Abstract
Background:
Health-related quality of life (HRQOL) is reduced in multiple sclerosis (MS). It is unclear whether HRQOL is associated with white matter lesion burden or measures of brain atrophy.
Methods:
A cross-sectional baseline analysis of 507 patients with MS in a prospective cohort study at the University of California, San Francisco was performed. Multivariate linear regression models were used to determine whether MRI measures were associated with the Emotional Well-Being and Thinking/Fatigue subscale scores of the Functional Assessment in Multiple Sclerosis, a validated HRQOL measure in MS. The difference in each MRI metric associated with a minimal clinically important difference in each HRQOL subscale was calculated.
Results:
Higher T1 lesion load (15 mL; p = 0.024), normalized T1 lesion volume (20 mL; p = 0.016), or T2 lesion load (25 mL; p = 0.028) was associated with worse scores for Emotional Well-Being. Meaningfully lower scores on this subscale were correlated with lower normalized gray matter volume (118 mL; p = 0.037). Reduced Thinking/Fatigue scores were associated with higher normalized T1 lesion volume (21 mL; p = 0.024), or T2 lesion load (22 mL; p = 0.010) and with lower normalized gray matter (87 mL; p = 0.004), white matter (85 mL; p = 0.025), or brain parenchymal (98 mL; p = 0.001) volume.
Conclusions:
Aspects of health-related quality of life (HRQOL) in multiple sclerosis are associated with MRI evidence of white matter lesions and brain atrophy. These findings strengthen the argument for the use of HRQOL outcome measures in trials and suggest that lesion burden on conventional MRI is important for HRQOL.
GLOSSARY
- CIS
= clinically isolated syndrome;
- DMT
= disease-modifying therapy;
- EDSS
= Expanded Disability Status Scale;
- EWB
= Emotional Well-Being;
- FAMS
= Functional Assessment in Multiple Sclerosis;
- FOV
= field of view;
- HRQOL
= health-related quality of life;
- IQR
= interquartile range;
- IRSPGR
= inversion recovery spoiled gradient-recalled;
- PASAT
= Paced Auditory Serial Addition Test;
- PPMS
= primary progressive multiple sclerosis;
- PRMS
= progressive relapsing multiple sclerosis;
- MS
= multiple sclerosis;
- MSFC
= Multiple Sclerosis Functional Composite;
- nBPV
= normalized brain parenchymal volume;
- NEX
= number of excitations;
- nGMV
= normalized gray matter volume;
- nT1LV
= normalized T1 lesion volume;
- nWMV
= normalized white matter volume;
- RRMS
= relapsing–remitting multiple sclerosis;
- SPMS
= secondary progressive multiple sclerosis;
- TE
= echo time;
- TI
= inversion time;
- TF
= Thinking/Fatigue;
- TR
= repetition time;
- UCSF
= University of California, San Francisco.
Measures of health-related quality of life (HRQOL) are considered more comprehensive in capturing the overall impact of multiple sclerosis (MS) than physical disability scales such as the Expanded Disability Status Scale (EDSS).1 As a result, the US Food and Drug Administration now mandates the incorporation of HRQOL measures into MS clinical trials.2
It is postulated that irreversible neuroaxonal loss, which begins in the early stages of MS and is in part independent of new lesion formation,3–7 may be the primary contributor to disease progression. Although patients with early MS often have normal or only mildly abnormal neurologic examinations, they often report reduced HRQOL scores.1,8 We hypothesized that such reduced HRQOL may be related to neurodegeneration in MS. As such, we sought to determine whether there is an association between aspects of HRQOL, specifically emotional well-being and thinking and fatigue, and disease burden as assessed by high-resolution MRI techniques. Establishing such an association would further support the use of patient-reported HRQOL outcomes in MS trials.
METHODS
Research participants.
The protocol was approved by the Committee on Human Research at the University of California, San Francisco (UCSF), and informed consent was obtained from all participants. White (Hispanic and non-Hispanic) patients aged 18–70 years with an EDSS score less than 8.0 were recruited for inclusion in this study between July 2004 and September 2005, primarily from the UCSF Multiple Sclerosis Center. The diagnosis of MS or clinically isolated syndrome (CIS) was required and was made using the International Panel criteria.9,10 CIS was defined as the first well-defined neurologic clinical demyelinating event lasting more than 48 hours. In patients presenting with CIS, the brain MRI had to meet three of four Barkhof criteria.10 Patients were not enrolled if they had experienced a clinical relapse or had received treatment with glucocorticosteroids within the previous month, if they were participating in a study of nonapproved medications for MS, or if they were unable to undergo MRI. Patients with medical conditions that could put them at risk by participating in the study or who had recently abused drugs or alcohol were also excluded.
Clinical and laboratory assessments.
For all subjects, the baseline EDSS and Multiple Sclerosis Functional Composite (MSFC) scores were measured.11,12 Additional data included age at disease onset and at enrollment, sex, disease subtype, disease duration, and treatment status (use of disease-modifying therapy [DMT] at the time of study).
Health-Related Quality-of-Life assessment.
To assess aspects of HRQOL, the Emotional Well-Being and Thinking/Fatigue subscales of the Functional Assessment in Multiple Sclerosis (FAMS)13 version 4 were administered within 2 weeks of the brain MRI scans. The FAMS is a validated HRQOL instrument that uses self-assessment based on how well patients agree with statements about aspects of quality of life in the past 7 days. Scores ranging from 0 (not at all) to 4 (very much) were assigned to the Emotional Well-Being (seven questions) and Thinking/Fatigue (nine questions) sections. The raw scores of negatively worded questions, per the protocol, were reversed so that higher item and subscale scores reflected better HRQOL.13 Subscale summary scores were generated based on the answers to the questions; the possible range for Emotional Well-Being was therefore 0 to 28 (with 28 reflecting the best possible score), whereas for Thinking/Fatigue, the scores range from 0 to 36 (with 36 reflecting the best possible score).
MRI protocol.
Image acquisition.
Brain MRI scans were performed in all subjects after entry into the study, and analyses were performed without knowledge of disease subtype, duration, treatment history, or performance on HRQOL measures. MRI images were acquired using an eight-channel phased array coil in reception and a body coil in transmission on a 3-tesla GE Excite scanner (GE Healthcare Technologies, Waukesha, WI). Each MRI examination included scout localizers and axial dual-echo spin echo sequences (echo time [TE] at 20 and 90 msec, repetition time [TR] = 2,000 msec, 512 × 512 × 44 matrix, 240 × 240 × 132-mm3 field of view [FOV], slice thickness = 3 mm, interleaved). A high-resolution inversion recovery gradient-echo T1-weighted isotropic, volumetric sequence (three-dimensional inversion recovery spoiled gradient-recalled (IRSPGR) 1 × 1 × 1 mm3, 180 slices) was also performed (TE/TR/inversion time [TI] = 2/7/400 msec, flip angle = 15°, 256 × 256 × 180 matrix, 240 × 240 × 180-mm3 FOV, number of excitations [NEX] = 1). Conventional spin echo, T1-weighted images were acquired 5 minutes after administration of a single dose (0.1 mM/kg) of contrast agent (TE/TR = 8/467 msec, 256 × 256 × 44 matrix, 240 × 240 × 132-mm3 FOV, NEX = 1).
Lesion identification.
Brain lesions were identified on the baseline high-resolution T1-weighted, T2-weighted, and proton density–weighted images. Regions of interest were manually drawn on the high-resolution three-dimensional IRSPGR T1-weighted images based on a semiautomated pixel intensity threshold with manual editing, using in-house software, and T1 lesion masks were created.14
Brain tissue segmentation and normalization.
Brain segmentation and normalization were performed using SIENAX (Image Analysis Group, Oxford, UK), a fully automated technique. T1 lesion masks (described above) were incorporated into the SIENAX program to correct for misclassifications of parenchymal tissue while high-resolution T1-weighted images were segmented into images representing the volume of each voxel containing gray matter, white matter, CSF, and white matter lesions. The lesion masks overrode all SIENAX tissue classifications. Normalized tissue volumes were calculated by summing the lesion-corrected, partial volume estimate maps, multiplied by the brain scaling factor calculated by the SIENAX program yielding the following metrics: normalized T1 lesion volume (nT1LV), normalized white matter volume (nWMV), normalized gray matter volume (nGMV), normalized brain parenchymal volume (nBPV), and nT1LV/nWMV.
Statistical analyses.
Calculations and statistical analyses were performed using Stata 10.0 statistical software (StataCorp, College Station, TX). Means ± SDs or medians (with interquartile ranges) were used to summarize demographic and clinical data. Linear regression models were used to examine the relation between HRQOL scores and MRI predictors of interest. Based on estimates from the literature, we used the Cohen formulation of the (standardized) effect size, a method in which a standardized effect size of 0.20 is deemed a “small” effect size, which can be considered the equivalent of the minimal clinically important difference.15 The standardized effect size is multiplied by the baseline SD of the HRQOL scale/subscale score to obtain a corresponding effect size on the actual scale. Using the standard deviations obtained here for Emotional Well-Being (4.85) and for Thinking/Fatigue (8.63), the corresponding minimal clinically important differences were calculated to be 0.97 and 1.73 points. We then determined the difference in each individual predictor (MRI parameter) that was associated with the minimal clinically important difference on these subscales and, from this, rescaled each predictor. We generated new linear regression models and calculated the 95% confidence interval (CI) surrounding these rescaled regression lines. Rather than using automated methodologies, we added covariates to the multivariate models that were considered as potential confounders a priori or were necessary for face validity, including age at enrollment, sex, disease duration, and DMT status. Treatment was considered important because DMTs have, in some MS studies, independently predicted HRQOL.16,17 Disability and disease subtype appeared to be mediators (part of the causal pathway between the MRI predictor and the outcome) rather than confounders and were therefore not included in the final multivariate models because to do so would represent overadjustment for the particular research question. Mediation was assessed using the technique recommended by Vittinghoff et al.18
RESULTS
Five hundred seven patients whose characteristics are presented in table 1 were enrolled in the study. The majority had relapsing–remitting MS (n = 358 patients; 71%) or CIS (n = 82; 16%).
Table 1 Demographic characteristics of the study cohort (n = 507)
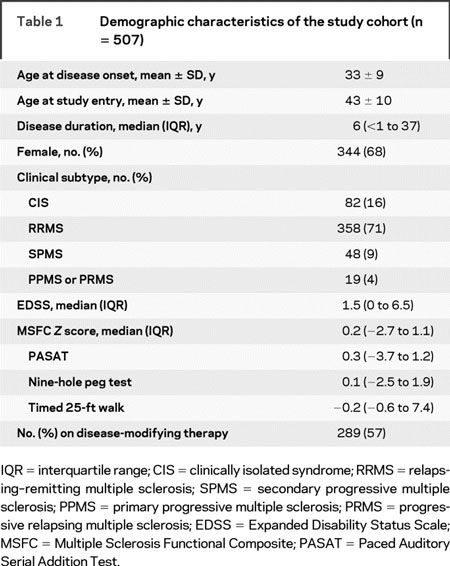
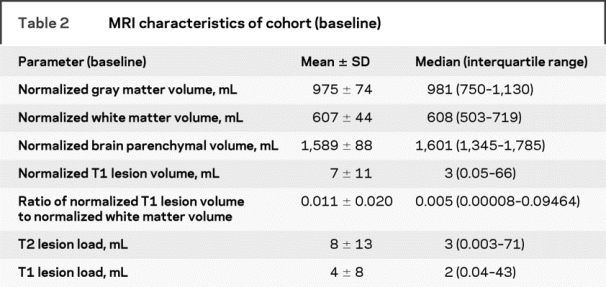
Most patients reported difficulties with both emotional well-being and thinking and fatigue. The mean (±SD) score for the Emotional Well-Being subscale was 22.5 ± 4.9 points; for the Thinking/Fatigue subscale, it was 23.5 ± 8.6 points. The untransformed distribution of responses to the questions is presented in table e-1 on the Neurology® Web site at www.neurology.org. The descriptive statistics for brain MRI parameters are presented in table 2. Five hundred one of the 507 enrolled patients had a gadolinium-enhanced scan performed; 81 (16%) had at least one enhancing lesion.
Table 2 MRI characteristics of cohort (baseline)
Emotional Well-Being.
In the univariate analyses (not shown), worse scores for Emotional Well-Being were associated with higher T2 and T1 lesion load as well as with nT1LV and nT1LV/nWMV ratio. On the other hand, substantially better scores for Emotional Well-Being were predicted by larger nGMV, nBPV, and nWMV.
The results of the multivariate analyses are shown in table 3. Higher nGMV was correlated with higher scores for Emotional Well-Being; clinically important differences (0.97 points) in this HRQOL subscale were associated with a 118-mL difference in nGMV. There was a trend for higher nBPV to correlate with higher HRQOL scores. There did not appear to be an association of nWMV and Emotional Well-Being, although the confidence intervals are wide enough that a relationship cannot be completely excluded.
Table 3 Results of multivariate analyses for MRI predictors of Emotional Well-Being
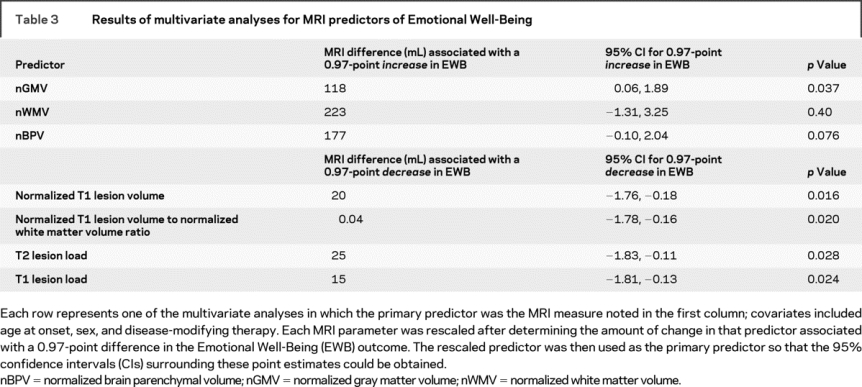
Differences in T1 and T2 lesion volumes were associated with clinically meaningful differences in self-reported Emotional Well-Being in the multivariate models (table 4). A 15 mL greater T1 lesion load, a 20 mL greater nT1LV, or a 25 mL greater T2 lesion load corresponded to a clinically meaningful reduction in this aspect of HRQOL. The presence of one or more contrast-enhancing lesions did not seem to be associated with this subscale score (0.23 points; 95% CI −0.94, 1.41; p = 0.70). DMT was not independently associated with the outcome in any of the models.
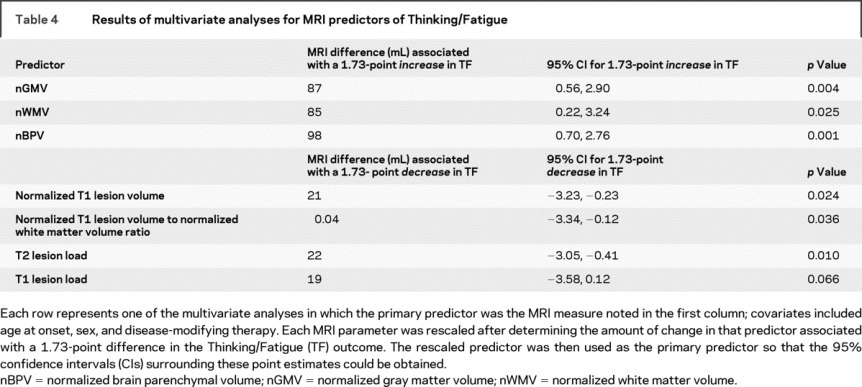
Table 4 Results of multivariate analyses for MRI predictors of Thinking/Fatigue
Thinking/Fatigue.
In the univariate analyses (not shown), larger nGMV, nWMV, or nBPV was associated with substantially better Thinking/Fatigue scores. Conversely, higher T2 and T1 lesion load, nT1LV, and nT1LV/nWMV ratio were associated with worse scores for this subscale.
In the multivariate models, higher nBPV, nGMV, and nWMV were strongly related to better Thinking/Fatigue scores; volumes associated with a meaningful difference ranged from 85 mL (nWMV) to 98 mL (nBPV). Because the role of disease subtype as a mediator in the nGMV and Thinking/Fatigue model was weaker, we added it to the multivariate model but found no substantive changes compared with when it was not in the model (a 93-mL difference in nGMV predicted a meaningful difference in Thinking/Fatigue; 95% CI 0.44, 2.81; p = 0.007).
As seen for Emotional Well-Being, small differences in lesion volume were associated with worse scores for Thinking/Fatigue. A 21-mL (nT1LV) to 22-mL (T2 lesion load) greater lesion burden correlated with a clinically meaningful decrement in Thinking/Fatigue. The association between the subscale score and T1 lesion load was somewhat attenuated, and the presence of a contrast-enhancing lesion was not associated with this subscale (0.02 points; 95% CI −2.04, 2.07; p = 0.99). DMT was not independently associated with the outcome in any of the models.
DISCUSSION
Fatigue and reductions in emotional and cognitive health are common in patients with MS, contributing substantially to the impact of the disease on daily life. In a well-characterized, single-center cohort of subjects with relatively little disability, we demonstrate that patients’ perceptions of how MS impacts these aspects of health correlate with both MRI lesion burden and brain volume, in particular gray matter volume. These associations persisted independent of treatment status, an important finding because DMTs by themselves have been shown in some studies to influence HRQOL.16,17
Brain atrophy in MS is thought to be caused both by direct axonal damage associated with lesion development and tissue loss accruing independently of new lesion development. Atrophy, particularly of the gray matter, begins early in the course of the disease, when changes in the clinical examination, except as related to relapses, may be less apparent.4,7,19,20 Neuroaxonal loss, a major contributor to atrophy, is thought to underlie the long-term development of disability in patients with MS. Neuroaxonal loss seems to have a more prominent effect on gray matter than on white matter volume, because reductions in gray matter volume are prominent early in the disease course and increase as the duration of the disease increases, whereas the rate of white matter atrophy is much lower and relatively constant.19,21 Reduced gray matter volume has been shown to be associated with long-term disability.20–23 The strong association of Emotional Well-Being and Thinking/Fatigue scores and atrophy, particularly with nGMV, together with the strong association of atrophy and neuroaxonal loss, implies that neuro-axonal loss may be a contributor to reduced HRQOL in MS. HRQOL outcomes may therefore represent clinical correlates of this disease process. These observations strengthen the rationale for incorporating HRQOL instruments into MS clinical trials, particularly of those in which the prevention of disability with putative neuroprotective agents is the primary outcome measure.
In addition to being associated with atrophy, Emotional Well-Being and Thinking/Fatigue scores correlated with lesion load/volume; smaller differences in lesion volume than in parenchymal volume correlated with a meaningful difference in the HRQOL outcomes. These findings are important because they suggest that even the lesion burden as assessed on standard clinical MRI may have an important impact on patients’ well-being. Furthermore, there is some indication that lesion burden is also associated with disability.22
Other studies have evaluated the association of patient-reported fatigue outcomes and MRI features in MS.24–30 Fatigue was not associated with brain parenchymal fraction in a cross-sectional analysis of 134 patients but was associated longitudinally.30 Another study showed that some aspects of HRQOL could be predicted by lesions or atrophy in specific anatomic locations in the brain.27 Fatigue in MS and in other chronic conditions in which it plays a prominent role, such as chronic fatigue syndrome, has been shown to have imaging correlates on functional MRI,31–33 and in a small study of chronic fatigue syndrome, affected patients had less gray matter volume than healthy controls.34 Although consistent with these previous reports, the present study demonstrates stronger associations between global MRI measures of disease burden and HRQOL. Reduced cognition, as measured by neuropsychological batteries, has been shown to strongly correlate with brain atrophy35 and lesion burden36; some studies have shown that the correlation of cognition is stronger with the former than with the latter.37,38 The results of these previous studies support our findings that self-reported cognitive dysfunction is strongly associated with brain atrophy.
Despite the large size of this cohort, our work has some limitations. The original study was not designed to evaluate overall HRQOL as a primary outcome measure. As such, some aspects of HRQOL, particularly those capturing physical and social well-being, were not evaluated in this cohort and need to be explored in future studies. Furthermore, because estimates of clinically important differences in the Emotional Well-Being and Thinking/Fatigue FAMS subscales are not available in the literature, we used standardized effect size benchmarks to estimate the minimal clinically important difference. Although there is good rationale for such an approach, the responsiveness of these FAMS subscales needs to be studied longitudinally. In addition, we cannot conclude that the association between HRQOL measures and nGMV is solely related to atrophy, because lesions in the cortical gray matter are difficult to detect on MRI.
A longitudinal analysis in our cohort is currently under way. In addition to assessing the long-term correlation between HRQOL and radiographic burden of disease, we will also determine whether these HRQOL subscales predict subsequent brain atrophy and disability. In one study, early accumulation of fatigue was a better predictor of longer-term reductions in brain atrophy than the MSFC.37 Moreover, two small reports have suggested that some aspects of HRQOL are weakly associated with subsequent decline in physical function.39,40 Therefore, further evaluation of HRQOL as a predictor of MS outcomes should be pursued. If such predictive value can be established, patient-reported HRQOL may gain a more prominent role not only in the research arena, but also in the clinical care of patients with MS.
AUTHOR CONTRIBUTIONS
Statistical analyses were performed by E.M. Mowry.
ACKNOWLEDGMENT
The authors thank Dr. Patricia Katz for her constructive advice and the patients who generously agreed to serve as study participants.
Supplementary Material
Address correspondence and reprint requests to Dr. Ellen M. Mowry, University of California, San Francisco, UCSF Multiple Sclerosis Center, 350 Parnassus Ave., Suite 908, San Francisco, CA 94117 ellen.mowry@ucsf.edu
Supplemental data at www.neurology.org
Supported in part by grants from the NIH (NS26799, AI067152, R01 NS049477, U19 AI067152, K23 NS048869), the National Multiple Sclerosis Society (RG 3517), a research grant from GlaxoSmithKline, and gifts from the Signe Ostby Foundation and the Friends of Amy. This work was also made possible by a Partners MS Center Clinical Fellowship Award, a Genentech Fellowship Award, and a National Multiple Sclerosis Society Sylvia Lawry Fellowship Award (to E.M.M.). D.P. is a Harry Weaver Neuroscience Scholar of the National Multiple Sclerosis Society.
Disclosure: The authors report no disclosures.
Medical Device: 3-Tesla GE Excite scanner (GE Healthcare Technologies, Waukesha, WI).
Received December 4, 2008. Accepted in final form February 17, 2009.
REFERENCES
- 1.Nortvedt MW, Riise T, Myhr KM, Nyland HI. Quality of life in multiple sclerosis: measuring the disease effects more broadly. Neurology 1999;53:1098–1103. [DOI] [PubMed] [Google Scholar]
- 2.Miller DM, Kinkel RP. Health-related quality of life assessment in multiple sclerosis. Rev Neurol Dis 2008;5:56–64. [PubMed] [Google Scholar]
- 3.Pascual AM, Martinez-Bisbal MC, Bosca I, et al. Axonal loss is progressive and partly dissociated from lesion load in early multiple sclerosis. Neurology 2007;69:63–67. [DOI] [PubMed] [Google Scholar]
- 4.Henry RG, Shieh M, Okuda DT, Evangelista A, Gorno-Tempini ML, Pelletier D. Regional grey matter atrophy in clinically isolated syndromes at presentation. J Neurol Neurosurg Psychiatry 2008;79:1236–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chard DT, Griffin CM, Parker GJ, Kapoor R, Thompson AJ, Miller DH. Brain atrophy in clinically early relapsing remitting multiple sclerosis. Brain 2002;125:327–337. [DOI] [PubMed] [Google Scholar]
- 6.Simon JH, Jacobs LD, Campion MK, et al. A longitudinal study of brain atrophy in relapsing multiple sclerosis. The Multiple Sclerosis Collaborative Research Group. Neurology 1999;53:139–148. [DOI] [PubMed] [Google Scholar]
- 7.Trapp BD, Peterson J, Ransohoff RM, Rudick R, Mork S, Bo L. Axonal transection in the lesions of multiple sclerosis. N Engl J Med 1998;338:278–285. [DOI] [PubMed] [Google Scholar]
- 8.Janssens AC, van Doorn PA, de Boer JB, van der Meche FG, Passchier J, Hintzen RQ. Impact of recently diagnosed multiple sclerosis on quality of life, anxiety, depression and distress of partners. Acta Neurol Scand 2003;108:389–395. [DOI] [PubMed] [Google Scholar]
- 9.McDonald WI, Compston A, Edan G, et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the international panel on the diagnosis of multiple sclerosis. Ann Neurol 2001;50:121–127. [DOI] [PubMed] [Google Scholar]
- 10.Polman CH, Reingold SC, Edan G, et al. Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald criteria.” Ann Neurol 2005;58:840–846. [DOI] [PubMed] [Google Scholar]
- 11.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 1983;33:1444–1452. [DOI] [PubMed] [Google Scholar]
- 12.Fischer JS, Rudick RA, Cutter GR, Reingold SC. The multiple sclerosis functional composite measure (MSFC): an integrated approach to MS clinical outcome assessment. Mult Scler 1999;5:244–250. [DOI] [PubMed] [Google Scholar]
- 13.Cella DF, Dineen K, Arnason B, et al. Validation of the functional assessment of multiple sclerosis quality of life instrument. Neurology 1996;47:129–139. [DOI] [PubMed] [Google Scholar]
- 14.Blum D, Yonelinas AP, Luks T, et al. Dissociating perceptual and conceptual implicit memory in multiple sclerosis patients. Brain Cogn 2002;50:51–61. [DOI] [PubMed] [Google Scholar]
- 15.Samsa G, Edelman D, Rothman ML, Williams GR, Lipscomb J, Matchar D. Determining clinically important differences in health status measures. Pharmacoeconomics 1999;15:141–155. [DOI] [PubMed] [Google Scholar]
- 16.Arnoldus JH, Killestein J, Pfennings LE, Jelles B, Uitdehaag BM, Polman CH. Quality of life during the first 6 months of interferon-beta treatment in patients with MS. Mult Scler 2000;6:338–342. [DOI] [PubMed] [Google Scholar]
- 17.Rice GP, Oger J, Duquette P, et al. Treatment with interferon beta-1b improves quality of life in multiple sclerosis. Can J Neurol Sci 1999;26:276–282. [DOI] [PubMed] [Google Scholar]
- 18.Vittinghoff E, Glidden DV, Shiboski SC, McCullouch CE. Regression Methods in Biostatistics. New York: Springer Science & Business Media; 2005. [Google Scholar]
- 19.Dalton CM, Chard DT, Davies GR, et al. Early development of multiple sclerosis is associated with progressive grey matter atrophy in patients presenting with clinically isolated syndromes. Brain 2004;127:1101–1107. [DOI] [PubMed] [Google Scholar]
- 20.Losseff NA, Wang L, Lai HM, et al. Progressive cerebral atrophy in multiple sclerosis: a serial MRI study. Brain 1996;119:2009–2019. [DOI] [PubMed] [Google Scholar]
- 21.Fisher E, Lee JC, Nakamura K, Rudick RA. Gray matter atrophy in multiple sclerosis: a longitudinal study. Ann Neurol 2008;64:255–265. [DOI] [PubMed] [Google Scholar]
- 22.Fisniku LK, Chard DT, Jackson JS, et al. Gray matter atrophy is related to long-term disability in multiple sclerosis. Ann Neurol 2008;64:247–254. [DOI] [PubMed] [Google Scholar]
- 23.Fisher E, Rudick RA, Cutter G, et al. Relationship between brain atrophy and disability: an 8-year follow-up study of multiple sclerosis patients. Mult Scler 2000;6:373–377. [DOI] [PubMed] [Google Scholar]
- 24.van der Werf SP, Jongen PJ, Lycklama a Nijeholt GJ, et al. Fatigue in multiple sclerosis: interrelations between fatigue complaints, cerebral MRI abnormalities and neurological disability. J Neurol Sci 1998;160:164–170. [DOI] [PubMed] [Google Scholar]
- 25.Mainero C, Faroni J, Gasperini C, et al. Fatigue and magnetic resonance imaging activity in multiple sclerosis. J Neurol 1999;246:454–458. [DOI] [PubMed] [Google Scholar]
- 26.Bakshi R, Miletich RS, Henschel K, et al. Fatigue in multiple sclerosis: cross-sectional correlation with brain MRI findings in 71 patients. Neurology 1999;53:1151–1153. [DOI] [PubMed] [Google Scholar]
- 27.Janardhan V, Bakshi R. Quality of life and its relationship to brain lesions and atrophy on magnetic resonance images in 60 patients with multiple sclerosis. Arch Neurol 2000;57:1485–1491. [DOI] [PubMed] [Google Scholar]
- 28.Codella M, Rocca MA, Colombo B, Martinelli-Boneschi F, Comi G, Filippi M. Cerebral grey matter pathology and fatigue in patients with multiple sclerosis: a preliminary study. J Neurol Sci 2002;194:71–74. [DOI] [PubMed] [Google Scholar]
- 29.Codella M, Rocca MA, Colombo B, Rossi P, Comi G, Filippi M. A preliminary study of magnetization transfer and diffusion tensor MRI of multiple sclerosis patients with fatigue. J Neurol 2002;249:535–537. [DOI] [PubMed] [Google Scholar]
- 30.Marrie RA, Fisher E, Miller DM, Lee JC, Rudick RA. Association of fatigue and brain atrophy in multiple sclerosis. J Neurol Sci 2005;228:161–166. [DOI] [PubMed] [Google Scholar]
- 31.Filippi M, Rocca MA, Colombo B, et al. Functional magnetic resonance imaging correlates of fatigue in multiple sclerosis. Neuroimage 2002;15:559–567. [DOI] [PubMed] [Google Scholar]
- 32.Cook DB, O’Connor PJ, Lange G, Steffener J. Functional neuroimaging correlates of mental fatigue induced by cognition among chronic fatigue syndrome patients and controls. Neuroimage 2007;36:108–122. [DOI] [PubMed] [Google Scholar]
- 33.Rocca MA, Agosta F, Colombo B, et al. fMRI changes in relapsing-remitting multiple sclerosis patients complaining of fatigue after IFNβ-1A injection. Hum Brain Mapp 2007;28:373–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.de Lange FP, Kalkman JS, Bleijenberg G, Hagoort P, van der Meer JW, Toni I. Gray matter volume reduction in the chronic fatigue syndrome. Neuroimage 2005;26:777–781. [DOI] [PubMed] [Google Scholar]
- 35.Christodoulou C, Krupp LB, Liang Z, et al. Cognitive performance and MR markers of cerebral injury in cognitively impaired MS patients. Neurology 2003;60:1793–1798. [DOI] [PubMed] [Google Scholar]
- 36.Rovaris M, Filippi M, Falautano M, et al. Relation between MR abnormalities and patterns of cognitive impairment in multiple sclerosis. Neurology 1998;50:1601–1608. [DOI] [PubMed] [Google Scholar]
- 37.Benedict RH, Weinstock-Guttman B, Fishman I, Sharma J, Tjoa CW, Bakshi R. Prediction of neuropsychological impairment in multiple sclerosis: comparison of conventional magnetic resonance imaging measures of atrophy and lesion burden. Arch Neurol 2004;61:226–230. [DOI] [PubMed] [Google Scholar]
- 38.Zivadinov R, Sepcic J, Nasuelli D, et al. A longitudinal study of brain atrophy and cognitive disturbances in the early phase of relapsing-remitting multiple sclerosis. J Neurol Neurosurg Psychiatry 2001;70:773–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Visschedijk MA, Uitdehaag BM, Klein M, et al. Value of health-related quality of life to predict disability course in multiple sclerosis. Neurology 2004;63:2046–2050. [DOI] [PubMed] [Google Scholar]
- 40.Nortvedt MW, Riise T, Myhr KM, Nyland HI. Quality of life as predictor for change in disability in MS. Neurology 2000;55:51–54. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


