Abstract
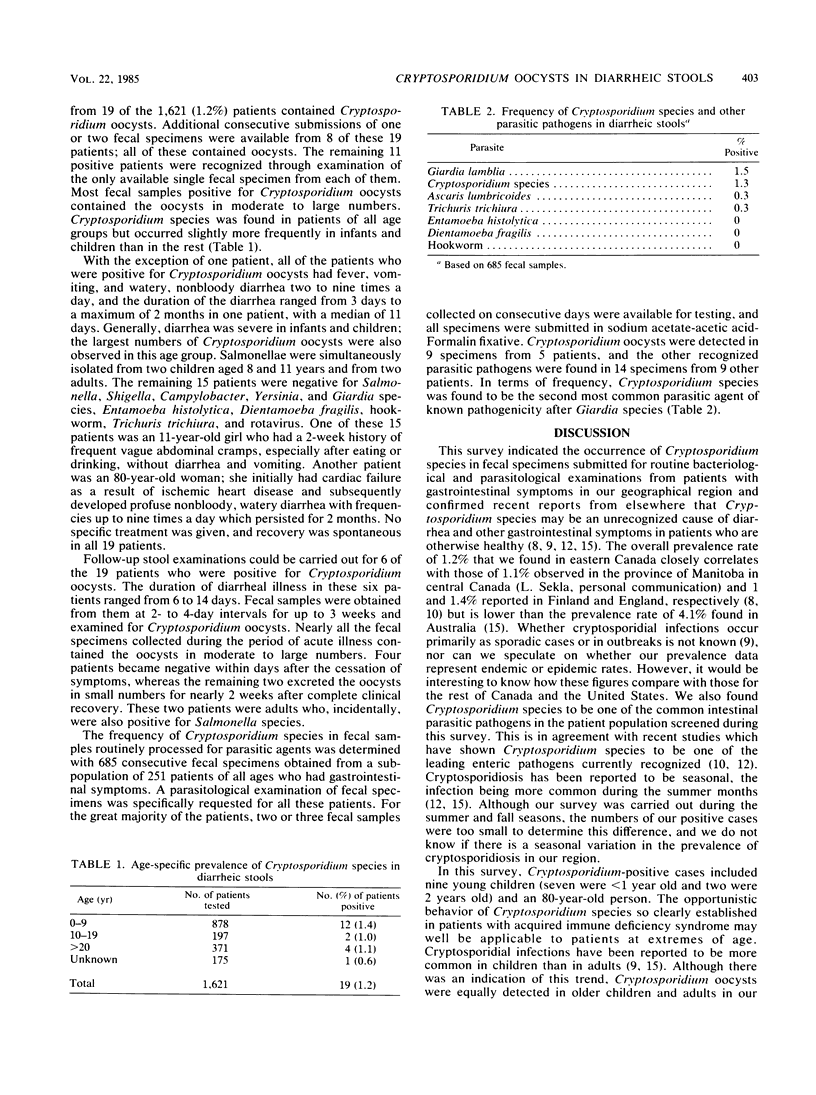
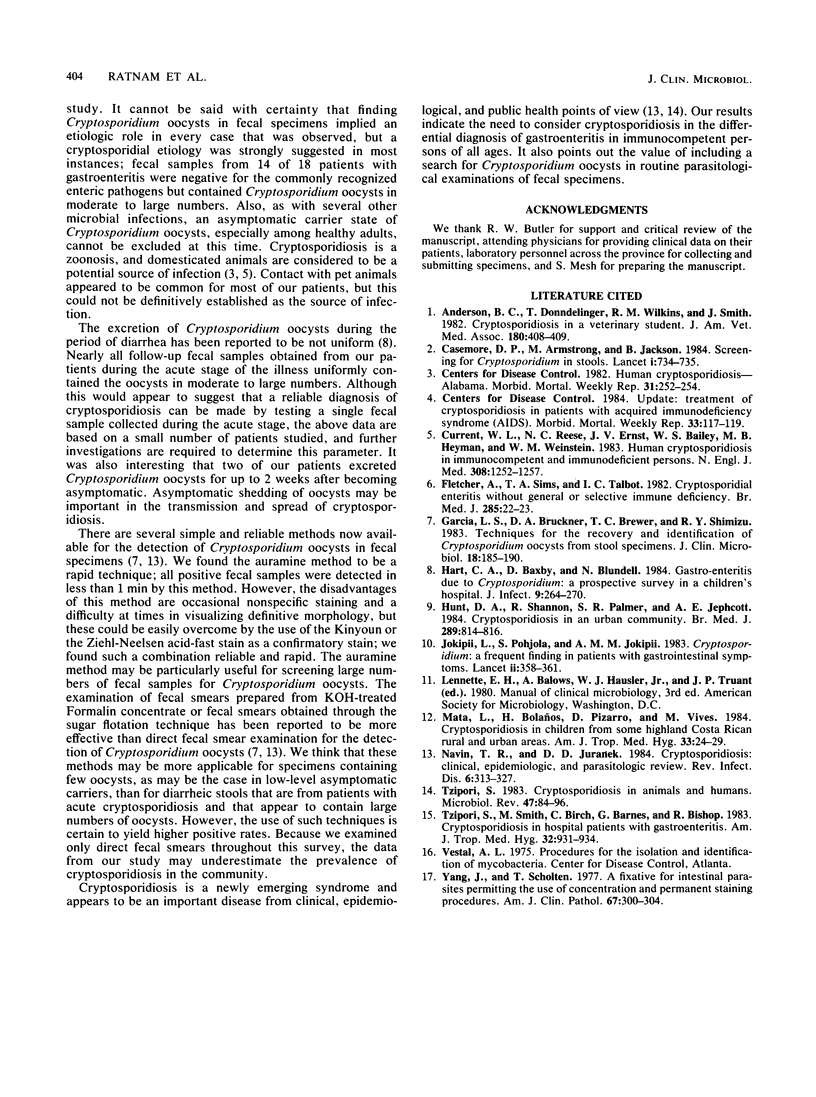
During a 7-month period, 2,252 fecal samples submitted for routine microbiological examination from 1,621 patients were screened for Cryptosporidium oocysts by the auramine staining method with Kinyoun acid-fast stain as the confirmatory stain. Cryptosporidium oocysts were detected in fecal samples from 19 (1.2%) patients, 18 of whom had gastroenteritis. Diarrheic stools from 14 of these 18 patients were negative for the usual enteropathogens but contained the oocysts in moderate to large numbers. Although Cryptosporidium oocysts were found in patients of all ages, they occurred slightly more frequently in infants and children than in the rest. Cryptosporidium species was one of the common enteropathogens identified in fecal samples submitted for routine parasitological examination during the period of the survey and was second only to Giardia species in terms of frequency. Considering cryptosporidiosis in the differential diagnosis of gastroenteritis in immunocompetent persons and including a search for Cryptosporidium oocysts in routine parasitological examinations of fecal samples appear warranted.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anderson B. C., Donndelinger T., Wilkins R. M., Smith J. Cryptosporidiosis in a veterinary student. J Am Vet Med Assoc. 1982 Feb 15;180(4):408–409. [PubMed] [Google Scholar]
- Current W. L., Reese N. C., Ernst J. V., Bailey W. S., Heyman M. B., Weinstein W. M. Human cryptosporidiosis in immunocompetent and immunodeficient persons. Studies of an outbreak and experimental transmission. N Engl J Med. 1983 May 26;308(21):1252–1257. doi: 10.1056/NEJM198305263082102. [DOI] [PubMed] [Google Scholar]
- Fletcher A., Sims T. A., Talbot I. C. Cryptosporidial enteritis without general or selective immune deficiency. Br Med J (Clin Res Ed) 1982 Jul 3;285(6334):22–23. doi: 10.1136/bmj.285.6334.22-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia L. S., Bruckner D. A., Brewer T. C., Shimizu R. Y. Techniques for the recovery and identification of Cryptosporidium oocysts from stool specimens. J Clin Microbiol. 1983 Jul;18(1):185–190. doi: 10.1128/jcm.18.1.185-190.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart C. A., Baxby D., Blundell N. Gastro-enteritis due to Cryptosporidium: a prospective survey in a children's hospital. J Infect. 1984 Nov;9(3):264–270. doi: 10.1016/s0163-4453(84)90574-7. [DOI] [PubMed] [Google Scholar]
- Hunt D. A., Shannon R., Palmer S. R., Jephcott A. E. Cryptosporidiosis in an urban community. Br Med J (Clin Res Ed) 1984 Sep 29;289(6448):814–816. doi: 10.1136/bmj.289.6448.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jokipii L., Pohjola S., Jokipii A. M. Cryptosporidium: a frequent finding in patients with gastrointestinal symptoms. Lancet. 1983 Aug 13;2(8346):358–361. doi: 10.1016/s0140-6736(83)90341-0. [DOI] [PubMed] [Google Scholar]
- Mata L., Bolaños H., Pizarro D., Vives M. Cryptosporidiosis in children from some highland Costa Rican rural and urban areas. Am J Trop Med Hyg. 1984 Jan;33(1):24–29. doi: 10.4269/ajtmh.1984.33.24. [DOI] [PubMed] [Google Scholar]
- Navin T. R., Juranek D. D. Cryptosporidiosis: clinical, epidemiologic, and parasitologic review. Rev Infect Dis. 1984 May-Jun;6(3):313–327. doi: 10.1093/clinids/6.3.313. [DOI] [PubMed] [Google Scholar]
- Tzipori S. Cryptosporidiosis in animals and humans. Microbiol Rev. 1983 Mar;47(1):84–96. doi: 10.1128/mr.47.1.84-96.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tzipori S., Smith M., Birch C., Barnes G., Bishop R. Cryptosporidiosis in hospital patients with gastroenteritis. Am J Trop Med Hyg. 1983 Sep;32(5):931–934. doi: 10.4269/ajtmh.1983.32.931. [DOI] [PubMed] [Google Scholar]
- Yang J., Scholten T. A fixative for intestinal parasites permitting the use of concentration and permanent staining procedures. Am J Clin Pathol. 1977 Mar;67(3):300–304. doi: 10.1093/ajcp/67.3.300. [DOI] [PubMed] [Google Scholar]


