Abstract
Choroidal neovascular membrane (CNVM) is one of the most common causes of submacular hemorrhage (SMH). Conventional treatment involves management of the SMH with pneumatic displacement with or without tissue plasminogen activator (TPA) followed by intravitreal injection of bevacizumab in a second sitting. We decided to assess the efficacy of treating SMH secondary to CNVM with pneumatic displacement using sulphur hexafluoride (SF6) gas and intravitreal bevacizumab. Four patients with SMH secondary to CNVM were included in this study. Intravitreal bevacizumab, 0.05 ml, along with 0.5 ml of SF6 was injected through the pars plana into the vitreous cavity. Postoperative best corrected visual acuity improved in all eyes with complete or partial displacement of SMH out of the foveal area.
Keywords: Bevacizumab, choroidal neovascular membrane, pneumatic displacement, submacular hemorrhage
Submacular hemorrhage (SMH) is a complication of a range of ocular pathologies like age-related macular-degeneration (AMD), trauma, myopia and retinal artery macroaneurysm.[1] Early removal of subretinal blood with treatment of the underlying cause allows for better visual recovery. However, clearing of the media may take some time, so we decided to combine intravitreal bevacizumab with pneumatic displacement of the hemorrhage, for early visual rehabilitation of patients with choroidal neovascular membrane (CNVM) and SMH.
We report our results of four cases of CNVM with SMH who were treated by combining intravitreal bevacizumab with pneumatic displacement of the hemorrhage using sulphur hexafluoride (SF6).
Case Reports
Case 1
A 65-year-old male patient presented to us with diminution of vision of one-day duration in the right eye. The best-corrected-visual-acuity (BCVA) in the right eye was 10/200. Slit-lamp evaluation and intraocular pressure (IOP) was normal. Fundus of the eye showed an SMH along with a large pigmentary epithelial detachment (PED) [Fig. 1]. Fluorescein angiography (FFA) showed blocked choroidal fluorescence. Leakage of the dye on indocyanine green angiography (ICG) and variable reflectivity on optical coherence tomography (OCT) suggested a subfoveal CNVM [Fig. 2]. Left eye was within normal limits.
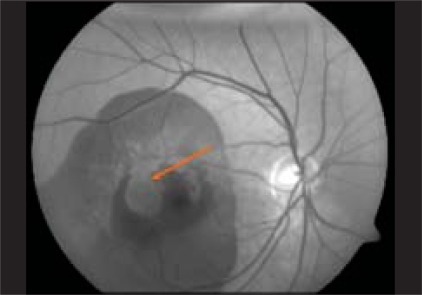
Figure 1.
Red free image of right eye showing submacular hemorrhage (blue arrow) along with pigmentary epithelial detachment (red arrow)
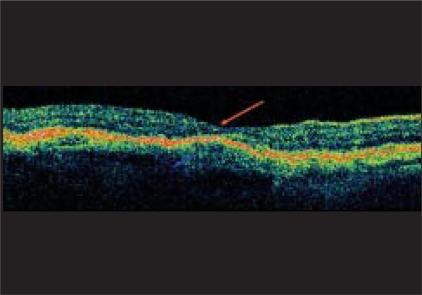
Figure 2.
Optical coherence tomography showing variable reflectivity of the retinal pigmentary epithelium (blue arrow) suggestive of choroidal neovascular membrane with subretinal blood and large pigmentary epithelial detachment (red arrow)
Case 2
A 62-year-old male presented with sudden diminution of vision in the right eye since one week. BCVA in the right eye was 3/200. Anterior segment was normal. Fundus examination revealed a subretinal hemorrhage in the macular area with serous detachment. Left eye fundus had evidence of dry AMD. OCT showed variable reflectivity of the retinal pigment epithelium (RPE) along with an increase in the retinal thickness suggestive of subfoveal CNVM with macular edema.
Case 3
A 35-year-old female presented to us with diminution of vision in the left eye since seven days. BCVA in the left eye was 3/200. Patient had undergone refractive surgery for myopia 10 years back. Left eye fundus showed a subretinal hemorrhage and OCT showed hyper-reflectivity in the RPE suggestive of CNVM. Fundus examination of the right eye was within normal limits.
Case 4
A 65-year-old female came to us with complaint of diminution of vision in the left eye since one week. Visual acuity in the left eye was 10/200. Anterior segment and IOP were within normal limits. Right eye had changes suggestive of AMD. Left eye fundus showed SMH along with chorio-retinal atrophy at the edge. FFA showed blocked fluorescence in the area of hemorrhage with late hyperfluorescence of the chorioretinal atrophy. A CNVM at the edge of chorioretinal atrophy was suspected.
All patients were given an intravitreal injection of 1.25 mg or 0.05 ml bevacizumab (one vial of bevacizumab contains 100 mg in 4 ml) along with pneumatic displacement of the SMH by 0.4-0.5 ml of SF6 [Micro SFR, Micromed S.r.l, Italy]. Intravitreal gas was injected using 30G needles (PriconR, ISCON Surgicals Ltd., Jodhpur, India). Patients were advised to maintain prone position for five to seven days. Two patients required a repeat intravitreal injection of bevacizumab. Results were noted at one week, one month and three months postoperatively.
The post-procedure results are summarized in Table 1.
Table 1.
Summary of results after pneumatic displacement and intravitreal bevacizumab
| Case No. | VA 1 week | VA 1 month | VA 3 months | Comments |
|---|---|---|---|---|
| 1. | 3/200 | 20/200 | 20/120 | Patient received repeat injection after two months of first injection |
| 2. | 20/200 | 20/40 | 20/40 | - |
| 3. | 20/200 | 20/80 | - | Patient was advised repeat injection but was lost to follow-up |
| 4. | 12/200 | 20/80 | 20/60 |
VA- Visual acuity
Discussion
CNVM is a common cause of SMH. Treatment, if delayed, leads to poor recovery due to the delay in diagnosis and treatment of the primary pathology as well as due to the harmful effect of persistent subretinal blood on photoreceptors.[1] Treatment options have included CNVM and hemorrhage removal with forceps, pneumatic displacement with/ without intravitreal tissue plasminogen activator (TPA), injection of subretinal TPA with displacement by perfluorocarbon liquid, injection of subretinal TPA followed by hemorrhage evacuation, vitrectomy with intravitreal/ subretinal injection of TPA with an intraocular gas bubble to help displace the hemorrhage inferiorly.[2]
Previously, pneumatic displacement was the treatment of choice in patients of SMH in CNVM, at our center. Subsequent management of the underlying pathology used to be done in a second sitting. With the widespread use of intravitreal bevacizumab in treatment of wet AMD, we decided to combine the two approaches for a faster visual recovery. Intravitreal injection of SF6 displaces the hemorrhage from the macular area, allowing for increase in visual acuity as well as better visualization of the primary pathology. India being a developing country with limited availability and high cost of TPA, bevacizumab seemed a good alternative. It helps in regression of the CNVM and also decreases the associated macular edema.[3] This resulted in a better definitive delineation of the primary pathology on subsequent FFA and OCT [Figs. 3 and 4].
Figure 3.
Red free image of the right eye showing clearing of submacular hemorrhage after intra-vitreal bevacizumab and SF6 injection (red arrow)
Figure 4.
Optical coherence tomography of the same patient showing normal reflectivity of the retinal pigmentary epithelium after the procedure with normal foveal contour (red arrow)
Gopalakrishan et al.,[4] have reported a series of 20 cases of SMH who were treated with pneumatic displacement out of which five had AMD. In these patients they concluded that pneumatic displacement without TPA had poor results. They suggested use of TPA with pneumatic displacement for such patients. In contrast, all the four cases in our series had good recovery of visual acuity.
This is an observation with very few patients but seems a promising technique in patients of AMD with SMH. Since earlier studies have had poor results with the other techniques available, more patients need to undergo this treatment for a better analysis of outcome.
References
- 1.Avery RL, Fekrat S, Hawkins BS, Bressler NM. Natural history of subfoveal subretinal hemorrhage in age-related macular degeneration. Retina. 1996;16:183–9. doi: 10.1097/00006982-199616030-00001. [DOI] [PubMed] [Google Scholar]
- 2.Thompson JT, Sjaarda RN. Vitrectomy for the treatment of submacular hemorrhages from macular degeneration: A comparison of submacular hemorrhage/membrane removal and submacular tissue plasminogen activator-assisted pneumatic displacement. Trans Am Ophthalmol Soc. 2005;103:98–107. [PMC free article] [PubMed] [Google Scholar]
- 3.Etet N, Krohne T, Holz FG. Essentials in ophthalmology. Berlin, Heidelberg, New York: Springer; Pharmacological approaches to age related macular degeneration; pp. 168–9. [Google Scholar]
- 4.Gopalakrishan M, Giridhar A, Bhat S, Saikumar SJ, Elias A, N S. Pneumatic displacement of submacular hemorrhage: Safety, efficacy, and patient selection. Retina. 2007;27:329–34. doi: 10.1097/01.iae.0000231544.43093.40. [DOI] [PubMed] [Google Scholar]