Abstract
The relationship between perceived health and walker use has seldom been addressed. Concerns over falls and falls risk are precursors to walker use. We compared the SF-36 scores of 26 women and 14 men, mean age 86.8 ± 6.0 years based on walker use and faller status. An analysis of covariance (ANCOVA) with age as the covariate, compared groups for the SF-36 constructs and totals score. Significant differences were noted between walker users and nonusers in physical functioning, role limitations due to physical problems, general health, and the total SF-36 score. Pairwise comparisons favored nonusers, while no differences were seen due to faller status. Walker use is associated with lower self-perceptions of physical functioning, role limitations due to physical problems, and general health in assisted-living residents. Faller status is not associated with self-perceived health status. Although walker use aids mobility and lowers the probability of falls, further research is needed to determine if the prescription of assistive devices has a more negative impact on self-perceived health than does falling. This possibility could be explained, in part, by the greater activity levels of those individuals who do not depend on walkers.
Keywords: physical function, threshold, walking aid, elderly, perceived health
Introduction
With increasing numbers of vulnerable and frail seniors entering assisted-living facilities, concern about falls and their prevention has grown (Hawes et al 1999; NIC 2000). Falls can negatively impact perceptions of health and well-being, reducing self-confidence, physical activity, and independence (O’Loughlin et al 1993; Vellas et al 1997; Parry et al 2000). Healthcare professionals increasingly recommend walkers to improve ambulation and reduce the risk of falls (Gasman-Hedstrom et al 1995; Molaschi et al 1995). While the mobility and safety benefits of walker use have been reported (Tyson 1998), no information has emerged on whether walker use affects seniors’ perceptions of their health status or physical functioning, both of which are closely associated with overall quality of life.
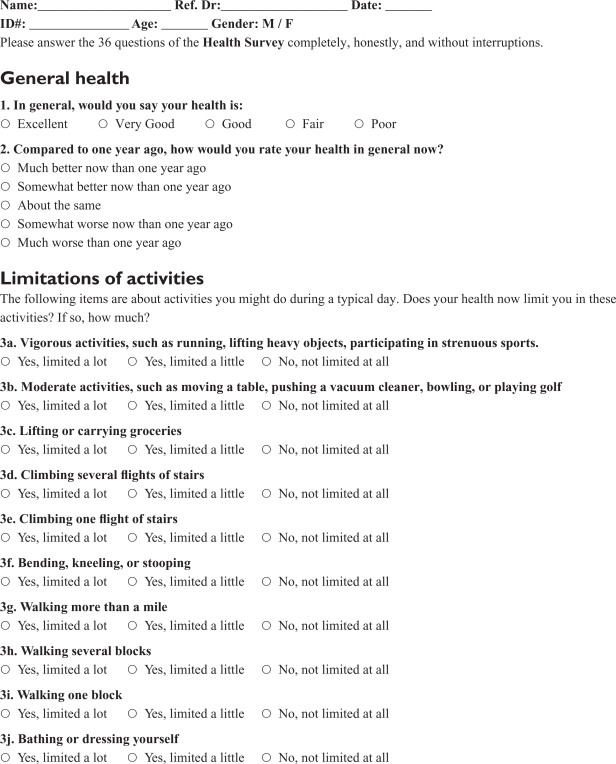
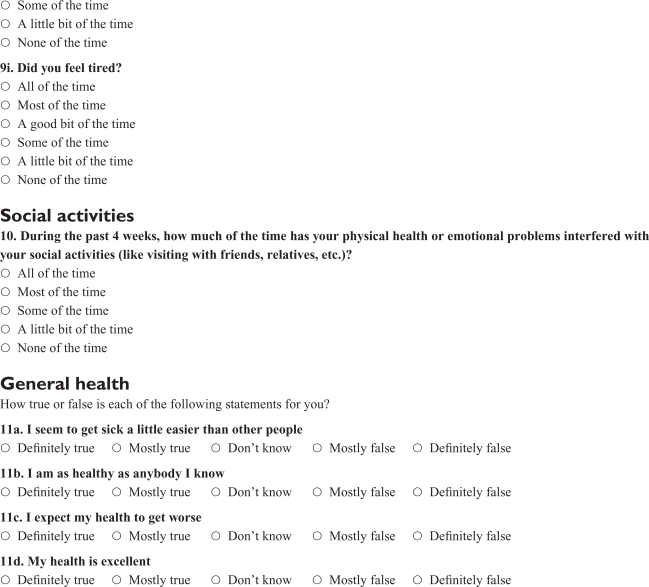
A reliable tool for measuring perceived health is the Short Form 36 (SF-36) questionnaire, created during the Medical Outcomes Study to survey health status (Brazier et al 1992; Ware and Sherbourne 1992; Hayes et al 1995). The SF-36 consists of eight health scales, or constructs, measuring three aspects of health: functional status, well-being, and overall evaluation of health. It also includes an unscaled question measuring change in health status (Hayes et al 1995). It has been validated for use with elderly subjects in an interview setting (Lyons et al 1994).
Low scores on the SF-36, especially on the physical functioning and bodily pain constructs, indicate a reduced level of self-perceived health and physical well-being. Although studies have examined the impact of walker use on cardiorespiratory function (Foley et al 1996) and falls (Hogue 1984), no studies, to our knowledge, have investigated the relationship between walker use and self-perceived health status. Furthermore, no direct comparisons of SF-36 scores in fallers and nonfallers have been reported in relation to walker use.
Here we report total SF-36 scores, as well as scores on eight questionnaire constructs (physical functioning, mental health, general health, role limitations due to physical problems, role limitations due to emotional problems, social functioning, pain, and energy/vitality) for a group of residents from an assisted-living facility at the baseline interview before beginning an exercise intervention study. Scores were analyzed in relation to each resident’s history of falls and walker use. The results indicate that walker use (with or without a history of falls) is associated with self-perceptions of lower health status, whereas a history of falls without walker use is not.
Methods
Participants
Data were collected and analyzed for 40 men and women, mean age 86.8 ± 6.0 years (Mean ± Standard Deviation [SD]), recruited from two assisted-living facilities on the campus of the Miami Jewish Home and Hospital for the Aged (MJHHA). All participants were volunteers for a training study which was later performed as part of Florida’s Teaching Nursing Home program, coordinated through MJHHA’s academic arm, the Stein Gerontological Institute. However, the data presented in this paper were collected before any exercise intervention and participation in the training study was not necessary for a subject’s data to be included in this analysis. Prior to enrolling in the training study, each participant signed an informed consent approved by the MJHHA’s Committee for the Protection of Human Subjects.
The participants in this study had not received any form of exercise intervention or physical therapy within the past year. In addition, to be considered for participation in the study, participants could not present with current cardiovascular problems. These conditions included unstable angina (new onset with activity); active pericarditis, myocarditis, or endocarditis; resting ST segment depression (>3 mm); myocardial infarction within the past three months; symptomatic coronary artery disease or abnormal results on an exercise stress test performed during the initial screening or within the past year; uncontrolled symptomatic congestive heart failure, ejection fraction less than 30%; moderate to severe aortic stenosis, thrombophlebitis, or recent embolism requiring anticoagulants; resting systolic blood pressure 165 mm Hg or above or resting diastolic 95 mm Hg; history of hypertension with exercise or resting pulse rate greater than 90 or less than 50. All participants were free of chronic obstructive pulmonary disease requiring oxygen or steroid medication; renal problems requiring dialysis; anemia (Hgb,10 g/dl); active endocrine disease, such as hyperthyroidism or adrenal insufficiency; and uncontrolled diabetes mellitus (fetal bovine serum >250 mg/dl). Other exclusion criteria included nutrition problems (30 < Body Mass Index <20 kg/m2 and/or albumin <3.2 g/dl), significant unexplained weight change, dementia (Mini-Mental State Examination [MMSE] <25), active major depression (Geriatric Depression Scale >5), poor vision (unable to read size 18 font), orthopedic problems that would limit or be aggravated by resistance training or related exercises, or more than six falls in last six months. Study physicians also screened subjects for medications or drug interactions that might put subjects at risk for falls or other negative events that might occur due to participation in a resistance and agility training exercise program.
Persons who reported falling within the past year were classified as fallers, while those who had not were classified as nonfallers. Falling was defined as an involuntary change of position from standing, bending, reaching, or walking to a position where the person was no longer being supported by both feet, finding himself or herself in contact with the ground or floor. Participants were also classified as walker users or nonusers. Walker use was initially determined by observing which subjects arrived at appointments at the Stein Gerontological Institute using a walker, or were regularly seen using walkers on the MJHHA campus. Additionally, during subsequent visits, all subjects were met at their rooms and accompanied across the campus to our facility, allowing us to observe if they regularly used a walking aid. Since the MJHHA had a specific policy concerning the type of walker acceptable for use in the facility, the only type of walker used by our participants was the traditional four-leg walker (see Figure 1). Most walkers had tennis balls or rollers on the front legs to facilitate movement. Therefore, no stratification was needed for type of walker used. Table 1 presents the age and gender data for the entire sample: fallers and nonfallers; walker users and nonusers; and each of the four comparison groups created using faller status and walker use (NN: nonfaller, nonuser; NW: nonfaller, walker user; FN: faller, nonuser; and FW: faller, walker user).
Figure 1.
Typical four-legged walker used by subjects in the present study.
Table 1.
Subject characteristics
| Group | n | Age (yr) (Mean ± SD) | Gender |
|---|---|---|---|
| Sample | 40 | 86.8 ± 6.0 | M = 14
F = 26 |
| Fallers | 23 | 84.1 ± 5.6 | M = 10
F = 13 |
| Nonfallers | 17 | 88.8 ± 6.2 | M = 4
F = 13 |
| Walker users | 21 | 86.0 ± 4.8 | M = 9
F = 12 |
| Nonusers | 19 | 86.1 ± 7.2 | M = 5
F = 14 |
| NN | 11 | 87.7 ± 4.4 | M = 3
F = 8 |
| NW | 6 | 90.7 ± 8.8 | M = 1
F = 5 |
| FN | 8 | 83.6 ± 4.4 | M = 2
F = 6 |
| FW | 15 | 85.1 ± 6.2 | M = 8
F = 6 |
Abbreviations: FN, faller–no walker; FW, faller–walker; NN, nonfaller–no walker; NW, nonfaller–walker.
Testing
Participants were administered a number of physical tests and questionnaires prior to training. Among these were the two questionnaires used for this study: the SF-36 and a simple inquiry about whether the subjects had fallen during the past year. Both questionnaires were administered by interview.
The SF-36 is a widely used generic patient-based health status survey that measures patient-assessed health based on eight constructs: physical functioning, mental health, general health, role limitations due to physical or emotional problems, social functioning, pain, and energy/vitality. The 35 items that are scored on the SF-36 questionnaire were organized for statistical analysis using these eight constructs (Gasman-Hedstrom et al 1995). Table 2 presents each construct by area, dimension, number of questions, and item number. The 36th item on the SF-36 (question 2), which measures change in health, is neither scored as part of the SF-36 total nor included in any of the eight constructs; therefore, it was not included in this analysis.
Table 2.
Constructs of the SF-36 Health Survey questionnaire (for item numbers see Appendix 1).
| Area | Dimension | Number of questions | Item Numbers |
|---|---|---|---|
| Functional status | Physical functioning | 10 | 3a–j |
| Social functioning | 2 | 6 & 10 | |
| Role limitations (physical problems) | 4 | 4a–d | |
| Role limitations (emotional problems) | 3 | 5a–c | |
| Well-being | Mental health | 5 | 9b, c, d, f, h |
| Vitality | 4 | 9a, e, g, I | |
| Pain | 2 | 7 & 8 | |
| Overall evaluation of health | General health perception | 5 | 1 & 11a–d |
| Health change | 1 | 2 |
Each construct of the SF-36 has a different measurement scale, so scores were transformed to a uniform 0–100 scale using the technique presented in the Biodex Corporation’s Fall Risk Assessment and Conditioning Program manual (BMS 2000). The conversions used the following formula:
Since the total SF-36 score did not involve comparisons among constructs, it was not converted to the 0–100 scale. This conversion algorithm allowed for comparison amongst constructs that would otherwise have noncomparable scores. It was necessary to perform this transformation to interpret differences in perceived health in each area across the groups.
Statistical analysis
A two-way analysis of covariance (ANCOVA), with an interaction term, was performed for each of the eight constructs on the SF-36 and for the total SF-36 score, using faller status and walker use as fixed factors and age as a covariate. Variables that had a significant F value (p ≤ 0.050) in the ANCOVA were analyzed further, with least significant difference (LSD) tests for pairwise comparisons, to measure simple effects. To assist in making multiple comparisons, dummy variables were created using the four previously defined groups. All analyses were performed using the statistical package for the social sciences (SPSS), version 10.1 (SPSS Inc, Chicago, IL, USA).
Results
The study population’s mean age was 86.8 ± 6.0 years. Their mean duration of stay was 16.6 ± 19.6 years. Mean ages did not differ significantly by falling status or walking aid use, nor did they differ by falling status by walking aid use grouping. Duration of stay at the assisted-living facility was not different among falling status by walking aid groups or by falling status. However, walking aid users did have a significantly longer duration of stay 22.9 ± 24.4 months than nonusers 9.7 ± 8.7 months (p = 0.03). The mean scores on the total SF-36 and each construct for both dichotomous mobility variables can be found in Table 3.
Table 3.
Mean scores on individual constructs of the SF-36 and the SF-36 total score based on faller status and walker use
| Fall (1) | PHYSFUNT | ROLEPHYT | ROLEEMOT | MENHEALT | PAINT | ENERGYT | GENHEALT | SF-36 total | |
|---|---|---|---|---|---|---|---|---|---|
| 0 | Mean | 67.35 | 37.50 | 93.75 | 76.24 | 78.47 | 61.25 | 67.65 | 664.36 |
| N | 17 | 16 | 16 | 17 | 16 | 16 | 17 | 17 | |
| Std. Deviation | 24.375 | 18.257 | 18.130 | 16.277 | 15.957 | 22.472 | 17.421 | 159.679 | |
| 1 | Mean | 55.22 | 27.72 | 73.91 | 68.35 | 66.18 | 56.74 | 66.09 | 598.29 |
| N | 23 | 23 | 23 | 23 | 23 | 23 | 23 | 23 | |
| Std. Deviation | 28.702 | 19.928 | 36.177 | 14.518 | 25.619 | 18.806 | 19.185 | 143.982 | |
| Total | Mean | 60.38 | 31.73 | 82.05 | 71.70 | 71.23 | 58.59 | 66.75 | 626.37 |
| N | 40 | 39 | 39 | 40 | 39 | 39 | 40 | 40 | |
| Std. Deviation | 27.301 | 19.628 | 31.387 | 15.595 | 22.759 | 20.227 | 18.242 | 152.475 | |
| Aid (1) | PHYSFUNT | ROLEPHYT | ROLEEMOT | MENHEALT | PAINT | ENERGYT | GENHEALT | SF-36 total | |
| 0 | Mean | 80.53 | 40.79 | 85.96 | 72.84 | 77.78 | 62.37 | 73.95 | 702.06 |
| N | 19 | 19 | 19 | 19 | 19 | 19 | 19 | 19 | |
| Std. Deviation | 14.424 | 14.932 | 33.913 | 19.713 | 22.222 | 20.437 | 15.686 | 127.978 | |
| 1 | Mean | 42.14 | 23.13 | 78.33 | 70.67 | 65.00 | 55.00 | 60.24 | 557.89 |
| N | 21 | 20 | 20 | 21 | 20 | 20 | 21 | 21 | |
| Std. Deviation | 23.053 | 19.981 | 29.170 | 11.051 | 22.009 | 19.868 | 18.267 | 142.225 | |
| Total | Mean | 60.38 | 31.73 | 82.05 | 71.70 | 71.23 | 58.59 | 66.75 | 626.37 |
| N | 40 | 39 | 39 | 40 | 39 | 39 | 40 | 40 | |
| Std. Deviation | 27.301 | 19.628 | 31.387 | 15.595 | 22.759 | 20.227 | 18.242 | 152.475 | |
Abbreviations: ENERGYT, energy; GENHEALT, general health; MENHEALT, mental health; PAINT, pain; PHYSFUNT, physical functioning; ROLEPHYT, role limitations due to physical problems; ROLEEMOT, role limitations due to emotional problems.
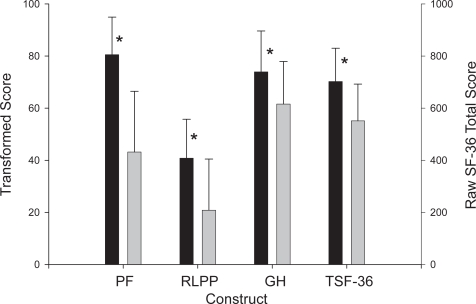
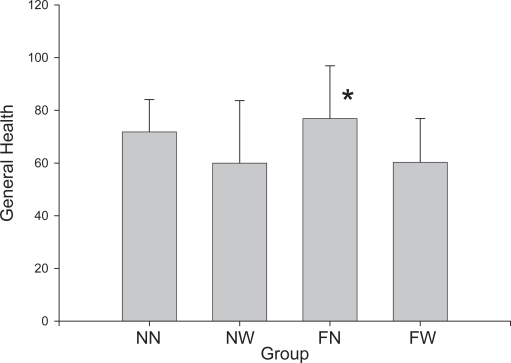
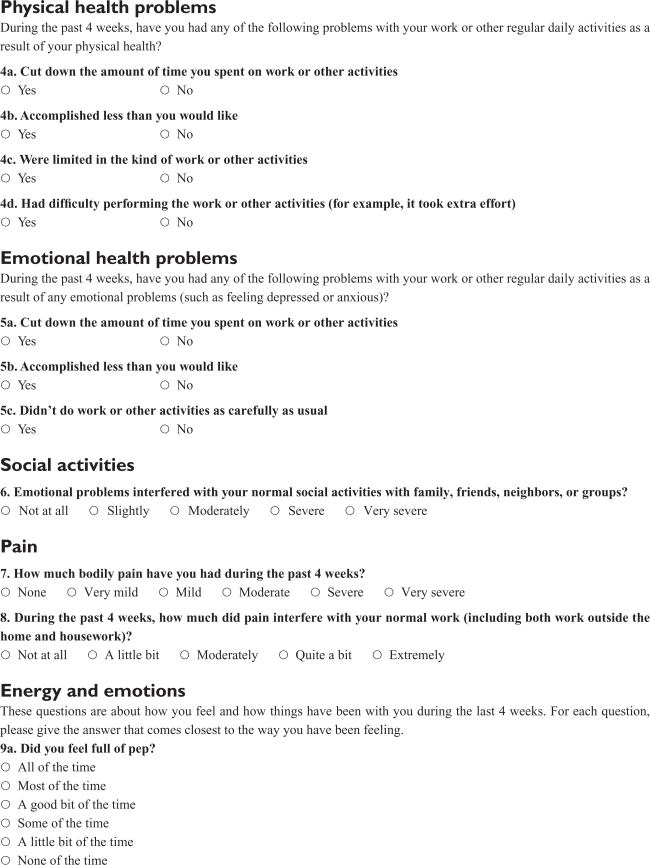
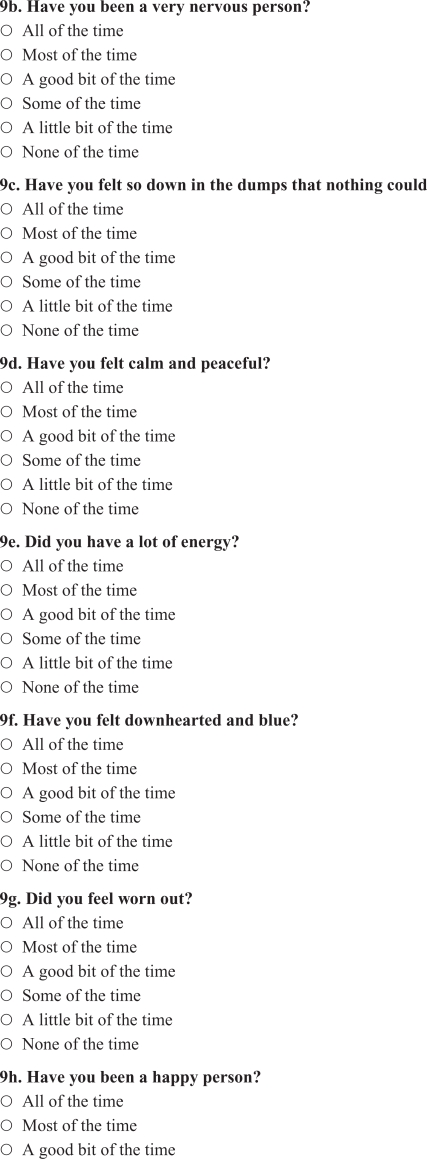
The ANCOVA identified significant differences between those who used walkers and those who did not for three constructs: physical functioning (p < 0.001), role limitations due to physical problems (p = 0.012), and general health (p = 0.015), as shown in Figure 2. Significant differences were also found in the total SF-36 score (p = 0.006). The ANCOVA failed to show significant differences between fallers and nonfallers for any of the other dependent variables. Age was not a significant factor in this analysis. There was no significant interaction between walker use and faller status.
Figure 2.
Results of ANCOVA comparing walker users to nonusers on the physical functioning (PF), role limitations due to physical problems (RLPP), and general health (GH) constructs, as well as the total SF-36 score (TSF-36).
Note: *Significant difference between groups, p < 0.05.
Abbreviations: ANCOVA, analysis of covariance.
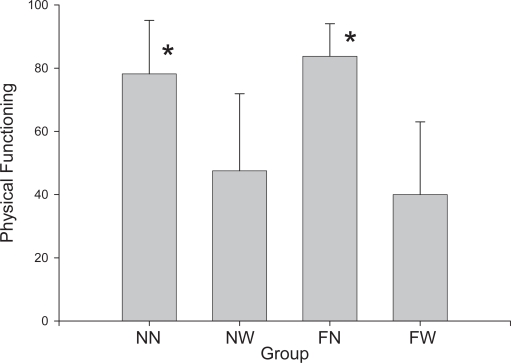
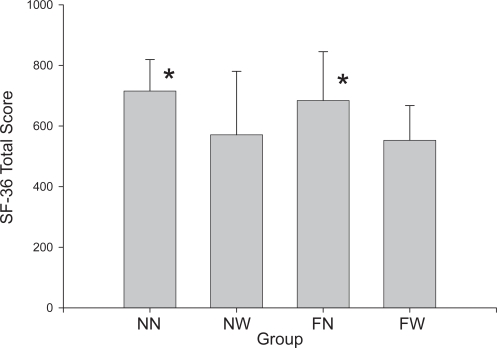
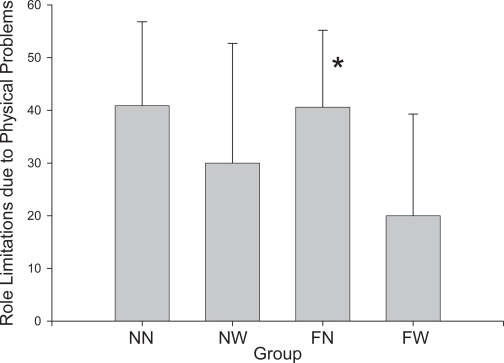
Figures 3 through 6 show the scores for the physical functioning construct, the role limitations due to physical problems construct, the general health construct, and the total SF-36, respectively. Table 4 presents the results of the multiple comparisons using the LSD test. On physical functioning, the NN group scored 30.7% higher (better functioning) than the NW group (p = 0.004), and the FN group scored 36.25% higher than the FW group (p < 0.001). The FN group also scored 19.79% higher than the FW group (p = 0.017) on the role limitations due to physical problems construct, and 16.54% higher on the general health construct (p = 0.037). Comparisons of the total SF-36 scores (not scaled) showed that the NN group scored 144.25 points higher than the NW group (p = 0.048), while the FN group scored 131.26 points higher than the FW group (p = 0.037).
Figure 3.
Data for the four comparison groups on the physical functioning construct.
Note: *Significant difference between NN and NW or FN and FW groups, p < 0.05.
Abbreviations: FN, faller–no walker; FW, faller–walker; NN, nonfaller–no walker; NW, nonfaller–walker.
Figure 6.
Data for the four comparison groups on the total SF-36 score.
Note: *Significant difference between NN and NW or FN and FW groups, p < 0.05.
Abbreviations: FN, faller–no walker; FW, faller–walker; NN, nonfaller–no walker; NW, nonfaller–walker.
Table 4.
Multiple comparisons using LSD test
| Dependent variable | Group | Mean difference | Standard error | Significance | |
|---|---|---|---|---|---|
| Physical functioning | NN | NW | 30.68 | 10.00 | 0.004 |
| FN | FW | 43.75 | 8.63 | 0.000 | |
| Role limitations due to physical functioning | NN | NW | 10.91 | 9.68 | 0.268 |
| FN | FW | 19.79 | 7.86 | 0.017 | |
| General health | NN | NW | 11.82 | 8.87 | 0.191 |
| FN | FW | 16.54 | 7.65 | 0.037 | |
| SF-36 total | NN | NW | 144.25 | 70.43 | 0.048 |
| FN | FW | 131.26 | 60.76 | 0.037 |
Abbreviations: FN, faller–no walker; FW, faller–walker; LSD, least significant difference; NN, nonfaller–no walker; NW, nonfaller–walker; SF, short-form.
Discussion
The major finding of this study is that among participants in an assisted-living environment, those using walkers perceive themselves to have lower physical functioning, poorer general health, and more role limitations due to physical problems than nonusers. Furthermore, in this population, falling history does not appear to be associated with lower scores on the individual SF-36 constructs or the total SF-36 score.
Although the physical functioning, role limitations due to physical problems, and general health constructs and the overall SF-36 score showed significant differences due to walker use, differences within the other constructs were not statistically significant. The failure of the differences in percentage scores on the other constructs to reach statistical significance may be attributable to the composition of the questionnaire, with some constructs comprising a relatively small portion of the total number of questions. The constructs with fewer questions may, therefore, have an insufficient number of items to generate statistical significance. For example, the physical functioning, role limitations due to physical problems, and general health constructs represent 27%, 11%, and 14% of the total questions, respectively. The other constructs, with the exception of mental health (14%) and vitality (11%), each make up between 5% and 8% of the questionnaire. This may explain in part why the results for the physical functioning construct (p < 0.001) and the total SF-36 score (p = 0.006) showed the greatest levels of statistical significance among the constructs analyzed. However, the lack of significant difference among groups on the mental health and vitality constructs is difficult to explain, since they are substantial components of the SF-36 (14% and 11%, respectively) and seem intuitively associated with falls and walker use.
An alternative explanation is that significant differences can be expected between walker users and nonusers for the activity-based constructs, since the general public perceives factors dictating walker use, such as balance and mobility, as physically rather than mentally based. On that basis, this pattern seems logical, ie, that those who use walkers would perceive limitations in physical rather than mental health. This explanation also suggests that perceptions of physical health (38% of the SF-36) have a strong impact on a person’s perception of his or her overall health.
The findings of this study support the literature on the relationship between mobility and psychosocial factors of health. Decreased mobility often results in lower perceptions of health and well-being in elderly persons (Spirduso and Gilliam-MacRae 1991). In fact, researchers have determined mobility to be the most important factor in an older person’s perceived health and well-being (Gooding et al 1988; Bowling et al 1993). Mobility has also been identified as an integral part of both self-esteem and functional health (Bourrent et al 2002). Nurses have described the use of a walker as a stigma associated with old age, affecting an elderly person’s sense of identity and self-worth, and often resulting in a withdrawal from social interactions (Rush and Ouellet 1997). Similarly, Mitchell and Jonas-Simpson (1995) found that the freedom to move around independently significantly impacted quality of life, while Gignac and Cott (1998) found that a loss of physical independence was associated with poorer psychological well-being. Therefore, the prescription of walkers may focus elders on their limited mobility, resulting in a perception of decreased health and quality of life.
Our findings that walker use is more strongly associated with both physical functioning constructs and overall health score on the SF-36 than faller status are supported by the results of a number of studies. For example, Kressig and colleagues (2001) reported that individuals with a greater fear of falling, as measured by the Falls Efficacy Scale (FES) and the Activities-Specific Balance Confidence (ABC) Scale, were more likely to be depressed and more likely to report the use of a walking aid than individuals who were not fearful. In addition, in their multivariate logistic model, walking aid use, along with slow gait speed and being African-American, was directly related to being more fearful of falling.
It should be recognized, however, that walking aid use may positively affect both mobility and fitness levels. Honeyman and colleagues (1996) reported that the use of a wheeled walker resulted in a significant increase in 6-minute walking distance, a significant reduction in hypoxemia with walking, and a significant reduction in breathlessness during the walk test. By reducing disability and breathlessness, a wheeled walker may improve quality of life in individuals with severe impairments in daily function. Unfortunately, no measures of perceived self-health were included in that study. In contrast, Holder and colleagues (1996) found that unassisted ambulation resulted in the lowest oxygen consumption per meter walked, the greatest walking speed, and lowest ratings of perceived exertion when compared with nonweight-bearing ambulation using axillary crutches, standard walkers, and wheeled walkers. In addition, axillary crutches resulted in lower oxygen consumption and greater walking velocity than either standard or wheeled walker use (Holder et al 1996).
Our study had several limitations. First, the faller status of some participants was based on a single incident, which did not take into account the severity of the fall or if the fall resulted in serious injury. However, the physicians who screened subjects for the study did exclude them on the basis of musculo-skeletal limitations resulting from disease or injury that would limit their ability to perform upper and lower body exercise training.
Second, falls are often subject to misinterpretation due to a lack of consensus in the research community on falls classification (Lach et al 1991). We attempted to reduce the impact of this factor by clearly defining a fall within the intervention process, but subtle differences may still have existed among participants. Further, the baseline interview did not allow for us to separate repeat fallers, who may be at increased risk to perceive their health more negatively, and one-time or infrequent fallers.
Third, fall status was based on subject recall. While researchers have reported that patients recall falls and injuries well within a one-year period with the predictive value of recalling a fall at 92% (Hale et al 1993), there are certainly conflicting results (Cummings et al 1988). We attempted to reduce the recall bias among groups by uniform definition of the term, assurances of anonymity, and exclusion criteria that controlled MMSE scores.
Fourth, there is some question concerning the reliability and validity of the SF-36 with older patients with physical disabilities. To reduce this problem, all tests were given using face-to-face interviews and a minimal MMSE score of 25 was required for all subjects participating in the study. Using these criteria, Seymour and colleagues (2001) showed that the physical function dimension scores on the SF-36 attained the criterion level for construct validity when correlated with functional independence measures; however, their subjects still did not attain the levels of reliability and validity previously reported for the SF-36 in younger subjects.
Fifth, while other research has confirmed the reliability and validity of the SF-36 with frail older patients, its ability to monitor clinical change in this population remains in question (Stadnyk et al 1998). However, it is beyond the scope of this paper to estimate the degree to which this lack of clinical sensitivity could have affected our findings.
Since this study used a cross-sectional analysis, we cannot infer a causal relationship between walker use and decreased self-perceived health. Therefore, a fundamental question remains as to whether the walker itself was responsible for these perceptions, or whether they reflect the mobility and balance limitations that precipitated its use. Similarly, a prospective cohort study using a study population that is more diverse with regard to race, ethnicity, and socioeconomic status would better determine whether there is a causal relationship between walker use and lower self-perceived health.
Our results show that persons using walkers have a significantly lower perception of their physical health, as measured by the SF-36. The lower self-perception of physical ability in these patients could have serious psychological and physical consequences. Factors other than physical limitations, such as staff concerns, understaffing, or fear of institutional liability, may also be involved in the decision to prescribe walkers. Therefore, a clear diagnosis of the need for a walker is important to eliminate accelerated reductions in self-perceived physical function. Interventions such as exercise and motor skill practice, which can delay or even eliminate the need for walkers in certain individuals, may be feasible alternatives. Such interventions can also reduce dependence on walkers after they have been prescribed.
Once a walker is prescribed, emphasis should be placed on avoiding any stigma related to use of these devices, with efforts focusing on preserving the patient’s accurate perception of his or her physical health. Also, it may be useful to encourage individuals using assistive devices to remain as active as possible to maintain their level of self-efficacy. These methods may ensure that a proper balance is maintained between a patient’s health, safety, and dignity.
A final comment should be added concerning walker use and fall probability. In a study by Graafmans and colleagues (2003), the researchers found that 710 elderly men and women with very high levels of physical activity had an extremely low probability of falling and, therefore, would benefit little from the use of a walker or other walking aid. However, persons with intermediate or high intermediate activity levels were found to be at a much higher risk for falling. In fact, this relationship was nonlinear, which strongly favors a higher probability of falls as activity levels decrease. These data, in conjunction with our results, argue strongly for a nonlinear approach to exercise interaction and walking aid use. During early stages of fitness training, when exercise intervention is beginning to positively affect mobility, walking aid use may be advisable to reduce the probability of falls which increases with the increase in activity. Later, walker use might taper off as the patient reaches a high level of mobility and physical activity, thereby positively affecting both the physical and mental state of the patient.
While we feel this is an excellent theoretical model, specific questions such as functional thresholds, exercise adaptation patterns, and other modifying circumstances must be considered to properly structure the practical nature of the exercise intervention.
Figure 4.
Data for the four comparison groups on the role limitations due to physical problems construct.
Note: *Significant difference between NN and NW or FN and FW groups, p < 0.05.
Abbreviations: FN, faller–no walker; FW, faller–walker; NN, nonfaller–no walker; NW, nonfaller–walker.
Figure 5.
Data for the four comparison groups on the physical functioning construct.
Note: *Significant difference between NN and NW or FN and FW groups, p < 0.05.
Abbreviations: FN, faller–no walker; FW, faller–walker; NN, nonfaller–no walker; NW, nonfaller–walker
Acknowledgments
The authors are grateful for support from the Teaching Nursing Home program, funded by the State of Florida Agency for Health Care Administration, during the data analysis and manuscript preparation portions of this project. In addition, we would like to thank the University of Miami students and Stein Gerontological Institute employees who helped with data collection, including Aaron McEntire, David Sandler, and Angie Van Bemden. Finally, we would like to thank Drs. Jay Wilkinson, David Lee, and Robert Duncan of the University of Miami Department of Epidemiology and Public Health for their help and advice during the analysis of these data.
Appendix 1 Numerical coding for the SF-36 as used in this study (see Table 2)
SF-36 Questionnaire
References
- [BMS] Biodex Medical Systems, Inc. Fall risk assessment and conditioning program: balance and mobility evaluation and intervention protocol. Shirley; New York: 2002. [Google Scholar]
- Bourret EM, Bernick LG, Cott CA, et al. The meaning of mobility for residents and staff in long-term care facilities. J Adv Nurs. 2002;37:338–45. doi: 10.1046/j.1365-2648.2002.02104.x. [DOI] [PubMed] [Google Scholar]
- Bowling AA, Farquhar M, Grundy E, et al. Changes in life satisfaction over a two and a half year period among very elderly people living in London. Soc Sci Med. 1993;36:641–55. doi: 10.1016/0277-9536(93)90061-8. [DOI] [PubMed] [Google Scholar]
- Brazier JE, Harper R, Jones NM, et al. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. BMJ. 1992;305(6846):160–4. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings SR, Nevitt MC, Kidd S. Forgetting falls. The limited accuracy of recall of falls in the elderly. J Am Geriatr Soc. 1988;36:613–16. doi: 10.1111/j.1532-5415.1988.tb06155.x. [DOI] [PubMed] [Google Scholar]
- Foley MP, Prax B, Crowell R, et al. Effects of assistive devices on cardiorespiratory demands in older adults. Phys Ther. 1996;76:1313–19. doi: 10.1093/ptj/76.12.1313. [DOI] [PubMed] [Google Scholar]
- Gasman-Hedstrom G, Sonn V, Aneansson A. Different kinds of services and informal support in daily life activities in a community-based elderly population. Aging (Milano) 1995;7:371–8. doi: 10.1007/BF03324348. [DOI] [PubMed] [Google Scholar]
- Gignac AM, Cott C. A conceptual model of independence and dependence for adults with chronic physical illness and disability. Soc Sci Med. 1998;47:739–53. doi: 10.1016/s0277-9536(98)00149-x. [DOI] [PubMed] [Google Scholar]
- Gooding BA, Sloan M, Amsel R. The well-being of older Canadians. Can J Nurs Res. 1988;20:5–18. [PubMed] [Google Scholar]
- Graafmans WC, Lips P, Wyheuzen GJ, et al. Daily physical activity and the use of a walking aid in relation to falls in elderly people in a residential care setting. Z Gerontol Geriat. 2003;36:23–8. doi: 10.1007/s00391-003-0143-8. [DOI] [PubMed] [Google Scholar]
- Hale WA, Delany MJ, Cable T. Accuracy of patient recall and chart documentation of falls. J Am Board Fam Pract. 1993;6:239–42. [PubMed] [Google Scholar]
- Hawes C, Rose M, Phillips OS. A national study of assisted living for the frail elderly: results of a national survey of facilities. Beachwood, OH: Myers Research Institute; 1999. [Google Scholar]
- Hayes V, Morris J, Wolfe C, et al. The SF-36 health survey questionnaire: is it suitable for use with older adults? Age Ageing. 1995;24:120–5. doi: 10.1093/ageing/24.2.120. [DOI] [PubMed] [Google Scholar]
- Hogue CC. Falls and mobility in late life. J Am Geriatr Soc. 1984;32:858–61. doi: 10.1111/j.1532-5415.1984.tb06304.x. [DOI] [PubMed] [Google Scholar]
- Holder CG, Haskvitz EM, Weltman A. The effects of assistive devices on oxygen cost, cardiovascular stress, and perception of nonweight-bearing ambulation. J Orthop Sports Phys Ther. 1996;18:537–42. doi: 10.2519/jospt.1993.18.4.537. [DOI] [PubMed] [Google Scholar]
- Honeymann P, Barr P, Stubbing DG. Effects of a walking aid on disability, oxygenation, and breathlessness in patients with chronic airflow limitations. J Cardiopulm Rehabil. 1996;16:63–7. doi: 10.1097/00008483-199601000-00008. [DOI] [PubMed] [Google Scholar]
- Kressig RW, Wolf SL, Sattin RW, et al. Associations of demographic, functional and behavioral characteristics with activity-related fear of falling among older adults transitioning to frailty. J Am Geriatr Soc. 2001;49:1456–62. doi: 10.1046/j.1532-5415.2001.4911237.x. [DOI] [PubMed] [Google Scholar]
- Lach HW, Reed AT, Arfken CL, et al. Falls in the elderly: reliability of a classification system. J Am Geriatr Soc. 1991;39:197–202. doi: 10.1111/j.1532-5415.1991.tb01626.x. [DOI] [PubMed] [Google Scholar]
- Lyons RA, Perry HM, Littlepage BN. Evidence for the validity of the short-form 36 questionnaire (SF-36) in an elderly population. Age Ageing. 1994;23:182–4. doi: 10.1093/ageing/23.3.182. [DOI] [PubMed] [Google Scholar]
- Mitchell GJ, Jonas-Simpson C. Quality of life: exploring the client’s perspective. Toronto, Canada: The Queen Elizabeth Hospital; 1995. [Google Scholar]
- Molaschi M, Ponzetto M, Ferrario E, et al. Health and functional status in elderly patients living in nursing homes. Arch Gerontol Geriatr. 1995;21:267–76. doi: 10.1016/0167-4943(95)00661-4. [DOI] [PubMed] [Google Scholar]
- [NIC] National Investment Center for the Seniors Housing and Care Industries. NIC national supply estimate of seniors’ housing and care properties. Annapolis, MD: NIC; 2000. [Google Scholar]
- O’Loughlin JL, Robitaille Y, Boivin JF, et al. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993;137:342–54. doi: 10.1093/oxfordjournals.aje.a116681. [DOI] [PubMed] [Google Scholar]
- Parry SW, Steen N, Galloway SR, et al. Falls and confidence related quality of life outcome measures in an older British cohort. Postgrad Med J. 2000;77:103–8. doi: 10.1136/pmj.77.904.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush K, Ouellet L. Mobility aids and the elderly client. J Gerontol Nurs. 1997;23:7–15. doi: 10.3928/0098-9134-19970101-08. [DOI] [PubMed] [Google Scholar]
- Seymour DG, Ball AE, Russell EM, et al. Problems in using health survey questionnaires in older patients with physical disabilities. The reliability and validity of the SF-36 and the effect of cognitive impairment. J Eval Clin Pract. 2001;7:411–18. doi: 10.1046/j.1365-2753.2001.00296.x. [DOI] [PubMed] [Google Scholar]
- Spirduso W, Gilliam-MacRae P. Physical activity and quality of life in the frail elderly. In: Birren JE, Lubben JE, editors. The concept and measurement of quality of life in the frail elderly. New York: Academic Pr; 1991. pp. 226–55. [Google Scholar]
- Stadnyk K, Calder J, Rockwood K. Testing the measurement properties of the Short Form-36 Health Survey in a frail elderly population. Clin Epidemiol. 1998;51:827–35. doi: 10.1016/s0895-4356(98)00061-4. [DOI] [PubMed] [Google Scholar]
- Tyson SF. The support taken through walking aids during hemiplegic gait. Clin Rehabil. 1998;12:395–401. doi: 10.1191/026921598669871795. [DOI] [PubMed] [Google Scholar]
- Vellas BJ, Wayne SJ, Romero LJ, et al. Fear of falling and restriction of mobility in elderly fallers. Age Ageing. 1997;26:189–93. doi: 10.1093/ageing/26.3.189. [DOI] [PubMed] [Google Scholar]
- Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36) Med Care. 1992;30:473–83. [PubMed] [Google Scholar]