with treatment decisions for clinically localized prostate carcinoma. Results from the Prostate Cancer Outcomes Study. Cancer. 2003;97:1653–1662. doi: 10.1002/cncr.11233. [DOI] [PubMed] [Google Scholar]
- 18.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- 19.Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34:1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 20.Shi L, Stevens GD. Vulnerability and unmet health care needs. The influence of multiple risk factors. J Gen Intern Med. 2005;20:148–154. doi: 10.1111/j.1525-1497.2005.40136.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Iverson DC. Involving providers and patients in cancer control and prevention efforts. Barriers to overcome. Cancer. 1993;72(3 Suppl):1138–43. doi: 10.1002/1097-0142(19930801)72:3+<1138::aid-cncr2820721332>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 22.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 23.Maly RC, Frank JC, Marshall GN, et al. Perceived efficacy in patient-physician interactions (PEPPI): validation of an instrument in older persons. J Am Geriatr Soc. 1998;46:889–894. doi: 10.1111/j.1532-5415.1998.tb02725.x. [DOI] [PubMed] [Google Scholar]
- 24.Peterman AH, Fitchett G, Brady MJ, et al. Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy--Spiritual Well-being Scale (FACIT-Sp) Ann Behav Med. 2002;24:49–58. doi: 10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- 25.Deibert CM, Maliski S, Kwan L, et al. Prostate cancer knowledge among low income minority men. J Urol. 2007;177:1851–1855. doi: 10.1016/j.juro.2007.01.062. [DOI] [PubMed] [Google Scholar]
- 26.Krupski TL, Bergman J, Kwan L, et al. Quality of prostate carcinoma care in a statewide public assistance program. Cancer. 2005;104:985–992. doi: 10.1002/cncr.21272. [DOI] [PubMed] [Google Scholar]
- 27.Ware J, Jr., Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 28.McCorkle R, Young K. Development of a symptom distress scale. Cancer Nurs. 1978;1:373–378. [PubMed] [Google Scholar]
- 29.Krupski TL, Bergman J, Kwan L, et al. Quality of prostate carcinoma care in a statewide public assistance program. Cancer. 2005;104:985–992. doi: 10.1002/cncr.21272. [DOI] [PubMed] [Google Scholar]
- 30.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 31.Shapiro MF, Morton SC, McCaffrey DF, et al. Variations in the care of HIV-infected adults in the United States: results from the HIV Cost and Services Utilization Study. JAMA. 1999;281:2305–2315. doi: 10.1001/jama.281.24.2305. [DOI] [PubMed] [Google Scholar]
- 32.Scardino P. Update: NCCN prostate cancer Clinical Practice Guidelines. J Natl Compr Canc Netw. 2005;3(Suppl 1):S29–33. [PubMed] [Google Scholar]
- 33.Kiefe CI, McKay SV, Halevy A, et al. Is cost a barrier to screening mammography for low-income women receiving Medicare benefits? A randomized trial. Arch Intern Med. 1994;154:1217–1224. [PubMed] [Google Scholar]
- 34.Blustein J. Medicare coverage, supplemental insurance, and the use of mammography by older women. New Engl J Med. 1995;332:1138–1143. doi: 10.1056/NEJM199504273321706. [DOI] [PubMed] [Google Scholar]
- 35.Leybas-Amedia V, Nuno T, Garcia F. Effect of acculturation and income on Hispanic women’s health. J Health Care Poor Underserved. 2005;16:128–41. doi: 10.1353/hpu.2005.0127. [DOI] [PubMed] [Google Scholar]
- 36.Morales LS, Cunningham WE, Galvan FH, et al. Sociodemographic differences in access to care among Hispanic patients who are HIV infected in the United States. Am J Public Health. 2004;94:1119–1121. doi: 10.2105/ajph.94.7.1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baker DW, Hayes R, Fortier JP. Interpreter use and satisfaction with interpersonal aspects of care for Spanish-speaking patients. Med Care. 1998;36:1461–70. doi: 10.1097/00005650-199810000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Katz MH, Cunningham WE, Fleishman JA, et al. Effect of case management on unmet needs and utilization of medical care and medications among HIV-infected persons. Ann Intern Med. 2001;135:557–565. doi: 10.7326/0003-4819-135-8_part_1-200110160-00006. [DOI] [PubMed] [Google Scholar]
- 39.Bell RA, Kravitz RL, Thom D, et al. Unmet expectations for care and the patient-physician relationship. J Gen Intern Med. 2002;17:817–824. doi: 10.1046/j.1525-1497.2002.10319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Maliski SL, Kwan L, Krupski T, et al. Confidence in the ability to communicate with physicians among low-income patients with prostate cancer. Urology. 2004;64:329–334. doi: 10.1016/j.urology.2004.03.042. [DOI] [PubMed] [Google Scholar]
- 41.Senecal C, Nouwen A, White D. Motivation and dietary self-care in adults with diabetes: are self-efficacy and autonomous self-regulation complementary or competing constructs? Health Psychol. 2001;19:452–457. doi: 10.1037//0278-6133.19.5.452. [DOI] [PubMed] [Google Scholar]
- 42.Stutts WC. Physical activity determinants in adults. Perceived benefits, barriers, and self efficacy. AAOHN Journal. 2002;50:499–507. [PubMed] [Google Scholar]
- 43.Shiffman S, Balabanis MH, Paty JA, et al. Dynamic effects of self-efficacy on smoking lapse and relapse. Health Psychol. 2000;19:315–323. doi: 10.1037//0278-6133.19.4.315. [DOI] [PubMed] [Google Scholar]
- 44.Boehm S, Coleman-Burns P, Schlenk EA, et al. Prostate cancer in African American men: increasing knowledge and self-efficacy. J Community Health Nurs. 1995;12:161–169. doi: 10.1207/s15327655jchn1203_4. [DOI] [PubMed] [Google Scholar]