Abstract
The differential diagnosis between intracystic hemorrhage and cystadenocarcinoma of the liver is often difficult even with the use of various imaging modalities. A 73-year-old woman was admitted to our hospital with the complaint of right upper quadrant pain. Ultrasonography (US) demonstrated a heterogeneous echogenic cyst measuring 11 cm × 8 cm in size in S2 of the liver, indicated intracystic hemorrhage of simple liver cyst or cystadenocarcinoma, but the differential diagnosis was considerably difficult. Levovist (Schering, Berlin, Germany) US revealed no enhancement of the intracystic structures, suggesting a clot in the case of intracystic hemorrhage. An operation was performed and the resected lesion showed a solitary benign liver cyst, measuring 5.5 cm × 4.7 cm × 8.5 cm containing a large blood clot. The patient had an uneventful recovery after the surgery. Levovist US may play an important role in discrimination between intracystic hemorrhage of simple hepatic cysts and cystadenocarcinoma of the liver.
Keywords: Liver cyst, Cystadenocarcinoma, Simple cyst, Galactose acid palmitique, Levovist
INTRODUCTION
Hemorrhage into a simple liver cyst is rather uncommon. The differential diagnosis between intracystic hemorrhage and cystadenocarcinoma of the liver is difficult with the various imaging studies currently available[1,2]. Consequently, hepatectomy has been performed unnecessarily, even in cases with benign liver cysts with intracystic bleeding, based on a wrong preoperative diagnosis of cystadenocarcinoma. We report on a patient with intracystic hemorrhage complicating a simple liver cyst in whom the diagnosis was made accurately by Levovist (Schering, Berlin, Germany) Ultrasonography (US) Imaging.
CASE REPORT
A 73-year-old woman with chronic hepatitis C had been under follow-up for two years. She had been followed up by laboratory examination every month and imaging studies such as US and Computed Tomography (CT) every six months as screening procedures for hepatocellular carcinoma. The previous US and CT had only shown a simple cyst measuring 1.3 cm in diameter in segment 4 (S4) of the left lobe. The patient did not complain of any abdominal discomfort during this period, nor was there any history of abdominal injury.
The patient was admitted to hospital with the complaint of right upper quadrant pain. Her blood pressure was 110/62 mmHg, pulse was 84/min, and physical examination revealed spontaneous pain, tenderness, and no muscular defense in the abdomen. The liver was not palpable under the right rib cage. The laboratory examination findings were almost normal except as follows: anemia (red blood cell count, 399 ×104/mm3; hematocrit, 30%; hemoglobin, 12.6 g/dL) and elevated serum CRP (3.5 mg/dL). The serum was negative for antibody against Echinococcus antigens by enzyme-linked immunosorbent assay.
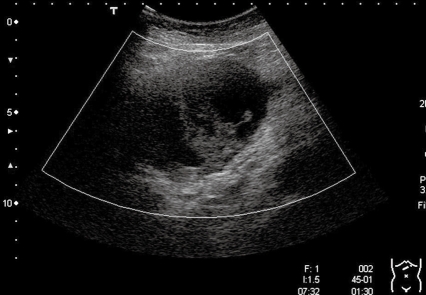
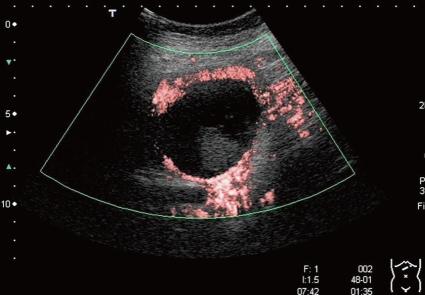
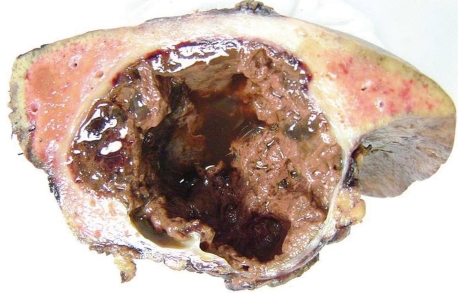
US demonstrated a heterogeneous echogenic cyst measuring 11 cm × 8 cm in size with intracystic structures in S2 of the liver (Figure 1), indicating a intracystic hemorrhage of simple liver cyst or cystadenocarcinoma, but the differential diagnosis was considerably difficult on the US imaging. Levovist (Schering, Berlin, Germany) US revealed no enhancement of the intracystic septations and structures, suggested a clot in case of intracystic hemorrhage. Moreover the enhanced cyst wall was smooth in contour, suggested a simple cyst (Figure 2). Hence, the hemorrhage into a simple cyst including intracystic blood clot was indicated by Levovist US. On plain CT, the intracyst showed heterogeneous low-density, and intracystic septations were not detected. On magnetic resonance imaging (MRI), T1-weighted images revealed the clot as a low-intensity and the fluid as a high-intensity, whereas T2-weighted image shows the clot as low-intensity and the fluid as high-intensity. Although a high-intensity lesion on T1-weighted images is not specific for hemorrhage and can be observed in other conditions (mucinous fluid, melanin component, and fat content), the visualization of a high-intensity lesion on T2-weighted images may suggest the diagnosis of intracystic hemorrhage. No contrast agent could be used both in CT and MRI studies, because of the patient’s history of asthma. Based on the imaging findings, we diagnosed the case as one of hemorrhage into a simple cyst. Because of the risk of the enlargement and rupture of the cystic lesion, operation was considered to be indicated. Lateral sectionectomy, cholecystectomy, and intraoperative cholangio-graphy (IOC) were performed. Exploratory laparotomy revealed a large cystic lesion which occupied the left lobe of the liver with adhesion of the omentum minor to its wall. IOC revealed no communication between the intrahepatic bile duct and the cystic lesion. The resected lesion showed a solitary benign liver cyst, measuring 5.5 cm × 4.7 cm × 8.5 cm containing a large blood clot (Figure 3). The blood clot in the cyst was apparently visualized as the intracystic structures on the US and MRI and CT. The cystic wall consisted of fibrous tissue with capillary proliferation and hemorrhage, and was lined by one row of cuboidal epithelial cells. The patient had an uneventful recovery and was discharged 17 d after the surgery.
Figure 1.
US image showing a heterogeneous echogenic cyst in S2, measuring 11.0 cm × 8.0 cm and showing intracystic septations and structures.
Figure 2.
CEU images demonstrating absence of enhancement of the intracystic septations and structures and smooth of the enhanced cyst wall.
Figure 3.
Histological examination showed that the intracystic structures were clots caused by the intracystic hemorrhage.
DISCUSSION
Cystic lesions in the liver are currently classified into acquired and congenital cysts, or parasitic and nonparasitic cysts. Acquired cysts include traumatic, inflammatory, and proliferative cysts[3]. Simple cysts or nonparasitic liver cysts are considered to be congenital and most simple cysts encountered in clinical practice are congenital. The etiology of simple cysts is unclear, and they presumably arise from developmental defects during the formation of bile ducts. The lining epithelium of these cysts is identical to that of the biliary tract[4], although an open communication with the biliary system is unusual.
Hepatic simple cysts are predominantly asymptomatic. However, symptoms may be caused by rapid growth or occurrence of complications. The complication rate has been reported to be about 10%, and complications include intracystic hemorrhage, infection, intraperitoneal rupture, torsion, inflammation, and obstructive jaundice, with hemorrhage and infection as the most commonly encountered complications[5].
In our case, the differential diagnosis would have been even more difficult if a cystadenocarcinoma was complicated by intracystic hemorrhage. One of the characteristic findings of cystadenocarcinoma on sonography has been reported to be highly echogenic internal septations[6].
In many countries, microbubble contrast agents are now available for improved US imaging. Levovist is one of such microbubble agents, consisting of an admixture of galactose granules with a small (0.1%) amount of palmitic acid that produces multiple small (approximately 3 μm) stabilized air bubbles when suspended in water. Levovist produces Doppler enhancement of the blood pool for 2-5 min[7], followed by a late hepatosplenic phase that lasts for more than 30 min[8]. In our patient, the intracystic structures mimicking malignancy that was visualized on US was demonstrated to be an avascular lesion on CEU, suggested a clot of intracystic hemorrhage. In addition, the enhanced cyst wall was shown to have a smooth contour, suggested the diagnosis of a simple cyst. Hence, we diagnosed the hemorrhage into a simple cyst.
The treatment of a simple liver cyst complicated by intracystic hemorrhage can be either surgical or nonsurgical. In recent years, there has been a trend away from surgical treatment, as injection of absolute alcohol into the cyst has been shown to yield better results with fewer complications. However, in our patient, surgery was chosen because the cyst began to grow rapidly in size, with the attendant risk of rupture. Therefore, we could examine the resected tissue specimens which showed that the lesion was an encapsulated unilobular cyst filled with morphologically irregular blood clots. The histological findings in resected tissue specimens in relation to the MR images of intracystic hemorrhage in simple liver cysts has previously been reported by one group[9]. In our reported case, we could compare the histological findings in the resected tissue specimens with the CEU findings. Moreover, some groups have even reported detection of the active bleeding point in such cases by CEU[10,11]. In our case, the active bleeding point was not detected, perhaps because the bleeding had already stopped. However, CEU may be useful for diagnosing active intracystic hemorrhage.
In conclusion, CEU may play an important role in the correct diagnosis of a simple hemorrhagic cyst by demonstrating the avascularity of the visualized intracystic structures. We followed up the patient of a simple liver cyst complicated by intracystic hemorrhage in whom CEU was very useful for diagnosis.
Peer reviewers: Mitsuo Shimada, Professor, Department of Digestive and Pediatric Surgery, Tokushima University, Kuramoto 3-18-15, Tokushima 770-8503, Japan; Dusan M Jovanovic, Professor, Institute of Oncology, Institutski Put 4, Sremska Kamenica 21204, Serbia; Yoshiharu Motoo, MD, PhD, FACP, FACG, Professor and Chairman, Department of Medical Oncology, Kanazawa Medical University, 1-1 Daigaku, Uchinada, Ishikawa 920-0293, Japan
S- Editor Zhu LH L- Editor Roberts SE E- Editor Wang HF
References
- 1.Ohhira M, Ohta H, Amizuka H, Yanagawa N, Matsumoto A, Murazumi K, Murazumi Y, Fujimoto Y, Namiki M, Fujii T. Intracystic hemorrhage of simple hepatic cyst simulating cystadenocarcinoma of the liver--report of two cases. Nippon Shokakibyo Gakkai Zasshi. 1994;91:2264–2268. [PubMed] [Google Scholar]
- 2.Zanen AL, van Tilburg AJ. Bleeding into a liver cyst can be treated conservatively. Eur J Gastroenterol Hepatol. 1995;7:91–93. [PubMed] [Google Scholar]
- 3.Hadad AR, Westbrook KC, Graham GG, Morris WD, Campbell GS. Symptomatic nonparasitic liver cysts. Am J Surg. 1977;134:739–744. doi: 10.1016/0002-9610(77)90314-2. [DOI] [PubMed] [Google Scholar]
- 4.Mandelbaum I, Shumacker HB Jr. Excision of congenital hepatic cyst of bile duct origin. Am J Surg. 1961;101:507–510. doi: 10.1016/0002-9610(61)90303-8. [DOI] [PubMed] [Google Scholar]
- 5.Murphy BJ, Casillas J, Ros PR, Morillo G, Albores-Saavedra J, Rolfes DB. The CT appearance of cystic masses of the liver. Radiographics. 1989;9:307–322. doi: 10.1148/radiographics.9.2.2538868. [DOI] [PubMed] [Google Scholar]
- 6.Federle MP, Filly RA, Moss AA. Cystic hepatic neoplasms: complementary roles of CT and sonography. AJR Am J Roentgenol. 1981;136:345–348. doi: 10.2214/ajr.136.2.345. [DOI] [PubMed] [Google Scholar]
- 7.Schlief R. Developments in echo-enhancing agents. Clin Radiol. 1996;51 Suppl 1:5–7. [PubMed] [Google Scholar]
- 8.Blomley MJ, Albrecht T, Cosgrove DO, Eckersley RJ, Butler-Barnes J, Jayaram V, Patel N, Heckemann RA, Bauer A, Schlief R. Stimulated acoustic emission to image a late liver and spleen-specific phase of Levovist in normal volunteers and patients with and without liver disease. Ultrasound Med Biol. 1999;25:1341–1352. doi: 10.1016/s0301-5629(99)00081-2. [DOI] [PubMed] [Google Scholar]
- 9.Hagiwara A, Inoue Y, Shutoh T, Kinoshita H, Wakasa K. Haemorrhagic hepatic cyst: a differential diagnosis of cystic tumour. Br J Radiol. 2001;74:270–272. doi: 10.1259/bjr.74.879.740270. [DOI] [PubMed] [Google Scholar]
- 10.Ueno N, Kawamura H, Hoshino T, Kadowaki A, Nakamura K. Detection of alimentary tract hemorrhage on contrast-enhanced ultrasonography. J Ultrasound Med. 2006;25:683–686. doi: 10.7863/jum.2006.25.5.683. [DOI] [PubMed] [Google Scholar]
- 11.Naganuma H, Funaoka M, Fujimori S, Niwa M, Ishida H, Komatsuda T, Yamada M, Furukawa K. Contrast-enhanced sonographic findings in a case of hepatobiliary cystadenoma with intracystic bleeding. J Clin Ultrasound. 2006;34:412–415. doi: 10.1002/jcu.20262. [DOI] [PubMed] [Google Scholar]