Abstract
Adhesion of platelets to blood vessel walls is a shear stress dependent process that promotes arrest of bleeding and is mediated by the interaction of receptors expressed on platelets with various extracellular matrix (ECM) proteins that may become exposed upon vascular injury. Studies of dynamic platelet adhesion to ECM-coated substrates in conventional flow chambers require substantial fluid volumes and are difficult to perform with blood samples from a single laboratory mouse. Here we report dynamic platelet adhesion assays in two new microfluidic devices made of PDMS. Small cross-sections of the flow chambers in the devices reduce the blood volume requirements to <100 microliters per assay, making the assays compatible with samples of whole blood obtained from a single mouse. One device has an array of 8 flow chambers with shear stress varying by a factor of 1.93 between adjacent chambers, covering a 100-fold range from low venous to arterial. The other device allows simultaneous high-resolution fluorescence imaging of dynamic adhesion of platelets from two different blood samples. Adhesion of platelets in the devices to three common ECM substrate coatings was verified to conform with published results. The devices were subsequently used to study the roles of extracellular and intracellular domains of integrin αIIbβ3, a platelet receptor that is a central mediator of platelet aggregation and thrombus formation. The study involved wild-type mice and two genetically modified mouse strains and showed that the absence of the integrin impaired adhesion at all shear stresses, whereas a mutation in its intracellular domain reduced the adhesion only at moderate and high stresses. Because of small sample volumes required, the devices could be employed in research with genetically-modified model organisms and for adhesion tests in clinical settings with blood from neonates.
INTRODUCTION
Regulated reactivity of platelets to extracellular matrices (ECM) is fundamental to thrombosis and stoppage of bleeding. Vascular injury and atherosclerotic plaque rupture expose ECM on which platelets may be captured from bulk blood transport and adhere through multiple receptors. These receptors, including GPIb-IX-V for von Willebrand factor (VWF) and GPVI and α2β1 for collagen, cooperate to stimulate complex “inside-out” signaling networks that activate integrin αIIbβ3 (reviewed in Ref. 1), resulting in stable platelet capture to ECM and thrombus growth.2, 3 Atherosclerotic lesions have been reported to contain adsorbed fibrinogen,4 which can be recognized by non-activated platelet αIIbβ3.5 Furthermore, platelet-vessel wall interactions may promote leukocyte recruitment, which has an impact on atherogenesis, inflammation and pathological thrombosis.6, 7
Because of the importance of inside-out αIIbβ3 signaling for platelet function, it has been investigated in some detail. A current model holds that a final step in effecting the requisite conformational change and activation of the integrin involves the binding of talin to the β3 cytoplasmic tail of the integrin.8, 9 Support for this model is provided by recent studies of a strain of knock-in mice (β3Y747A) harboring a point mutation in the β3 tail (Y747A) that abrogates interaction with talin and other integrin binding proteins.10 Platelets from these mice exhibit deficient agonist-induced platelet activation in vitro and impaired thrombus formation in vivo. However, no detailed study has been made on how this mutation affects the adhesion of platelets under physiologically relevant shear conditions.
In the circulation, platelets experience a wide range of shear stresses from approximately 0.8–8 dynes/cm2 in the venous circulation to 10–60 dynes/cm2 in the arterial circulation.11 Various flow devices, particularly parallel plate flow chambers, have been used in ex vivo platelet studies to mimic flow conditions occurring in vivo.12,5 Conventional flow chambers often have a depth of 0.1–0.3 mm and a width of 2–10 mm, requiring a relatively large volume of blood (milliliters) for an assay. For tests with mouse blood, this volume is often obtained by mixing blood samples drawn from several laboratory animals. In addition, conventional flow chambers typically test adhesion at a single shear stress or in a small range of shear stresses per experiment. Therefore, studies of platelet adhesion over the entire physiological range of shear stresses are costly in terms of time and laboratory animals. The sample volume requirements are dramatically reduced in microfluidic flow chambers. Microfluidic perfusion chambers have been applied to capturing different sub-populations of lymphocytes to substrates with various coatings from continuous flow13,14 and testing the strength of adhesion of different cells to a substratum.15,16 Recently, microfluidic devices were used to study initiation of blood clotting17 particle adhesion in complex channel networks,18 the dynamics of adhesion of infected erythrocytes to different substrata19 and of neutrophils to endothelial monolayers.20 However, the microfluidic technology has not yet been applied to studies of shear-dependent trends in platelet adhesion.
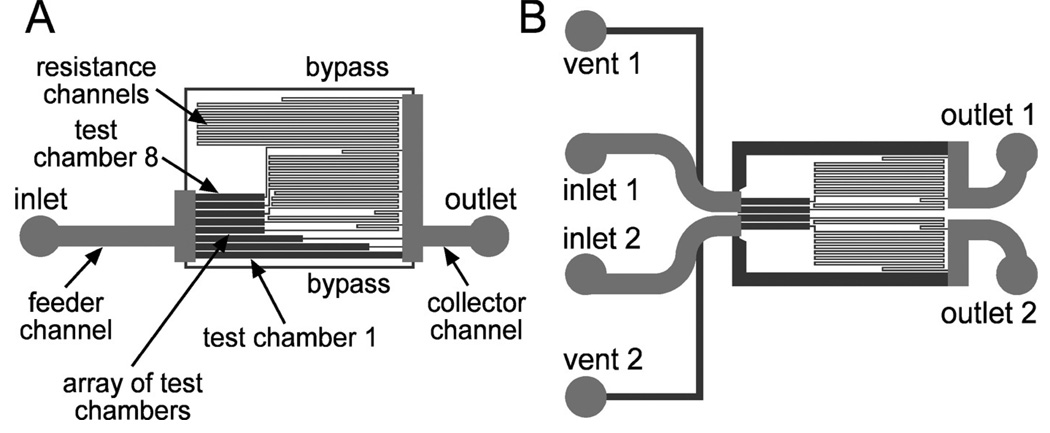
Here we report platelet adhesion assays in two novel microfluidic devices (Fig. 1). Both devices have flow chambers with a small cross-section, resulting in a blood consumption of 2–3 orders of magnitude less than in conventional flow chambers and making it possible to run tests with blood samples obtained from a single laboratory mouse. Device 1 (Fig. 1A) has an array of 8 identical rectilinear flow chambers with shear stresses, τ, varying by a factor of 1.93 between adjacent chambers, thus covering a 100-fold range in τ, representative of low venous to arterial blood flow. Device 2 (Fig. 1B) is similar to device 1, but consists of two separate mirror-symmetric microchannel networks, permitting observation of dynamic adhesion of platelets from two different blood samples in a single field of view of a high-resolution fluorescence imaging setup.
Figure 1.
Drawings of microchannel networks of the two microfluidic devices used in the study: A. device 1 and B. device 2. 24 µm and 250 µm deep channels are shown in dark and light grey, respectively. The 250 µm deep feeder channels minimize the shear stress on the way from the inlet to the test chamber and, just as the collector channels, have low flow resistance and nearly uniform pressure in them. Flow rate through the 24 µm test chambers is set by the flow resistance of the resistance channels connected in series with the test chambers. The flow rate is highest for the test chamber 1 and lowest for the test chamber 8. The bypass channels help synchronize the injection of blood into different test chambers.
To test the devices and validate their application to platelet adhesion assays, we first verified that the dynamic adhesion of platelets to substrates coated with three commonly used ECM molecules (fibrinogen, collagen, and VWF) occurred in agreement with previous reports. To demonstrate the utility of the proposed microfluidic devices for biological studies, we used the devices to explore the role of integrin αIIbβ3 in dynamic adhesion of platelets to fibrinogen and collagen in the physiological range of shear stresses, τ. The study was performed with blood from normal mice (β3+/+) and mice whose platelets either lack αIIbβ3 (β3−/−), or have normal extracellular domains, but are activation-defective by virtue of a point mutation in the β3 cytoplasmic domain (β3Y747A). The results showed that the dynamic adhesion of platelets that lack αIIbβ3 was strongly impaired at all τ, whereas the adhesion of the activation defective mutant was only reduced at intermediate and high τ. Furthermore, β3−/− (and β3Y747A) platelets that adhered to collagen did not form aggregates and remained as a monolayer, thus enabling the use of the microfluidic devices for exploring the rolling and arrest of granulocytes on platelet monolayers.
Experimental
Construction and operation of microfluidic devices
Microfluidic devices (Fig. 1) consisted of PDMS chips sealed with #1.5 microscope coverglasses. The chips were cast out of PDMS (Sylgard 184 by Dow Corning) using master molds fabricated with a two-step protocol described in detail elsewhere.21 The mold fabrication involved two consecutive coatings of a silicon wafer with different formulations of a UV-curable epoxy, SU8 (Microchem, Newton, MA), and their exposure to UV-light through two different photomasks. All test chambers (flow chambers) in both microfluidic devices (Fig. 1) had a depth h = 24 µm and a width w = 200 µm. The substratum shear rate, γ̇, in an internal region of a test chamber (away from the side walls) is found as γ̇ ≍ 6ν̅/h, where ν̅ is the mean flow velocity in the chamber. The substratum shear stress is given by τ ≍ 6ν̅η/h, where η ≍ 0.038 Ps is the viscosity of blood. (A shear rate γ̇ = 1 s−1 corresponds to a shear stress τ = 0.038 dyne/cm2.) The volumetric flow rate, Q, through a test chamber is found as Q = whν̅ ≍ wh2γ̇/6 = wh2τ/(6η)The rate of consumption of blood at a given shear stress is proportional to the chamber width and to the chamber depth squared and is ∼340 times lower for the microfluidic devices than for a 0.125×2.5 mm commercial flow chamber (GlycoTech Inc., MD).
The microfluidic device 1 (Fig. 1A) had one inlet, one outlet and an array of 8 parallel test chambers. All test chambers, except for test chamber 1, were connected at their exits to resistance channels (24 µm deep and 40 µm wide). A test chamber and its resistance channel constituted a channel line. Each channel line was connected to the feeder channel on the upstream side and to the collector channel on the downstream side (Fig. 1A). The feeder and collector channels were both ∼250 µm deep and ∼500 µm wide, making their flow resistances negligible compared with those of the 24 µm deep channel lines, and providing equal pressures at the entrances and equal pressures at the exits of all 8 channel lines. Thus the differential pressures, ΔP, across the 8 channel lines were all equal to each other and equal to the difference in pressure between the inlet and outlet of the device. The volumetric flow rate, Q, through a test chamber is found as Q = ΔP/R where R is the cumulative hydrodynamic resistance of the channel line. The values of R were designed to vary by a factor of 1.93 between adjacent channel lines, thus providing a 1.93-fold change in Q and shear stress, τ, between adjacent test chambers, with a total 100-fold variation between the test chambers 1 and 8. We note that the microchannel architecture of device 1 was essentially different from the architectures of some perfusion devices described earlier, where shear stress variations were achieved by varying the width of the flow chambers, limiting the variations to about one order of magnitude.12, 13, 15, 16
Because of the large cross-section of the feeder channel as compared with the test chambers, the shear stress in the feeder channel was ∼2 times lower than the lowest shear stress in the test chambers (found in the chamber 8), resulting in a minimal activation of platelets by shear stress prior to their arrival at the test chambers. Bypass channels at the edges of the test chamber array (Fig. 1) had relatively low flow resistance and were added to suppress the formation of air bubbles in the corners and to better synchronize the arrival of blood at different test chambers.
The microfluidic device 2 (Fig. 1B) had a set of two identical (mirror-symmetric) disconnected microchannel networks that were placed in close proximity of each other. Each network had an inlet, an outlet, and a vent port, marked by numbers 1 and 2 for networks 1 and 2, respectively. Each network had two separate channel lines identical to two of the channel lines of device 1 (cf. Fig. 1A). For the device in Fig. 1B, these two channel lines were 1 and 3, with test chambers 1 of the two microchannel networks adjacent to each other with a 40 µm partition between them. (We also used two other versions of device 2, in which the adjacent test chambers were from channel lines 3 and 5.)
Flow control
Flow in the microfluidic devices was driven by differential hydrostatic pressure, ΔP, applied between the inlet and outlet, generated by gravity, and controlled within ∼10 Pa.21 Care was taken to prevent platelet activation by avoiding exposure of blood to glass or metal components: blood and buffer solutions used in the experiments were kept in plastic syringes (1 mL and 10 mL) connected to the device through flexible Tygon tubing (0.5 mm inner diameter) and short polyimide capillaries that were inserted into the device ports.
Reagents and blood preparation
Function-blocking monoclonal antibody 1B5 against murine αIIbβ3 was from Dr. Barry Coller (Rockefeller University, New York, NY).22 Monoclonal antibody AP-1 against human GP Ibα was from Dr. Thomas Kunicki (Scripps Research Institute, La Jolla, CA).23 Monoclonal antibody 5H1 against mouse P-selectin24 was from Dr. Rodger McEver (Oklahoma Medical Research Foundation, Oklahoma City, OK), and a polyclonal anti-mouse PSGL-1 blocking antibody was from Dr. Bruce Furie (Harvard University, Boston, MA).25 Integrilin, a selective antagonist to human or murine αIIbβ3 26 was from Dr. David Phillips (Portola Pharmaceuticals, Inc., South San Francisco, CA). Non-function-blocking antibodies to αIIb and granulocyte Ly-6 (Gr-1) were from Invitrogen/BD Biosciences (Carlsbad, CA), as were control IgG antibodies. Human plasma VWF was a gift from Dr. Zaverio Ruggeri (Scripps Research Institute, La Jolla CA).27 Fibrinogen was from Enzyme Research Co (South Bend, IN). All other reagents were from Sigma Chemical Co. (St. Louis, MO). 1.9 µm fluorescent beads, used to measure the flow rates by particle tracking, were purchased from Bangs Laboratories (Fishers, IN).
Human blood obtained from normal, drug-free donors was anticoagulated with 20 U/mL heparin, which maintains normal calcium concentrations and does not interfere with the platelet adhesion assays.28 Mouse blood was drawn by cardiac puncture into heparin-containing syringes. Mice deficient in integrin β3 (β3−/−)29 were obtained from Jackson Laboratories (Bar Harbor, Maine), and β3 knock-in mice (β3Y747A) were generated at UCSD.10 Wild-type mice (β3+/+) represented littermate controls. The platelet counts of mice of all three genotypes were similar.
Experimental protocol
Platelets were visualized by adding 2 µM mepacrine5 to whole blood to label dense granules. At high concentrations, mepacrine (which also labels leukocytes) may inhibit phospholipase A2. Nevertheless at 2 µM, platelet and leukocyte functions are maintained. 5, 30 For studies of platelet-granulocyte interactions, granulocytes in whole blood were additionally labeled with 16 µg/mL of a phycoerythrin (PE)-conjugated anti-Gr-1 antibody. No bleed-through occurred between the green fluorescence of mepacrine and red fluorescence of phycoerythrin. All inhibitors were added 25 min prior to onset of blood flow through the device, except ethanol control and prostaglandin E1 (PGE1), that were added 5 min prior to flow onset.
To coat the glass substrata of the microfluidic devices with physiological matrices, the microchannels were filled with 20 µg/mL fibrinogen, 300 µg/mL acid-soluble Type I collagen or 10 µg/mL VWF, and incubated for 1 hour at room temperature. Subsequently, the devices were rinsed with an excessive amount of Hepes buffer (150 mM NaCl, 20 mM Hepes, pH 7.4) or rinsed with buffer and then blocked with 1% BSA for another 30 minutes, with similar results. The flow through the device was stopped by clamping the Tygon tubing, and the outlet syringe was placed at a level of ∼10 cm above the microscope stage. 200 µl of human or mouse blood with or without indicated inhibitors was gently drawn into a 1 cc plastic syringe through a Tygon tubing line by pushing the plunger to ∼1/5 of the syringe length, immersing the tubing into blood, pulling the plunger to the end of the syringe (thus creating a gauge pressure of −1/5 atm), waiting till the amount of blood in the syringe reached ∼100 µL (plus ∼100 µL in the tubing), and then quickly removing the plunger. The tubing was then connected to the device inlet. The inlet was pressurized at ΔP = 2.5 kPa with respect to the outlet by raising the syringe with the blood so that the level of blood was 25 cm the above the level of the buffer in the outlet syringe. Alternatively, ∼100 µL of mouse blood was loaded into a 0.5 mL Eppendorf tube that was sealed by a PDMS plug with two openings, for a luer stub connecting the tube to a source of compressed air with a pressure P = 2.5 kPa, and for PE 10 polyethylene tubing. One end of the tubing line (that was ∼10 cm long) was touching the bottom of the tube, and its other end was directly inserted into the device port. Because of small volume of blood in the polyethylene tubing line (∼6 µL), almost entire blood sample loaded into the Eppendorf tube could be used for perfusion experiments.
For the device 1 (Fig. 1A), flow of blood through the device was initiated by removing the clamp from the outlet tubing. Because of relatively low volume of buffer between the test channels and the tubing with the blood (∼0.5 µL) and relatively high total volumetric flow rate through the device (∼3.7 µL/min), the transient time of injection of blood into the test channels was only ∼8 sec, which was substantially shorter than the duration of adhesion assays. In the device 2 (Fig. 1B), there were four syringes with buffer connected to the outlets and vents of each of the two microchannel networks (marked by numbers 1 and 2 in Fig. 1B) through four separate Tygon tubing lines. The lines connected to both outlets were initially clamped, and when the syringes with blood were connected to the inlets, the flow of blood was from the inlets to the vents. Once the buffer was purged from the channels connecting the inlets with the vents, and the channels were filled with whole blood, the vent tubing lines were clamped, completely stopping the flow through the device. The adhesion assay was started by simultaneous removal of the clamps from both outlet lines, thus starting flow of blood from inlets 1 and 2 to outlets 1 and 2, respectively (Fig. 1B). At that moment, blood in both networks was separated from the test chambers by small and equal volumes of buffer in the feeder channels. Therefore, the arrival of blood at the test chambers was synchronized within less than a second and occurred within less than a second from the moment of clamp removal. The duration of a perfusion experiment was <10 min, and the total consumption of blood during an experiment was <40 µL (<100 µL with occasional sample loss during tubing reconnection). Cells were counted as stably attached if they moved by less than one cell diameter in 10 seconds. To fix cells after an adhesion assay, the device was perfused with 3.7% formaldehyde and incubated for 10 minutes. The device was then disassembled and coverglasses were rinsed with Hepes buffer.
Image acquisition and analysis
In the experiments with device 1 (Fig. 1A), the microfluidic device was mounted on a mechanical stage of a Nikon Diaphot inverted fluorescence microscope that was equipped with a Newport 850G linear actuator. The actuator was driving the stage in the direction perpendicular to the direction of flow in the test chambers and enabled moving the field of view of the microscope between different test chambers with a 5 µm positioning accuracy. Fluorescence microscopy was performed with a Nikon 100W mercury light source and a GFP filter set (Ex470/Em525). The images of the platelets were acquired with a 63×, NA=1.4 oil immersion objective lens, a 0.42× video adapter, and a Sony SX900 IEEE1394 camera with a 1/2", 1280×960 pixel CCD array. An ND8 neutral density filter was used to reduce the intensity of fluorescence illumination and minimize platelet photoactivation.31 Motion of the stage and image acquisition were controlled through RS232 and IEEE1394 interfaces, respectively, using a code in LabView7.1 (National Instruments, Austin, TX). The stage was programmed to move in periodic scanning loops between test chambers 1–8, with eight stops to take a fluorescence image of each chamber. One scanning loop took 16 sec that set the interval between consecutive images of individual test chambers. The images were acquired at ∼400 µm from the beginning of the test chambers.
In the experiments with device 2, when the adhesion of platelets from two different blood samples was simultaneously monitored, the device was mounted on a Nikon TE2000 inverted fluorescence microscope. The imaging was performed with a 40×, NA=1.3 PlanFluor oil immersion objective lens, a 0.42× Diagnostic Instruments video adapter, and a Hamamatsu C4742–95 IEEE1394 camera with a 2/3”, 1280×1024 pixels CCD array. The field of view of this video microscopy setup was 500×375 µm that allowed imaging the entire width of two adjacent test chambers (440 µm including a 40 µm partition) with different blood samples in them (Fig. 4B). For fluorescence microscopy, we used a Nikon 100W mercury light source, and either a FITC filter set (Ex470/Em535) for stained platelets or a TRITC-HQ filter (Ex545/Em620) for stained granulocytes.
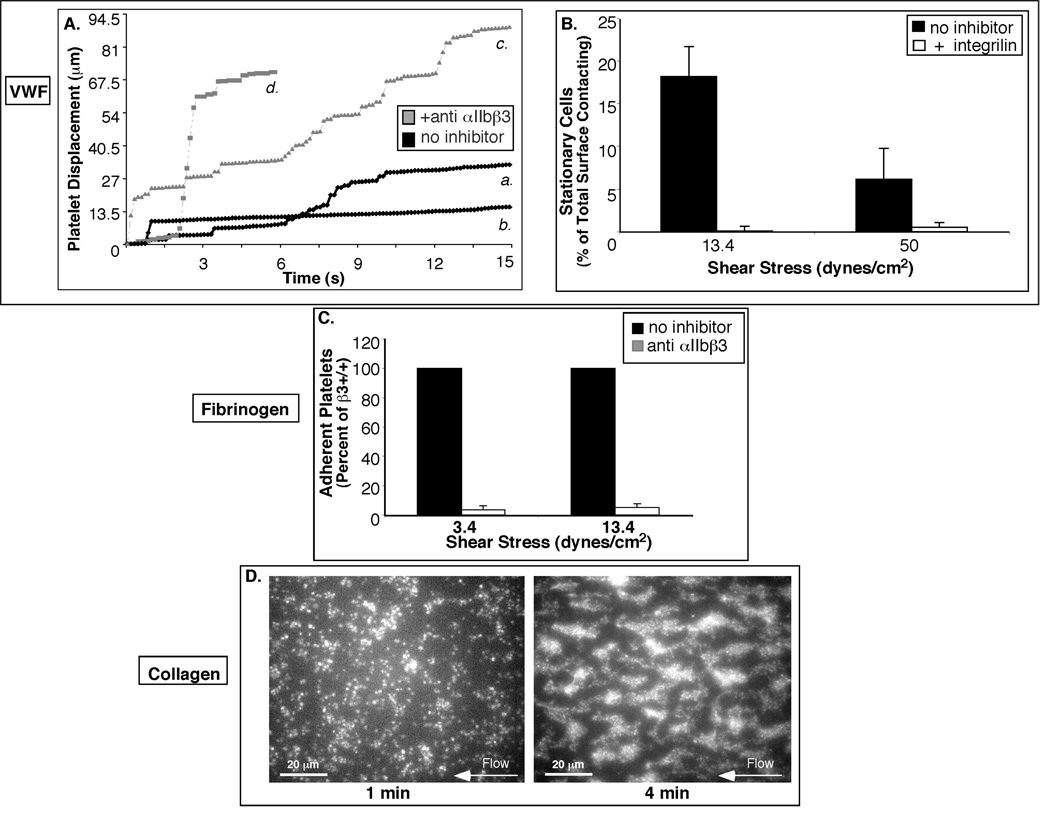
Figure 4.
Dynamic adhesion of platelets to collagen depends on the presence of αIIbβ3 and its cytoplasmic tail associations. A. Fluorescence micrographs of test chambers with β3+/+ (left panel) and β3−/− (right panel) blood after 2 minutes of flow at 3.4 dynes/cm2. β3+/+ but not β3−/− platelets exhibit characteristic thrombus growth. B. Adhesion of β3+/+ and β3−/− platelets to collagen in the two adjacent test chambers of the device 2 after 2 min of flow at 50 dynes/cm2 as evaluated from a fluorescence micrograph. Surface coverage by mepacrine-labeled platelets is represented by color-coded fluorescence intensity (red corresponds to highest platelet density). Data shown is representative of at least 3 separate experiments. C. Histogram of the levels of attachment of β3+/+ and β3Y747A platelets to collagen after 1 minute of flow. Data are depicted as the total integrated fluorescence intensity for the field in arbitrary units (a.u.), and are an average of 3 separate experiments ± SEM.
Quantification of adherent platelets, as well as velocity measurements by platelet tracking were performed using Image ProPlus (Media Cybernetics, Silver Spring, MD) at the UCSD Neurosciences Core Microscopy Center (NINDS grant no. NS047101).
Results
Characterization of Flow
Flow velocity in the test chambers was measured using a 50% aqueous solution of ethylene glycol, with viscosity matching the standard viscosity of mouse blood, η = 0.038 Ps, by seeding the solution with fluorescent beads and analyzing their streaklines. The measurements were done at the driving pressure, ΔP = 2.5 kPa, used in all platelet adhesion assays. The ratios between the values of maximal flow velocity, νmax, in adjacent test chambers in the device 1 were close to the target ratio of 1.93 (Table 1). Shear stresses in the test chambers, calculated as τ = 4νmaxη/h, assuming a fully developed laminar shear flow, covered a range of 0.5 – 50 dyne/cm2. The Reynolds number in the test chambers can be calculated as Re = ρν̅h/η, where ρ =1.05 g/cm3 is the density of blood. The values of Re in the test chambers were always low, ∼0.1 in the chamber 1 and <0.1 in the other chambers, suggesting that the flow was always laminar with negligible non-linear effects. The total volumetric flow rate through the device 1 was 3.7 µL/min.
Table 1.
Results of characterization of device 1 with flow of 50% aqueous solution of ethylene glycol (η = 3.8 cPs) driven by a differential pressure ΔP = 2.5 kPa between the inlet and outlet. Experimentally measured maximal flow velocities, νmax, in the test chambers 1–8 are shown along with the values of substrate shear rate, γ̇, and shear stress, τ, calculated from νmax as γ̇ = 4νmax/h and τ = 4νmaxη/h, respectively. The experimental values of τ are contrasted with shear stress values derived theoretically using the geometrical parameters of the channel lines and equations for laminar flow hydrodynamic resistances of rectangular channels. The uncertainly in the measurements of νmax was ∼3% and it propagated into uncertainties of the shear rate and shear stress.
| Test Chamber | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| νmax (mm/s) | 7.8 | 4.3 | 2.11 | 1.12 | 0.54 | 0.279 | 0.135 | 0.082 |
| Shear Rate (s−1) | 1310 | 720 | 351 | 184 | 89 | 47 | 22.5 | 13.6 |
| Shear Stress (dynes/cm2) | 50 | 27.5 | 13.4 | 7.0 | 3.4 | 1.77 | 0.86 | 0.50 |
| Theoretical Shear Stress (dynes/cm2) | 50 | 25.8 | 13.4 | 6.9 | 3.6 | 1.86 | 0.97 | 0.50 |
In a steady laminar flow in a microchannel driven by differential pressure, shear stress is a function of the pressure, ΔP, and channel geometry only and does not depend on the viscosity of the fluid. Therefore, the actual viscosity of the blood samples (that could be different from the standard value of 0.038 Ps) was not measured. For example, in a wide and shallow rectilinear channel, such as the test chamber 1 (Fig. 1A), in a region away from the side walls, the surface shear stress, τ, is found from the equation (ΔP/L)h = 2τ, where L is the channel length. The equation predicts a shear stress τ = ΔPh/(2L)= 50 dyne/cm2 for the 6 mm long test chamber 1, the same as the value of τ measured experimentally. Because the surface shear stress is proportional to the channel depth, adhesion of platelets to the substrate is expected to reduce the shear stress. An adherent platelet has a height of ∼1 µm, which is ∼4% of the channel depth. All quantitative results reported in this paper were obtained when platelets covered only a part of the substrate surface and before they started aggregating (platelet monolayer), thus limiting the expected reduction of the surface shear stress due to the platelet adhesion to <4%.
Validation of Platelet Adhesion to Common Physiological Matrices
Almost no platelets adhered to the glass substratum coated with BSA (≤5 platelets in a 180×240 µm field of view after 3 min perfusion at any of the shear stresses tested), indicating minimal non-specific adhesion (cf. Fig. 2D and Fig. 3A, left). No platelets attached to PDMS walls of the test chambers. Platelet adhesion to physiological substrata may involve different braking, stabilization or thrombus growth events depending on the matrix presented. Therefore in order to assess the suitability of microfluidic devices for platelet adhesion studies, we tested whether the adhesion to three common physiologic matrices, VWF, fibrinogen, and collagen, occurred in a manner consistent with previous reports.
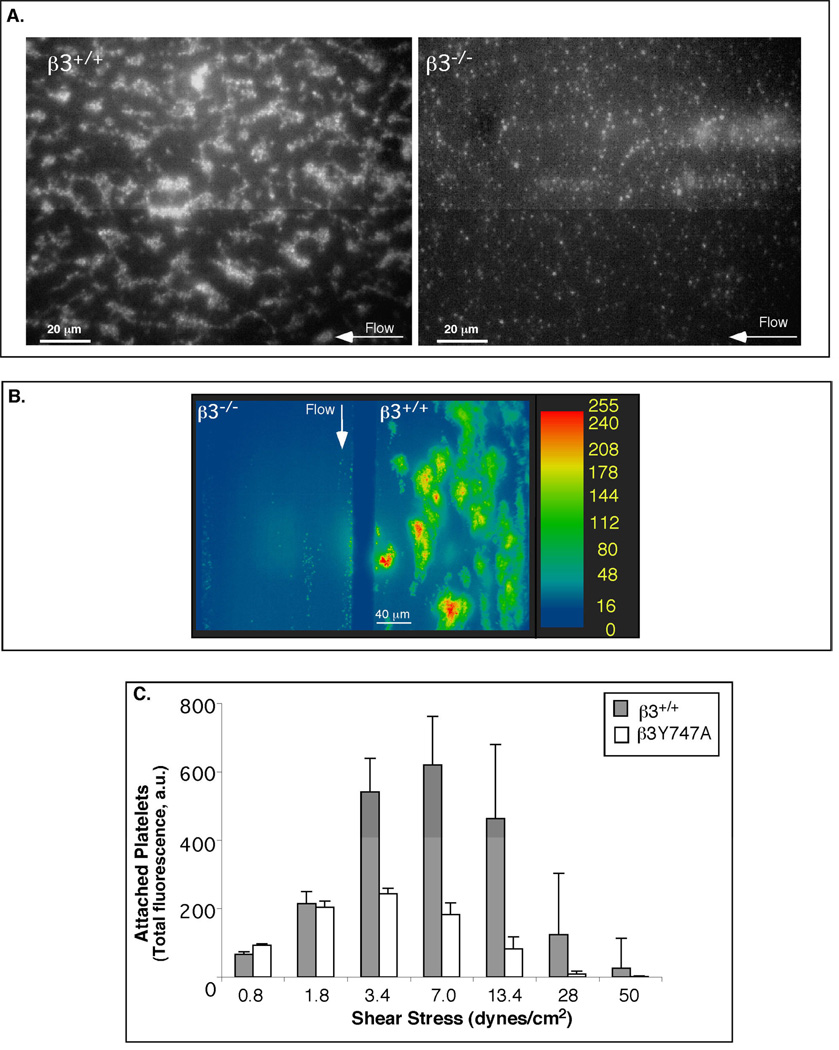
Figure 2.
Validation of platelet adhesion to physiologic matrices in microfluidic devices. A. Representative trajectories of individual platelets on VWF without inhibitor (black symbols; a and b) and with 20 µM integrilin, an anti-αIIbβ3 antagonist (grey symbols; c and d). Long plateaus correspond to prolonged periods of rest (a) that may lead to stable attachment (b) and are only observed for untreated cells. All platelet surface interactions are abolished in the presence of 10 µg/mL AP-1, an anti-GPIbα antibody (not shown). B. Histogram of the fraction of untreated cells and cells treated with integrilin that become stably attached to VWF at 3.4 and 50 dynes/cm2 after 1 min of flow. C. Adhesion to fibrinogen is αIIbβ3 dependent. Whole blood was incubated with or without 15 µg/mL Ib5, an anti-murine αIIbβ3 monoclonal antibody, and the platelet adhesion to fibrinogen was determined after 1 min of flow at τ = 3.4 and 13.4 dynes/cm2. Average values of 3 separate experiments ± SEM are shown. D. Fluorescence micrographs of a test chamber with collagen matrix in the device 1 at 13.4 dynes/cm2 showing normal thrombus growth from whole blood. After 1 minute of flow (left panel), there is a monolayer of adherent platelets serving as nucleation centers that develop into thrombi after 4 min of flow (right panel).
Figure 3.
Dynamic adhesion of platelets to fibrinogen depends on the presence of αIIbβ3 and its cytoplasmic tail associations. A. Fluorescence micrographs showing adhesion of β3+/+ (left panel) and β3−/− platelets (right panel) to fibrinogen at 3.4 dynes/cm2, after 1 min of flow. B.C. Histograms of numbers of β3+/+ and β3Y747A platelets attached to fibrinogen within the field of view at different shear stresses in the device 1. B. Attachment to fibrinogen after 1 and 2 min of flow (average of 4 separate experiments). C. Whole blood from β3+/+ or β3Y747A mice was pre-incubated with PGE1 or ethanol vehicle control and then perfused over fibrinogen. Average values of 3 separate experiments ± SEM after 1 minute of flow are shown.
Adhesion to VWF
Platelets interacting with VWF-coated substrata first translocate on VWF via GPIb-IX-V tethering5 and subsequently induce signaling pathways that activate αIIbβ3 32 for stable attachment. We used substrata coated with human VWF and assayed platelet adhesion to the substrata using human whole blood, because mouse platelets do not recognize human VWF and mouse VWF was not available. For an untreated blood sample, trajectories of individual platelets on VWF displayed intermittent intervals of translocation and rest (Fig. 2A). After 1 min of flow at 13.4 and 50 dynes/cm2, respectively, 18.2±8 and 6.6±3 % of platelets that interacted with the substratum within the field of view were stably attached to the substratum (Fig. 2B). Pretreatment of blood with an αIIbβ3 antagonist, integrilin, abolished stable attachment (Fig. 2B), and platelets showed increased translocation and shortened rest periods (Fig. 2A). No platelet-VWF surface interactions occurred in the presence of an antibody against GPIbα (not shown), confirming that initial platelet interactions with VWF were dependent on GPIb-IX-V.
Adhesion to fibrinogen and collagen
As we subsequently intended to use mouse models to investigate αIIbβ3-dependent adhesion to fibrinogen and collagen, further validations were performed using mouse blood. We assayed the adhesion dynamics of mouse platelets to fibrinogen-coated substrata using human fibrinogen, which mouse platelets are known to recognize via αIIbβ3;33 purified murine fibrinogen is not readily available. At both shear stresses tested, 3.4 and 13.4 dynes/cm2, wild-type platelets were captured from the bulk of flowing blood and were immediately arrested on immobilized fibrinogen. As expected, this platelet adhesion to fibrinogen was αIIbβ3 dependent, since it was almost completely inhibited (% I = 89.0 ± 2.4 %) by a function-blocking antibody against αIIbβ3 (Fig. 2C). Thus, the adhesion assay in the microfluidic device specifically reports on αIIbβ3-dependent platelet arrest on a fibrinogen matrix.
Collagen stimulates platelets through the two primary collagen receptors, GP VI and integrin α2β1, and induces αIIbβ3 activation that is required for aggregation of platelets and their incorporation into thrombi.34, 35 In agreement with the existing literature36 on platelet adhesion to collagen-coated substrata, wild-type platelets initially formed monolayers that induced platelet aggregation and thrombus formation (Fig. 2D).
The results of the assays described above agree with previous reports on platelet interactions with VWF, fibrinogen, and collagen-coated substrata, and thus indicate that the proposed microfluidic devices are appropriate tools to study shear-dependent platelet adhesion.
The role of αIIbβ3 extracellular domains and cytoplasmic tail associations in dynamic platelet adhesion to fibrinogen and collagen
Similar to human platelets,5, 37 wild-type mouse platelets (β3+/+) attached to fibrinogen in a shear stress dependent manner, with maximal attachment found at τ between 3.4 and 7 dynes/cm2 (Fig. 3 A,B). Platelets from knockout littermate mice lacking αIIbβ3 (β3−/−) 29 minimally attached to fibrinogen at any of the shear stresses tested (Fig. 3A), confirming that the adhesion of β3+/+ platelets to fibrinogen was critically dependent on αIIbβ3.
To study how the reduced αIIbβ3 activation and loss of cytoplasmic associations of αIIbβ3 due to the β3 Tyr 747 mutation modulate platelet adhesion to fibrinogen, we repeated the same flow experiments using blood from knock-in β3Y747A mice. In sharp contrast to β3−/− platelets, β3Y747A platelets were able to attach to fibrinogen at low shear stresses, attaining 50–80% of the attachment observed for β3+/+ littermate controls at τ ≤ 1.8 dynes/cm2 (Fig. 3B). This result was consistent with the close to 100% adhesion of β3Y747A platelets under static conditions.10 Nevertheless, the loss of β3 intracellular linkages became a more crucial factor at higher shear stresses: after 1 min of flow, the attachment of β3Y747A platelets was only 25.4 ± 6.8 % of β3+/+ controls (n = 5, p< 0.01) at τ = 3.4 dynes/cm2 and was minimal at τ > 7 dynes/cm2. Furthermore, β3+/+ platelets treated with PGE1 to inhibit αIIbβ3 activation had similar levels of adhesion to fibrinogen and shear stress dependence as β3Y747A platelets (e.g. 19.5 ±3.9% of untreated β3+/+ platelets at 3.4 dynes/cm2; p< 0.01, n = 3) (Fig. 3C). Therefore, linkage of the β3 cytoplasmic tail to intracellular proteins that promote its activation and stabilize it serve to enhance the platelet attachment to fibrinogen at τ = 3.4 – 13.4 dynes/cm2.
In contrast to the major differences observed in adhesion to fibrinogen, β3+/+, β3−/−, and β3Y747A platelets were all able to establish initial monolayers on collagen (Fig. 4A, right panel). Nevertheless, β3−/− and β3Y747A adherent platelets remained solitary, whereas most of the adherent β3+/+ platelets seeded recruitment of platelets from flow into small aggregate islands (thrombi) that expanded into a sheet-like structure (Fig. 4A, left panel). The aggregate formation was abolished when β3+/+ platelet activation was inhibited with PGE1 (not shown). Together with the lack of aggregate formation by β3−/− and β3Y747A platelets, this result suggested that αIIbβ3 must be present and retain intact cytoplasmic linkages that promote its activation in order to bind soluble ligands and form platelet aggregates on collagen.
In addition to its critical role in thrombus formation, the presence of αIIbβ3 strongly influenced the rate of primary attachment of platelets to collagen at arterial shear stresses (τS = 50 dynes/cm2; %I β3−/− attachment relative to β3+/+ controls: 93.7±5% (p<0.01) (Fig. 4B shown for β3−/− platelets). The reduced rate of primary attachment of β3−/− platelets to collagen was observed at all shear stresses, and the disparity between β3−/− and β3+/+ platelets increased with shear stress. For instance, after 1 min of flow, the surface coverage by β3−/− at τ = 0.8, 13.4, and 50 dynes/cm2 was reduced compared with β3+/+ platelets by 56, 78, and 94%, respectively, (n = 3; p<0.05). The extent of platelet adhesion was also severely compromised even after several minutes of flow at higher shear stresses. Thus, in the absence of αIIbβ3, interactions through GPVI and α2β1 alone cannot provide the strong attachment to collagen characteristic of wild-type platelets. The presence of a normal extracellular αIIbβ3 domain on β3Y747A platelets provided wild-type levels of attachment to collagen at low shear stresses (τ ≤ 1.8 dynes/cm2). Nevertheless, the attachment of β3Y747A platelets was still greatly reduced relative to β3+/+ platelets at τ ≥ 3.4 dynes/cm2 (Fig. 4C). This finding suggests that the contribution of integrin αIIbβ3 to primary platelet attachment to collagen at intermediate and high shear stresses strongly depends on the presence of normal β3 cytoplasmic tail linkages to intracellular proteins that permit αIIbβ3 activation and cytoskeletal associations.
Quantification of platelet-granulocyte interactions in microfluidic devices
To test whether the microfluidic devices could be used to study heterocellular interactions, we examined dynamic attachment of PE-anti-Gr1-labeled granulocytes to platelets adherent to collagen. Importantly, in our assay, platelet-granulocyte interactions evolved naturally over time from cellular levels present in blood and no exogenous agonists were added to activate cells. Granulocytes were often entrapped in growing platelet thrombi in β3+/+ blood (Fig. 5A), making it difficult to quantify granulocyte interactions with platelets. No thrombi formed from β3−/− blood, however. Therefore, rolling velocities and the subsequent attachment of granulocytes on β3−/− collagen-adherent platelet monolayers could both be determined. Transient β3−/− platelet-granulocyte interactions were observed even at τ > 30 dynes/cm2 and were often accompanied by extension and retraction of granulocyte tethers (Fig. 5A).
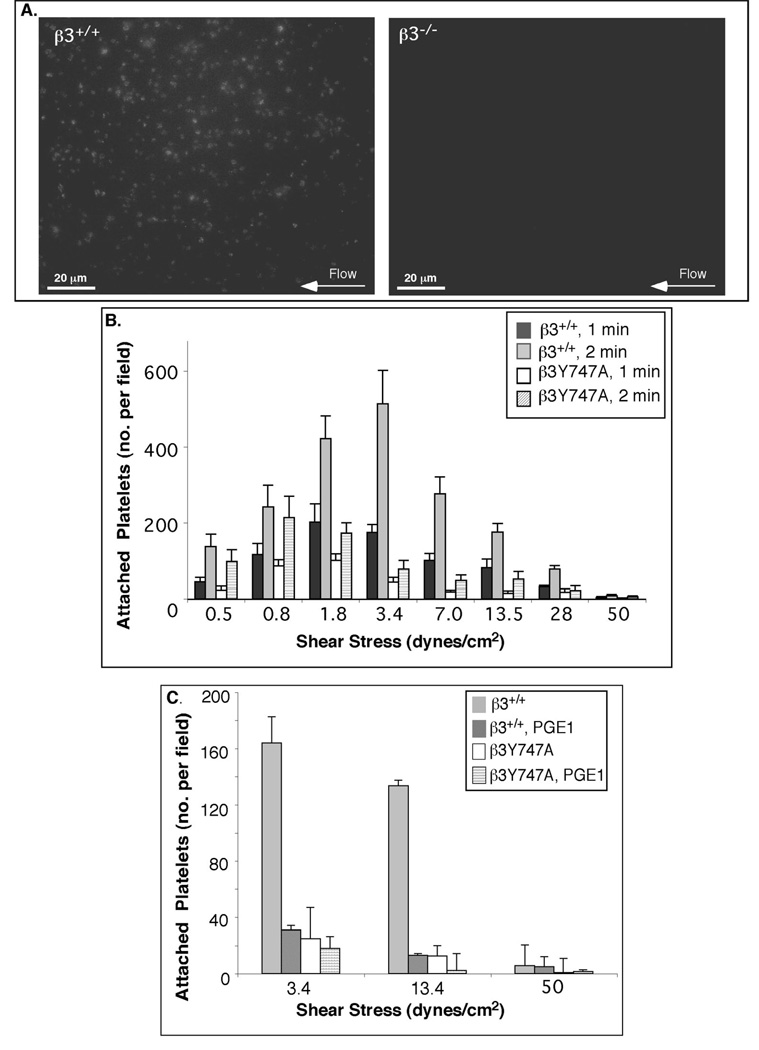
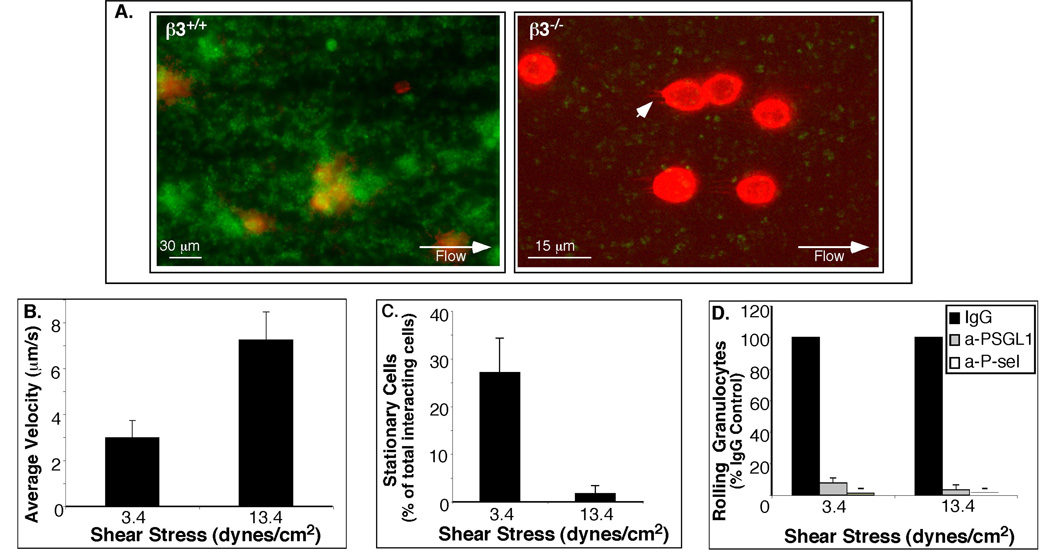
Figure 5.
Platelet-granulocyte interactions. A. Fluorescence micrographs of a test chamber with whole blood from wild-type (left panel) and β3−/− mice (right panel) labeled with PE-anti-Gr-1 antibody (granulocytes: red) and mepacrine (platelets: green) after 10 minutes of flow over collagen matrix at 3.4 dynes/cm2. Note extended β3−/− granulocyte tethers (arrowhead). (B-D). Quantification of interactions between granulocytes and collagen-adherent β3−/− platelets. B. Average translocation velocities of granulocytes on platelets. C. Percentage of stably attached granulocytes. D. Inhibition of granulocyte-platelet interactions. Whole blood from wild type and β3−/− mice was incubated with antibodies against P-selectin (a-P-sel), PSGL-1 (a-PSGL1) or with control IgG for 30 min, prior to flow. Histogram shows the percentage (± SEM) of granulocytes rolling on platelets from blood treated with each inhibitor versus IgG control antibody.
Mean rolling velocities of granulocytes on collagen-adherent β3−/− platelets increased with shear stress, from 3.0 ± 0.7 µm/s at 3.4 dynes/cm2 to 7.2 ± 1.2 µm/s at 13.4 dynes/cm2 (n = 5, p < .01) (Fig. 5B). At 3.4 dynes/cm2, initial interactions led to stable attachment of a substantial portion of granulocytes (27.1 ± 7.2 %), but at 3.4 dynes/cm2 the attachment was minimal (Fig. 5C). Interactions of granulocytes with β3−/− platelets were abolished by antibodies against P-selectin and PSGL-1, but not by control antibodies (% rolling granulocytes relative to IgG control at 3.4 and 13.4 dynes/cm2, respectively: 1.3 ± 0.8%, and 0% for anti P-selectin; 7.9 ± 3.4% and 3.4 ±3.0% for anti-PSGL-1; n= 3, p< 0.01) (Fig. 5D). Therefore, the granulocyte-platelet interactions were dependent on P-selectin and PSGL-1, in agreement with previous reports.38, 39 On the other hand, treatment of β3+/+ platelets with anti-P-selectin and anti-PSGL-1 antibodies did not entirely prevent the presence of granulocytes in thrombi derived from β3+/+ blood (not shown), providing further evidence for non-specific β3+/+ granulocyte entrapment in the thrombi. No rolling of granulocytes was observed on platelets attached to fibrinogen for either β3+/+ or β3−/− blood, presumably due to lower surface expression of P-selectin compared to platelets adherent to collagen (not shown).
Discussion
Motivated by the importance of platelets for arrest of bleeding (hemostasis) and thrombosis, we constructed two new microfluidic devices to study dynamic platelet adhesion at shear stresses typically found in the circulation. Due to small amounts of blood required for assays in the device (3.7 µL/min and <100 µL per assay for the device 1), it was possible for the first time to perform assays on dynamic platelet adhesion with whole blood samples obtained from a single laboratory mouse. The results of adhesion assays in the devices with VWF, fibrinogen, and collagen-coated substrata (Fig. 2) agreed with previous reports, thus validating the use of the proposed microfluidic devices for studying shear-dependent platelet adhesion. To demonstrate an application of the proposed adhesion assays, we performed an extensive series of experiments with blood from wild-type, β3-deficient29 and activation-defective β3Y747A10 mice at shear stresses ranging from low venous to arterial (0.8 – 50 dynes/cm2) with fibrinogen and collagen coated substrates (Fig. 3 and Fig. 4).
The experiments highlighted the key advantages of the proposed microfluidic devices as compared to traditional flow chambers for studies of platelet adhesion. Small blood consumption and high throughput dramatically reduced the costs of the experiments in terms of both time and laboratory animals. A blood sample drawn from a single mouse was sufficient for several adhesion tests in different devices and could be used for tests with different ECM coatings or repeated tests with identical coatings. Moreover, simultaneous monitoring of platelet adhesion over the entire physiological range of shear stresses in device 1 eliminated the sample and matrix variability concerns that would inevitably arise, if tests at different shear stresses were performed with different blood samples or in different flow chambers. Side-by-side observation of dynamic adhesion of platelets from two different blood samples at identical flow conditions and with synchronized initiation times under a high-resolution fluorescence microscope in device 2 made comparisons between the two blood samples particularly simple and straightforward.
The experiments helped elucidate the roles of extracellular and intracellular domains of integrin αIIbβ3 in platelet adhesion to fibrinogen and collagen at different shear stresses, resulting in the following main findings: a) similar to human platelets, wild-type mouse platelets adhere to fibrinogen most efficiently at venous shear stresses; b) as shear stresses increase, structurally intact extracellular αIIbβ3 domains are no longer sufficient to mediate stable adhesion to fibrinogen in the absence of normal β3-cytoplasmic tail linkages that enable integrin activation and stabilization; c) the presence of intact αIIbβ3 extracellular domains and intracellular linkages provides a significant incremental contribution to primary platelet adhesion to collagen at arterial and venous shear stresses and is important for formation of thrombi at all shear stresses; d) collagen-adherent β3−/− platelet monolayers deposited from whole blood promote P-selectin and PSGL-1 dependent granulocyte rolling and stable adhesion. Above all, these results highlight the importance of β3 tyrosine747–mediated linkage to intracellular proteins that promote αIIbβ3 activation and stabilization for optimal platelet adhesion at physiologic shear stresses.
An interesting consequence of the absence of thrombus formation on collagen by β3−/− platelets was the facilitated access and recruitment of granulocytes to activated platelet monolayers. Our experiments on the granulocyte recruitment in the microchannels confirmed that rolling of granulocytes on collagen-adherent β3−/− platelets is mediated by P-selectin and PSGL-1. In vivo, rolling of granulocytes on β3−/− platelets and their subsequent stable attachment may increase the numbers of extravasating granulocytes and thus contribute to the inflammation and atherosclerosis described in the β3−/− mice.40 These observations warrant further investigation of the mechanisms by which αIIbβ3 modulates inflammation.
The proposed microfluidic devices are made of single casts of PDMS sealed with a coverglass and, as is common for this type of devices, they can be made at low cost in amounts sufficient for an extended series of laboratory experiments. The devices are also easily recycled by detaching the PDMS chip from the coverglass, cleaning the chip in a mild detergent, and sealing it with a new coverglass. The flow in the devices is driven by hydrostatic pressure, making them simple to operate, in particular the device 1, which has a single inlet and outlet. When a polyethylene (PE) tubing of an appropriate diameter is inserted into the device inlet, the tubing is held in place and makes an instantaneous sealed connection. The insertion of the other end of the tubing line into an artery of an anesthesized mouse would convert the device into an ex-vivo autoperfusion flow chamber,41, 42 reducing to a minimum the variation of blood between the circulation and the microfluidic test chambers. In addition to the dynamic adhesion of platelets, the proposed devices could also be used to study rolling and substrate adhesion of other cell types, e.g., neutrophils,43 without the need of sacrificing donor mice. Another possible application of the devices is studies of formation of platelet aggregates (thrombi) on various substrates at controlled flow conditions.44 Reduction of the test chamber cross-sections would further reduce the sample volumes and potentially enable adhesion assays in shear flow with blood from genetically amenable organisms, such as zebrafish.45 A possible clinical application of the proposed devices is for testing blood of neonates and young patients, where blood availability is limited. To conclude, the proposed microfluidic devices and dynamic adhesion assays could find multiple applications in research and in medical laboratories.
ACKNOWLEDGEMENTS
These studies were supported by grants HL78784, HL-31950, HL56595 and HL57900 from the NIH, the Cell Migration Consortium, NIH (U54 GM064346), NSF NIRT Grant No. 0608863, the Wellcome Trust (077532), UCSD/SDSU Institutional Research and Academic Career Development Award (NIH GM 68524), and a fellowship from the American Heart Association.
REFERENCES
- 1.Varga-Szabo D, Pleines I, Nieswandt B. Arterioscler Thromb Vasc Biol. 2008 doi: 10.1161/ATVBAHA.107.150474. [DOI] [PubMed] [Google Scholar]
- 2.Patel D, Vaananen H, Jirouskova M, Hoffmann T, Bodian C, Coller BS. Blood. 2003;101:929–936. doi: 10.1182/blood.V101.3.929. [DOI] [PubMed] [Google Scholar]
- 3.Savage B, Shattil SJ, Ruggeri ZM. J Biol Chem. 1992;267:11300–11306. [PubMed] [Google Scholar]
- 4.van Zanten GH, de Graaf S, Slootweg PJ, Heijnen HF, Connolly TM, de Groot PG, Sixma JJ. J Clin Invest. 1994;93:615–632. doi: 10.1172/JCI117014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Savage B, Saldivar E, Ruggeri ZM. Cell. 1996;84:289–297. doi: 10.1016/s0092-8674(00)80983-6. [DOI] [PubMed] [Google Scholar]
- 6.Evangelista V, Manarini S, Dell'Elba G, Martelli N, Napoleone E, Di Santo A, Lorenzet PS. Thromb Haemost. 2005;94:568–577. [PubMed] [Google Scholar]
- 7.Weyrich A, Cipollone F, Mezzetti A, Zimmerman G. Curr Pharm Des. 2007;13:1685–1691. doi: 10.2174/138161207780831374. [DOI] [PubMed] [Google Scholar]
- 8.Han J, Lim CJ, Watanabe N, Soriani A, Ratnikov B, Calderwood DA, Puzon-McLaughlin W, Lafuente EM, Boussiotis VA, Shattil SJ, Ginsberg MH. Curr Biol. 2006;16:1796–1806. doi: 10.1016/j.cub.2006.08.035. [DOI] [PubMed] [Google Scholar]
- 9.Tadokoro S, Shattil SJ, Eto K, Tai V, Liddington RC, de Pereda JM, Ginsberg MH, Calderwood DA. Science. 2003;302:103–106. doi: 10.1126/science.1086652. [DOI] [PubMed] [Google Scholar]
- 10.Petrich BG, Fogelstrand P, Partridge AW, Yousefi N, Ablooglu AJ, Shattil SJ, Ginsberg MH. J Clin Invest. 2007;117:2250–2259. doi: 10.1172/JCI31024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kroll MH, Hellums JD, McIntire LV, Schafer AI, Moake JL. Blood. 1996;88:1525–1541. [PubMed] [Google Scholar]
- 12.Usami S, Chen HH, Zhao Y, Chien S, Skalak R. Ann Biomed Eng. 1993;21:77–83. doi: 10.1007/BF02368167. [DOI] [PubMed] [Google Scholar]
- 13.Murthy SK, Sin A, Tompkins RG, Toner M. Langmuir. 2004;20:11649–11655. doi: 10.1021/la048047b. [DOI] [PubMed] [Google Scholar]
- 14.Cheng XH, Irimia D, Dixon M, Sekine K, Demirci U, Zamir L, Tompkins RG, Rodriguez W, Toner M. Lab On A Chip. 2007;7:170–178. doi: 10.1039/b612966h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gutierrez E, Groisman A. Anal Chem. 2007;79:2249–2258. doi: 10.1021/ac061703n. [DOI] [PubMed] [Google Scholar]
- 16.Lu H, Koo LY, Wang WM, Lauffenburger DA, Griffith LG, Jensen KF. Anal Chem. 2004;76:5257–5264. doi: 10.1021/ac049837t. [DOI] [PubMed] [Google Scholar]
- 17.Runyon MK, Kastrup CJ, Johnson-Kerner BL, Ha TG, Ismagilov RF. J Am Chem Soc. 2008;130:3458–3464. doi: 10.1021/ja076301r. [DOI] [PubMed] [Google Scholar]
- 18.Prabhakarpandian B, Pant K, Scott RC, Patillo CB, Irima D, Kiani MF, Sundaram S. Biomedical Microdevices. 2008 doi: 10.1007/s10544-008-9170-y. March8, 2008 e-pub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Antia M, Herricks T, Rathod PK. PLoS Pathog. 2007;3:e99. doi: 10.1371/journal.ppat.0030099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schaff UY, Xing MM, Lin KK, Pan N, Jeon NL, Simon SI. Lab Chip. 2007;7:448–456. doi: 10.1039/b617915k. [DOI] [PubMed] [Google Scholar]
- 21.Simonnet C, Groisman A. Anal Chem. 2006;15:5653–5663. doi: 10.1021/ac060340o. [DOI] [PubMed] [Google Scholar]
- 22.Lengweiler S, Smyth SS, Jirouskova M, Scudder LE, Park H, Moran T, Coller BS. Biochem Biophys Res Commun. 1999;262:167–173. doi: 10.1006/bbrc.1999.1172. [DOI] [PubMed] [Google Scholar]
- 23.Ruggeri ZM, De Marco L, Gatti L, Bader R, Montgomery RR. J Clin Invest. 1983;72:1–12. doi: 10.1172/JCI110946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Labow MA, Norton CR, Rumberger JM, Lombard-Gillooly KM, Shuster DJ, Hubbard J, Bertko R, Knaack PA, Terry RW, Harbison ML, et al. Immunity. 1994;1:709–720. doi: 10.1016/1074-7613(94)90041-8. [DOI] [PubMed] [Google Scholar]
- 25.Yang J, Hirata T, Croce K, Merrill-Skoloff G, Tchernychev B, Williams E, Flaumenhaft R, Furie BC, Furie B. J Exp Med. 1999;190:1769–1782. doi: 10.1084/jem.190.12.1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prasad KS, Andre P, He M, Bao M, Manganello J, Phillips DR. Proc Natl Acad Sci U S A. 2003;100:12367–12371. doi: 10.1073/pnas.2032886100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.De Marco L, Girolami A, Zimmerman TS, Ruggeri ZM. Proc Natl Acad Sci U S A. 1985;82:7424–7428. doi: 10.1073/pnas.82.21.7424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alevriadou BR, Moake JL, Turner NA, Ruggeri ZM, Folie BJ, Phillips MD, Schreiber AB, Hrinda ME, McIntire LV. Blood. 1993;81:1263–1276. [PubMed] [Google Scholar]
- 29.Hodivala-Dilke KM, McHugh KP, Tsakiris DA, Rayburn H, Crowley D, Ullman-Cullere M, Ross FP, Coller BS, Teitelbaum S, Hynes RO. J Clin Invest. 1999;103:229–238. doi: 10.1172/JCI5487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roberts PJ, Williams SL, Linch DC. Br J Haematol. 1996;92:804–814. doi: 10.1046/j.1365-2141.1996.432970.x. [DOI] [PubMed] [Google Scholar]
- 31.Haycox CL, BD R, TA H. J. Biomed.Mater.Res. 1991;25:1317–1320. [Google Scholar]
- 32.Kasirer-Friede A, Cozzi MR, Mazzucato M, De Marco L, Ruggeri ZM, Shattil SJ. Blood. 2004;103:3403–3411. doi: 10.1182/blood-2003-10-3664. [DOI] [PubMed] [Google Scholar]
- 33.Goncalves I, Hughan SC, Schoenwaelder SM, Yap CL, Yuan Y, Jackson SP. J Biol Chem. 2003;278:34812–34822. doi: 10.1074/jbc.M306504200. [DOI] [PubMed] [Google Scholar]
- 34.Watson SP, Auger JM, McCarty OJ, Pearce AC. J Thromb Haemost. 2005;3:1752–1762. doi: 10.1111/j.1538-7836.2005.01429.x. [DOI] [PubMed] [Google Scholar]
- 35.Kahn ML. Semin Thromb Hemost. 2004;30:419–425. doi: 10.1055/s-2004-833477. [DOI] [PubMed] [Google Scholar]
- 36.Kato K, Kanaji T, Russell S, Kunicki TJ, Furihata K, Kanaji S, Marchese P, Reininger A, Ruggeri ZM, Ware J. Blood. 2003;102:1701–1707. doi: 10.1182/blood-2003-03-0717. [DOI] [PubMed] [Google Scholar]
- 37.Zaidi TN, McIntire LV, Farrell DH, Thiagarajan P. Blood. 1996;88:2967–2972. [PubMed] [Google Scholar]
- 38.Evangelista V, Manarini S, Coller BS, Smyth SS. J Thromb Haemost. 2003;1:1048–1054. doi: 10.1046/j.1538-7836.2003.00214.x. [DOI] [PubMed] [Google Scholar]
- 39.Xiao Z, Goldsmith HL, McIntosh FA, Shankaran H, Neelamegham S. Biophys J. 2006;90:2221–2234. doi: 10.1529/biophysj.105.065789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weng S, Zemany L, Standley KN, Novack DV, La Regina M, Bernal-Mizrachi C, Coleman T, Semenkovich CF. Proc Natl Acad Sci U S A. 2003;100:6730–6735. doi: 10.1073/pnas.1137612100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Smith ML, Sperandio M, Galkina EV, Ley K. Journal Of Leukocyte Biology. 2004;76:985–993. doi: 10.1189/jlb.1003483. [DOI] [PubMed] [Google Scholar]
- 42.Hafezi-Moghadam A, Thomas KL, Cornelssen C. American Journal Of Physiology-Cell Physiology. 2004;286:C876–C892. doi: 10.1152/ajpcell.00500.2003. [DOI] [PubMed] [Google Scholar]
- 43.Chesnutt BC, Smith DF, Raffler NA, Smith ML, White EJ, Ley K. Microcirculation. 2006;286:99–109. doi: 10.1080/10739680500466376. [DOI] [PubMed] [Google Scholar]
- 44.Xu Z, Chen N, Kamocka MM, Rosen ED, M A. J R Soc Interface. 2007 doi: 10.1098/rsif.2007.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jagadeeswaran P, Gregory M, Day K, Cykowski M, Thattaliyath B. J Thromb Haemost. 2005;3:46–53. doi: 10.1111/j.1538-7836.2004.00999.x. [DOI] [PubMed] [Google Scholar]