Abstract
Significant host heterogeneity in susceptibility to tuberculosis exists both between and within mammalian species. Using a mouse model of infection with virulent Mycobacterium tuberculosis (Mtb), we identified the genetic locus sst1 that controls the progression of pulmonary tuberculosis in immunocompetent hosts. In this study, we demonstrate that within the complex, multigenic architecture of tuberculosis susceptibility, sst1 functions to control necrosis within tuberculosis lesions in the lungs; this lung-specific sst1 effect is independent of both the route of infection and genetic background of the host. Moreover, sst1-dependent necrosis was observed at low bacterial loads in the lungs during reactivation of the disease after termination of anti-tuberculosis drug therapy. We demonstrate that in sst1-susceptible hosts, nonlinked host resistance loci control both lung inflammation and production of inflammatory mediators by Mtb-infected macrophages. Although interactions of the sst1-susceptible allele with genetic modifiers determine the type of the pulmonary disease progression, other resistance loci do not abolish lung necrosis, which is, therefore, the core sst1-dependent phenotype. Sst1-susceptible mice from tuberculosis-resistant and -susceptible genetic backgrounds reproduce a clinical spectrum of pulmonary tuberculosis and may be used to more accurately predict the efficacy of anti-tuberculosis interventions in genetically heterogeneous human populations.
Tuberculosis remains a global epidemic, with one-third of the population infected, 9 million new active cases, and almost 2 million deaths each year.1 Existing anti-tuberculosis vaccines (BCG) and drugs have proven insufficient for global control of the disease. Many investigators are working to develop novel, more efficient interventions based on animal models that recapitulate key aspects of the human disease. For tuberculosis, however, which animal model better suits this purpose remains controversial.2,3
Mouse models have played a key role in identification of essential mechanisms of host resistance to mycobacterial infections.4,5,6 However, how closely the mouse disease resembles critical aspects of pulmonary tuberculosis in tuberculosis-susceptible, but immunocompetent humans, has been less clear. On the one hand, tuberculosis infection in immunocompetent inbred mouse strains, as in humans, predominantly targets the lungs.6 On the other hand, typical mouse lesions described in the literature lack central necrosis, a characteristic and defining feature of well-organized tuberculosis lesions in immunocompetent humans. Importantly, tuberculosis lung lesions in standard mouse strain are significantly less hypoxic than human granulomas.2,3,7 These differences in lesion environment are likely to induce dissimilar functional states of the bacteria in human and mouse lungs. This raises the concern that the efficacy of anti-tuberculosis vaccines, immunomodulators, or drug combinations determined using experimental mouse models may not foretell success in human populations.
This skepticism regarding the generic mouse model of tuberculosis is based on the analysis of granuloma pathobiology in a very limited set of mouse strains. Meanwhile, similar to humans and other mammalian species, there is broad variation in tuberculosis susceptibility among laboratory mouse strains,5 although the development of well-structured pulmonary granulomas has not been described until recently. The C3HeB/FeJ substrain of the standard inbred mouse strain C3H offers a rare, possibly unique phenotype: although immunocompetent, these mice nevertheless develop large necrotic lesions in the lungs, after either systemic intravenous or aerosol infections with virulent Mycobacterium tuberculosis.8,9 The C3HeB/FeJ lung lesions bear remarkable similarity to tuberculosis lesions in the lungs of susceptible human patients, nonhuman primates, rabbits, and guinea pigs.10 This allows use of the many tools and reagents available for mice to conduct in-depth immunological and genetic analysis of mechanisms underlying necrosis in lung lesions—a key element of M. tuberculosis virulence.11,12,13,14
Previously, we used forward genetic analysis of a cross of B6 (resistant) and C3HeB/FeJ (susceptible) inbred mouse strains to define the polygenic control of tuberculosis resistance in this model.8 We have found that the B6 mice carry four major resistant alleles of quantitative trait loci mapped to mouse chromosomes 1, 7, 15, and 17 (overlapping with the H2 locus) and one susceptibility allele on chromosome 12.9,15 The chromosome 1 locus sst1 (for supersusceptibility to tuberculosis 1) had an early effect on tuberculosis progression: ∼80% of mice homozygous for the C3H-derived susceptible allele of the sst1 locus succumbed to tuberculosis infection within the first 4 to 7 weeks.9 Their early death correlated with the formation of lung necrotic lesions typical for the parental C3HeB/FeJ strain. Transfer of the B6-derived resistant allele of the sst1 locus onto a C3H-susceptible background prevented necrosis formation and increased the survival of the sst1-resistant congenic C3H.B6-sst1 mice to 10 to 12 weeks.9 In contrast, resistance loci on chromosomes 7 and 15 did not prevent lung necrosis.16 We hypothesized that formation of necrosis within tuberculosis lung lesions is a specific effect of the C3HeB/FeJ-derived susceptible allele of the sst1 locus, a postulate tested in the experiments reported here.
In multigenic traits, phenotypic expression of individual quantitative trait loci may be significantly affected by genetic background and even disappear as a result of compensatory genetic interactions.17 Meanwhile the most consistent manifestation of the genetic locus, independent of the genetic background, will most likely reveal its fundamental role. Using novel congenic mice (B6.C3H-sst1), we tested the effect of the susceptible allele of the sst1 locus on tuberculosis progression in a genetically resistant background. This genetic background modified the sst1-mediated phenotype in a quantitative manner, but even in the presence of the resistance alleles on chromosomes 7, 15, and 17, the sst1 locus controlled formation of necrosis within tuberculosis lung lesions. This effect was lung-specific, but independent of a route of infection, systemic or pulmonary. Moreover the sst1-dependent necrosis was observed in the lungs at low bacterial loads after anti-tuberculosis drug therapy predisposing to pulmonary reactivation.
Materials and Methods
Mice
C57BL/6J (B6) mice were purchased from The Jackson Laboratory, Bar Harbor, ME. The congenic B6.C3H-sst1 mice were generated by introgression of a 12-cM interval of C3HeB/FeJ-derived susceptible sst1 allele into the B6 strain as previously described.15 Mice were bred and maintained under specific pathogen-free conditions in the animal facility of Harvard School of Public Health. Autoclaved food and water were provided ad libitum. All experiments were performed with the full knowledge of and approval of the Standing Committee on Animals at Harvard School of Public Health.
Bacteria and Infection of Mice
To cause tuberculosis infection, mice were infected intravenously via tail vein with 5 × 104 CFU/mouse of Mycobacterium tuberculosis (Erdmann strain; Trudeau Institute, Saranac Lake, NY) in 100 μl of phosphate-buffered saline (PBS). The preparation of mycobacterial suspensions has been described elsewhere.18 Briefly, M. tuberculosis was grown to mid-log phase in Middlebrook 7H9 liquid medium (BD Biosciences, Franklin Lakes, NJ) enriched with 10% OADC (oleic acid/albumin/catalase/dextrose), 0.05% Tween 80, and 0.5% glycerol, washed, resuspended in PBS containing 1% fetal calf serum and 10% glycerol, aliquoted, and frozen at −80°C until use. For infection of mice, the frozen stock was melted, sonicated, and diluted in PBS containing 0.05% Tween 80. To assess mycobacterial loads in spleens, livers, and lungs, 0.1 ml of serial 10-fold dilutions of organ homogenates were plated onto Middlebrook 7H10 agar enriched with 10% OADC and 0.5% glycerol, and colonies were counted after 21 to 28 days of incubation at 37°C. To assess drug resistance of M. tuberculosis isolated during reactivation we used a conventional drug susceptibility testing method APP (agar plate proportion) with minor modification. Aerosol infection was performed using Wisconsin aerosol chamber (College of Engineering Shops at the University of Wisconsin, Madison, WI) as described before.19
For infection of macrophages in vitro, the bacteria from a frozen stock were grown in liquid medium with agitation for 4 to 6 days, washed twice, sonicated using a cup sonifier (Branson Ultrasonics, Danbury, CT) twice for 5 seconds and filtered through a 5-μm filter (Pall Corporation, East Hills, NY). OD of the filtrate was measured at 600 nm to estimate the bacterial concentration. The exact number of bacteria in inoculum was determined by plating 10-fold serial dilutions on 7H10 agar. Colonies were counted after incubation for 3 weeks at 37°C. In the reactivation experiment, mice were infected intravenously with 5 × 104 CFU/mouse of mid-log phase M. tuberculosis. Three months after the challenge mice were given isoniazid (INH) in drinking water (10 mg per 100 ml) for 90 days.
Histopathology
Organs of infected animals were fixed for >24 hours in 10% formalin and embedded in paraffin. Hematoxylin and eosin staining and Gomori’s OneStep Trichrome staining were performed using standard procedures at the Rodent Histopathology Core Facility, Harvard Medical School. Slides were examined by a pathologist (L.K.) without knowledge of experimental group.
Immunohistochemistry
Histological sections were deparaffinized in xylene and rehydrated through a series of ethanol washes (100%, 95%, 70%, and 50%) for 3 minutes each, after which they were washed in distilled water. The sections were then blocked with peroxidase blocking solution (3% hydrogen peroxide in methanol) for 20 minutes and were placed in antigen retrieval buffer (10 mmol/L sodium citrate buffer, pH 6.0) for 10 minutes. Incubation with primary rabbit polyclonal antibody to iNOS (inducible nitric oxide synthase) (1:5000; Millipore Corp., Billerica, MA) took place for 2 hours in a humid chamber at room temperature. The sections were then washed with PBS and incubated with biotinylated SP-conjugated AffinPure donkey anti-rabbit IgG (1:500; Jackson ImmunoResearch Laboratories, West Grove, PA) at room temperature in a humid chamber. Detection was performed with the Vectastain Elite ABC kit (Vector Laboratories, Burlingame, CA) for 30 minutes. Sections were then incubated with the 3,3′-diaminobenzidine peroxidase substrate kit (Vector Laboratories) for 10 minutes. Negative and control sections were also stained for comparison analyses. Acid-fast fluorescence staining was used for identification of acid-fast bacilli with Auramine/Rhodamine dye (0.1% Auramine O, 0.01% Rhodamine B; Sigma-Aldrich, St. Louis, MO) for 15 minutes at 37°C. Sections were then counterstained with Mayer’s hematoxylin (Sigma-Aldrich) and dehydrated with a succession of ethanol washes according to standard protocols and mounted for viewing under light and fluorescent microscopy (Nikon, Tokyo, Japan).
Isolation of Bone Marrow-Derived Macrophages (BMDMs) and Infection with M. tuberculosis in Vitro
BMDMs were isolated from femurs and tibias of male mice (6 to 10 weeks old) by centrifugation at 1700 × g for 20 minutes at room temperature on a NycoPrep gradient (Axis-Shield PoC, Oslo, Norway), washed, and cultured in 25-cm2 tissue culture flasks (1 to 3 × 107 cells per flask; BD Falcon, Franklin Lakes, NJ) in Dulbecco’s modified Eagle’s medium/F12 50/50 medium (HyClone, Logan, UT) supplemented with 10% fetal calf serum (HyClone), 2 mmol/L l-glutamine (HyClone), 1 ng/ml interleukin (IL)-3 (Sigma-Aldrich), and 10% L-929 fibroblast-conditioned medium as a source of macrophage colony stimulation factor (M-CSF). Next day nonadherent cells were harvested and transferred into 75-cm2 tissue culture flacks (BD Falcon) for 2 days. Nonadherent cells were harvested, washed, and plated to six-well tissue culture plates (BD Falcon) in the same medium without IL-3. The cells were maintained for 6 days by feeding with fresh medium every 2 days to form monolayer. BMDM monolayers were infected with M. tuberculosis at a multiplicity of infection (MOI) one bacteria per one macrophage (MOI 1:1). Six hours after infection cells were washed to remove extracellular mycobacteria and incubated in complete medium. At indicated time points supernatants and TRIzol samples (see below) were collected.
RNA Isolation and Quantitative Real-Time Polymerase Chain Reaction (PCR)
RNA samples from BMDMs were prepared using TRIzol reagent (Invitrogen, Carlsbad, CA) followed by treatment with the DNAfree kit (Ambion, Austin TX) according to the manufacturer’s instructions. Total RNA was reverse-transcribed using RETROscript kit (Ambion) and random decamers and diluted with sterile water to 100 μl. Expression of genes was analyzed by quantitative real-time PCR, each reaction sample contained the following reagents in 25 μl: 1.25 U of AmpliTaqGold DNA polymerase (Applied Biosystems, Foster City, CA), 1× GeneAmp PCR buffer II, 2.5 mmol/L MgCl2, 0.2 mmol/L dNTPs, 0.1 μmol/L primers, 1/30,000 dilution of 10,000× Syber Green nucleic acid stain (Invitrogen), 100 nmol/L 6-carboxy-X-rhodamine (ROX reference dye; Invitrogen), and 5 μl of cDNA sample. Reaction was run on ABI Prism 7900HT sequence detection system (Applied Biosystems) using the following conditions: 10 minutes at 95°C, 40 cycles (95°C, 20 seconds; 60°C, 30 seconds; 72°C, 40 seconds), 5 minutes at 72°C, and one cycle (95°C, 15 seconds; 60°C, 15 seconds; 72°C, 15 seconds) for a dissociation curve analysis. cDNA standards were prepared as 10-fold serial dilutions of purified amplicon of each gene from 107 to 102 copies. 18S rRNA was used as an internal control and each reaction was set up in triplicate.
Primers for PCR were designed to have an annealing temperature from 55 to 60°C as following sequences: 18S rRNA: forward, 5′-AGTCCCTGCCCTTTGTACACA-3′; reverse, 5′-CGATCCGAGGGCCTCACTA-3′; ENA-78: forward, 5′-AGGCAATGCTGTCATCCTCTCTCT-3′; reverse, 5′-GGTTTCTGCATGACACAGCAGCTT-3′; IL-6: forward, 5′-TAAGCTGGAGTCACAGAAGGAGTG-3′; reverse, 5′-TAACGCACTAGGTTTGCCGAGTAG-3′; I-TAC: forward, 5′-AGATCCAAGCAAGCTCGCCTCATA-3′; reverse, 5′-TCAGGTTCCTGGCACAGAGTTCTT-3′.
Cytokine Assays
Interferon (IFN)-β content in BMDM supernatants was assessed using sandwich enzyme-linked immunosorbent assays. The mouse IFN-β ELISA kit was purchased from R&D Systems (Minneapolis, MN) and used according to the manufacturer’s instructions (sensitivity 15.6 pg/ml). MCP-1, KC, IL-6, IL-1β, IL-10, tumor necrosis factor (TNF)-α, and vascular endothelial growth factor contents were measured simultaneously using the Bio-Plex mouse cytokine assay kit (Bio-Rad Laboratories, Hercules, CA) using Luminex 100 (Luminex Corporation, Austin, TX). Each BMDM supernatant sample was performed in duplicates and 10-fold dilutions according to the manufacturer’s instructions. Standard curves for each cytokine were generated by using the reference cytokine standards supplied by the manufacturer. Raw data (mean fluorescent intensity) were analyzed by MasterPlex Quantitation Software v2.0 (MiraiBio, Inc., Alameda, CA) to obtain concentration values.
Statistical Analysis
Analysis was performed using GraphPad Prism (version 4.0; GraphPad, San Diego, CA). Bacterial loads and cytokine expression in the groups of congenic animals were compared using Student’s t-test. The differences between experimental groups were considered statistically significant at P < 0.05. Survival curves were plotted using GraphPad Prism (version 4.0), and compared using log-rank test.
Results
Specific Effect of the sst1 Locus on the Progression of Tuberculosis Infection in Genetically Resistant B6 Mice
To specifically evaluate the effect of the sst1 locus in a context of tuberculosis-resistant genetic background, we compared the course of infection in a standard inbred mouse strain C57BL/6J (B6) and the sst1-susceptible congenic strain, B6.C3H-sst1. The B6.C3H-sst1 strain is 99.5% genetically identical to the resistant B6 with the exception of a 12-cM interval on mouse chromosome 1 encompassing the sst1 susceptibility locus, which has been introgressed from the sst1 -susceptible C3HeB/FeJ mouse strain using marker-assisted backcross breeding.15
Within the first 2 weeks after a low-dose aerosol infection with virulent M. tuberculosis Erdman (25 to 50 CFU per mouse), we observed a similar rate of bacterial multiplication in both B6 and B6.C3H-sst1 mouse strains. The bacteria grew rapidly in the lungs with a doubling time of ∼30 hours (Figure 1A). Dissemination of the bacteria from the lungs to spleen and liver was similar in both strains and was observed at 2 weeks after infection, ie, approximately a week earlier as compared with mice of the C3H genetic background.20 These data indicate that the sst1 locus, although shown previously to mediate innate resistance to M. tuberculosis affects neither control of early multiplication of M. tuberculosis in the lungs, nor early hematogenous spread of bacteria from the lungs to other organs.
Figure 1.
Effect of the sst1 locus on the course of tuberculosis infection after low-dose aerosol challenge with M. tuberculosis Erdman. A: Kinetics of M. tuberculosis growth in organs of B6 and B6.C3H-sst1 congenic mice 2 to 8 weeks after aerosol infection with 15 to 30 CFU of M. tuberculosis; n = 4 males per group. B: M. tuberculosis loads in organs of B6 and B6.C3H-sst1 mice 5 months after aerosol infection with 35 to 50 CFU of M. tuberculosis, n = 4 females per group. C: Survival of the B6 and B6.C3H-sst1 strains after aerosol infection with 35 to 50 CFU of M. tuberculosis, n = 7 to 16 mice per group. D: Histopathology of tuberculous lung lesions in B6 (left) and B6.C3H-sst1 mice (middle and right) 5 months after aerosol infection with M. tuberculosis. Left and middle: H&E staining; right: trichrome staining (fibrotic capsule). Original magnifications, ×40.
Bacterial growth reached a plateau in both strains between the 2nd and the 4th weeks of infection, although in the B6.C3H-sst1 mice this plateau was established at an ∼10-fold higher level (Figure 1A). Between the 4th and the 8th weeks after infection, the bacterial burden in the lung, spleen, and liver decreased in both B6 and B6.C3H-sst1 strains, presumably because of activation of sst1-independent systemic mechanism(s) of anti-tuberculosis resistance. By the 8th week of infection the bacterial loads in the organs of the B6 and B6.C3H-sst1 mice reached their lowest levels. At this time tuberculosis inflammation in the lungs of the sst1-susceptible congenic mouse strain occupied larger areas as compared with the parental B6 mice. However, in both strains we observed interstitial inflammatory lesions with no signs of necrosis or neutrophil infiltration. Acid-fast bacilli were entirely intracellular and the majority of M. tuberculosis-infected macrophages of both strains contained no more than one to two bacteria per cell.
At 20 weeks after infection the sst1S congenic mice displayed clinical signs of illness (decreased movement, weight loss, ruffled fur), whereas the B6 mice appeared disease-free. At this point, the bacterial loads in the organs of the B6.C3H-sst1 mice were on average 10-fold higher, as compared with B6, with the highest bacterial burdens observed in the lungs of both strains (Figure 1B). There was a striking interstrain difference in lung pathology (Figure 1D): the lesions of the B6.C3H-sst1 mice contained large areas of necrosis separated from the surrounding lung tissue by prominent cell wall and fibrotic capsule (Figure 1D, middle and right). Using acid-fast fluorescent staining, we detected both extracellular M. tuberculosis inside the necrotic areas, as well as few intracellular acid-fast bacilli within macrophages in the granuloma wall surrounding the necrotic areas (not shown). At this time point we have frequently observed eruption of necrotic masses containing acid-fast bacteria in the airways. Most sst1S mice succumbed to the infection within 20 to 30 weeks after the low-dose aerosol challenge. Their survival was significantly reduced as compared with the sst1-resistant parental strain B6 (Figure 1C).
The sst1 Locus Determines Relapse Rate after Anti-Tuberculosis Chemotherapy
A similar effect of the sst1 locus on the pulmonary disease progression was observed after systemic infection. Previously we determined that time to death of the B6.C3H-sst1 mice infected intravenously with 5 × 104 CFU of M. tuberculosis was 122 days as compared with 226 days of B6 mice.15 Here we followed the disease progression after intravenous infection with the same dose of the bacteria and response to chemotherapy with INH. At 2 months after infection, the B6.C3H-sst1 mice started to develop clinical signs of illness and lose weight, whereas the B6 mice did not. The mortality of the B6.C3H-sst1 mice by the end of the 3rd month after infection was 45%, as compared with only 5% in the B6 mice (Figure 2, A and B). At that time the bacterial loads in organs of the B6.C3H-sst1 mice were 1.5 to 2 log10 higher than in B6 mice (Figure 2C; BT, before therapy). Microscopically extensive tissue damage in a form of large areas of necrosis containing numerous acid-fast bacilli was observed in the lungs of the B6.C3H-sst1 mice, whereas only moderate interstitial lesions without necrosis were found in the lungs of the B6 mice (Figure 2D; top and bottom left, respectively). Notably, no necrotic lesions were found in spleens and livers of either mouse strain at this or later times after infection (not shown). Thus, 3 months after systemic intravenous infection, we observed an advanced stage of pulmonary tuberculosis in the B6.C3H-sst1 mice and a chronic persistent infection in the B6 mice.
Figure 2.
Effect of sst1 locus on the course of tuberculosis after systemic intravenous challenge, INH treatment, and reactivation. A: Experimental protocol. C57BL/6J and B6.C3H-sst1 mice were infected intravenously with 5 × 104 CFU of M. tuberculosis Erdmann. Treatment with isoniazid (see Materials and Methods for details) was started 3 months after infection and administered orally for 90 days. B: Survival of the B6 and B6.C3H-sst1 mice after infection with M. tuberculosis and treatment with INH (n = 22 to 25 mice per group). Arrows indicate start and end of the INH treatment. C: Bacterial loads in lungs, spleens, and livers of B6 (circles) and B6.C3H-sst1 (squares) mice after infection with M. tuberculosis and treatment with INH (n = 3 to 5 mice per group). BT, before treatment; AT, 1 week after cessation of treatment; Re, reactivation 2 months after the INH withdrawal. D: Histopathology of the B6 (top) and B6.C3H-sst1 lungs (bottom) before treatment (BT, left) or 1 week after INH treatment (AT, right). H&E staining. E: Microanatomy of a tuberculous granuloma in the lungs of B6.C3H-sst1 mice after treatment with INH. Top left: H&E staining; top right: Trichrome staining (showing fibrotic capsule in blue); bottom: simultaneous immunostaining for iNOS and acid-fast fluorescent staining for mycobacteria; left: bright-field (iNOS labeled brown in macrophage cytoplasm); right: fluorescent M. tuberculosis in the same field. Original magnifications: ×40 (D); ×100 (E).
To study response to treatment and subsequent reactivation, the bactericidal anti-tuberculosis drug INH was administrated in drinking water (100 mg/L) uninterrupted for 3 months (Figure 2A). This regimen prevented further deaths in both groups of mice (Figure 2B), and all of the animals appeared healthy after completion of the 3 months course of INH therapy. One week after termination of the INH treatment, the bacterial loads were determined. In the resistant B6 mice the numbers of culturable M. tuberculosis decreased by 3 to 4 log10 and were below the threshold of detection in our assay, ie, less than 100 CFU per organ (with the exception of one liver sample, Figure 2C; AT, after therapy). Approximately 2 to 2.5 log10 decreases in the bacterial load were observed in lungs, spleens, and livers of the B6.C3H-sst1 mice. Nevertheless, M. tuberculosis bacilli were detectable in all sst1S animals tested (Figure 2C; AT).
Histopathology showed small areas of mild inflammation in the lungs of B6 mice (Figure 2D, top right), and no mycobacteria were found using acid-fast fluorescence staining. In contrast, after termination of the INH therapy the B6.C3H-sst1 mice had prominent tuberculous lung lesions seen as well-organized granulomas walled-off from normal lung tissue (Figure 2D, bottom right). The core region of the lung granulomas contained clusters of foamy macrophages (Figure 2E, top left) and, in some rare cases, residual necrotic tissue (Figure 2E, top right). The granuloma wall contained substantial zone of collagen fibers (trichrome staining, Figure 2E, top right), lymphocytes, and macrophages. The macrophages within the granuloma wall were activated as demonstrated by expression of iNOS (Figure 2E, bottom left). Acid-fast bacilli were confined to the core of the granulomas and could be found both extracellularly within necrotic debris and intracellularly inside the foamy macrophages (Figure 2E, bottom right). Thus, monotherapy with INH was successful in elimination of 99 to 99.9% of M. tuberculosis in the sst1S congenic mice. Ninety percent of the residual population of M. tuberculosis in the B6.C3H-sst1 was in the lungs, sequestered inside well-organized granulomatous lesions.
Two months after cessation of the INH treatment, the M. tuberculosis growth was observed in both the B6 and B6.C3H-sst1 mice (Figure 2C, Re). In the sst1-susceptible group this bacterial growth was observed primarily in the lungs, where the number of bacilli increased more than 10-fold (Figure 2C, Re). Remarkably no bacterial multiplication was observed in spleens and livers of the B6.C3H-sst1 mice during reactivation (Figure 2C, Re), demonstrating efficient control of M. tuberculosis in these organs. Nevertheless, the B6.C3H-sst1 mice succumbed to the infection within 3 months after INH withdrawal (Figure 2B). Microscopy revealed that reactivation of M. tuberculosis in sst1S mice was associated with expanding areas of necrosis within lung lesions (Figure 3A, left). The collagen capsule was destroyed, disorganized trichrome-positive fibers were found within inflammatory areas, and the bacteria spread throughout the lung tissue. In the spleens of these mice, the bacteria were intracellular and associated with clusters of macrophages, each infected macrophage containing one or few M. tuberculosis (Figure 3A, right).
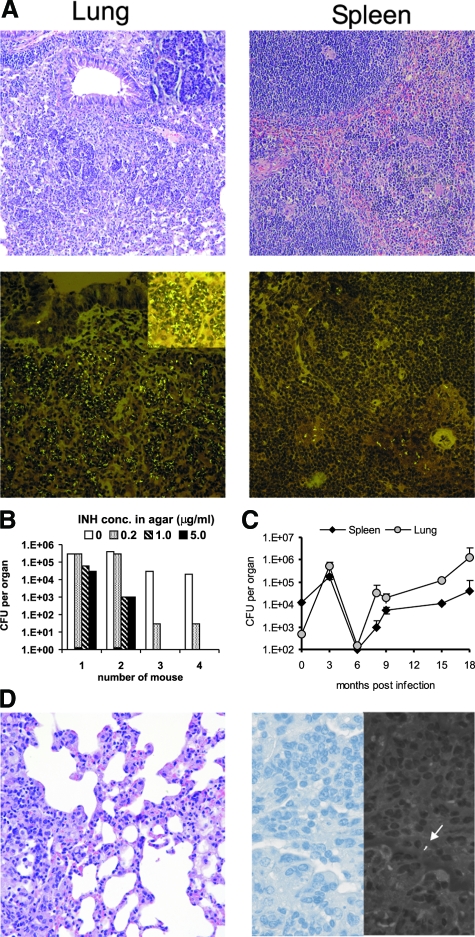
Figure 3.
Reactivation of tuberculosis infection after INH therapy. A: Histopathology of the lungs (left) and spleens (right) of B6.C3H-sst1 mice during relapse 2 months after the end of INH treatment. Top: H&E staining; bottom: acid-fast fluorescence staining for M. tuberculosis. B: Bacterial loads of M. tuberculosis and INH-resistant M. tuberculosis mutants in the lungs of B6.C3H-sst1 mice during relapse 2 months after the end of INH treatment; C: Course of tuberculosis infection in resistant B6 mice after intravenous challenge with M. tuberculosis and treatment with INH. D: Histopathology of the B6 lungs 9 months after the INH withdrawal. Left: H&E staining; right: acid-fast fluorescence staining for mycobacteria (corresponding light and fluorescent images of the same field), arrow: M. tuberculosis. Original magnifications: ×40 (D, left); × 100 (A); ×400 (A, inset; D, right).
We have determined that during reactivation the bacterial pools in the B6.C3H-sst1 lungs were represented by mixed populations of INH-sensitive and -resistant M. tuberculosis and observed marked heterogeneity in this respect between individual animals (Figure 3B). The great majority of M. tuberculosis isolated from the lungs of three of four B6.C3H-sst1 mice tested during relapse were sensitive to INH (Figure 3B). Nevertheless, reactivation and lung necrosis developed in all B6.C3H-sst1 mice, excluding appearance or selection of INH-resistant mutants as a major cause of reactivation in this model. However, greater proportion of INH-resistant mutants in the lungs of mice 1 and 2 was associated with ∼10-fold higher bacterial loads, as compared with animals 3 and 4. Interestingly, no INH-resistant mutants were found in spleens of the same animals (not shown). These findings indicated that lungs and spleens contained distinct bacterial populations, and that the lung necrotic lesions in the sst1S mice represented a favorable environment for emergence and survival of the drug-resistant mutants.
A different pattern of reactivation was observed in B6 mice. Two to three months after the INH treatment the bacterial burden in their lungs, spleens, and livers reached a plateau, which was approximately one log below the pretreatment level (Figure 3C). The bacterial burden remained at approximately the same level for the next 6 months, during which the B6 animals appeared healthy. Nine months after the INH withdrawal the inflammatory areas were prominent, but contained no necrotic areas. The lung lesions contained large proportion of lymphoid cells often organized in follicles. Acid-fast bacteria within these inflammatory areas were rare, localized inside macrophages, most of which contained single bacteria per cell (Figure 3D, right).
Thus, in the sst1-resistant B6 mice, the reappearance of culturable M. tuberculosis after INH treatment was observed in a context of well-controlled infection, during which a stable balance of host-pathogen interaction was maintained for at least a 9-month period. In contrast, in the presence of the sst1-susceptible allele, reactivation of progressive tuberculosis occurred within 2 months after termination of the INH treatment and was associated with the development of necrosis within the B6.C3H-sst1 tuberculosis lung lesions followed by rampant disease progression and death of the host. The disease-promoting effect of the sst1-susceptible allele was lung-specific and occurred at the bacterial levels that did not elicit necrosis in the sst1-resistant B6 mice even after prolonged periods of infection.
The Effect of the sst1 Locus in Vivo Is Modified by the Genetic Background of the Host
Although in principle the effect of the sst1-susceptible allele on progression of pulmonary tuberculosis in the B6.C3H-sst1 mice was similar to previously reported effect in the C3HeB/FeJ mice, we observed that time to death after either aerosol or intravenous infection with M. tuberculosis was significantly different between the sst1-susceptible C3HeB/FeJ and B6.C3H-sst1 mice. After intravenous infection with a standard dose of M. tuberculosis Erdman (5 × 104 CFU per mouse), the B6.C3H-sst1 mice survived for 9 to 12 weeks, whereas the C3HeB/FeJ succumbed within 3.5 to 5.5 weeks. A low-dose aerosol challenge with M. tuberculosis resulted in a median survival time (MST) in B6.C3H-sst1 and C3HeB/FeJ mice of 225 days and 153 days, respectively.
The genetic background also significantly influenced the histopathological type of progression of pulmonary tuberculosis in these sst1-susceptible hosts. In the more susceptible C3H genetic background tuberculosis infection proceeded via the development of pneumonia. By the 6th week after a low-dose aerosol challenge extensive inflammatory reaction with prominent exudation occupied large contiguous areas, which were not clearly separated from the rest of the lung. At that time initial formation of necrosis within the areas of pneumonia-like inflammation was observed (Figure 4A). Myeloid cells represented the majority of the inflammatory cells. A significant proportion of the myeloid cells contained large numbers of intracellular acid-fast mycobacteria.
Figure 4.
Tuberculosis progression in the lungs of the sst1-susceptible mice of the genetically resistant (B6) and susceptible (C3H) genetic backgrounds. Histopathology of tuberculosis lesions in the lungs of C3HeB/FeJ (A) and B6.C3H-sst1 (B) mice 6 (left) and 12 (right) weeks after aerosol infection with M. tuberculosis. H&E staining; acid-fast fluorescent staining for mycobacteria. Original magnifications: ×40 (H&E); ×100 (AFF).
Remarkably, the mice were able to survive through this stage of the disease and partially curb the spread of the pathogen: at 9 to 12 weeks after infection the inflammatory reaction decreased and the bacteria were mostly confined to lesions with large central necrotic areas which were separated from the normal tissue by fibrotic capsule. Acid-fast M. tuberculosis predominantly localized extracellularly within necrotic tissue debris, while some of the bacteria were intracellular inside macrophages that formed clusters within the cellular wall surrounding the necrotic lesions (Figure 4A, right).
In the lungs of the sst1-susceptible congenic mice on the resistant B6 genetic background, tuberculosis progressed more slowly, as a chronic infection with distinctly milder histopathology. At 6 weeks after infection, the pulmonary lesions were composed of patchy interstitial inflammation, without necrosis, and well separated from adjacent normal lung. The acid-fast bacteria localized intracellularly and the proportion of infected macrophages within the lesions was lower as compared with C3HeB/FeJ mice (Figure 4B, bottom left). Formation of necrosis within well-organized tuberculous lung lesions in some of the B6.C3H-sst1 mice was observed starting 9 to 12 weeks after infection. The necrotic lesions were separated from relatively intact lung tissue by massive cell wall (Figure 4B, top right). The wall was well structured: central area of necrosis was surrounded by a thick fibrotic capsule as confirmed by trichrome staining. The outer layer was composed of macrophages and lymphocytes. The lymphocytes were found both interspersed and closely associated with clusters of myeloid cells as well as in tight formations mostly composed of lymphoid cells (Figure 4B). The acid-fast M. tuberculosis was associated with central necrosis and rarely appeared within the outer layer (Figure 4B, bottom right).
To conclude, formation of necrosis within tuberculosis lung lesions is a specific phenotype associated with the susceptible allele of the sst1 locus. However, in the B6 background this phenotype is modified by other B6-derived genetic resistance factors, which slow the disease progression, increase time between infection and formation of necrosis, and strengthen local defenses limiting the spread of the pathogen from the necrotic core of the granuloma.
The sst1-Independent Genetic Control of Inflammation Is Mediated by Macrophages
Two studies have identified transcriptional responses of M. tuberculosis-infected macrophages characteristic of tuberculosis-susceptible genetic backgrounds. Macrophages isolated from several inbred mouse strains susceptible to tuberculosis expressed higher levels of mRNA encoding pro-inflammatory cytokines after infection with M. tuberculosis in vitro,21,22 which correlated with greater inflammation in the lungs of corresponding strains after infection with M. tuberculosis in vivo.23,24 To test whether the differences in disease pattern in our strain combination may also reflect differences in the macrophage production of proinflammatory mediators, we analyzed BMDMs isolated from B6 and C3HeB/FeJ mice after infection with M. tuberculosis in vitro. Indeed, the C3HeB/FeJ-susceptible macrophages produced significantly higher levels than B6 macrophages of the pro-inflammatory cytokines IL-1β, IL-6, and KC (not shown). However, no difference in production of these cytokines was observed between macrophages isolated from the sst1 congenic mouse strains C3HeB/FeJ and C3H.B6-sst1, indicating that their enhanced cytokine production (relative to B6) is controlled not by the sst1 locus, but by other unlinked genetic loci. To further investigate the sst1-independent effect of the genetic background on macrophage responses to M. tuberculosis, we compared cytokine expression profiles of BMDMs isolated from mouse strains that share sst1-susceptible alleles but differ in background (C3HeB/FeJ and B6.C3H-sst1) after infection with virulent M. tuberculosis. The M. tuberculosis-infected C3HeB/FeJ macrophages produced significantly more proinflammatory cytokines IL-1β, IL-6, KC, and MCP-1, whereas production of TNF-α, IL-10, and vascular endothelial growth factor was similar in macrophages of both genetic backgrounds (Table 1 and Figure 5A).
Table 1.
Multiplex Analysis (Luminex) of Cytokine Production in Supernatants of Bone Marrow-Derived Macrophages from C3H and B6.C3H-sst1 Mice 30 Hours after Infection with M. tuberculosis in Vitro (MOI 1:1)
| Mouse strain, cytokine | C3H | B6.C3H-sst1 | P value |
|---|---|---|---|
| IL-1β | 9311 ± 102* | 3120 ± 305 | 0.0007 |
| IL-6 | 24,573 ± 1402 | 2600 ± 129 | 0.0010 |
| KC | 51,578 ± 2091 | 4681 ± 553 | 0.0005 |
| MCP-1 | 4821 ± 524 | 160 ± 35 | 0.0031 |
| IL-10 | 708 ± 35 | 561 ± 101 | 0.0956 |
| TNF-α | 905 ± 64 | 896 ± 157 | 0.4735 |
| VEGF | 6939 ± 465 | 6964 ± 413 | 0.4799 |
Concentration of cytokines (pg/ml) ± SD.
Figure 5.
Differential production of inflammatory mediators by the C3HeB/FeJ and B6.C3H-sst1 BMDMs after infection with M. tuberculosis in vitro. A: Ratio of cytokine concentrations in supernatants of the C3HeB/FeJ and B6.C3H-sst1 BMDMs 30 hours after infection with M. tuberculosis Erdman, MOI 1:1. B: Kinetics of IFN-β production by the BMDMs after infection with M. tuberculosis Erdman, MOI 1:1. C: Kinetics of IL-6, ENA-78, and I-TAC mRNA expression by the BMDMs after infection with M. tuberculosis Erdman, MOI 1:1 (quantitative RT-PCR).
Using RT-PCR we studied the kinetics of gene expression of these and several other pro-inflammatory cytokines after the infection (Figure 5C). Similar to previous studies,22,24 we observed that macrophages from the tuberculosis-susceptible strain, C3HeB/FeJ, expressed 50- to 100-fold higher levels of ENA-78 and I-TAC as compared with the B6.C3H-sst1. These differentially expressed genes are known targets of type I IFNs. In the Listeria monocytogenes infection model transcriptional activation of IFN-responsive genes was associated with induction of IFN-β expression and production, which required cytoplasmic escape of the pathogen from phagocytic vacuoles.25,26 Importance of the type I IFN responses in pathogenesis of tuberculosis was also demonstrated.27,28,29 The ESX-1 secretion system, a major determinant of M. tuberculosis virulence, was shown to be required for the production of host type I IFNs during infection in vivo and in macrophages in vitro.29
We hypothesized that the sst1-independent difference between macrophages of the susceptible C3H and resistant B6 genetic backgrounds in response to M. tuberculosis infection was either because of differential production of type I IFNs or differential responsiveness to these cytokines. As shown in Figure 5B, after M. tuberculosis infection in vitro the levels of IFN-β produced by the susceptible C3HeB/FeJ macrophages was ∼10-fold higher as compared with more resistant B6.C3H-sst1. Taken together these data demonstrate that in addition to the sst1 locus other genetic factors are responsible for intrinsic control of how macrophages interact with virulent M. tuberculosis.
Discussion
Our studies illuminate mechanisms of multigenic control of tuberculosis susceptibility in immunocompetent hosts. First, we demonstrate a powerful and specific effect of the sst1 locus on the progression of pulmonary tuberculosis: control of necrosis within tuberculosis lung lesions. The same effect was observed after a low-dose aerosol infection, a standard systemic (intravenous) infection, as well as during relapse after incomplete eradication of M. tuberculosis by chemotherapy. Second, we show that, consistent with multigenic control of host resistance, the effect of the sst1 locus on tuberculosis progression is modified by other resistance loci. Specifically, a quantitative trait loci on chromosome 7 controls intracellular growth of M. tuberculosis systemically.16 Another quantitative trait loci on mouse chromosome 17 encompasses the H-2 locus and is most likely responsible for greater Th1 response to mycobacterial antigens in B6 background, which was associated with the H-2b haplotype of the mouse MHC complex in previous studies.12,13,30 The more pronounced lung inflammation observed in the C3H background is likely to reflect the greater production of pro-inflammatory cytokines by C3H macrophages infected with M. tuberculosis. This intrinsic macrophage phenotype is controlled in an sst1-independent manner by an as-yet unidentified locus (Figure 5). The B6-derived resistant alleles of those loci act in combination to reduce lung inflammation, delay necrosis formation, alter cellular composition, and increase stability of the necrotic lung granulomas. However, they could not prevent the formation of necrosis within granulomas, a process driven by the sst1S allele in B6.C3H-sst1 mice. The monogenic control of the development of necrosis within tuberculosis lung lesions by the sst1 demonstrates a unique nonredundant role of this locus in complex genetic architecture of tuberculosis susceptibility.
By convention, gene knockout or mutant alleles are transferred to or generated on the B6 genetic background to standardize effects of nonlinked genes on their phenotypic expression. Having generated the B6.C3H-sst1 congenic mouse strain by transfer of the C3HeB/FeJ-derived susceptible allele of the sst1 locus onto the standard B6 genetic background, we could directly compare specific effect of the sst1-susceptible allele (characterized by the lack of Ipr1 gene expression19) with the effects of other genes, implicated in host resistance to tuberculosis using knockout mice. Based on time to death after systemic intravenous infection performed using identical stock and a standard dose of M. tuberculosis Erdman in our laboratory, the B6.C3H-sst1 mice were significantly more resistant to M. tuberculosis than the IFN-γ, T-cell receptor, interleukin-12 p40, and inducible nitric oxide synthase (iNOS) knockout mice of the B6 background.14 The latter genes, along with TNF-α and TNF-α receptor, are essential components of anti-mycobacterial defense both in the mouse4,6 and human hosts.5 In the mouse inactivation of those essential genes resulted in fulminant disseminated tuberculosis infection characterized by extremely high bacterial loads and lack of the granuloma formation. In addition, the bacterial loads increased progressively in all organs without any preponderance of the lung, pointing toward a global failure of host resistance. Necrosis was usually observed in all organs of those mice at the terminal stage of infection, when the bacterial loads reached extremely high levels (108 to 109 CFU per organ). Both the bacteria and areas of necrosis were diffuse without clear separation from normal tissue. In contrast, the sst1-susceptible congenic B6 mice were capable of establishing initial control of the infection as evidenced by stabilization and even decrease in the bacterial counts after the 4th week of infection (Figure 1A). Their survival was comparable with moderately susceptible phenotypes observed in mutant mice, in which essential Th1 cell functions had been diminished, but not completely abrogated, as in genetic deletion of CD4, MHC class II or tbet.31,32 Inflammatory reactions in the lungs of all those mouse strains were considerably greater when compared with the wild-type B6 mice. However, only in the sst1-susceptible B6.C3H-sst1 mice was progression of inflammation associated with the appearance of central necrosis within well-organized granulomas.
We have previously demonstrated that lung necrosis in the sst1-susceptible mice could not be simply explained by extremely high bacterial burdens. In fact, formation of necrotic microfoci preceded the rampant multiplication of the bacteria in the lungs of the sst1-susceptible C3HeB/FeJ mice.18 In the present study of B6.C3H-sst1 mice, we have observed well-organized necrotic lesions in the lungs, which contained ∼107 CFU of M. tuberculosis (Figure 1, B and D). Notably, a bacterial burden of similar magnitude does not cause necrosis in the lungs of the sst1-resistant congenic mice of either C3H or B6 genetic backgrounds. To further address the relationship between the sst1-dependent necrotic phenotype and microbe burden, we used the bactericidal anti-tuberculosis drug INH to reduce the bacterial loads in the lungs of the B6.C3H-sst1 mice at a postnecrotic stage of the disease (Figure 2). After 3 months of the chemotherapy, the bacterial loads in the lungs of the B6.C3H-sst1 mice were reduced ∼1000-fold, and we observed considerable resorption of the necrotic masses. Two months after cessation of the INH therapy, necrotic foci reappeared within the residual lung lesions (Figure 3A), although the bacterial loads in the lungs at that time were at relatively low levels (Figure 2C). Remarkably, necrotic lesions developed specifically in the lungs of the B6.C3H-sst1 mice, whereas the bacterial loads were static and maintained at low levels in the spleens and livers. We determined that the relapse was not explained by selection of INH-resistant M. tuberculosis mutants, because the majority of the bacteria in the lungs of three of four animals tested during relapse were INH-sensitive (Figure 3B). However, the development and/or selection of the drug-resistant M. tuberculosis was indeed observed in the lung lesions of individual sst1-susceptible mice, in which greater proportion of resistant clones correlated with higher lung bacterial burdens and, most likely, more rapid relapse progression. Further analysis of population dynamics and mechanisms of drug tolerance and resistance in this model is necessary to better understand how variation in host resistance affects these processes.
In general, lung specificity of the sst1 effect on tuberculosis progression is puzzling because the sst1-dependent phenotype is clearly mediated by the bone marrow-derived cells.19 The sst1 locus was also implicated in innate resistance to another intracellular bacteria—Listeria monocytogenes.33 In that model, we have observed necrosis within hepatic inflammatory lesions. We hypothesize that the sst1-mediated function is not organ-specific per se, but it is critical at the sites of maximal inflammation and bacterial replication that are pathogen-specific. Thus, the observed lung predilection of the sst1 is not universal, rather it is specific for tuberculosis and, possibly, some other lung pathogens, which share certain elements of pathogenesis with M. tuberculosis.
In other mouse models the role of T cells, either as producers of IFN-γ,34 or as producers of Th2 cytokines,35 in granuloma necrosis was demonstrated. We also analyzed the kinetics of gene expression in tuberculosis lung lesions of the sst1 congenic mice and found no evidence that Th1/Th2 dysbalance was responsible for phenotypic expression of the sst1 locus in our model.18 Moreover, we have demonstrated that lung necrosis occurred in the sst1-susceptible scid mice even after adoptive transfer of mycobacteria-specific Th1 cells isolated from BCG-immunized sst1-resistant congenic mice.18 In addition, we have shown that inactivation of transcription factor tbet that controls Th1 differentiation, increases susceptibility of the resistant B6 mice to tuberculosis systemically, but does not cause necrosis of tuberculosis lung lesions.32 Combined our data pointed toward macrophage-mediated mechanism of the sst1 phenotype, although we found that this mechanism was iNOS-independent.18
The forward genetic analysis (from phenotype to gene), which we use as a major strategy in our studies, is a systematic, unbiased approach to identification of critical genetically encoded molecular mechanisms, either known or unknown. Using positional cloning we have identified a strong candidate gene within the sst1 locus, Ipr1.19 The full-length Ipr1 gene and the Ipr1-encoded protein are not expressed in the sst1-susceptible mice (H. Pan, in preparation). We found that overexpression of the full-length Ipr1 transgene in the sst1S macrophages increases their resistance to necrotic cell death induced by the virulent intracellular pathogens M. tuberculosis and Listeria monocytogenes in vitro. The Ipr1 is an IFN-inducible protein localized in macrophage nuclei, where it participates in formation of protein complexes in an IFN-inducible manner36 and associates with chromatin (Pan, in preparation). Because it has several protein interaction domains but no known functional domains, Ipr1 is likely an adaptor protein that plays a currently unrecognized role in macrophage responsiveness to type I and II IFNs, and, possibly, adaptation to harsh environments encountered by macrophages within inflammatory lesions. We used several independent genetic and functional criteria to identify the Ipr1 gene.19 However, additional 21 genes are present within the sst1 critical interval, as determined using genetic recombination. None of the other genes can be implicated in host resistance to tuberculosis based on their known sequence variation or inferred function. Nevertheless, it is possible that products of other sst1-encoded genes also participate in Ipr1-mediated pathway. Indeed, recent analysis identified blocks of functionally related genes in genomes of inbred mice.37
Further characterization of sst1-encoded molecular mechanisms may not only shed a light on a key aspect of tuberculosis pathogenesis, but also suggest therapeutic interventions to reduce lung pathology and transmission of the pathogen. In addition, parallels with human pulmonary tuberculosis in the B6.C3H-sst1 mouse strain offer advantages for evaluating anti-tuberculosis strategies. In this mouse model a major genetic factor affecting the disease progression is known and its mechanistic effect(s) on lung disease is increasingly understood. Hence, using a panel of mouse strains that include B6 and B6.C3H-sst1 could substantially improve preclinical testing of anti-tuberculosis vaccines, drugs, and other interventions. The efficacy of therapies could be assessed more accurately, and linked more precisely to specific defects of host resistance, anatomy of tuberculosis lesions, and clinical forms of the disease. Combined with advanced analytical and genetic engineering tools available exclusively for the mouse, this genetic mouse model of tuberculosis will have greater predictive power and help accelerate the development of anti-tuberculosis strategies effective in genetically heterogeneous host populations.
Acknowledgments
We thank Dr. Roderick Bronson for insightful discussions and Dr. Angele Nalbandian for technical advice.
Footnotes
Address reprint requests to Igor Kramnik, Departments of Immunology and Infectious Diseases, Harvard School of Public Health, 665 Huntington Ave., SPH-1, Boston, MA 02115. E-mail: ikramnik@hsph.harvard.edu.
Supported by the National Institutes of Health (grants HL59836 and AI49421 to I.K.).
Present address of B.-S.Y.: Institute of Microbiology and Immunology, National Yang-Ming University, Taipei City, Taiwan.
References
- Geneva: World Health Organization (WHO/ HTM/TB/2007.376),; Global Tuberculosis Control: surveillance, planning, financing. WHO Report. 2007 [Google Scholar]
- Via LE, Lin PL, Ray SM, Carrillo J, Allen SS, Eum SY, Taylor K, Klein E, Manjunatha U, Gonzales J, Lee EG, Park SK, Raleigh JA, Cho SN, McMurray DN, Flynn JL, Barry CE., III Tuberculous granulomas are hypoxic in guinea pigs, rabbits, and nonhuman primates. Infect Immun. 2008;76:2333–2340. doi: 10.1128/IAI.01515-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai MC, Chakravarty S, Zhu G, Xu J, Tanaka K, Koch C, Tufariello J, Flynn J, Chan J. Characterization of the tuberculous granuloma in murine and human lungs: cellular composition and relative tissue oxygen tension. Cell Microbiol. 2006;8:218–232. doi: 10.1111/j.1462-5822.2005.00612.x. [DOI] [PubMed] [Google Scholar]
- Cooper AM, Flynn JL. The protective immune response to Mycobacterium tuberculosis. Curr Opin Immunol. 1995;7:512–516. doi: 10.1016/0952-7915(95)80096-4. [DOI] [PubMed] [Google Scholar]
- Fortin A, Abel L, Casanova JL, Gros P. Host genetics of mycobacterial diseases in mice and men: forward genetic studies of BCG-osis and tuberculosis. Annu Rev Genom Hum Genet. 2007;8:163–192. doi: 10.1146/annurev.genom.8.080706.092315. [DOI] [PubMed] [Google Scholar]
- North RJ, Jung YJ. Immunity to tuberculosis. Annu Rev Immunol. 2004;22:599–623. doi: 10.1146/annurev.immunol.22.012703.104635. [DOI] [PubMed] [Google Scholar]
- Aly S, Wagner K, Keller C, Malm S, Malzan A, Brandau S, Bange FC, Ehlers S. Oxygen status of lung granulomas in Mycobacterium tuberculosis-infected mice. J Pathol. 2006;210:298–305. doi: 10.1002/path.2055. [DOI] [PubMed] [Google Scholar]
- Kramnik I, Demant P, Bloom BB. Susceptibility to tuberculosis as a complex genetic trait: analysis using recombinant congenic strains of mice. Novartis Found Symp. 1998;217:120–132. doi: 10.1002/0470846526.ch9. [DOI] [PubMed] [Google Scholar]
- Kramnik I, Dietrich WF, Demant P, Bloom BR. Genetic control of resistance to experimental infection with virulent Mycobacterium tuberculosis. Proc Natl Acad Sci USA. 2000;97:8560–8565. doi: 10.1073/pnas.150227197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helke KL, Mankowski JL, Manabe YC. Animal models of cavitation in pulmonary tuberculosis. Tuberculosis (Edinb) 2006;86:337–348. doi: 10.1016/j.tube.2005.09.001. [DOI] [PubMed] [Google Scholar]
- Chackerian AA, Behar SM. Susceptibility to Mycobacterium tuberculosis: lessons from inbred strains of mice. Tuberculosis (Edinb) 2003;83:279–285. doi: 10.1016/s1472-9792(03)00017-9. [DOI] [PubMed] [Google Scholar]
- Kamath AB, Alt J, Debbabi H, Taylor C, Behar SM. The major histocompatibility complex haplotype affects T-cell recognition of mycobacterial antigens but not resistance to Mycobacterium tuberculosis in C3H mice. Infect Immun. 2004;72:6790–6798. doi: 10.1128/IAI.72.12.6790-6798.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamath AB, Behar SM. Anamnestic responses of mice following Mycobacterium tuberculosis infection. Infect Immun. 2005;73:6110–6118. doi: 10.1128/IAI.73.9.6110-6118.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramnik I. Genetic dissection of host resistance to Mycobacterium tuberculosis: the sst1 locus and the Ipr1 gene. Curr Top Microbiol Immunol. 2008;321:123–148. doi: 10.1007/978-3-540-75203-5_6. [DOI] [PubMed] [Google Scholar]
- Yan BS, Kirby A, Shebzukhov YV, Daly MJ, Kramnik I. Genetic architecture of tuberculosis resistance in a mouse model of infection. Genes Immun. 2006;7:201–210. doi: 10.1038/sj.gene.6364288. [DOI] [PubMed] [Google Scholar]
- Sissons J, Yan BS, Pichugin AV, Kirby A, Daly MJ, Kramnik I. Multigenic control of tuberculosis resistance: analysis of a QTL on mouse chromosome 7 and its synergism with sst1. Genes Immun. 2009;10:37–46. doi: 10.1038/gene.2008.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramnik I, Boyartchuk V. Immunity to intracellular pathogens as a complex genetic trait. Curr Opin Microbiol. 2002;5:111–117. doi: 10.1016/s1369-5274(02)00295-3. [DOI] [PubMed] [Google Scholar]
- Yan BS, Pichugin AV, Jobe O, Helming L, Eruslanov EB, Gutierrez-Pabello JA, Rojas M, Shebzukhov YV, Kobzik L, Kramnik I. Progression of pulmonary tuberculosis and efficiency of bacillus Calmette-Guerin vaccination are genetically controlled via a common sst1-mediated mechanism of innate immunity. J Immunol. 2007;179:6919–6932. doi: 10.4049/jimmunol.179.10.6919. [DOI] [PubMed] [Google Scholar]
- Pan H, Yan BS, Rojas M, Shebzukhov YV, Zhou H, Kobzik L, Higgins DE, Daly MJ, Bloom BR, Kramnik I. Ipr1 gene mediates innate immunity to tuberculosis. Nature. 2005;434:767–772. doi: 10.1038/nature03419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chackerian AA, Alt JM, Perera TV, Dascher CC, Behar SM. Dissemination of Mycobacterium tuberculosis is influenced by host factors and precedes the initiation of T-cell immunity. Infect Immun. 2002;70:4501–4509. doi: 10.1128/IAI.70.8.4501-4509.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller C, Lauber J, Blumenthal A, Buer J, Ehlers S. Resistance and susceptibility to tuberculosis analysed at the transcriptome level: lessons from mouse macrophages. Tuberculosis (Edinb) 2004;84:144–158. doi: 10.1016/j.tube.2003.12.003. [DOI] [PubMed] [Google Scholar]
- Orlova MO, Majorov KB, Lyadova IV, Eruslanov EB, M'Lan CE, Greenwood CM, Schurr E, Apt AS. Constitutive differences in gene expression profiles parallel genetic patterns of susceptibility to tuberculosis in mice. Infect Immun. 2006;74:3668–3672. doi: 10.1128/IAI.00196-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eruslanov EB, Lyadova IV, Kondratieva TK, Majorov KB, Scheglov IV, Orlova MO, Apt AS. Neutrophil responses to Mycobacterium tuberculosis infection in genetically susceptible and resistant mice. Infect Immun. 2005;73:1744–1753. doi: 10.1128/IAI.73.3.1744-1753.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller C, Hoffmann R, Lang R, Brandau S, Hermann C, Ehlers S. Genetically determined susceptibility to tuberculosis in mice causally involves accelerated and enhanced recruitment of granulocytes. Infect Immun. 2006;74:4295–4309. doi: 10.1128/IAI.00057-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCaffrey RL, Fawcett P, O'Riordan M, Lee KD, Havell EA, Brown PO, Portnoy DA. A specific gene expression program triggered by Gram-positive bacteria in the cytosol. Proc Natl Acad Sci USA. 2004;101:11386–11391. doi: 10.1073/pnas.0403215101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Riordan M, Yi CH, Gonzales R, Lee KD, Portnoy DA. Innate recognition of bacteria by a macrophage cytosolic surveillance pathway. Proc Natl Acad Sci USA. 2002;99:13861–13866. doi: 10.1073/pnas.202476699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manca C, Tsenova L, Bergtold A, Freeman S, Tovey M, Musser JM, Barry CE, III, Freedman VH, Kaplan G. Virulence of a Mycobacterium tuberculosis clinical isolate in mice is determined by failure to induce Th1 type immunity and is associated with induction of IFN-alpha /beta. Proc Natl Acad Sci USA. 2001;98:5752–5757. doi: 10.1073/pnas.091096998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ordway D, Henao-Tamayo M, Harton M, Palanisamy G, Troudt J, Shanley C, Basaraba RJ, Orme IM. The hypervirulent Mycobacterium tuberculosis strain HN878 induces a potent TH1 response followed by rapid down-regulation. J Immunol. 2007;179:522–531. doi: 10.4049/jimmunol.179.1.522. [DOI] [PubMed] [Google Scholar]
- Stanley SA, Johndrow JE, Manzanillo P, Cox JS. The type I IFN response to infection with Mycobacterium tuberculosis requires ESX-1-mediated secretion and contributes to pathogenesis. J Immunol. 2007;178:3143–3152. doi: 10.4049/jimmunol.178.5.3143. [DOI] [PubMed] [Google Scholar]
- Chackerian AA, Perera TV, Behar SM. Gamma interferon-producing CD4+ T lymphocytes in the lung correlate with resistance to infection with Mycobacterium tuberculosis. Infect Immun. 2001;69:2666–2674. doi: 10.1128/IAI.69.4.2666-2674.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caruso AM, Serbina N, Klein E, Triebold K, Bloom BR, Flynn JL. Mice deficient in CD4 T cells have only transiently diminished levels of IFN-gamma, yet succumb to tuberculosis. J Immunol. 1999;162:5407–5416. [PubMed] [Google Scholar]
- Sullivan BM, Jobe O, Lazarevic V, Vasquez K, Bronson R, Glimcher LH, Kramnik I. Increased susceptibility of mice lacking T-bet to infection with Mycobacterium tuberculosis correlates with increased IL-10 and decreased IFN-gamma production. J Immunol. 2005;175:4593–4602. doi: 10.4049/jimmunol.175.7.4593. [DOI] [PubMed] [Google Scholar]
- Boyartchuk V, Rojas M, Yan BS, Jobe O, Hurt N, Dorfman DM, Higgins DE, Dietrich WF, Kramnik I. The host resistance locus sst1 controls innate immunity to Listeria monocytogenes infection in immunodeficient mice. J Immunol. 2004;173:5112–5120. doi: 10.4049/jimmunol.173.8.5112. [DOI] [PubMed] [Google Scholar]
- Ehlers S, Benini J, Held HD, Roeck C, Alber G, Uhlig S. Alphabeta T cell receptor-positive cells and interferon-gamma, but not inducible nitric oxide synthase, are critical for granuloma necrosis in a mouse model of mycobacteria-induced pulmonary immunopathology. J Exp Med. 2001;194:1847–1859. doi: 10.1084/jem.194.12.1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rook GA, Hernandez-Pando R, Dheda K, Teng Seah G. IL-4 in tuberculosis: implications for vaccine design. Trends Immunol. 2004;25:483–488. doi: 10.1016/j.it.2004.06.005. [DOI] [PubMed] [Google Scholar]
- Pan H, Mostoslavsky G, Eruslanov E, Kotton DN, Kramnik I. Dual-promoter lentiviral system allows inducible expression of noxious proteins in macrophages. J Immunol Methods. 2008;329:31–44. doi: 10.1016/j.jim.2007.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petkov PM, Graber JH, Churchill GA, DiPetrillo K, King BL, Paigen K. Evidence of a large-scale functional organization of mammalian chromosomes. PLoS Biol. 2007;5:e127. doi: 10.1371/journal.pbio.0050127. author reply e128. [DOI] [PMC free article] [PubMed] [Google Scholar]