Abstract
Crime and neighborhood disorder may negatively impact the health of urban residents. Neighborhoods with high levels of violent crime may also increase residents’ risk of experiencing violence. Most studies supporting the assertion that neighborhood disorder impacts mental health have used residents’ own ratings of their neighborhoods. The present study examines the relationships among block-group level crime, perceived neighborhood disorder, violence experienced in the neighborhood, and depression. The sample was comprised of current and former drug users (n=786) nested in 270 block groups within Baltimore, Maryland, USA. Using path analysis, we tested the hypothesis that neighborhood violent crime has a direct impact on experiences of violence. Also, we hypothesized that neighborhood violence had a direct and indirect impact on depressive symptoms. Results support a model in which violence is associated with psychological distress through perceptions of neighborhood disorder, and through experiences of violence. We conclude that community and structural level interventions are needed to decrease neighborhood crime and improve residents’ perception of their neighborhood.
Keywords: USA, neighborhood, violence, depression, crime, urban, inner-city, drug users
Introduction
Depression is a major health problem in itself and has been prospectively linked to cardiovascular disease and other serious morbidities (Glassman & Shapiro, 1998; Jiang, Krishnan, & O’Connor, 2002; MacMahon & Lip, 2002; Maddock & Pariante, 2001). In addition, depression is strongly patterned by socioeconomic status (Inaba et al., 2005; Kessler, 1979; McLeod & Kessler, 1990). Although the majority of studies focusing on correlates, consequences, and causes of depression have largely focused on individual, family, and social network factors, some researchers have evaluated the role of structural and contextual factors such as neighborhood.
Studies conducted in Canada, the United Kingdom, and the U.S. have examined how neighborhood problems, such as place of residence and exposure to violent crime, vacant housing, might contribute to mental health (Bogat et al., 2005; Dupere & Perkins, 2007; Fauth, Leventhal, & Brooks-Gunn, 2004; Goldsmith, Holzer III, & Manderscheid, 1998; Propper et al., 2005; Ross, 2000; Galea et al., 2007). Neighborhood conditions in these studies are usually viewed as chronic stressors, producing psychological distress (Avison & Turner, 1988; Matheson et al., 2006; Steptoe & Feldman, 2001). However, it is still unclear how these chronic stressors operate to produce psychological distress. Do these conditions impact individual perceptions of environment, leading to feelings of fear, anxiety, or hopelessness? Or, do violent neighborhoods impact psychological distress by increasing individual exposure to actual violence?
After screening 8,562 studies, Truong and Ma (2006) conducted a systematic review of 29 studies that examined the relationship between neighborhood factors and mental health. The authors included studies that assessed neighborhood factors through objective measures as well as subjective measures. Objective measures refer to empirical data collected at the group level, rather than from an individual, such as number of dwellings, unemployment rates, crime rates, and income levels. Subjective measures refer to self-reported data collected from individuals which assess perceptions, attitudes, and personal experiences within the neighborhood. The authors concluded that there was a consistent positive relationship between neighborhood characteristics and mental health. However, this association tended to be modest, especially after adjusting for individual level factors. This review indicates that both subjective and objectives measures of neighborhood factors are associated with mental health.
Researchers have demonstrated a consistent link between self-reported perceptions of one’s neighborhood, a subjective measure, and physical and mental health. In a sample of Caucasians and African Americans living Baltimore, MD, Gary, Stark, and LaVeist (2007) found that individuals who perceived that their neighborhood had more severe problems (e.g. physical, social, and criminal problems) were more likely to experience higher levels of stress and depression. Similarly, Latkin and Curry (2003) found that baseline perceptions of one’s neighborhood problems predicted higher rates of depression at a follow-up assessment in Baltimore, MD.
In an Australian sample, Ziersch and researchers (2005) evaluated the impact of a variety of perceived neighborhood characteristics including perceived safety, perception of the physical environment, neighborhood trust, neighborhood connections, and social capital on physical and mental health. These researchers found that perceived neighborhood safety was associated with physical health. In addition, mental health was related to perceived safety and neighborhood connections.
There is a growing body of literature assessing the impact of objective measures of neighborhood on health status. Research conducted among 4.5 million Swedes has shown associations between neighborhood level factors, including proportion of residents with low income and low social capital, and mental health hospitalizations and disorders (Lofors & Sundquist, 2007; Sundquist & Ahlen, 2006). Likewise, Silver and colleagues (2002) reported that neighborhood disadvantage and mobility were associated with higher rates of depression and substance abuse in a large community sample of U.S. residents.
Many researchers have posited that objective measures of neighborhood influence physical and mental health through mediating variables such as perceptions of one’s neighborhood. Cutrona and colleagues (2006) proposed three mechanisms by which neighborhood characteristics affect individual depression levels. These pathways include 1) level of daily stress imposed by lack of resources, physical stressors, and other people; 2) heightened vulnerability to experiencing negative events; and 3) disruption of social networks.
Through multi-level analyses, Matheson et al (2006) studied the role of neighborhood stress, operationalized as residential mobility and material deprivation, on depression among Canadian residents. They found that after controlling for individual characteristics, there was a significant association between neighborhood stress and depression. In a study conducted in Michigan U.S., Kruger and researchers (2007) found that the relationship between physical deterioration of neighborhood and depression was mediated by social contact with neighbors, social capital, and perceptions of crime.
Wen and colleagues (2006) evaluated the relationships between objective and perceived neighborhood characteristics, psychosocial variables, and self-rated health in a sample of older adults in Illinois. They utilized neighborhood census data to construct an objective measure of neighborhood SES. Subjective assessment of neighborhood was measured as perceptions of physical, social, and service environment. Through a series of regression models, their findings indicated that objective measures of neighborhood affected self-reported health through perceptions of neighborhood and psychosocial factors including stress and depression.
Using structural equation modeling, Stiffman et al. (1999) examined the pathways between objective neighborhood conditions, perceived neighborhood conditions, environmental support, and mental health outcomes among adolescents living in inner-city areas of St. Louis. Although they found no direct impact of neighborhood conditions on mental health, they did find an indirect pathway through individual perceptions of neighborhood conditions.
Our previous research tested and confirmed a direct association between perceptions of neighborhood disorder and depression using the same SHIELD dataset that is reported on here (Latkin & Curry, 2003). Although the present study also considers the role of neighborhood perceptions on distress, we have expanded our model to assess the impact of an objective neighborhood measure (i.e., police crime report) and personal experiences of violence. The present study prospectively examined the pathways between an objective measure of neighborhood violence and depressive symptoms in a population of adults living in an inner-city environment. Unlike Stiffman et al (1999) and Wen et al (2006), who used census variables at a census tract level of aggregation, our measure of objective neighborhood conditions is comprised of police crime records, aggregated to a block group level. Research on violence in Baltimore has shown that the block group is an appropriate level of aggregation due to clustering of violent events and stressors (Harries, 1997).
While there is often a high degree of correlation between census variables such as median household income, and rates of violent crime, violent crime may be more proximal in the causal pathway that leads from neighborhood factors to mental health outcomes. Our choice of block groups versus census tracts was motivated by previous research that found that perceptions of neighborhood disorder, aggregated to a block group level, were a more reliable measure than perceptions of neighborhood disorder aggregated to a census tract level (Curry, 2004). In the present study, we employed correlation and path analysis to help answer the following questions:
To what extent does neighborhood violent crime, at the block group level, correlate with perceptions of neighborhood problems at the individual level among current and former drug users living in an inner-city environment?
Is neighborhood violent crime positively associated with individual experiences of violent crime?
Do perceptions of neighborhood problems mediate the relationship between neighborhood violent crime and level of depressive symptoms; or
Is there a direct impact of neighborhood violent crime on levels of depressive symptoms?
We hypothesized that higher levels of neighborhood violence would be directly associated with higher levels of depressive symptoms. Also, we posited that higher levels of neighborhood violence would be indirectly associated with higher levels of depressive symptoms, with perceptions of neighborhood crime and experiences of violence acting as intermediate variables.
Methods
Survey Assessment and Data Collection
The survey data used in this analysis were collected as a part of a social network-based HIV prevention intervention. Targeted outreach was used to recruit participants. Areas of high drug activity were assessed using focus groups, geocoding of drug related arrests over a 3-year period, and ethnographic observations. A description of the study and a telephone number to call was provided to potential participants. Those that contacted our research staff were given a brief screening to assess eligibility. Individuals who were eligible and agreed to participate were administered consent information and forms followed by a face-to-face interview on their socioeconomic background, HIV related behaviors, and their social networks.
Study inclusion criteria consisted of: 1) being at least 18 years old, 2) having daily or weekly contact with drug users through either drug-related or non-drug related interactions, 3) willingness to conduct AIDS outreach education, 4) willingness to recruit social network members into the study, and 5) not being enrolled in other HIV prevention or network studies. Prior to data collection, the Johns Hopkins School of Public Health Committee on Human Research reviewed and approved all study protocols.
The present study is a longitudinal study of former and current drug users. In this study, we analyze data collected from participants at two time points. Baseline data were collected from June 1997 through February 1999 and are referred to as Time 1 data. Time 2 data refer to data collected during the follow-up assessment which occurred three years (April 2000-June 2002) after baseline assessment, on average. In addition to the data collected from participants, geographic data, specifically police crime reports, were analyzed. These data were collected one year prior to baseline assessment (i.e. 1996) and are referred to as Time 0 data.
Measures
This study includes both individual-level measures and group-level measures (i.e. referred to as objective data throughout the remainder of this manuscript).
Block group neighborhood violence
Our objective measure of neighborhood disorder was crime data obtained from the Baltimore City Police Department. We used crime data for 1996 (referred to as Time 0), since most of the interviews were conducted in 1997-1998. Only Part One crimes were available, meaning that misdemeanor and drug related crimes such as drug possession or selling could not be included in the analysis. To calculate rates of violent crime in each block group, we geocoded the location of each crime using the address provided by the Baltimore City Police Department. We then aggregated by block group, and computed a rate per 1000 residents per year for each category of crime. Since the distributions of the rates of crime were highly skewed, we used a natural log transformation. We were interested only in violent or person-to-person crimes, and thus used 4 of the 8 categories of crimes available: assaults, murders, rapes, and robberies. Arson, larceny, burglary, and stolen vehicle crimes were not used in the analysis. To create an overall measure of violent crime, we summed the rates of the four violent crime categories. The Cronbach’s alpha for this scale was 0.79 (N = 385 block groups, in the full Baltimore dataset).
Perceived neighborhood disorder
Perceptions of neighborhood disorder were collected at baseline (Time 1) through an adapted survey based on Perkins and Taylor’s Block Environmental Inventory (Perkins, Meeks, & Taylor, 1992). The Perceptions of Neighborhood Disorder Scale (NPDS) consists of seven items measured on a three-point scale. Participants were asked about the following events on their block: vandalism, litter or trash in the streets, vacant housing, groups of teenagers hanging out on the street, burglary, people selling drugs, and people getting robbed on the street. Response options included “not a problem”, “somewhat of a problem”, or a “big problem.” The Cronbach’s alpha for this scale was 0.88. Among participants, the NPDS scores ranged from 0-14 with a mean score of 7.2 (sd=4.3).
Experiencing crime and violence
Participants’ experience with crime and violence in the past year was collected at follow-up assessment (Time 2). To measure this construct, we utilized a scale that was adapted from the My Exposure to Violence Scale, originally designed for children and adolescents, to capture exposure to violent events that occur in an inner-city environment (Selner-O’Hagan, Kindlon, Buka, Raudenbush, & Earls, 1998). Participants were asked to recall violent events that occurred in their neighborhoods. First, participants were asked if they had ever experienced nine events: 1) chased when you thought that you could really get hurt; 2) hit, slapped, punched, or beaten up; 3) attacked with a weapon, like a knife or bat; 4) shot; 5) shot at, but not actually wounded; 6) been in a serious accident where you or someone was hurt very badly, or someone else died; 7) sexually assaulted, molested, or raped; 8) threatened to seriously hurt you; 9) found a dead body. For each event that a participant had experienced, they were asked how many times they had experienced it, the last time they had experienced it, and if the event had occurred in their neighborhood.
To create a single measure of exposure to violence, we added the number of violent events experienced in the past year within the participant’s neighborhood (block group). To maintain validity, we did not include events that occurred outside of the participant’s neighborhood or events that occurred more than one year prior to the time of the survey. In this sample, experiencing violence scores ranged from 0-5 with a mean score of 0.2 (sd=0.6).
Depressive symptoms
Data on depressive symptoms were collected at follow-up (Time 2). Depression was assessed using the Centers for Epidemiological Studies Depression Scale (CES-D) (Radloff, 1977). The CES-D, which has high validity and reliability, is a 20-item, 4-point scale developed for use in the general population (Radloff & Locke, 1986). Also, this scale has been shown to have a high sensitivity for DSM-IV major depression, and to have adequate specificity as a screening instrument for depression (Zimmerman & Coryell, 1988). In this sample, the CES-D scores ranged from 0-58 with a mean score of 15.8 (sd=11.9).
Additional Covariates
In addition to the aforementioned constructs, several other variables that have been linked to depression, violence, and neighborhood characteristics were collected through the survey and used in the analyses. Sociodemographic variables include gender, education (<12 grade versus high school diploma or higher), employment (at least employed part-time versus unemployed), age, and having a main partner status (yes or no). Also, behaviors such as injected any drugs in the past 6 months (yes or no), number of hours per day spent on the street, and number of roles in the drug economy (i.e. selling drugs, preparing drugs, exchanging sex for money or drugs, etc.) were assessed since they may influence perceptions of one’s neighborhood as well as experience with violence. These data were collected during baseline assessments (Time 1).
Analyses
Geocoding
To calculate the rates of violent crime in each block group, the location of each crime was geocoded using the address provided by the Baltimore City Police Department. These data were then aggregated by block group, and computed a rate per 1000 residents per year for each category of crime. Since the distributions of the rates of crime were highly skewed, a natural log transformation was applied.
Our sample (n=786) resided in 270 of the 385 Baltimore City block groups. Of the 270 represented block groups, 175 block groups had 1 or 2 participants, and 95 block groups had 3 or more participants.
Correlation Analysis
To examine the bivariate relationships among block group level violent crime, participants’ experience with violent crime, perceptions of neighborhood disorder, and level of depressive symptoms, we used Spearman Correlation Coefficients since the violent crime variable was highly left skewed. For comparison, however, we present both Pearson and Spearman coefficients.
Path Model
To test the hypothesis that neighborhood rates of crime impacted CES-D scores directly and indirectly though perceptions of neighborhood problems, we estimated a path model using Mplus (Muthen & Muthen, Los Angeles, CA, 2002). We chose this strategy because it allowed us to simultaneously assess perceptions of neighborhood disorder and experiences of violence as outcomes of neighborhood level violence, and as predictors of depressive symptoms. A series of ordinary regression models would not allow simultaneous estimation of coefficients. The path analysis method was also preferred over a structural equation approach, since our primary interest was in the pathways between neighborhood violence and level of depressive symptoms, and not in the measurement models. We present standardized path coefficients (standardized to 0 mean, unit variance) to facilitate comparisons among the coefficients.
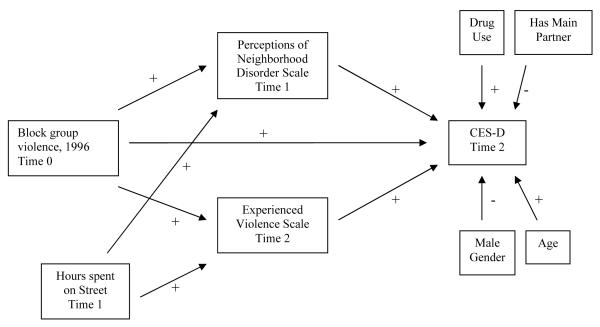
We tested a model in which objective neighborhood violence impacted depression through perceptions of neighborhood disorder. In the initial path model (see Figure 1), the level of neighborhood block group crime impacted both perceptions of neighborhood level of disorder and level of depressive symptoms. The level of neighborhood crime also impacted experiences of violence in the neighborhood, which in turn impacted level of depressive symptoms. Other factors (gender, age, injection drug use status, main partner status, and number of hours per day spent on the street) were hypothesized to impact level of depressive symptoms, while the amount of time spent on the street was hypothesized to impact both experiencing violence and perceptions of neighborhood disorder.
Figure 1.
Initial Path Model of Effects of Block Group Level Violence on Psychological Distress Among Sample of Current and Former Drug Users in Baltimore, Maryland
*All exogenous variables are specified as correlated, curved arrows not shown.
We used a Weighted Least Squares Minimum Variance estimation method to compute path coefficients, since our model included several categorical variables. All coefficients are standardized to allow direct comparisons. For model fit evaluation, we used a Chi-Square Test of Model Fit and evaluated the Root Mean Square Error of Approximation. As rules of thumb, the RMSEA should be below .05 and the Chi-Square statistic should be non-significant (p>0.05).
Results
Sample Characteristics
Data were collected from 786 participants who were nested in 270 residential block groups. The sample was predominantly comprised of males (61.2%). The mean age was 39.0 (sd= 7.3). The sample is highly disadvantaged, relative to the general population. Only 22% of the sample was employed at least part-time at the time of the initial interview, and only 52% had completed at least a high school education. Sixty-four percent of participants reported having a main sexual partner. Approximately 57% reported injecting drugs in the previous six months while 36% reported having at least one role in the street drug economy. In addition, 14% of participants experienced at least one violent event in their neighborhood in the past year, and the average study participant spent 6 hours per day on the street.
Block Group Data
Descriptive statistics for the Block Groups are presented in Table 1. The average population size of each group was 878.4 (sd=401.6). A mean of 2.8 (sd=3.2) SHIELD participants were represented in each block group. Regarding crime levels, the two highest rates were robbery (mean=32.7 per 1000, sd=59.2) and assault (mean=28.3 per 1000, sd=29.5).
Table 1.
Descriptive statistics for Block Groups (N=270) in Baltimore, MD*
| Block Group Characteristics | Percent | |||
|---|---|---|---|---|
| Percent Completed High School | 59.3 | |||
| Mean | Minimum | Maximum | STD | |
| Total Population per Block Group, 2000 Census |
878.4 | 139 | 2455 | 401.6 |
| SHIELD Participants per Block Group | 5.4 | 1 | 78 | 7.1 |
| Rate of Assault per 1000 residents, 1996 |
28.3 | 0 | 308.1 | 29.5 |
| Rate of Murders per 1000 residents, 1996 |
0.9 | 0 | 13.0 | 1.7 |
| Rate of Rape per 1000 residents, 1996 | 2.1 | 0 | 46.5 | 3.6 |
| Rate of Robbery per 1000 residents, 1996 |
32.7 | 0 | 875.0 | 59.2 |
The sample of 786 participants resided in 270 block groups.
Correlation Analyses
The variable measuring neighborhood violent crime was modestly, but significantly correlated with the Perceptions of Neighborhood Disorder Scale (PNDS) (Rho = 0.19) and with the experiences of violence scale (Rho = 0.09), but not with level of depressive symptoms (see Table 2). The PNDS was not correlated with experiences of violence in the neighborhood. However, there was a modestly significant association with level of depressive symptoms (Rho = 0.13). Finally, the experiencing violence scale was marginally correlated with level of depressive symptoms (Rho = 0.11).
Table 2.
Spearman and Pearson correlation coefficients among actual level of violent crime, perceptions of neighborhood disorder, experiences of violence, and depressive symptoms, SHIELD Study, N=786
| Spearman Coefficients (Pearson Coefficients) |
|||
|---|---|---|---|
| Variable | Actual Level of Violent Crime |
Perceptions of Neighborhood Disorder |
Experiences of Violence in Neighborhood |
| Perceptions of Neighborhood Disorder |
|||
| 0.19 (0.19)*** | |||
| Experiences of Violence in Neighborhood |
|||
| 0.09 (0.07)* | 0.02 (0.03) | ||
| Depressive Symptoms (CES-D score) |
|||
| 0.03 (0.03) | 0.13 (0.14)*** | 0.11 (0.12)** | |
p<.05
p<.01
p<.001
Path Analyses
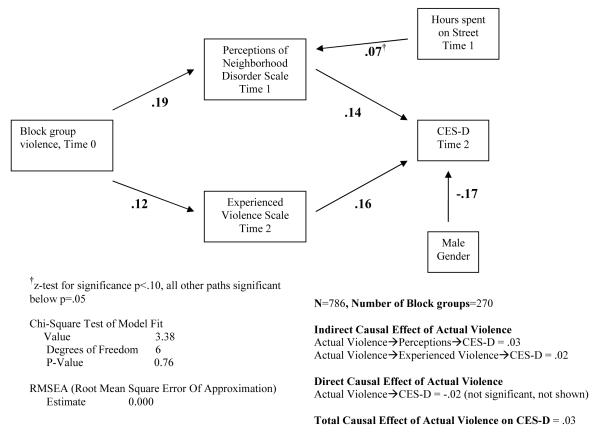
The path model that was initially tested did not adequately fit the data, as indicated by both the Chi-Square Test of Model Fit and the RMSEA (Chi-Square test significant p=.01, and RMSEA > 0.05). There were several path coefficients that were not statistically significant (z-score test). First, the direct path between neighborhood block group violence and CES-D score was not significant, in contrast to our initial hypothesis. We removed this path from the model. Stiffman et al. (1999) observed a similar result: their measure of actual neighborhood conditions did not directly impact on the mental health status of the adolescents in their study. Second, time spent on the street did not appear to impact experiences of violence in the neighborhood, and thus this path was removed from the model. Finally, age, drug use status, and main partner status were not significantly associated with level of CES-D, and were removed from the model. Only gender remained a significant predictor, with males having lower CES-D scores than females.
The final model included two indirect paths by which level of violent block group level crime was associated with CES-D: through perceptions of neighborhood disorder and through experiences of violence in the neighborhood. The total indirect effect of neighborhood level of violent crime (using standardized coefficients) was .05. The direct effect of neighborhood violent crime was -.02, but was not significant. Thus, the total effect of actual violence on CES-D was .03. For the NPDS, the R2 (variance explained) was .04; for the experiences of violence in the neighborhood, the R2 was .02, and for CES-D score, the R2 was .07. The final model, although different from the initial model, provided support for the hypothesis that neighborhood violence was associated with depressive symptoms through perceptions of neighborhood and experiences of violence.
Discussion
The findings from this current study suggest that neighborhood crime is associated with depressive symptoms. Although we did not observe a direct path between neighborhood level of violent crime and depressive symptoms, we did find support for two indirect pathways by which neighborhood violent crime is associated with depressive symptoms: through perceptions of neighborhood disorder and through experiences of violence in the neighborhood. Our hypothesized sequence (neighborhood violence impacts perceptions of neighborhood disorder and exposure to violence, which both in turn impact level of psychological distress) is further supported by the use of a prospective design. Psychological distress was measured approximately 2 years after measurement of neighborhood violent crime and perceptions of neighborhood disorder. Experiencing violence was measured concurrently with psychological distress, at time 2.
Our sample represented a homogenous group of individuals with a low socioeconomic background living in neighborhoods with high levels of drug activity. The homogeneity of the sample is both a strength and weakness of this study. If the sample had included a wider range of affluent neighborhoods and participants, it is likely that the results would be strengthened due to the increase in variation of both predictors and outcomes. However, different processes and pathways may operate within different populations. In more affluent neighborhoods, with little crime or disorder, there may be no observable impact of violent crime on mental health status. Furthermore, higher levels of available social support and social resources in more affluent neighborhoods may have a greater impact on mental health status. The vast majority of studies that have examined the mitigating impacts of social support and social resources on the relationship between neighborhood conditions and negative outcomes have focused on children and adolescents (Drukker, Kaplan, Schneiders, Feron, & van Os, 2006; Garmezy, 1993). More research is needed that examines this association among adults.
The significant but modest correlation between perceptions of neighborhood disorder and neighborhood violent crime indicates that residents’ perception of the condition of their neighborhood may be accurate. The correlation however is not strong, partially due to the fact that level of violent crime and neighborhood disorder are not identical constructs. Furthermore, police data, while considered an ’objective’ measure of the level of violent crime in a block group, may be inadequate to assess less serious and more frequent forms of neighborhood violence. In extremely disadvantaged areas with high levels of illicit drug trade and serious violence, police may not be able to arrest or report many less serious violent incidents. Additionally, violent incidents of a less serious nature may go unreported to the police, in part due to mistrust and lack of confidence in the ability of police to address less serious violent crimes. More research is needed to examine how less violent crime may be associated with perceived neighborhood disorder and depression.
Our findings have several alternative interpretations. First, the association between exposure to violence and psychological distress could be accounted for by social capital. Using state-level crime rates, Kawachi and colleagues (1999) found that violence is associated with low social capital. The authors propose that fear of crime and violence leads to few interactions among residents and disorganization which impede social capital. Further, researchers have shown that low levels of social capital are associated with poor mental health outcomes (Fitzpatrick, Piko, Wright, & LaGory, 2005; Phongsavan, Chey, Bauman, Brooks, & Silove, 2006).
Another possible explanation for the violence-depression association is mood-congruent bias; that is, individuals who are more distressed may be more likely to recall violent events. Third, it is possible that depressed individuals move into areas of the city that are more violent and have more outward signs of disorder. Lack of financial means could force persons to move to such neighborhoods. In this case, the pathways linking neighborhood conditions and distress that we observed would therefore be spurious, since neighborhood conditions did not cause psychological distress. Our study found an association between neighborhood factors and depression. While the good model fit provides support for the sequence of variables we specify, we cannot claim that higher levels of neighborhood violence cause higher levels of depressive symptoms.
One limitation of this study is our modeling approach. The purpose of this study was not to account for all factors that may influence psychological distress. Rather, the study was an exploratory analysis of the pathways that exist between neighborhood conditions and psychological distress. Path analysis is widely used as an exploratory data analysis tool. However, we recognize that path models are inherently sensitive to correct model specification and that if variables which lie in the ’true’ causal pathways are left out, other model parameters may be incorrectly estimated. Furthermore, it is unlikely that the two pathways we specified are the only ones that lead from neighborhood conditions to psychological distress. However, our results are similar to that of Stiffman et al (1992), which provide support for the relationship between neighborhood conditions and mental health outcomes. Another limitation of the study is that due to sampling the study’s generalizability is limited.
Despite these limitations, this study has several implications. Both neighborhood crime and perceptions of neighborhood are related to mental health of local residents. Community-wide and structural violence prevention interventions, such as stricter enforcement of laws, increased police presence, neighborhood watch groups, and installation of surveillance cameras are needed in urban communities. Such interventions may serve as a barrier for perpetuators, thus decreasing neighborhood criminal levels as well as likelihood of being victimized. Further, Cohen et al. (2003) suggest that stricter enforcement of zoning and housing codes and additional efforts to keep streets clean are policies that cities can consider to decrease the impact of “broken windows” on the health of inner-city residents. Although this theory is the product of debate, (Taylor, 2001), these policies may improve residents’ perceptions of their neighborhood which may ultimately lead to lower levels of depressive symptoms.
Figure 2.
Final Path Model of Indirect Effects of Block Group Level Violence on Psychological Distress Among Sample of Current and Former Drug Users in Baltimore, Maryland
Acknowledgments
This work was funded by the National Institute on Drug Abuse, grant R01DA016555.
References
- Avison WR, Turner RJ. Stressful life events and depressive symptoms: disaggregating the effects of acute stressors and chronic strains. Journal of Health and Social Behavior. 1988;29:253–264. [PubMed] [Google Scholar]
- Bogat GA, Leahy K, von Eye A, Maxwell C, Levendosky AA, Davidson WS. The influence of community violence on the functioning of women experiencing domestic violence. American Journal of Community Psychology. 2005;36:123–132. doi: 10.1007/s10464-005-6237-2. [DOI] [PubMed] [Google Scholar]
- Cohen DA, Farley TA, Mason K. Why is poverty unhealthy? Social and physical mediators. Social Science & Medicine. 2003;57:1631–1641. doi: 10.1016/s0277-9536(03)00015-7. [DOI] [PubMed] [Google Scholar]
- Curry AD. Pathways to depression: The impact of neighborhood violent crime on inner-city residents in Baltimore, Maryland. Dissertation Abstracts International. 2004 doi: 10.1016/j.socscimed.2008.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutrona CE, Wallace G, Wesner KA. Neighborhood characteristics and depression: An examination of stress processes. Current Directions in Psychological Science. 2006;15:188–192. doi: 10.1111/j.1467-8721.2006.00433.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drukker M, Kaplan C, Schneiders J, Feron FJ, van Os J. The wider social environment and changes in self-reported quality of life in the transition from late childhood to early adolescence: a cohort study. BMC Public Health. 2006;6(133):133. doi: 10.1186/1471-2458-6-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupere V, Perkins DD. Community types and mental health: a multilevel study of local environmental stress and coping. American Journal of Community Psychology. 2007;39:107–119. doi: 10.1007/s10464-007-9099-y. [DOI] [PubMed] [Google Scholar]
- Fauth RC, Leventhal T, Brooks-Gunn J. Short-term effects of moving from public housing in poor to middle-class neighborhoods on low-income, minority adults’ outcomes. Social Science & Medicine. 2004;59:2271–2284. doi: 10.1016/j.socscimed.2004.03.020. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick KM, Piko BF, Wright DR, LaGory M. Depressive symptomatology, exposure to violence, and the role of social capital among African American adolescents. American Journal of Orthopsychiatry. 2005;75:262–274. doi: 10.1037/0002-9432.75.2.262. [DOI] [PubMed] [Google Scholar]
- Galea S, Ahern J, Nandi A, Tracy M, Beard J, Vlahov D. Urban neighborhood poverty and the incidence of depression in a population-based cohort study. Annals of Epidemiology. 2007;17:171–179. doi: 10.1016/j.annepidem.2006.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garmezy N. Children in poverty: resilience despite risk. Psychiatry. 1993;56:127–136. doi: 10.1080/00332747.1993.11024627. [DOI] [PubMed] [Google Scholar]
- Gary TL, Stark SA, LaVeist TA. Neighborhood characteristics and mental health among African Americans and whites living in a racially integrated urban community. Health and Place. 2007;13:569–575. doi: 10.1016/j.healthplace.2006.06.001. [DOI] [PubMed] [Google Scholar]
- Glassman AH, Shapiro PA. Depression and the course of coronary artery disease. American Journal of Psychiatry. 1998;155:4–11. doi: 10.1176/ajp.155.1.4. [DOI] [PubMed] [Google Scholar]
- Goldsmith HF, Holzer CE, III, Manderscheid RW. Neighborhood characteristics and mental illness. Evaluation and Programming Planning. 1998;21:211–225. [Google Scholar]
- Harries K. Social stress and trauma: synthesis and spatial analysis. Social Science & Medicine. 1997;45:1251–1264. doi: 10.1016/s0277-9536(97)00053-1. [DOI] [PubMed] [Google Scholar]
- Inaba A, Thoits PA, Ueno K, Gove WR, Evenson RJ, Sloan M. Depression in the United States and Japan: gender, marital status, and SES patterns. Social Science. 2005;61:2280–2292. doi: 10.1016/j.socscimed.2005.07.014. [DOI] [PubMed] [Google Scholar]
- Jiang W, Krishnan RR, O’Connor CM. Depression and heart disease: evidence of a link, and its therapeutic implications. CNS Drugs. 2002;16:111–127. doi: 10.2165/00023210-200216020-00004. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Kennedy BP, Wilkinson RG. Crime: social disorganization and relative deprivation. Social Science & Medicine. 1999;48:719–731. doi: 10.1016/s0277-9536(98)00400-6. [DOI] [PubMed] [Google Scholar]
- Kessler RC. Stress, social status, and psychological distress. Journal of Health and Social Behavior. 1979;20:259–272. [PubMed] [Google Scholar]
- Kruger DJ, Reischl TM, Gee GC. Neighborhood Social Conditions Mediate the Association Between Physical Deterioration and Mental Health. American Journal of Community Psychology. 2007 doi: 10.1007/s10464-007-9139-7. [DOI] [PubMed] [Google Scholar]
- Latkin CA, Curry AD. Stressful neighborhoods and depression: a prospective study of the impact of neighborhood disorder. Journal of Health and Social Behavior. 2003;44:34–44. [PubMed] [Google Scholar]
- Lofors J, Sundquist K. Low-linking social capital as a predictor of mental disorders: A cohort study of 4.5 million Swedes. Social Science & Medicine. 2007;64:21–34. doi: 10.1016/j.socscimed.2006.08.024. [DOI] [PubMed] [Google Scholar]
- MacMahon KM, Lip GY. Psychological factors in heart failure: a review of the literature. Archives of Internal Medicine. 2002;162:509–516. doi: 10.1001/archinte.162.5.509. [DOI] [PubMed] [Google Scholar]
- Maddock C, Pariante CM. How does stress affect you? An overview of stress, immunity, depression and disease. Epidemiologia e psichiatria sociale. 2001;10:153–162. doi: 10.1017/s1121189x00005285. [DOI] [PubMed] [Google Scholar]
- Matheson FI, Moineddin R, Dunn JR, Creatore MI, Gozdyra P, Glazier RH. Urban neighborhoods, chronic stress, gender and depression. Social Science & Medicine. 2006;63:2604–2616. doi: 10.1016/j.socscimed.2006.07.001. [DOI] [PubMed] [Google Scholar]
- McLeod JD, Kessler RC. Socioeconomic status differences in vulnerability to undesirable life events. Journal of Health and Social Behavior. 1990;31:162–172. [PubMed] [Google Scholar]
- Perkins DD, Meeks JW, Taylor RB. The physical environment of street blocks and resident perceptions of crime and disorder: Implications for theory and measurement. Journal of Environmental Psychology. 1992;12:21–34. [Google Scholar]
- Phongsavan P, Chey T, Bauman A, Brooks R, Silove D. Social capital, socio-economic status and psychological distress among Australian adults. Social Science & Medicine. 2006;63:2546–2561. doi: 10.1016/j.socscimed.2006.06.021. [DOI] [PubMed] [Google Scholar]
- Propper C, Jones K, Bolster A, Burgess S, Johnston R, Sarker R. Local neighbourhood and mental health: evidence from the UK. Social Science & Medicine. 2005;61:2065–2083. doi: 10.1016/j.socscimed.2005.04.013. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Radloff LS, Locke BZ. The community mental health assessment survey and the CES-D scale. In: Weissman MM, Myers JK, Ross CE, editors. Community Surveys of Psychiatric Disorder. Rutgers University Press; New Brunswick, NJ: 1986. pp. 177–189. [Google Scholar]
- Ross CE. Neighborhood disadvantage and adult depression. Journal of Health and Social Behavior. 2000;41:177–187. [Google Scholar]
- Selner-O’Hagan MB, Kindlon DJ, Buka SL, Raudenbush SW, Earls FJ. Assessing exposure to violence in urban youth. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1998;39:215–224. [PubMed] [Google Scholar]
- Silver E, Mulvey EP, Swanson JW. Neighborhood structural characteristics and mental disorder: Faris and Dunham revisited. Social Science & Medicine. 2002;55:1457–1470. doi: 10.1016/s0277-9536(01)00266-0. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Feldman PJ. Neighborhood problems as sources of chronic stress: development of a measure of neighborhood problems, and associations with socioeconomic status and health. Annals of Behavioral Medicine. 2001;23:177–185. doi: 10.1207/S15324796ABM2303_5. [DOI] [PubMed] [Google Scholar]
- Stiffman AR, Dore P, Earls F, Cunningham R. The influence of mental health problems on AIDS-related risk behaviors in young adults. Journal of Nervous Mental Disorders. 1992;180:314–320. doi: 10.1097/00005053-199205000-00005. [DOI] [PubMed] [Google Scholar]
- Stiffman AR, Hadley-Ives E, Elze D, Johnson S, Dore P. Impact of environment on adolescent mental health and behavior: structural equation modeling. American Journal of Orthopsychiatry. 1999;69:73–86. doi: 10.1037/h0080383. [DOI] [PubMed] [Google Scholar]
- Sundquistm K, Ahlen H. Neighbourhood income and mental health: A multi-level follow-up study of psychiatric hospital admissions among 4.5 million women and men. Health & Place. 2006;12:594–602. doi: 10.1016/j.healthplace.2005.08.011. [DOI] [PubMed] [Google Scholar]
- Taylor RB. Breaking away from broken windows: Baltimore neighborhoods and the nationwide fight against crime, grime, fear, and decline. xviii ed Westview Press; Boulder, CO: 2001. [Google Scholar]
- Truong KD, Ma S. A systematic review of relations between neighborhoods and mental health. The Journal of Mental Health Policy and Economics. 2006;9:137–154. [PubMed] [Google Scholar]
- Wen M, Hawkley LC, Cacioppo JT. Objective and perceived neighborhood environment, individual SES and psychosocial factors, and self-rated health: An analysis of older adults in Cook County, Illinois. Social Science & Medicine. 2006;63:2575–2590. doi: 10.1016/j.socscimed.2006.06.025. [DOI] [PubMed] [Google Scholar]
- Ziersch AM, Baum FE, Macdougall C, Putland C. Neighbourhood life and social capital: the implications for health. Social Science & Medicine. 2005;60:71–86. doi: 10.1016/j.socscimed.2004.04.027. [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Coryell W. The validity of a self-report questionnaire for diagnosing major depressive disorder. Archives of General Psychiatry. 1988;45:738–740. doi: 10.1001/archpsyc.1988.01800320050006. [DOI] [PubMed] [Google Scholar]