Abstract
Background
Palifermin is a recombinant human keratinocyte growth factor that is used to reduce the duration and severity of oral mucositis in patients undergoing hematopoietic stem cell transplantation after myelotoxic therapy. Cutaneous adverse reactions associated with keratinocyte growth factor are reported to be rash, pruritus, and erythema.
Observations
After receiving palifermin following autologous hematopoietic stem cell transplantation and treatment with melphalan, a patient developed erythema and lichenoid papules that were distributed primarily in intertriginous areas. A biopsy specimen of the papules showed a striking resemblance to verrucae, but in situ hybridization studies were negative for human papillomavirus. Immunohistochemical staining with antibodies to Ki-67 and cytokeratin 5/6 showed increased keratinocyte proliferation in lesional skin.
Conclusions
After treatment with palifermin, a papular eruption clinically resembling lichen planus or plane warts, with histologic features of verruca plana, and intertriginous erythema may occur. In this case, neither eruption required treatment, and spontaneous resolution was observed over days to weeks. Histopathologic staining patterns of Ki-67 and cytokeratin 5/6 may be useful in identifying adverse reactions to palifermin therapy.
KERATINOCYTE GROWTH FACtor (KGF) is a member of the family of fibroblast growth factors. While many fibroblast growth factors affect the proliferation, migration, and/or differentiation of a variety of different cell types, KGF acts specifically on epithelial cells in a broad range of tissues, including skin, oral mucosa, gastrointestinal tract, lung, and genitourinary tract.1-3 Mucosal epithelial cell proliferation assessed by Ki-67 immunohistochemical staining is increased in the setting of KGF exposure.4 Palifermin (recombinant human KGF) is a truncated version of endogenous KGF that demonstrates similar biologic activities with increased stability.
A phase 3 trial published in 2004 demonstrated the efficacy and safety of palifermin therapy in reducing the duration and severity of oral mucositis in patients undergoing autologous hematopoietic stem cell transplantation after total-body irradiation and high-dose chemotherapy.5 In that trial, palifermin was administered for 3 consecutive days before total-body irradiation and again for 3 consecutive days after transplantation. Cutaneous adverse reactions, similar to those seen in phase 1 and 2 trials, occurred approximately 3 days after the third dose of palifermin, lasted approximately 3 days, and were reported to be “rash, pruritus, erythema, and paresthesia.” The rash is not described further.
A review of the literature since 2004 revealed 3 case reports of cutaneous eruptions in the setting of palifermin treatment. The first case report describes palmoplantar erythrodysesthesia (a reaction not uncommonly seen with high-dose cytarabine therapy) in a patient after BEAM (carmustine, etoposide, cytarabine, and melphalan) chemotherapy, which includes low-dose cytarabine. The authors hypothesized that enhanced epithelial proliferation due to palifermin therapy increased the susceptibility to cytarabine-induced palmoplantar erythrodysesthesia.6 In the second case report, a “papulopustular (acne-like)” eruption of the head and upper trunk was observed in a patient 11 days after treatment with busulfan, cyclophosphamide, and antithymocyte globulin and concurrent with the administration of palifermin.7 In a third report, a “mild rash presumed to be due to palifermin” therapy was reported in one patient (the features of the rash are not described), and a desquamating rash of the groin, axillae, and palmoplantar surfaces initially thought to be due to palifermin therapy but later attributed to the use of etoposide was reported in another patient.8 Biopsy results were not mentioned in any of these reports.
REPORT OF A CASE
A 70-year-old man with multiple myeloma whose disease was progressing despite previous treatment with melphalan, thalidomide, bortezomib, lenalidomide, and cyclophosphamide was hospitalized for autologous peripheral blood stem cell transplantation. After 2 days of treatment with melphalan and decadron, he underwent infusion of peripheral blood stem cells and started daily intravenous palifermin therapy for 3 consecutive days. Three days after peripheral blood stem cell transplantation and 1 day after completing a course of palifermin, he was noted to have 3 morphologically distinct oral mucosal and cutaneous eruptions: (1) asymptomatic blanching erythema of the neck and inframammary folds, axillae (Figure 1A), groin, back, and buttocks; (2) numerous 2- to 6-mm, pink to purple, polyangular, planar papules without scale primarily within and immediately peripheral to the intertriginous distribution of the aforementioned erythema (Figure 1A) but also scattered on the trunk and all 4 extremities (sparing the palms and soles); and (3) confluent, white plaques on the tongue and remaining oral mucosa. He denied a history of a similar eruption or any other skin condition. There was no antecedent or concurrent fever, chills, diaphoresis, cough, nausea, vomiting, or diarrhea. At the time of the initial dermatology evaluation, a shave biopsy specimen was obtained from a papule on the left proximal thigh area. Two days later, by which time there had already been noticeable fading of the intertriginous erythema, a second shave biopsy specimen was obtained from a papule on the right upper inner arm area. Over the following week, without treatment, the intertriginous erythema resolved without desquamation, and the lichenoid papules regressed (Figure 1B).
Figure 1.

Clinical appearance on initial evaluation revealed erythema and a papular eruption in a predominantly intertriginous distribution (A); 1 week later, the eruption was largely resolved (B).
METHODS
After the patient gave informed consent, shave biopsy specimens were obtained from papules located on the left thigh and right arm. Tissue specimens were fixed in 10% buffered formalin, embedded in paraffin, and stained with hematoxylin-eosin according to standard procedures. Immunohistochemical studies were performed with antibodies to Ki-67 (Dako Corp, Carpinteria, California) (prediluted) and cytokeratin (CK) 5/6 (Dako Corp) (dilution 1:40). This latter antibody was selected based on reports that epidermal growth factors specifically induce activation- and hyperproliferation-associated CKs 6 and 16,9 coupled with the lack of availability of monospecific antisera to CK 6 or 16. For controls, the tips of excisional specimens of 5 nevi and 5 verrucae from unrelated patients were used.
In situ hybridization was performed using a previously published protocol10 to test for human papillomavirus (HPV) types 1, 2, 5, 6, 8, 11, 16, 18, 30, 31, 33, 35, 39, 42, 43, 44, 45, 51, 52, 56, 57, 58, 68, and 70 as well as other “novel” types (an HPV detected that is related to but distinct from those included in the probe cocktail). Control specimens included plantar warts, verruca vulgaris, warts of epidermodysplasia verruciformis, condyloma acuminata, and cervical low- and high-grade squamous intraepithelial lesions.
RESULTS
HISTOPATHOLOGIC FINDINGS
Histologic examination of the specimen of the papule from the left thigh showed a discrete area of papillated epidermal hyperplasia, hypergranulosis, and laminated hyperorthokeratosis with slight inward bowing of the lateral rete ridges (Figure 2A). Notably, koilocytes and parakeratotis were absent. Histologic examination of the specimen of the papule from the right inner arm area obtained 2 days later showed a gradual transition from normal epidermis to digitated epidermal hyperplasia, hypergranulosis, and compact hyperorthokeratosis (data not shown). The lesion lacked sharp circumscription, koilocytosis, and parakeratosis. Additional testing for HPV and markers of cellular proliferation were performed to further assess the possibility of verruca.
Figure 2.
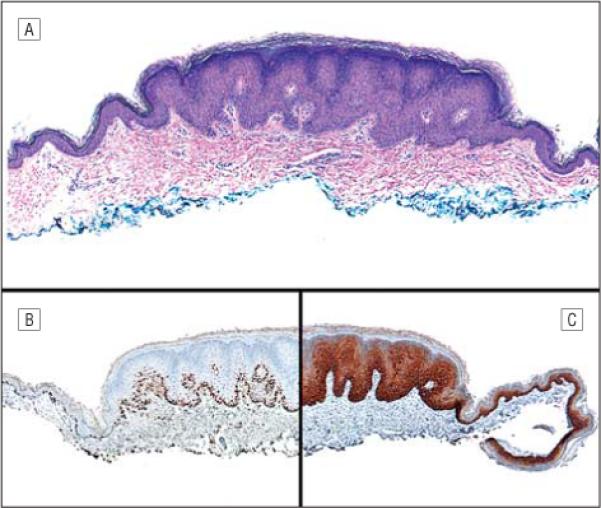
Skin biopsy specimen of an early lesion. A, Hematoxylin-eosin staining shows papillated epidermal hyperplasia, hypergranulosis, and laminated hyperkeratosis (original magnification ×40). B, Immunostaining with Ki-67, a proliferation marker, shows dramatically increased labeling of basilar and suprabasilar keratinocytes (original magnification ×40). C, Immunostaining with cytokeratin 5/6 shows activation of the entire basal layer and stratum spinulosum (original magnification ×40).
SPECIAL STUDIES
In situ hybridization was negative for numerous HPV types, while control specimens revealed the presence of the virus (see the “Methods” section). Immunohistochemical staining of the initial shave biopsy specimen for Ki-67 showed positivity in contiguous basal and suprabasal keratinocytes throughout the area of epidermal hyperplasia (Figure 2B). The margins of the biopsy specimen (which included clinically uninvolved skin) showed an epidermis of normal thickness and only scattered discontinuous staining of occasional basal keratinocyte nuclei. The staining pattern of the margins was similar to that seen in 5 normal skin control specimens obtained from the tips of excisional specimens of nevi from unrelated patients in which only occasional discontinuous keratinocyte nuclei labeled for Ki-67. In contrast, 5 randomly chosen verrucae showed nearly continuous Ki-67 labeling of lesional basal and suprabasal keratinocytes, similar to the staining pattern of the biopsy specimen from the papule and increased over that seen in normal skin.
Staining for Ki-67 was much less marked in the biopsy specimen obtained 2 days after the initial one. In this tissue, only discontinuous basal keratinocytes labeled with Ki-67. Staining for CK 5/6 followed a similar pattern. In the first biopsy specimen, there was labeling of the entire basal layer and stratum spinulosum within the area of epidermal hyperplasia, while staining for CK 5/6 was localized predominantly to basal keratinocytes at the periphery of the specimen (Figure 2C). The biopsy specimen obtained 2 days later showed predominantly basal and only slight suprabasal staining of CK 5/6 in both normal and hyperplastic skin. Five verrucae showed CK 5/6 staining of basal and suprabasal keratinocytes, but none showed labeling of the entire epidermis. In the tips of excisional specimens of nevi, CK 5/6 labeled only basal keratinocytes.
COMMENT
In this study, we observed a cutaneous eruption consisting of planar papules and erythema mainly in an intertriginous distribution as well as confluent white plaques of the oral mucosa in a patient after treatment with palifermin, a KGF. While erythema and the effects on the oral mucosa have previously been noted in response to palifermin therapy,4,5,7 to our knowledge a planar papular eruption has not been described.
The papular lesions resembled lichen planus or plane warts in a predominantly (but not exclusively) intertriginous distribution (Figure 1A). However, while histopathologic analysis revealed verrucous epidermal hyperplasia (Figure 2A), the absence of koilocytes and parakeratosis as well as negative results of in situ hybridization studies for HPV makes the diagnosis of verruca unlikely. There were no histopathologic features to suggest a lichenoid inflammatory dermatosis. The markedly increased expression of Ki-67, a cell proliferation marker, throughout the affected areas of skin relative to both clinically unaffected skin (skin adjacent to the area of epidermal hyperplasia, Figure 2B) and normal controls mirrors what is observed in oral mucosa after palifermin treatment.4 Interestingly, the biopsy specimen that was obtained 2 days after the first one, at a time when the eruption was clinically resolving, showed decreased staining with Ki-67 (despite the persistence of epidermal hyperplasia), similar to the decrease in Ki-67 staining observed in oral mucosa biopsy specimens obtained at 48 and 72 hours after palifermin exposure in a clinical study.4
Staining with CK 5/6, a marker of keratinocyte proliferative activity, further distinguishes the unique nature of the observed epidermal proliferation in our patient. In the early specimen, there was labeling of the entire basal layer and stratum spinulosum in lesional skin, while clinically uninvolved skin at the periphery of the specimen showed a predominantly basal layer pattern of staining (Figure 2C). Decreased keratinocyte proliferation was already evident in the biopsy specimen obtained 2 days later, in which there was only basal and suprabasal staining with CK 5/6 within the lesion, following the same trend of attenuated staining seen with Ki-67 over the 2-day interval.
It appears that a unique hyperproliferative state of keratinocytes underlies the papular eruption that was observed in our patient. The 2 possible culprits in this case are melphalan and palifermin, neither of which has previously been associated with any such eruption, to our knowledge. Melphalan has been used for decades without any report of a reaction like the one described herein. Palifermin, on the other hand, is a recently developed drug that is used expressly as a stimulus for keratinocyte growth with a well-described effect of oral mucosa proliferation.4,5 This same keratinocyte growth stimulation is likely the origin of both the papular eruption observed clinically and the epidermal hyperplasia seen histopathologically, providing a biochemical explanation for these findings. We can only speculate as to the reason for the predominantly intertriginous distribution of this eruption, but it may be attributable to increased sensitivity of the keratinocytes to the drug or to increased concentration of the drug at these sites owing to the effects of friction, local temperature, occlusion, eccrine gland density or activity, or a combination thereof.
In conclusion, a new papular eruption that developed after palifermin therapy has been described. The appearance of these lesions likely corresponds to a hyperproliferative state of keratinocytes in response to KGF and appears to be a benign and self-limited condition. Dermatologists, especially those working in inpatient settings, should be aware of this eruption.
Footnotes
Financial Disclosure: None reported.
REFERENCES
- 1.Rubin JS, Osada H, Finch PW, Taylor WG, Rudikoff S, Aaronson SA. Purification and characterization of a newly identified growth factor specific for epithelial cells. Proc Natl Acad Sci U S A. 1989;86(3):802–806. doi: 10.1073/pnas.86.3.802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Farrell CL, Bready JV, Rex KL, et al. Keratinocyte growth factor protects mice from chemotherapy and radiation-induced gastrointestinal injury and mortality. Cancer Res. 1998;58(5):933–939. [PubMed] [Google Scholar]
- 3.Werner S. Keratinocyte growth factor: a unique player in epithelial repair processes. Cytokine Growth Factor Rev. 1998;9(2):153–165. doi: 10.1016/s1359-6101(98)00010-0. [DOI] [PubMed] [Google Scholar]
- 4.Zia-Amirhosseini P, Salfi M, Leese P, et al. Pharmacokinetics, pharmacodynamics, and safety assessment of palifermin (rHuKGF) in healthy volunteers. Clin Pharmacol Ther. 2006;79(6):558–569. doi: 10.1016/j.clpt.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 5.Spielberger R, Stiff P, Bensinger W, et al. Palifermin for oral mucositis after intensive therapy for hematologic cancers. N Engl J Med. 2004;351(25):2590–2598. doi: 10.1056/NEJMoa040125. [DOI] [PubMed] [Google Scholar]
- 6.Keijzer A, Huijgens PC, van de Loosdrecht AA. Palifermin and palmar–plantar erythrodysesthesia. Br J Haematol. 2007;136(6):856–860. doi: 10.1111/j.1365-2141.2007.06509.x. [DOI] [PubMed] [Google Scholar]
- 7.Grzegorczyk-Jaźwińska A, Kozak I, Karakulska-Prystupiuk E, et al. Transient oral cavity and skin complications after mucositis preventing therapy (palifermin) in a patient after allogeneic PBSCT: case history. Adv Med Sci. 2006;51(suppl 1):66–68. [PubMed] [Google Scholar]
- 8.Keefe D, Lees J, Horvath N. Palifermin for oral mucositis in the high-dose chemotherapy and stem cell transplant setting: the Royal Adelaide Hospital Cancer Centre experience. Support Care Cancer. 2006;14(6):580–582. doi: 10.1007/s00520-006-0048-3. [DOI] [PubMed] [Google Scholar]
- 9.Jiang C-K, Magnaldo T, Ohtsuki M, Freedberg IM, Bernerd F, Blumenberg M. Epidermal growth factor and transforming growth factor a specifically induce the activation- and hyperproliferation-associated keratins 6 and 16. Proc Natl Acad Sci U S A. 1993;90(14):6786–6790. doi: 10.1073/pnas.90.14.6786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nuovo GJ, Ishag M. The histologic spectrum of epidermodysplasia verruciformis. Am J Surg Pathol. 2000;24(10):1400–1406. doi: 10.1097/00000478-200010000-00010. [DOI] [PubMed] [Google Scholar]


