Abstract
Context
In contact lens-intolerant keratoconus patients, intrastromal placement of Intacs is becoming a promising new modality of treatment.
Aims
To study the safety and efficacy of implantation of microthin corneal inserts (Intacs) in Asian-Indian keratoconus patients.
Settings and Design
Retrospective interventional case series, in the cornea and refractive surgery service, at a tertiary care eye hospital in South India, between May 2006 and July 2007.
Materials and Methods
Intacs (Addition Technology, USA) were successfully implanted by mechanically creating tunnels, in 12 eyes of 12 keratoconus patients, who were contact lens-intolerant. The patients (mean age 25.58 years, nine male and three female) had a minimum follow-up of six months. Five patients had severe keratoconus (mean K > 53 D) and nine had central cones.
Results
All patients improved or retained visual acuity. The uncorrected visual acuity (UCVA) improved from a mean value of 0.06, (SD ± 0.08) to 0.19 postoperatively (SD± 0.15) (P= 0.01). The change in mean best corrected visual acuity (BCVA) was from 0.51, (SD ± 0.24), to 0.69, (SD ±0.00) (P = 0.01) postoperatively. The average central keratometry reading was 52.55 D. The change in mean K from 52.84 to 49.16 and 49.15 at one and six months respectively, was statistically significant. We did not have any major intra- or early postoperative complications. Eight of 12 eyes became contact lens-tolerant post-surgery.
Conclusion
The procedure of Intacs implantation appears to be safe and effective in a small group of Indian population at an intermediate follow-up.
Keywords: Intacs, intrastromal corneal ring, keratoconus
Keratoconus is a progressive, non-inflammatory, bilateral corneal dystrophy causing para-central thinning and ectasia leading to progressive severe astigmatism, visual distortion, light sensitivity and reduced best corrected visual acuity (BCVA). In the early stages of the disease, patients are fitted with spectacles or rigid gas-permeable contact lenses to improve the quality of vision.[1] In more severe disease, corneal transplantation may be commonly used, at which stage, in selected cases, the cornea may still be transparent.
Intacs, intracorneal microthin prescription inserts (Addition Technology Inc., USA) are currently approved in the United States by the US Food and Drug Administration (FDA) and in Europe by the European Commission for use in keratoconus. They have been reported to be an effective modality for the treatment of low to moderate degree of keratoconus, (mean K reading ≤53D) myopia or other ectatic conditions.[2,3]
Intacs were first used for the correction of low myopia.[3,4] and subsequently more information has become available regarding its other indications and biomechanical effects.[5,6]
Safety concerns have been raised in advanced keratoconus patients.[7] Preliminary studies indicate that Intacs seem to allow better quality of vision in patients with mild to moderate keratoconus, by permitting refitting of these patients with contact lenses, and may delay or eliminate the need for a corneal transplant procedure.[2]
Currently, to the best of our knowledge, there is no data on the usefulness of Intacs in Indian patients.
The purpose of this study was to report the six months safety and early efficacy data of Intacs implanted in Asian-Indian eyes.
Materials and Methods
A retrospective interventional study was conducted at our tertiary care eye institute in south India between May 2006 and July 2007. Approval of the institutional ethics committee (IEC) was obtained and the procedures followed were in accordance with the Indian council of medical research - good clinical practice (ICMR-GCP) guidelines and the Helsinki Declaration. All patients signed an informed consent.
Inclusion criteria were patients with confirmed keratoconus, with clear central corneas, aged 18 years or above. Patients with minimal corneal thickness of 450 µ at the implantation site were included. We did not consider central corneal thickness as a parameter for exclusion.
The patients were contact lens-intolerant with shortened wearing periods or had inability to achieve BCVA of 20/40 or better with contact lenses due to failure of contact lens fitting. Exclusion criteria were any previous corneal, refractive or intraocular surgery, diagnosed or suspected systemic autoimmune disease or herpetic keratitis.
All the patients underwent slit-lamp examination, Goldman applanation tonometry, videokeratoscopy by the Orbscan II (Bausch and Lomb, Salt Lake City), pachymetry (IOPAC, Heidelberg Engineering, Germany) and dilated fundus evaluation preoperatively. Preoperative measurements included uncorrected visual acuity (UCVA), BCVA, after subjective and objective refraction.
Treatment nomograms based on patients' preoperative spherical equivalent, the location of the cone, and asymmetric astigmatism induced by the keratoconus were used to determine the thickness of the appropriate Intacs placement for a particular patient.[8] The decision of asymmetrical placement of segments was according to the corneal topography. The thicker segment (0.45 mm) was placed corresponding to the steeper half of the keratoconus cone, predominantly inferiorly, to lift the cone and produce the maximum flattening effect, and the thinner segment was placed in the opposite half of the cornea to counterbalance the thicker segment and flatten the rest of the corneal surface.
The Intacs procedures were performed under topical anesthesia; the geometric center of the cornea was identified using an 11 mm zone marker, and the center was marked using a Sinskey hook. The ‘incision mark’ of the zone marker was aligned 1 mm from the limbus, on the steep meridian as shown by the Orbscan– thus the incision was made on the steep axis of the Orbscan. Intra-operative pachymetry was performed at the site of the incision. A 1.8-mm long radial incision was created at the incision site using a calibrated diamond knife with a 15° angled blade, set to approximately 70% of the pachymetry reading. The incision was sited 7 mm from the center of the optical zone. A small stromal pocket was dissected on both sides of the incision at full depth of incision, using the pocketing hooks. Symmetric glides were used to test the completed pockets.
The vacuum centering guide (VCG) was placed along with the procedure marker on the corneal surface. This semi-automated device contains a suction ring placed around the limbus guided by the previously marked center of the cornea. The KV 2000 vacuum system was started on the low setting of 450 mBar and increased to the high setting of 630 mBar if the VCG was in the proper position. When the desired level of vacuum was obtained, the clockwise (CW) and counterclockwise (CCW) corneal separators were used. These are two semicircular lamellar dissectors, placed sequentially in the lamellar pocket, and steadily advanced by a rotational movement. Thus two 180-degree semicircular dissections into the stroma were achieved with an approximate diameter of 7.5 mm. The VCG was removed, and the desired insert thickness was implanted in each tunnel. The radial incision was gently hydrated, and was closed with a 10-0 or 11-0 nylon suture with the knot buried. Topical antibiotic and corticosteroids were administered to the patient postoperatively.
The patients were examined on Days 1, 7 and at one month, three months and six months postoperatively. At each postoperative visit the patients underwent the following evaluations: intraocular pressure, pachymetry, slit-lamp examination of the anterior segment, UCVA and BCVA, keratometry and corneal topography. Primary safety measure was the number of eyes losing BCVA of more than two lines (Snellen chart). Secondary parameters included operative and postoperative complications (short and long-term), other adverse events such as conditions requiring explantation of the implant or gross refractive change for the worse. Short-term efficacy (six months) was measured by the number of eyes achieving BCVA between 20/20 and 20/40 and the number of eyes able to tolerate contact lenses post-procedure. For the purpose of this study BCVA was defined as the best visual acuity achieved with spectacles or contact lenses, as applicable.
Data tabulation and statistical analysis was performed on Microsoft excel worksheets. All the visual acuity data (UVCA and BCVA) were converted into decimal values for analysis. All the “P” values were calculated using the paired “T” test. A “P” value less than 0.05 was considered statistically significant.
Results
Intacs were successfully implanted in 12 eyes, of 12 patients, and all patients were included in the analysis after completion of six months of follow-up. The mean age of the patients was 25.58 years. There were nine male subjects and three female subjects. The preoperative characteristics of the patients are included in Table 1. Five of the patients had moderate to severe keratoconus (defined as K value >53 D), with clear corneas.
Table 1.
Preoperative characteristics of subjects
| Subject number | Sex/ Age (years) | Cone pattern | UCVA (Decimal) | BCVA (Decimal) | D Sph | D Cyl | MRSE | MEAN K | PACHY (μ) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F /23 | Inferior temporal | 0.02 | 0.17 | 1.00 | -8.00 | -3.00 | 46.6 | 491 |
| 2 | M /32 | Central | 0.01 | 0.67 | -1.00 | -6.00 | -4.00 | 51.95 | 362 |
| 3 | F /21 | Central | 0.02 | 0.50 | -16.50 | -2.00 | -17.5 | 58.75 | 377 |
| 4 | M /27 | Nasal temporal | 0.25 | 0.50 | -5.50 | -5.00 | -8.00 | 50.55 | 391 |
| 5 | M /33 | Central | 0.02 | 0.50 | -11.00 | -4.50 | -13.25 | 54.3 | 494 |
| 6 | F /23 | Central | 0.02 | 0.10 | -5.00 | -5.00 | -7.50 | 55.5 | 374 |
| 7 | M /25 | Central | 0.01 | 0.50 | -13.00 | -2.00 | -14.00 | 56.65 | 388 |
| 8 | M /25 | Central | 0.02 | 0.33 | -14.00 | -3.00 | -15.50 | 47.85 | 317 |
| 9 | M /29 | Nasal temporal | 0.01 | 0.50 | 3.50 | -7.00 | 0.00 | 56.2 | 337 |
| 10 | M /18 | Central | 0.01 | 1.00 | -6.00 | -4.50 | -8.25 | 50 | 434 |
| 11 | M /28 | Central | 0.17 | 0.67 | 0.00 | -5.00 | -2.50 | 52.8 | 396 |
| 12 | M /23 | Central | 0.17 | 0.67 | -2.00 | -6.00 | -5.00 | 52.9 | 444 |
| Mean value | 25.58 | 0.06 | 0.51 | -5.79 | -4.83 | -8.20 | 52.83 | 400.41 |
Sex: F= female, M= Male, Age: in completed years, UVCA= uncorrected visual acuity (Snellen), BCVA= best spectacle corrected Snellen visual acuity, D Sph= spherical power in diopters, D cyl= cylindrical power in diopters, K= keratometry value, Pachy= Central corneal thickness measured in microns
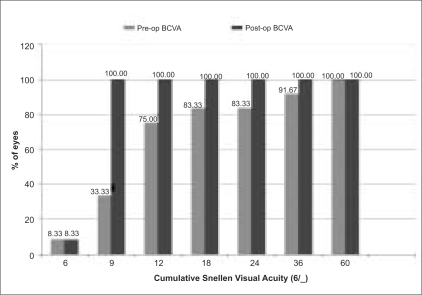
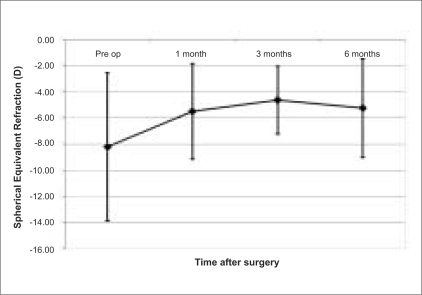
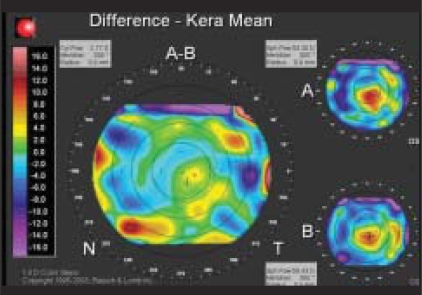
The UCVA changed from mean preoperative value of 0.06 (SD ± 0.08), to postoperatively 0.19 (SD ± 0.15) (P= 0.01). The change in mean BCVA was from 0.51 (SD ± 0.24) preoperatively, to 0.69 (SD ±0.10) (P = 0.01) postoperatively. Fig. 1 graphically depicts the change in BCVA from baseline to six months. The change in mean K from 52.84 at baseline to 49.16 and 49.15 at one and six months respectively, was statistically significant. The changes in visual acuity (UVCA and BCVA) and mean K along with their statistical significance are depicted in Table 2. Fig. 2 graphically represents the stability of refraction over time. Fig. 3 illustrates the pre and post-procedure changes in the Orbscan in one patient (Patient 10).
Figure 1.
The visual acuity graph compares the cumulative best corrected visual acuity at baseline and six months
Table 2.
Changes in pre- and postoperative refractive characteristics of subjects.
| UCVA Decimal | BCVA Decimal | D Sph | D Cyl | MRSE | Mean K | |
|---|---|---|---|---|---|---|
| Preop AVG ± SD | 0.06 ± 0.08 | 0.51 ± 0.24 | -5.79 ± 6.50 | -4.83 ± 1.84 | -8.21 ± 5.67 | 52.84 ± 3.67 |
| 1 month AVG ± SD | 0.19 ± 0.15 | 0.69 ± 0.10 | -3.77 ± 3.92 | -3.42 ± 1.44 | -5.48 ± 3.67 | 49.16 ± 3.77 |
| 3 months AVG ± SD | 0.20 ± 0.15 | 0.67 ± 0.08 | -2.94 ± 2.83 | -3.69± 1.54 | -1.43 ± 2.74 | 49.43 ± 3.86 |
| 6 months AVG ± SD | 0.19 ± 0.15 | 0.69 ± 0.10 | -3.56 ± 4.00 | -3.33 ± 1.47 | -5.23 ± 3.79 | 49.15 ± 3.93 |
AVG= Average (mean), SD= Standard deviation, UCVA= Uncorrected visual acuity, BCVA= Best corrected visual acuity
The difference in the mean decimal UCVA (P= 0.01), BCVA (P=0.01) and MEAN K (P<0.001) values at one and six months as compared to the preoperative baseline values were statistically significant (P< 0.05)
Figure 2.
Stability graph - showing spherical equivalent of manifest refraction plotted against time for the same cohort of patients followed through the postoperative period
Figure 3.
Difference mean of best fits sphere pre op (A) and post op (B) at six months, showing changes in the cone
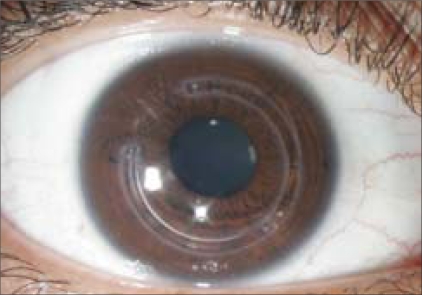
Eight of 12 eyes showed an improvement of atleast one line in BCVA. Two of these eyes showed improvement in vision equal to or more than three lines. Two eyes did not show any change in BCVA. All the eyes had postoperative BCVA of 20/30 or better (at one, and six months). None of the patients had postoperative UCVA of 20/40 or better. Eight of the 12 patients became contact lens-tolerant post surgery, which was fitted at three months in all these subjects. Mean anterior elevation, as determined by Orbscan on the anterior float was 0.0751 mm (SD± 0.0185) and at the end of six months it was 0.0415 mm (SD ± 0.0165). None of our patients lost BCVA of two or more lines (any vision) post implantation. Fig. 4 depicts high-magnification slit-lamp microphotographs of a patient to show Intacs in situ.
Figure 4.
High-magnification slit-lamp photograph of a patient to show Intacs in situ
No adverse events were noted intraoperatively in any of the subjects. In the early postoperative period, one eye (Patient 4) developed superficial corneal vascularization, directed towards the incision site, occurring at three weeks postoperatively before suture removal. The vascularization was self-limited and resolved after suture removal and with topical fluoromethalone eye drop therapy, and the visual recovery of the eye was unhampered. There were no features suggestive of an infection in this patient. In the late postoperative period, lamellar channel deposits occurred in three eyes (Patients 1, 4, 6) and channel haze was seen in two of these patients. The lamellar deposits increased by six months in all three eyes. All three eyes had 0.45 mm segment implant and this was seen in the thicker segment implant. Other early or late postoperative complications such as micro-perforation, infection, extrusion or implant migration were not observed. None of the patients required surgical removal of the implant due to any reason. One patient complained of ghost images, one patient complained of white band seen in lateral gaze and one patient developed mild photophobia. All these symptoms spontaneously resolved at the end of six months, without sequelae.
Discussion
The incidence and severity of keratoconus in Asian eyes may be high with an early onset and more rapid progress to the severe disease stage at a young age; frequently by the second decade.[9,10] Assiri et al.,[9] observed that this might reflect the influence of genetic and/or environmental factor(s) in the etiology of keratoconus. Also, keratoconus is the indication for corneal transplantation in about 7-10% of Indian subjects.[11] It is estimated that at the national level, we are able to procure only about 10% of required number of corneas (National Workshop on Corneal Blindness and Eye Banking, 2005). If Intacs are able to take care of a certain percentage of patients with advanced keratoconus, it will help reduce the burden of donor corneal requirement. We wanted to report the initial experience of safety and efficacy of Intacs in Indian eyes.
The standardized site for placement of implants is yet to be determined. We adhered to the nomogram for determining the thickness of the insert.[12] In our study, all segments were placed corresponding to the steep axis of the cone, on the steepest area, with inserts of different thickness being used only in the asymmetric cones, and similar thickness in central cones. We believe that this may be a good method of ensuring that the flattening occurs in the meridians that are the steepest.
None of our patients improved in UCVA, which has been suggested as a standard parameter for refractive surgeries.[13] However, the basic aim of Intacs is not to achieve potential vision with no correction. It is supposed to halt the progression of the disease and achieve flattening of the cone, thus improving the achievable vision with glasses or contact lenses. Also, contact lens tolerance is a major issue with keratoconus patients. Hence achieving contact lens tolerance would be a measure of its efficacy. Two-thirds of our patients became contact lens-tolerant after the procedure. Considering the fact that keratoconus is a complex refractive and mechanical challenge, the currently available standard reporting formats may be inadequate to demonstrate the benefits of Intacs for keratoconus.
Intacs implantation has been associated with non-sight-threatening and sight-threatening complications[7,12] in a small percentage of subjects in various series including: epithelial defects, anterior and posterior perforations during channel creation, extension of incision towards visual axis, uneven or shallow placement of implant, infectious keratitis, decentration, stromal thinning, segment exposure, and corneal melting. Thus at the end of six months, we did not have any serious adverse event. None of the eyes lost any lines of visual acuity. Suture removal had to be done earlier than usual in one of the patients because of superficial corneal vascularization. However, there was no evidence of infection in this patient. Thus the procedure appears to be safe in terms of vision for this small group of patients, at six months. The results from a long-term follow-up study have been encouraging.[14] In terms of quality, all the patients included in this study had bilateral keratoconus, except for two. The eye having the more severe keratoconus and inability to tolerate contact lens was chosen for Intacs implantation. The fellow eye was treated either with glasses or contact lenses. After Intacs implantation, one patient had complaints of ghost images binocularly, but with appropriate contact lens, the patient had satisfactory visual outcome. Lamellar channel deposits occurred in three eyes and channel haze was seen in two patients. However, these subjects had good visual outcome. All three eyes had 0.45 mm, thicker segment implant. Ruckhofer et al.,[15] report the frequency of intrastromal deposits at 74% after Intacs implantation. The authors noted that the presence of this material did not result in alteration of the optical performance of Intacs or anatomical or physiological corneal deterioration. In our patients also the lamellar deposits increased by six months in all three eyes.
Other authors have reported success mainly in mild keratoconus subjects (K value ≤53D),[16,17] with adoption of small variation in the placement of the Intacs rings.[17] We had a mixture of mild, moderate and advanced cases and found Intacs to be safe.
Studies have shown a loss of UCVA and BCVA in a small percentage of patients,[16,17] which were not noted in any of the patients in our study. This may be a possible unfavorable outcome if larger numbers are studied. However, the advantage of the Intacs insert technique is that it can be easily modified or reversed. We did not report the predictability component as we did not have target refraction before the procedure. Target refraction and predictability nomograms have not been developed for keratoconus. Presumably this will be a complex issue, again because of the above discussion.
The category of patients most likely to benefit from implantation of Intacs also needs to be defined. Recent reports demonstrate a better result in corneas with lower initial keratometric readings (K < 53 D) as opposed to higher (K >55 D).[12,16] Preoperative predictors of good outcome also include a better preoperative BCVA, lower astigmatism, and significant spherical myopia.[18] This study corroborates our experience, where although most of the patients showed improvement in BCVA, the eyes which achieved better outcomes had lower K readings preoperatively, along with a better preoperative BCVA. This may have an impact on patient selection criteria in the future. Limitations of our study include retrospective study design, small group of patients, mixed severity of keratoconus and lack of predictability data.
We conclude that Intacs as a procedure for keratoconus may hold a great promise in Asian-Indian patients. The procedure was safe in a small group of Asian-Indians. Larger studies are necessary to define the exact criteria for patient selection. Further studies on specific surgical methods need to be conducted for optimum use of resources in India.
Footnotes
Nil
None declared.
References
- 1.Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42:297–319. doi: 10.1016/s0039-6257(97)00119-7. [DOI] [PubMed] [Google Scholar]
- 2.Colin J, Cochener B, Savary G, Malet F. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg. 2000;26:1117–22. doi: 10.1016/s0886-3350(00)00451-x. [DOI] [PubMed] [Google Scholar]
- 3.Nosé W, Neves RA, Burris TE, Schanzlin DJ, Belfort Júnior R. Intrastromal corneal ring: 12-month sighted myopic eyes. J Refract Surg. 1996;12:20–28. doi: 10.3928/1081-597X-19960101-08. [DOI] [PubMed] [Google Scholar]
- 4.Schanzlin DJ, Asbell PA, Burris TE, Durrie DS. The intrastromal corneal ring segments: Phase II results for the correction of myopia. Ophthalmology. 1997;104:1067–78. doi: 10.1016/s0161-6420(97)30183-3. [DOI] [PubMed] [Google Scholar]
- 5.Burris TE, Ayer CT, Evensen DA, Davenport JM. Effects of intrastromal corneal ring size and thickness on corneal flattening in human eyes. Refract Corneal Surg. 1991;7:46–50. [PubMed] [Google Scholar]
- 6.Alió J, Salem T, Artola A, Osman A. Intracorneal rings to correct corneal ectasia after laser in situ keratomileusis. J Cataract Refract Surg. 2002;28:1568–74. doi: 10.1016/s0886-3350(01)01275-5. [DOI] [PubMed] [Google Scholar]
- 7.Kanellopoulos AJ, Pe LH, Perry HD, Donnenfeld Ed. Modified intracorneal ring segment implantations (INTACS) for the management of moderate to advanced keratoconus: Efficacy and complications. Cornea. 2006;25:29–33. doi: 10.1097/01.ico.0000167883.63266.60. [DOI] [PubMed] [Google Scholar]
- 8.Colin J. European clinical evaluation: use of Intacs in treatment of keratoconus. J Cataract Refract Surg. 2006;32:747–55. doi: 10.1016/j.jcrs.2006.01.064. [DOI] [PubMed] [Google Scholar]
- 9.Assiri AA, Yousuf BI, Quantock AJ, Murphy PJ. Incidence and severity of Keratoconus in Asir province, Saudi Arabia. Br J Ophthalmol. 2005;89:1403–6. doi: 10.1136/bjo.2005.074955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saini JS, Saroha V, Singh P, Sukhija JS, Jain AK. Keratoconus in Asian eyes at a tertiary eye care facility. Clin Exp Optom. 2004;87:97–101. doi: 10.1111/j.1444-0938.2004.tb03155.x. [DOI] [PubMed] [Google Scholar]
- 11.Rao SK, Sudhir RR, Fogla R, Rajagopal R, Sitalakshmi G, Padmanabhan P. Bilateral penetrating keratoplasty--indications, results and review of literature. Int Ophthalmol. 1999;23:161–6. doi: 10.1023/a:1010635231828. [DOI] [PubMed] [Google Scholar]
- 12.Ertan A, Colin J. Intracorneal rings for keratoconus and keratectasia. J Cataract Refract Surg. 2007;33:1303–14. doi: 10.1016/j.jcrs.2007.02.048. [DOI] [PubMed] [Google Scholar]
- 13.Koch D, Kohnen T, Obstbaum S, Rosen ES. Format for reporting refractive surgery data. J Cataract Refract Surg. 1998;24:285–7. doi: 10.1016/s0886-3350(98)80305-2. [DOI] [PubMed] [Google Scholar]
- 14.Kymionis GD, Siganos CS, Tsiklis NS, Anastasakis A, Yoo SH, Pallikaris AI, et al. Long-term follow-up of Intacs in keratoconus. Am J Ophthalmol. 2007;143:236–44. doi: 10.1016/j.ajo.2006.10.041. [DOI] [PubMed] [Google Scholar]
- 15.Ruckhofer J, Twa MD, Schanzlin DJ. Clinical characteristics of lamellar channel deposits after implantation of Intacs. J Cataract Refract Surg. 2000;26:1473–9. doi: 10.1016/s0886-3350(00)00575-7. [DOI] [PubMed] [Google Scholar]
- 16.Alio JL, Shabayek MH, Belda JI, Correas P, Feijoo ED. Analysis of results related to good and bad outcomes of Intacs implantation for keratoconus correction. J Cataract Refract Surg. 2006;32:756–61. doi: 10.1016/j.jcrs.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 17.Boxer Wachler BS, Christie JP, Chandra NS, Chou B, Korn T, Nepomuceno R. Intacs for keratoconus [errata p.1475] Ophthalmology. 2003;110:1031–40. doi: 10.1016/s0161-6420(03)00094-0. [DOI] [PubMed] [Google Scholar]
- 18.Levinger S, Pokroy R. Keratoconus managed with intacs: One-year results. Arch Ophthalmol. 2005;123:1308–14. doi: 10.1001/archopht.123.10.1308. [DOI] [PubMed] [Google Scholar]