Abstract
BACKGROUND
Smoking cigarettes is associated with lower risk of Parkinson’s disease (PD). Despite the clinical links between PD and essential tremor (ET), there are few data on smoking in ET. One study showed an association between smoking and lower ET prevalence. We now study whether baseline smoking is associated with lower risk of incident ET.
METHODS
Using a population-based, cohort design, baseline cigarette smoking habits were assessed in 3,348 participants in an epidemiological study in Spain, among whom 77 developed incident ET.
RESULTS
There were 3,348 participants, among whom 397 (11.9%) were smokers at baseline. Five (6.5%) of 77 incident ET cases had been smokers at baseline compared with 392 (12.0%) of 3,271 controls (p = 0.14). Baseline pack-years were lower in incident ET cases than controls (9.2 ± 17.7 vs. 15.7 ± 28.4, p = 0.002). Participants were stratified into baseline pack-year tertiles and few incident ET cases were in the highest tertile (4 [5.2%] cases vs. 431 [13.2%] controls, p = 0.039). In Cox Proportional Hazards Models, highest baseline pack-year tertile was associated with lower risk of incident ET; those in the highest pack-year tertile were one-third as likely to develop ET when compared to non-smokers (RR = 0.37, 95% CI = 0.14–1.03, p = 0.057 [unadjusted model] and RR = 0.29, 95% CI = 0.09–0.90, p = 0.03 [adjusted model]).
CONCLUSIONS
We demonstrated an association between baseline heavy cigarette smoking and lower risk of incident ET. The biological basis for this association requires future investigation.
Keywords: essential tremor, Parkinson’s disease, cigarette smoking, epidemiology
Introduction
Essential tremor (ET) is one of the most common adult-onset neurological disorders.1, 2 Both genetic3, 4 and non-genetic (environmental factors)5–9 are likely to play an role in disease etiology.
A possible link between ET and Parkinson’s disease (PD) has been suggested in the clinical literature.10–12 The development of PD has been described in some ET patients, as has the co-occurrence of the two disorders in the same patient.11, 13 In addition, recent pathological studies have described Lewy bodies in some ET patients.14–16
Many studies have demonstrated an association between cigarette smoking and lower risk of PD. 17, 18 Despite the clinical10–13 and pathological14–16 links between ET and PD, there are few data examining whether there is an association between smoking and ET. In a population-based study in Spain, we demonstrated an association between smoking and lower prevalence of ET.19 However, given the cross-sectional design of those analyses, we were unable to assess whether a reduction in cigarette smoking preceded the onset of ET or merely followed the onset of disease (e.g., perhaps in an attempt to reduce nicotine-associated tremor). To address this shortcoming, we now utilize longitudinal data from that population-based study to test the hypothesis that cigarette smoking, which was assessed at baseline, was associated with a reduced risk of incident ET at follow-up.
Methods
Study population
This investigation was part of the Neurological Disorders in Central Spain (NEDICES), a longitudinal, population-based survey of major age-associated conditions of persons age 65 years and older. As described previously,20–27 the study sample was taken from the census of three communities in central Spain: Las Margaritas, Lista, and Arévalo. The three communities represent a broad spectrum of current social and economic conditions in Spain. The registered study population consisted of 6,395 individuals, but 481 were ineligible (e.g., census issues, incorrect address, death), leaving 5,914 eligible subjects, of whom 5,278 (89.2%) were evaluated at baseline (1994 to 1995).24 All procedures were approved by the University’s ethical standards committee on human experimentation. Written (signed) informed consent was obtained from all participants upon enrollment.
Baseline evaluation
At baseline (1994–1995), a detailed in-person evaluation was administered to enrollees. A questionnaire collected data on demographics, medical and neurological disorders, current medications, and lifestyle variables (smoking status and ethanol consumption). A screening question for depression was also administered (“Do you suffer from depression?”). The questionnaire also included a screening question for ET (“have you ever suffered from tremor of the head, hands, or legs that has lasted longer than several days?”) This question was a Spanish adaptation of that used by the Italian Longitudinal Study on Aging (ILSA) Working Group.8, 23 The sensitivity of the screening question for ET was 68.6% in our incidence study of ET.24
Persons who screened positive for ET underwent a neurological evaluation that included a standardized medical history and a general neurological examination (mental status, speech, cranial nerves, strength and tone, primary sensory modalities, reflexes, extensor toe signs, coordination and gait, as well as the motor portion of the Unified Parkinson’s Disease Rating Scale [UPDRS]).28 During the neurological examination, participants were asked to perform three manual tasks to assess postural and kinetic tremors including sustained bilateral arm extension, bilateral finger-nose-finger maneuver (with a minimum of six repetitions with each arm), and an Archimedes spiral drawn with the dominant arm. The neurological examination was performed by one of eight senior neurologists who met at the inception of the study to establish standardized methods to perform and interpret the examination (J. B–L., F. B–P., and see acknowledgements A.B., A. M–S., J. D–G., J.O., J.P., and J. P–E.). For participants who could not be examined, medical records were obtained from their general practitioners, from in-patient hospitalizations, and from neurological specialists (if they had visited one).
Diagnostic criteria for ET, which were used both in participants who were examined and those whose medical records were reviewed, were similar to those used in the Sicilian Study.8 Thus, participants were diagnosed as having ET if they had an action tremor of the head or limbs without any other recognizable cause.20, 24, 29 The tremor had to be of gradual onset (i.e., slow and progressive) and either (1) present for at least 1 year or (2) accompanied by a family history of the same disorder (at least one reportedly-affected first-degree relative). 20, 24, 29 On an Archimedes spiral, tremor severity had to be moderate or greater (rating ≥ 2 according to the Washington Heights-Inwood Genetic Study of ET Rating Scale).30 Based on their medical and medication history, participants were not considered to have ET if their tremor was related to alcohol withdrawal, hyperthyroidism, anxiety, or medications (including an extensive list of medications that result in dopamine receptor blockade and another list of medications that induce action tremor). Similarly, based on their neurological examination, participants with action tremor attributed to PD, dystonia, orthostatic tremor or other movement disorders were not considered to have ET. In most cases, ET cases identified by one of the eight neurologists were subsequently examined independently by two additional neurologists (who were chosen from among the eight). These participants were classified as having ET only when the three neurologists agreed. Their agreement was high (>90%).
Of the 5,278 participants who were evaluated at baseline (1994–1995), 256 prevalent ET cases (4.8%) were detected,23 and these were excluded from the current analyses, leaving 5,022 who were free of ET at baseline.
Follow-up evaluation
As described,24 follow-up data were available on 3,942 (78.5%) of 5,022 participants, with the majority (N = 840) of those who were lost to follow-up being deceased.24 Follow-up data were derived either from: (1) an in-person follow-up evaluation (1997–1998, approximately 80% of participants) that was similar to the baseline evaluation or (2) medical data from health care providers and family on those who had died prior to that evaluation (approximately 20% of participants).24 The diagnostic approach to ET cases was identical to that performed during the baseline evaluation.24 At follow-up, there were 83 incident ET cases24 and 3,859 participants without incident ET (3,942 total).
Final sample
Of the 5,278 participants screened for ET at baseline (1994–1995), 256 prevalent ET cases (4.8%) were detected,23 and these were excluded from our analyses. As documented previously,24 follow-up data were available on 3,942 of the remaining 5,022 participants (including 83 incident ET cases and 3,859 participants without incident ET). We further excluded participants if data on smoking or ethanol consumption were unavailable, which left 3,348 remaining participants who were included in our analyses. These remaining 3,348 participants were similar to the original 5,278 participants in terms of mean ± SD baseline age (73.6 ± 6.6 years vs. 74.3 ± 7.0 years), gender (57.2% vs. 57.3% women), and education (e.g., 13.1% illiterate vs. 12.1% illiterate).
Data analyses
Statistical analyses were performed in SPSS Version 13.0 (SPSS, Inc., Chicago, IL). Baseline characteristics of study groups were compared using Student’s t tests and chi-square tests. For all participants, we calculated pack-years (i.e., packs of cigarettes smoked per day multiplied by years smoked). In some analyses, pack-years were categorized in tertiles (<19.2, 19.2–49.0, >49.0). Participants who had never smoked were coded as having 0 pack-years and they served as the reference group in those analyses, which included all participants. Also, data on ethanol consumption (average number of drinks consumed per day and duration of consumption in years) were used to compute drink years. One “drink-year” was defined as the intake of one drink of ethanol per day for one year. One drink consisted of one can of beer (360 mL), one glass of wine (120 mL) or 30 mL of liquor.17
We used Cox proportional-hazards modelsto estimate the relative risk of incident ET; this generated relative risks (RR) with 95% confidence intervals (CI). Person-years for participants who developed incident ET were calculated as the time between the baseline evaluation and the reported date of ET onset. When the date of onset of ET was unknown, person-years were calculated as the midpoint between the first evaluation and the follow up evaluation. Person-years for participants who did not develop incident ET were calculated as the time between the baseline evaluation and: (1) the follow up evaluation or (2) death in the participants who died prior to follow-up evaluation. We began with an unadjusted model and then, in adjusted models, included as confounding variables those variables that were associated either with baseline smoking or with incident ET in univariate analyses (Tables 1 and 2).
Table 1.
Baseline characteristics of participants who were vs. were not cigarette smokers at baseline
| Baseline characteristics | Current cigarette smoker (at baseline) n=397 | Current non- smoker (at baseline) n=2,951 | p value |
|---|---|---|---|
| Age in years (mean ± SD) | 71.2 ± 5.5 | 73.9 ± 6.7 | < 0.001 a |
|
| |||
| Gender (women) | 71 (17.9%) | 1,844 (62.5%) | < 0.001 b |
|
| |||
| Educational level | < 0.001 b | ||
| Illiterate | 25 (6.3%) | 415 (14.1%) | |
| Can read and write | 175 (44.1%) | 1,239 (42.0%) | |
| Primary studies | 109 (27.5%) | 873 (29.6%) | |
| Secondary studies | 88 (22.2%) | 424 (14.4%) | |
|
| |||
| Drink-years | 95.9 ± 76.2 | 50.3 ± 68.2 | < 0.001 a |
|
| |||
| Depressive symptoms (“Do you suffer from depression?”) | 81 (20.4%) | 783 (26.6%) | 0.008 b |
NS = not significant.
Independent samples t-test.
Chi-square.
Table 2.
Baseline characteristics of incident ET cases and control subjects
| Baseline characteristics | Incident ET cases n = 77 | Control subjects n = 3,271 | p value |
|---|---|---|---|
| Age in years (mean ± SD) | 73.8 ± 6.3 | 73.6 ± 6.6 | 0.82 a |
|
| |||
| Gender (women) | 46 (59.7%) | 1,869 (57.1%) | 0.65 b |
|
| |||
| Educational level | 0.57 b | ||
| Illiterate | 13 (16.9%) | 427 (13.1%) | |
| Can read and write | 35 (45.5%) | 1,379 (42.2%) | |
| Primary studies | 18 (23.4%) | 964 (29.5%) | |
| Secondary studies | 11 (14.3%) | 501 (15.3%) | |
|
| |||
| Drink-years | 61.1 ± 70.5 | 55.6 ± 70.8 | 0.50 a |
|
| |||
| Depressive symptoms (“Do you suffer from depression?”) | 29 (37.7%) | 835 (25.6%) | 0.016 b |
|
| |||
| Current cigarette smoker | 5 (6.5%) | 392 (12.0%) | 0.14 b |
|
| |||
| Cigarette pack-years* | 9.2 ± 17.7 | 15.7 ± 28.4 | 0.002 a |
|
| |||
| Pack-year tertile | 0.24 b | ||
| Non-smokers | 51 (66.2%) | 1,982 (60.6%) | |
| Lowest tertile (<19.2) | 11 (14.3%) | 421 (12.9%) | |
| Middle tertile (19.2–49.0) | 11 (14.3%) | 437 (13.4%) | |
| Highest tertile (>49.0) | 4 (5.2%) | 431 (13.2%) | |
|
| |||
| Pack-year tertile | 0.039 b | ||
| Non-smokers + lowest + middle tertile | 73 (94.8%) | 2,840 (86.8%) | |
| Highest tertile | 4 (5.2%) | 431 (13.2%) | |
NS = not significant.
Independent samples t-test.
Chi-square.
In these analyses, participants who had never smoked were classified as having 0 pack-years. In an additional analysis that excluded participants who had never smoked, we compared pack-years in ET cases vs. controls: ET (N = 26) = 27.2 ± 12.1 vs. controls (N = 1,289) = 39.8 ± 33.0, p = 0.006.
Results
There were 3,348 participants, among whom 397 (11.9%) were current cigarette smokers (at baseline). At baseline, the 397 current smokers were younger, more educated, had more drink years, and were less likely to be women and less likely to have depressive symptoms than the 2,951 current non-smokers (Table 1).
The mean (SD) follow-up was 3.3 ± 0.8 years (range = 0.1–6.6 years). At follow-up, there were 77 incident ET cases (2.3%). The incident ET cases and controls were compared in terms of their baseline characteristics; incident ET cases were similar in age and gender to the controls, but a larger proportion had had depressive symptoms at baseline (Table 2). The higher number of drink years in incident cases than in controls did not reach statistical significance (Table 2).
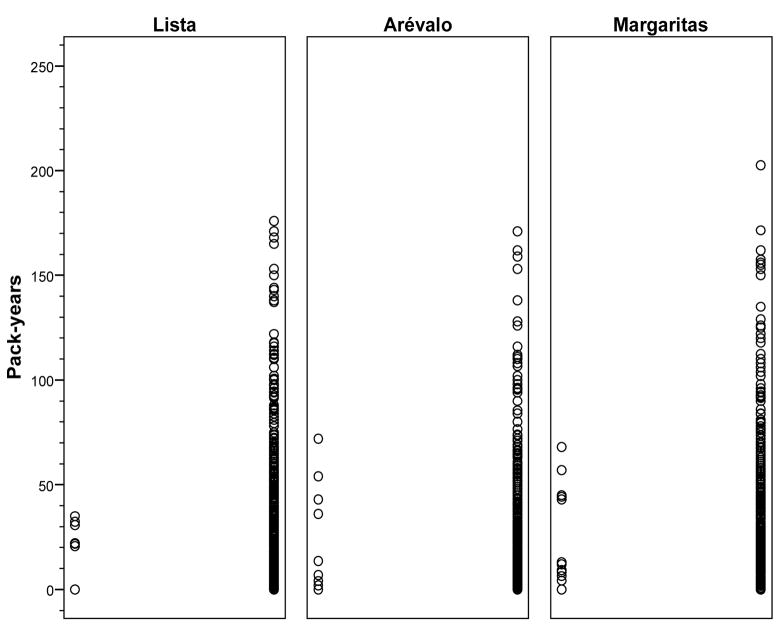
The 3,348 participants included 1,173 (35.0%) from Las Margaritas, 1,103 (32.9%) from Lista, and 1,072 (32.0%) from Arévalo. In each community, the number of cigarette pack-years at baseline was plotted for incident ET cases vs. controls, demonstrating that few incident ET cases had large numbers of pack-years of smoking (Figure 1).
Figure 1.
Lista (N = 1,103, left panel), Arévalo (N = 1,072, middle panel), and Las Margaritas (N = 1,173, right panel). The number of cigarette pack-years at baseline was plotted for participants with incident ET (left column in each panel) vs. controls (right column in each panel), demonstrating that few incident ET cases had large numbers of pack-years of smoking.
The proportion of incident ET cases who had smoked at baseline was half that of controls who had smoked at baseline (6.5% vs. 12.0%), although this trend was not significant (Table 2). Baseline cigarette pack-years were lower in incident ET cases than controls (Table 2). Participants were stratified into baseline pack-year tertiles and fewer of the incident ET cases were in the highest tertile (p = 0.039, Table 2).
In an unadjusted Cox proportional hazards model, baseline smoking was marginally associated with lower risk of incident ET (RR = 0.52, 95% CI = 0.21–1.29, p = 0.16). In an analysis that adjusted for age, gender, educational level, drink-years, and depressive symptoms, RR = 0.50, 95% CI = 0.20–1.28, p = 0.15. In an unadjusted Cox proportional hazards model, pack-years was marginally associated with lower risk of incident ET (RR = 0.989, 95% CI = 0.978–1.000, p = 0.057). In an analysis that adjusted for age, gender, educational level, drink-years, and depressive symptoms, RR = 0.984, 95% CI = 0.971–0.998, p = 0.02. Pack-years were stratified into tertiles, and in unadjusted and then adjusted models, highest pack-year tertile was associated with lower risk of ET such that those in the highest pack-year tertile were one-third as likely to develop incident ET when compared to non-smokers (Table 3).
Table 3.
Risk of ET by cigarette pack-year tertiles
| Unadjusted Model |
Adjusted model* |
|||||
|---|---|---|---|---|---|---|
| RR | 95% CI | p value | RR | 95% CI | p value | |
| Lowest pack-year tertile (<19.2) | 1.02 | 0.53–1.96 | 0.95 | 0.88 | 0.41–1.89 | 0.74 |
|
| ||||||
| Middle pack-year tertile (19.2–49.0) | 1.003 | 0.52–1.93 | 0.99 | 0.82 | 0.36–1.88 | 0.65 |
|
| ||||||
| Highest pack-year tertile (>49.0) | 0.37 | 0.14–1.03 | 0.057 | 0.29 | 0.09–0.90 | 0.03 |
|
| ||||||
| Test for trend | p = 0.13 | p = 0.048 | ||||
The reference category was non-smokers.
Adjusted for age in years, gender, educational level, drink-years, and depressive symptoms.
The sample included 149 participants with dementia and 56 with PD. When they were excluded, results did not change: in a Cox proportional hazards model that adjusted for age, gender, educational level, drink-years, and depressive symptoms, pack-years was associated with lower risk of incident ET (RR = 0.984, 95% CI = 0.970–0.998, p = 0.025) and those in the highest pack-year tertile were one-third as likely to develop incident ET when compared to non-smokers (adjusted RR = 0.28, 95% CI = 0.09–0.90, p = 0.03).
While 71 (92.2%) of incident ET cases were diagnosed by NEDICES examination, six (7.8%) were diagnosed by medical record review. When these six were excluded, results did not change: in a Cox proportional hazards model that adjusted for age, gender, educational level, drink-years, and depressive symptoms, pack-years was associated with lower risk of incident ET (RR = 0.983, 95% CI = 0.969–0.998, p = 0.02) and those in the highest pack-year tertile were one-fourth as likely to develop incident ET when compared to non-smokers (adjusted RR = 0.26, 95% CI = 0.08–0.82, p = 0.02).
Discussion
In this prospective, population-based study, we examined baseline smoking habits and risk of incident ET. Our data show that elderly ET cases have a similar smoking pattern to that which has been reported previously for patients with PD. When compared with never smokers, smokers in the highest pack-year tertile were one third as likely to develop incident ET.
Two previous studies examined smoking habits in prevalent ET cases compared to controls.5, 19 In one of these, 5 although the proportion of ET cases and controls who smoked did not differ, the number of cigarette pack years was significantly lower in ET cases than controls (29.93 ± 23.54 vs. 35.91 ± 24.56, t = 2.40, p = 0.02). The second of these studies used NEDICES baseline data to examine the association between smoking and prevalent ET.19 In that study, ever smokers were approximately one-half as likely to have ET when compared with never smokers (OR = 0.58, 95% CI = 0.40–0.84, p = 0.004) and ever smokers in the highest pack-year tertile were one third as likely to have ET when compared with never smokers (adjusted OR = 0.39, 95% CI = 0.22–0.69, p = 0.001). We now extend these observations by examining smoking behavior prior to the onset of ET.
Smoking has been reported to play a role in neurodegenerative diseases, including PD and multiple system atrophy.19, 20, 29 Although there are other agents in tobacco smoke that could be responsible for this possible neuroprotective effect, nicotine has been the focus of considerable research for several reasons. First, nicotine is known to protect against the degenerative effects of toxic insults in different experimental systems.31–33 Nicotine pre-treatment consistently reduces the detrimental effects of excitotoxin exposure in cultured cells,31–33 including neurotoxin-induced degeneration of nigral dopamine-containing neurons.34 In rats and mice, nicotine can protect against parkinsonism-inducing neurotoxins, like 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) and methamphetamine, probably by increasing the level of neurotrophic factors.35
This study had a number of potential limitations. Screening questions for ET often fail to ascertain mild cases. Our screening questionnaire for ET was of modest sensitivity (68.6%). If at baseline, however, we had included among our controls some participants with mild ET, this would not have explained our results. Furthermore, if at follow-up, we had mis-classified some mild ET cases as controls, this misclassification would have biased our results towards the null hypothesis as it would have made it more difficult to detect true case-control differences. A second issue is that although the criteria for ET we used in this study were identical to those we have used in our previous studies, 20, 21, 23, 24, 36 there is the possibility that some of our ET cases were misdiagnosed and that they actually had PD rather than ET. However, a complete UPDRS motor examination was conducted specifically to assess subtle motor features of parkinsonism; none of our ET cases had tremor at rest or other features of parkinsonism on these examinations and none was taking medication for PD (levodopa-carbidopa, dopamine agonists or anticholinergic medications). In addition, when compared with other population-based studies, the prevalence of PD in NEDICES is similar to the expected prevalence of PD in this age group,26 indicating that it is unlikely that we under-diagnosed PD. Nevertheless, our follow-up interval was modest and we cannot fully exclude the possibility that some of the incident ET cases might develop PD during additional follow-up. Hence, additional follow-up time may be important. Third, we examined an elderly population of people older than 65 years of age. Therefore, this study can only define the relationship between smoking and ET in an elderly population. Finally, baseline smoking was associated with lower risk of incident ET (adjusted RR = 0.50), but the association was only marginal (p = 0.15). Despite enrolment of several thousand participants, the prevalence of smoking was low in the cohort; hence, for this one analysis, the study only had sufficient power to detect a RR ≤ 0.44.
Acknowledgments
The authors gratefully acknowledge the vital help of the other members of the NEDICES Study Group: S. Vega, J.M. Morales, R, Gabriel, A. Portera-Sánchez, A. Berbel, A. Martínez-Salio, J. Díaz-Guzmán, J. Olazarán, J. Pardo, J. Porta-Etessam, F. Pérez del Molino, J. Rivera-Navarro, M. Alonso, C. Gómez, C. Saiz, G. Fernández, P. Rodríguez and Fernando Sánchez-Sánchez. Finally, we also wish to express our sincere thanks to J. de Pedro-Cuesta, M.J. Medrano, and J. Almazán, the municipal authorities, family doctors, nurses, and the populations of Getafe, Lista, and Arévalo county. NEDICES was supported by the Spanish Health Research Agency and the Spanish Office of Science and Technology. Dr. Louis is supported by NIH R01 NS042859, R01 NS039422, and ES P03 09089 from the National Institutes of Health, Bethesda, MD.
Footnotes
Other members of the Neurological Disorders in Central Spain (NEDICES) Study Group are listed in the Acknowledgments.
Disclosure: The authors report no conflicts of interest.
Statistical Analyses: The statistical analyses were conducted by Drs. Louis and Benito-Leon.
References
- 1.Dogu O, Sevim S, Camdeviren H, et al. Prevalence of essential tremor: door-to-door neurologic exams in Mersin Province, Turkey. Neurology. 2003;61:1804–1806. doi: 10.1212/01.wnl.0000099075.19951.8c. [DOI] [PubMed] [Google Scholar]
- 2.Louis ED, Ottman R, Hauser WA. How common is the most common adult movement disorder? estimates of the prevalence of essential tremor throughout the world. Mov Disord. 1998;13:5–10. doi: 10.1002/mds.870130105. [DOI] [PubMed] [Google Scholar]
- 3.Higgins JJ, Loveless JM, Jankovic J, Patel PI. Evidence that a gene for essential tremor maps to chromosome 2p in four families. Mov Disord. 1998;13:972–977. doi: 10.1002/mds.870130621. [DOI] [PubMed] [Google Scholar]
- 4.Deng H, Le W, Jankovic J. Genetics of essential tremor. Brain. 2007;130:1456–1464. doi: 10.1093/brain/awm018. [DOI] [PubMed] [Google Scholar]
- 5.Jiménez-Jiménez FJ, de Todelo-Heras M, Alonso-Navarro H, et al. Environmental risk factors for essential tremor. Eur Neurol. 2007;58:106–113. doi: 10.1159/000103646. [DOI] [PubMed] [Google Scholar]
- 6.Prakash KM, Fook-Choong S, Yuen Y, Tan EK. Exploring the relationship between caffeine intake and essential tremor. Journal of the neurological sciences. 2006;251:98–101. doi: 10.1016/j.jns.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 7.Fabrizio E, Vanacore N, Valente M, et al. High prevalence of extrapyramidal signs and symptoms in a group of Italian dental technicians. BMC Neurol. 2007;7:24. doi: 10.1186/1471-2377-7-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salemi G, Aridon P, Calagna G, et al. Population-based case-control study of essential tremor. Italian journal of neurological sciences. 1998;19:301–305. doi: 10.1007/BF00713856. [DOI] [PubMed] [Google Scholar]
- 9.Louis ED. Etiology of essential tremor: should we be searching for environmental causes? Mov Disord. 2001;16:822–829. doi: 10.1002/mds.1183. [DOI] [PubMed] [Google Scholar]
- 10.Tan EK, Matsuura T, Nagamitsu S, et al. Polymorphism of NACP-Rep1 in Parkinson’s disease: an etiologic link with essential tremor? Neurology. 2000;54:1195–1198. doi: 10.1212/wnl.54.5.1195. [DOI] [PubMed] [Google Scholar]
- 11.Yahr MD, Orosz D, Purohit DP. Co-occurrence of essential tremor and Parkinson’s disease: clinical study of a large kindred with autopsy findings. Parkinsonism & related disorders. 2003;9:225–231. doi: 10.1016/s1353-8020(02)00057-3. [DOI] [PubMed] [Google Scholar]
- 12.Shahed J, Jankovic J. Exploring the relationship between essential tremor and Parkinson’s disease. Parkinsonism & related disorders. 2007;13:67–76. doi: 10.1016/j.parkreldis.2006.05.033. [DOI] [PubMed] [Google Scholar]
- 13.Chaudhuri KR, Buxton-Thomas M, Dhawan V, et al. Long duration asymmetrical postural tremor is likely to predict development of Parkinson’s disease and not essential tremor: clinical follow up study of 13 cases. Journal of neurology, neurosurgery, and psychiatry. 2005;76:115–117. doi: 10.1136/jnnp.2004.046292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Louis ED, Vonsattel JP, Honig LS, et al. Neuropathologic findings in essential tremor. Neurology. 2006;66:1756–1759. doi: 10.1212/01.wnl.0000218162.80315.b9. [DOI] [PubMed] [Google Scholar]
- 15.Louis ED, Honig LS, Vonsattel JP, et al. Essential tremor associated with focal nonnigral Lewy bodies: a clinicopathologic study. Archives of neurology. 2005;62:1004–1007. doi: 10.1001/archneur.62.6.1004. [DOI] [PubMed] [Google Scholar]
- 16.Ross GWDD, Cerosimo M, et al. Pathological investigation of essential tremor. Neurology. 2004;62:A537–A538. [Google Scholar]
- 17.Gorell JM, Rybicki BA, Johnson CC, Peterson EL. Smoking and Parkinson’s disease: a dose-response relationship. Neurology. 1999;52:115–119. doi: 10.1212/wnl.52.1.115. [DOI] [PubMed] [Google Scholar]
- 18.Ritz B, Ascherio A, Checkoway H, et al. Pooled analysis of tobacco use and risk of Parkinson disease. Archives of neurology. 2007;64:990–997. doi: 10.1001/archneur.64.7.990. [DOI] [PubMed] [Google Scholar]
- 19.Benito-Leon J, Louis ED, Permejo-Pareja F. Population-based case-control study of cigarette smoking and essential tremor. Mov Disord. 2007 doi: 10.1002/mds.21810. In Press. [DOI] [PubMed] [Google Scholar]
- 20.Benito-Leon J, Louis ED, Bermejo-Pareja F. Population-based case-control study of cognitive function in essential tremor. Neurology. 2006;66:69–74. doi: 10.1212/01.wnl.0000192393.05850.ec. [DOI] [PubMed] [Google Scholar]
- 21.Benito-Leon J, Louis ED, Bermejo-Pareja F. Elderly-onset essential tremor is associated with dementia. Neurology. 2006;66:1500–1505. doi: 10.1212/01.wnl.0000216134.88617.de. [DOI] [PubMed] [Google Scholar]
- 22.Morales JM, Bermejo-Pareja F, Benito-Leon J, et al. Methods and demographic findings of the baseline survey of the NEDICES cohort: a door-to-door survey of neurological disorders in three communities from Central Spain. Public Health. 2004;118:426–433. doi: 10.1016/j.puhe.2003.10.007. [DOI] [PubMed] [Google Scholar]
- 23.Benito-Leon J, Bermejo-Pareja F, Morales JM, et al. Prevalence of essential tremor in three elderly populations of central Spain. Mov Disord. 2003;18:389–394. doi: 10.1002/mds.10376. [DOI] [PubMed] [Google Scholar]
- 24.Benito-Leon J, Bermejo-Pareja F, Louis ED. Incidence of essential tremor in three elderly populations of central Spain. Neurology. 2005;64:1721–1725. doi: 10.1212/01.WNL.0000161852.70374.01. [DOI] [PubMed] [Google Scholar]
- 25.Bermejo F, Gabriel R, Vega S, et al. Problems and issues with door-to-door, two-phase surveys: an illustration from central Spain. Neuroepidemiology. 2001;20:225–231. doi: 10.1159/000054794. [DOI] [PubMed] [Google Scholar]
- 26.Benito-Leon J, Bermejo-Pareja F, Rodriguez J, et al. Prevalence of PD and other types of parkinsonism in three elderly populations of central Spain. Mov Disord. 2003;18:267–274. doi: 10.1002/mds.10362. [DOI] [PubMed] [Google Scholar]
- 27.Benito-Leon J, Bermejo-Pareja F, Morales-Gonzalez JM, et al. Incidence of Parkinson disease and parkinsonism in three elderly populations of central Spain. Neurology. 2004;62:734–741. doi: 10.1212/01.wnl.0000113727.73153.68. [DOI] [PubMed] [Google Scholar]
- 28.Fahn SER. Members of the UPDRS Development Committee. In: Fahn SMC, Goldtein M, Calne DB, editors. Recent Developments in Parkinson’s Disease. Florham Park, NJ: Macmillan Health Care Information; 1987. pp. 153–163. [Google Scholar]
- 29.Bermejo-Pareja F, Louis ED, Benito-Leon J. Risk of incident dementia in essential tremor: A population-based study. Mov Disord. 2007;22:1573–1580. doi: 10.1002/mds.21553. [DOI] [PubMed] [Google Scholar]
- 30.Louis ED, Ford B, Frucht S, et al. Risk of tremor and impairment from tremor in relatives of patients with essential tremor: a community-based family study. Annals of neurology. 2001;49:761–769. doi: 10.1002/ana.1022. [DOI] [PubMed] [Google Scholar]
- 31.Mudo G, Belluardo N, Fuxe K. Nicotinic receptor agonists as neuroprotective/neurotrophic drugs. Progress in molecular mechanisms. J Neural Transm. 2007;114:135–147. doi: 10.1007/s00702-006-0561-z. [DOI] [PubMed] [Google Scholar]
- 32.Meissner W, Hill MP, Tison F, et al. Neuroprotective strategies for Parkinson’s disease: conceptual limits of animal models and clinical trials. Trends Pharmacol Sci. 2004;25:249–253. doi: 10.1016/j.tips.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 33.Zanardi A, Leo G, Biagini G, Zoli M. Nicotine and neurodegeneration in ageing. Toxicol Lett. 2002;127:207–215. doi: 10.1016/s0378-4274(01)00502-1. [DOI] [PubMed] [Google Scholar]
- 34.Jeyarasasingam G, Tompkins L, Quik M. Stimulation of non-alpha7 nicotinic receptors partially protects dopaminergic neurons from 1-methyl-4-phenylpyridinium-induced toxicity in culture. Neuroscience. 2002;109:275–285. doi: 10.1016/s0306-4522(01)00488-2. [DOI] [PubMed] [Google Scholar]
- 35.Maggio R, Riva M, Vaglini F, et al. Nicotine prevents experimental parkinsonism in rodents and induces striatal increase of neurotrophic factors. J Neurochem. 1998;71:2439–2446. doi: 10.1046/j.1471-4159.1998.71062439.x. [DOI] [PubMed] [Google Scholar]
- 36.Louis ED, Benito-Leon J, Ottman R, Bermejo-Pareja F. A population-based study of mortality in essential tremor. Neurology. 2007 doi: 10.1212/01.wnl.0000279339.87987.d7. (In Press) [DOI] [PubMed] [Google Scholar]