Abstract
Chikungunya fever is a relatively rare from of vector-borne viral fever caused by chikungunya virus and spread by bites of the Aedes aegypti and Aedes albopictus mosquito. Epidemics of chikungunya fever have been reported in the past from different parts of the world. Although the virus had been passive for quite some time, recent reports of outbreaks of chikungunya fever in several parts of Southern India have confirmed the re-emergence of this virus. Symptoms of this infection include abrupt onset of fever, chills, and headache, rash, severe joint pain, conjunctival injection and photophobia. Ocular manifestations have been recently reported with this infection. We report a case of a 48-year-old female patient, who presented with defective vision two weeks after a serology proven chikungunya infection. There was bilateral neuroretinitis with peripapillary cotton wool spots. These findings should be kept in mind as an ocular manifestation of chikungunya virus infection.
Keywords: Chikungunya, neuroretinitis, ocular, optic neuritis, retinitis
Chikungunya is a relatively rare form of virus infection caused by an alpha virus that is spread by the bite of infected Aedes aegypti and Aedes albopictus mosquito. After a quiescent period of three decades this virus has made a comeback in the last couple of years. Recent reports of large-scale outbreaks from South India have confirmed the re-emergence of the virus. Ocular involvement in chikungunya virus infection was unheard of till the end of 2006. It was reported to cause photophobia and conjunctival injection along with the other systemic manifestations like fever, chills, joint pain, joint swelling, low back pain and skin and mucous membrane rashes.[1–3] Reports have started coming from the Indian subcontinent regarding the possible ocular manifestations of chikungunya virus infection.[4–8] Anterior uveitis, optic neuritis and retinitis associated with chikungunya fever have been reported in the past few months.[4,5,7,8] There is no mention about clinical features and characteristics of bilateral stellar neuroretinitis following chikungunya virus infection except in a series published recently.[7] We present a case of a 48-year-old female presenting with bilateral blurring of vision following a chikungunya virus infection. The clinical features and investigations suggest the diagnosis of bilateral chikungunya neuroretinitis. Clinical features and management of this rare but important public health problem are discussed.
Case Report
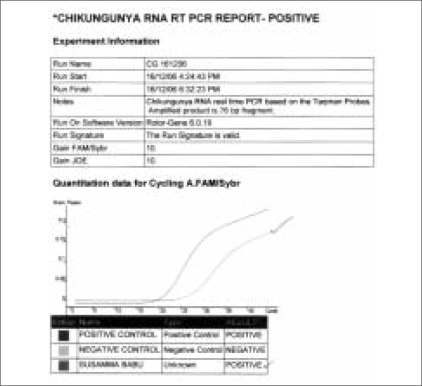
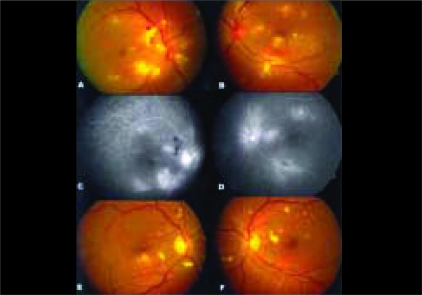
A 48-year-old female presented with diminution of vision in both eyes of one-week duration. She was admitted with fever, headache and arthralgia in the local hospital, two weeks prior to the onset of blurring of vision. She was investigated thoroughly and was diagnosed to be suffering from chikungunya fever. The investigations were as follows. Erythrocyte sedimentation rate 61 mm in 1 h (Westergren's method), hemoglobin: 12.5 gm%, total count: 14000 cells / cubic mm. Differential count showed polymorphs 62%, lymphocytes 28%, eosinophils 8% and basophils 2%. Platelet count was 1.8 lakhs / cubic mm. Random blood sugar was 240 mg%. Diabetic status was first detected when admitted with fever and antidiabetic medicines were started. Blood urea was 30 mg%, serum creatinine was: 0.8 mg/dL. SGOT was 42 U/L, SGPT was 67 U/L. ELISA test for HIV and VDRL test were negative. Chikungunya (Card) IgM ELISA test was positive. Polymerase chain reaction (PCR) test confirmed the presence of CHIKV infection. Chikungunya RNA real time PCR based on Taqman probes with an amplification product of 76 bp fragment was done. Fig. 1 shows the real time Chikungunya virus (CHIKV) RNA PCR report. Both these were done from serum sample one week after the fever started. Lack of hemorrhagic manifestations, normal platelet count and absence of epidemic of dengue in the area were against a diagnosis of dengue fever. She was given symptomatic treatment, which included antipyretic analgesic tablets like paracetamol and diclofenac sodium. She was discharged once the fever subsided. After two weeks of the discharge from the hospital she complained of defective vision of both eyes and was referred to an ophthalmologist. On ophthalmic examination, her best-corrected visual acuity was 20/80 N18 in the right eye and 20/60 N6 in the left eye. Slit-lamp examination revealed no evidence of inflammation in the anterior chamber in both eyes. Intraocular pressure by applanation tonometry was 16 mmHg in both the eyes. There was no relative afferent pupillary defect and color vision testing using Ishihara's pseudoisochromatic chart was normal. Fundus examination by indirect ophthalmoscopy and slit-lamp biomicroscopy revealed few vitreous cells, optic disc edema, intra-retinal hemorrhages, peripapillary cotton wool spots and areas of retinitis with macular star in both eyes [Fig. 2A and B]. Visual field analysis by Humphrey field analyzer showed bilateral centrocaecal scotoma. Fluorescein angiography was characterized by leakage from disc margins and from peripapillary vessels and blocked fluorescence due to retinal hemorrhage. The area of retinitis showed staining in the late phase of the angiogram [Fig. 2C and D]. A diagnosis of bilateral neuroretinitis was made. Since there was no fever and optic nerve head involvement she was started on a course of systemic steroids. Tablet Prednisolone 1 mg / kg body weight was started and tapered over six weeks. Fasting blood sugar was 142 mg% on starting the steroid therapy and her diabetes mellitus was simultaneously controlled in consultation with a physician. At the end of two months the best-corrected visual acuity was 20/30, N6 in right eye and 20/20, N6 in the left eye. Fundus examination revealed bilateral resolution of disc edema with decrease in the retinal hemorrhages and cotton wool spots [Fig. 2E and F]. Repeat Humphrey visual field analysis showed improvement of scotomas seen.
Figure 1.
Real time PCR for CHIKV RNA using Taqman probe
Figure 2.
A and B: Color fundus photograph of right and left eye at presentation. C and D: Late films of fluorescein angiography of both eyes showing disc leakage. E and F: Six weeks after treatment showing reduction in optic disc edema and retinitis
Discussion
Chikungunya virus infection has recently been reported to cause different ocular manifestations like non-granulomatous anterior uveitis, episcleritis, panuveitis, granulomatous anterior uveitis, optic neuritis, sixth nerve palsy, retrobulbar neuritis, retinitis with vitritis, neuroretinitis, keratitis, central retinal artery occlusion, multifocal choroiditis, exudative retinal detachment and secondary glaucoma.[4–8] Bilateral neuroretinitis is described in viral infections caused by measles, influenza, Epstein-Barr virus, dengue virus[9] and Rift valley fever virus. This typically occurs subsequent to an acute viral systemic illness. In our case a typical picture of bilateral neuroretinitis was seen after two weeks of serology-proven chikungunya infection. It is not clear whether the neuroretinitis is immunologically mediated or due to the virus itself. Systemic acyclovir has been given in some patients with ocular manifestations in chikungunya fever without evidence.[7] As there was optic disc involvement in our case we feel systemic steroids were indicated. Delayed onset of the eye problem after the fever subsided and prompt response to steroids in our case points towards an immune-mediated underlying cause. Optic neuritis following CHIKV infection has been treated successfully with parenteral steroids.[4] There are recent reports which show the need to institute early treatment after the onset of optic disc involvement. Delay in the treatment could result in poor visual outcome.[4] In our case visual recovery had been very satisfactory probably because there was no delay in starting systemic steroids. Being a single case report this result cannot be generalized to draw a conclusion regarding the prognosis of chikungunya neuroretinitis. We may be able to get a better picture once larger case series are published. To conclude, chikungunya neuroretinitis should be kept as a differential diagnosis of any bilateral neuroretinitis. We feel that to better understand and manage the full spectrum of ocular disease caused by chikungunya infection, all patients who have suffered from chikungunya fever and have eye problem should be referred for detailed ophthalmologic evaluation.
Acknowledgments
Dr. Suseela. K.K. MS. St Gregorious Mission Hospital. Department of Ophthalmology, Parumala, Kerala.
References
- 1.Ravi V. Re-emergence of Chikungunya virus in India. Indian J Med Microbiol. 2006;24:83–4. doi: 10.4103/0255-0857.25175. [DOI] [PubMed] [Google Scholar]
- 2.Enserink M. Massive outbreak draws fresh attention to little known virus. Science. 2006;311:1085. doi: 10.1126/science.311.5764.1085a. [DOI] [PubMed] [Google Scholar]
- 3.Yours SL, Forster DJ, Rao NA. Systemic viral infection and their retinal and choroidal manifestations. Surv Ophthalmol. 1993;37:313–52. doi: 10.1016/0039-6257(93)90064-e. [DOI] [PubMed] [Google Scholar]
- 4.Mittal A, Mittal S, Bharati MJ, Ramakrishnan R, Saravanan S, Sathe PS. Optic neuritis associated with Chikungunya virus infection in South India. Arch Ophthalmol. 2007;125:1381–6. doi: 10.1001/archopht.125.10.1381. [DOI] [PubMed] [Google Scholar]
- 5.Lalitha P, Rathinam S, Banushree K, Maheshkumar S, Vijayakumar R, Sathe P. Ocular involvement associated with an epidemic outbreak of Chikungunya virus infection. Am J Ophthalmol. 2007;144:552–6. doi: 10.1016/j.ajo.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 6.Chanana B, Azad RV, Nair S. Bilateral macular choroiditis following Chikungunya virus infection. Eye. 2007;21:1020–1. doi: 10.1038/sj.eye.6702863. [DOI] [PubMed] [Google Scholar]
- 7.Mahendradas P, Ranganna SK, Shetty R, Balu R, Narayana KM, Babu RB, et al. Ocular manifestations associated with Chikungunya. Ophthalmology. 2008;115:287–91. doi: 10.1016/j.ophtha.2007.03.085. [DOI] [PubMed] [Google Scholar]
- 8.Mittal A, Mittal S, Bharathi JM, Ramakrishnan R, Sathe PS. Uveitis during outbreak of Chikungunya fever. Ophthalmology. 2007;114:1798. doi: 10.1016/j.ophtha.2007.03.045. [DOI] [PubMed] [Google Scholar]
- 9.de Amorim Garcia CA, Gomes AH, de Oliveira AG. Bilateral stellar neuroretinitis in a patient with dengue fever. Eye. 2006;20:1382–3. doi: 10.1038/sj.eye.6702219. [DOI] [PubMed] [Google Scholar]