Abstract
A young man with a previous history of episodes of mild solid food dysphagia was admitted with a total dysphagia. The esophagogastroduodenoscopy (EGDS) showed an extensive disruption of mucosal layer with a cul-de-sac in the lower part of the esophagus. Soon after the procedure, the patient suffered from an acute chest pain and subsequent CT scan demonstrated an intramural circumferential dissection of thoracic esophagus, and a mediastinal emphysema. An emergency right thoracotomy was performed, followed by a total esophagectomy with esophagogastroplasty and jejunostomy. The histopathology confirmed that mucosal and submucosal layers were circumferentially detached from muscular wall and showed an eosinophilic infiltration of the whole organ with necrosis and erosions of mucosal, submucosal and muscular layers. The diagnosis was esophageal perforation in eosinophilic esophagitis.
Keywords: Thoracic surgery emergency, Esophageal perforation, Eosinophilic esophagitis, Esophageal mucosal dissection, Esophagus surgery
INTRODUCTION
Idiopathic eosinophilic esophagitis is an underdiagnosed disease with typical endoscopic findings. The clinical presentation includes solid food dysphagia in young adults who have an atopic predisposition. Food impaction necessitating endoscopic intervention is common. Mucosal rents and rarely perforations occur with simple passage of the endoscope[1]. We report a case of circumferential mucosal dissection in a young man with eosinophilic esophagitis.
CASE REPORT
A 32-year-old man was admitted into a local hospital service of gastroenterology with a diagnosis of food impaction. The patient had no previous history of upper gastrointestinal disease and had suffered from mild solid food dysphagia over the last years. All previous dysphagic episodes underwent spontaneous resolution and some of them were occasionally associated with various atopic symptoms. Upon admission, the patient was in good general conditions although presented mild distress due to tachypnea (RR 35/min); other vital signs were within normal limits. Since the patient complained of a total dysphagia in swallowing any liquids, it was impossible to perform a gastrografin esophagography. Therefore, the patient underwent EGDS that showed no food impaction, but an extensive disruption of mucosal layer with a cul-de-sac in the lower part of the esophagus. Soon after the endoscopy, the patient suffered from an acute chest pain and a severe discomfort with development of an extensive neck and anterior thoracic emphysema. A CT scan was performed.
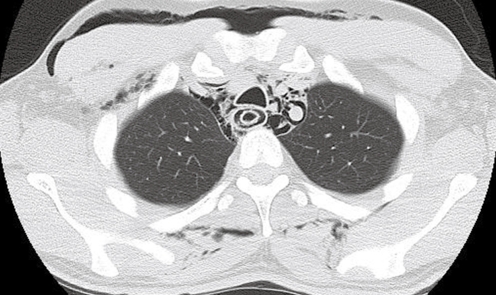
The CT scan identified an intramural circumferential dissection of thoracic esophagus, a pneumomediastinum and a subcutaneous emphysema of the neck and of the anterior thoracic wall (Figure 1). Following the diagnosis of esophageal perforation, a right thoracotomy was performed. During the operation a 1.5 cm esophageal perforation at T1 level was detected. A peroperative EGDS was executed, and the mucosal and submucosal layers were circumferentially dissected from the muscular part of the esophageal wall. The dissection extended from 19 cm below the upper dental arcade up to the lower portion of the thoracic esophagus, ending at a cul-de-sac that stopped the endoscope progression. The mucosal and submucosal layers, circumferentially detached from muscular wall, looked like a whitish flap distally-fixed and floating inside the esophageal lumen (Figure 2). The endoscopy allowed to explore both the false and true visceral lumens. Due to the severe alteration of almost the whole thoracic esophagus wall, a simple suture of the perforation appeared hazardous, thus a total esophagectomy with esophagogastroplasty and jejunostomy was performed.
Figure 1.
CT scan shows oesophageal double lumen associated with pmeumo-mediastinum and subcutaneous emphysema.
Figure 2.
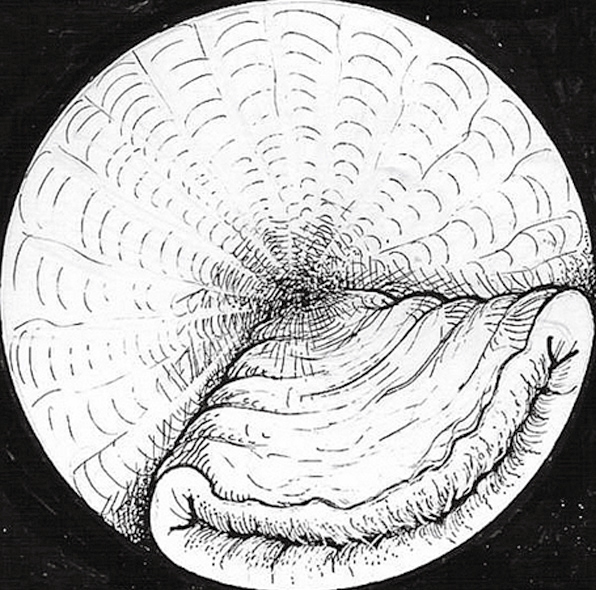
The drawing shows the endoscopic view of the esophagus: mucosal and submucosal layers are totally dissected from muscular wall. The false lumen ends in a cul de sac.
The histopathology confirmed an eosinophilic infiltration of the whole organ with necrosis and erosions of all mucosa, submucosa and in some areas of the muscular layer. The diagnosis was eosinophilic esophagitis.
The patient received 2 d of ICU. Gastrografin esophagogram on the 10th post- operative day showed normal pattern and motility of the neoesophagus. Three months after surgery, the patient had a good quality of life, ate a normal diet and did not experience any weight loss.
DISCUSSION
Eosinophilic esophagitis (EE) is an isolated, eosinophilic inflammation of the esophagus. The symptoms of EE used to be confused with gastroesophageal reflux (GERD).
Recent reports suggest a multi-step allergy process starting with an atopic skin response that primes the esophagus for further allergen exposure. A population of eosinophils different from gut and blood that specifically reaches the esophagus in EE was demonstrated[2]. The allergic reaction involved in EE is non-IgE mediated. The most commonly involved food includes milk, eggs, nuts, beef, wheat, fish, shellfish, corn and soy. However, almost all the food is implicated[3].
The diagnosis of EE is suggested by an unexplained dysphagia or by a food impaction in a young adult with a personal and family allergic history.
Clinical features include dysphagia (93%), food impaction (62%), heartburn (23.6%) and history of atopia (51.6%)[4]. Endoscopic findings are mucosal fragility/oedema, rings, strictures, whitish pinpoint exudates and small-calibre esophagus in various cases whereas 8.8% of patients have a normal endoscopy[4]. The presence of more than 15 eosinophils per high power field on esophageal biopsies is required to establish the diagnosis[4]. Therapeutic options include restriction of diets, various medicaments (systemic and topical corticosteroids, leukotriene receptor antagonists and, most recently, an anti-interleukin-5 monoclonal antibody) and endoscopic dilatation[5]. The administration of corticosteroids resulted in symptomatic improvement in more than 95% of cases. A trial with corticosteroids before bougienage may reduce the active inflammation and the complication rate[2]. Esophageal perforation is described as a complication[4] and one case was treated with subtotal esophagectomy[6]. Although a spontaneous circumferential mucosal dissection was already described[7], we are not aware of any other cases associated with eosinophilic esophagitis.
We believe that in our patient the dissection is most likely spontaneous, since no impacted food has been found in either the endoscopic examination or the resected esophagus. However, we can not exclude that the dissection may be caused or enlarged by the esophagoscopy, therefore this risk must be always born in mind while deciding to perform an endoscopy for young patients with sudden total dysphagia and with a personal and familial history of atopic symptoms. With regard to esophageal perforation, it is certainly iatrogenic, since the symptoms correlated with this complication (acute chest pain, severe discomfort, extensive neck and anterior thoracic emphysema) appeared at the end of the endoscopic examination.
Peer reviewer: Nikolaus Gassler, Professor, Institute of Pathology, University Hospital RWTH Aachen, Pauwelsstrasse 30, Aachen 52074, Germany
S- Editor Liu Y L- Editor Ma JY E- Editor Liu Y
References
- 1.Kaplan M, Mutlu EA, Jakate S, Bruninga K, Losurdo J, Losurdo J, Keshavarzian A. Endoscopy in eosinophilic esophagitis: "feline" esophagus and perforation risk. Clin Gastroenterol Hepatol. 2003;1:433–437. doi: 10.1016/s1542-3565(03)00222-2. [DOI] [PubMed] [Google Scholar]
- 2.Katzka DA. Eosinophilic esophagitis. Curr Opin Gastroenterol. 2006;22:429–432. doi: 10.1097/01.mog.0000231820.71761.70. [DOI] [PubMed] [Google Scholar]
- 3.Liacouras CA, Ruchelli E. Eosinophilic esophagitis. Curr Opin Pediatr. 2004;16:560–566. doi: 10.1097/01.mop.0000141071.47572.eb. [DOI] [PubMed] [Google Scholar]
- 4.Sgouros SN, Bergele C, Mantides A. Eosinophilic esophagitis in adults: a systematic review. Eur J Gastroenterol Hepatol. 2006;18:211–217. doi: 10.1097/00042737-200602000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Arora AS, Yamazaki K. Eosinophilic esophagitis: asthma of the esophagus? Clin Gastroenterol Hepatol. 2004;2:523–530. doi: 10.1016/s1542-3565(04)00236-8. [DOI] [PubMed] [Google Scholar]
- 6.Riou PJ, Nicholson AG, Pastorino U. Esophageal rupture in a patient with idiopathic eosinophilic esophagitis. Ann Thorac Surg. 1996;62:1854–1856. doi: 10.1016/s0003-4975(96)00553-x. [DOI] [PubMed] [Google Scholar]
- 7.Kim SH, Lee SO. Circumferential intramural esophageal dissection successfully treated by endoscopic procedure and metal stent insertion. J Gastroenterol. 2005;40:1065–1069. doi: 10.1007/s00535-005-1692-y. [DOI] [PubMed] [Google Scholar]