Abstract
AIM: To clarify the characteristic features of biliary lesions in patients with autoimmune pancreatitis (AIP) and compare them with those of primary sclerosing cholangitis (PSC).
METHODS: The clinicopathological characteristics of 34 patients with sclerosing cholangitis (SC) associated with AIP were compared with those of 4 patients with PSC.
RESULTS: SC with AIP occurred predominantly in elderly men. Obstructive jaundice was the most frequent initial symptom in SC with AIP. Only SC patients with AIP had elevated serum IgG4 levels, and sclerosing diseases were more frequent in these patients. SC patients with AIP responded well to steroid therapy. Segmental stenosis of the lower bile duct was observed only in SC patients with AIP, but a beaded and pruned-tree appearance was detected only in PSC patients. Dense infiltration of IgG4-positive plasma cells was detected in the bile duct wall and the periportal area, as well as in the pancreas, of SC patients with AIP.
CONCLUSION: SC with AIP is distinctly different from PSC. The two diseases can be discriminated based on cholangiopancreatographic findings and serum IgG4 levels.
Keywords: Autoimmune pancreatitis, IgG4, Primary sclerosing cholangitis, Sclerosing cholangitis
INTRODUCTION
Autoimmune pancreatitis (AIP) is a unique form of pancreatitis in which autoimmune mechanisms are suspected of being involved in the pathogenesis. AIP has many clinical, radiological, serological and histopathological characteristics: (1) elderly male preponderance; (2) initial symptom is frequently painless obstructive jaundice; (3) occasional association with impaired pancreatic endocrine or exocrine function, and various extrapancreatic lesions; (4) favorable response to steroid therapy; (5) radiological findings of irregular narrowing of the main pancreatic duct and enlargement of the pancreas; (6) serological findings of elevated serum γ globulin, IgG, or IgG4 levels, along with the presence of some autoantibodies; and (7) histopathological findings of dense infiltration of T lymphocytes and IgG4-positive plasma cells with fibrosis and obliterative phlebitis in the pancreas[1–3]. Bile duct stenosis occurs frequently with AIP, and the major initial symptom in AIP patients is obstructive jaundice. The lower portion of the common bile duct is frequently stenotic. However, when AIP patients develop stenosis in the intrahepatic bile duct, the cholangiographic appearance is similar to that of primary sclerosing cholangitis (PSC)[4,5]. PSC is a progressive disease involving the intra- and extra-hepatic bile ducts. Despite therapy, PSC sometimes leads to liver cirrhosis. However, since AIP patients respond well to steroid therapy, it is necessary to discriminate between sclerosing cholangitis (SC) associated with AIP and PSC. This study aimed to clarify the characteristic features of biliary lesions in AIP patients and compare them with those of PSC.
MATERIALS AND METHODS
Study patients
Over a 27-year-period, 43 patients (36 male and 7 female, average age 66.4 years) at Tokyo Metropolitan Komagome Hospital were diagnosed with AIP based on the following clinicopathological criteria: irregular narrowing of the main pancreatic duct on endoscopic retrograde pancreatography (n = 43), pancreatic enlargement on ultrasonography (US) or computed tomography (CT) (n = 42), presence of autoantibodies (n = 22), elevated serum IgG4 level in excess of 135 mg/dL (n = 31), characteristic histological findings in the pancreas (n = 12), and responsiveness to steroid therapy (n = 32). In the 43 AIP patients, 34 had SC (lower bile duct in 34, and intrahepatic bile duct in 4). During the same time, 4 patients were diagnosed with PSC according to appropriate criteria[6].
Methods
The stenotic portion of the bile duct was examined by endoscopic retrograde cholangiopancreatography and/or magnetic resonance cholangiopancreatography, and wall thickening of the bile duct in which stenosis was not obvious on cholangiography was assessed on CT and US. Two experienced gastroenterologists retrospectively reviewed these imaging findings without information on the patients. Extrapancreatic lesions, including sclerosing sialadenitis, sclerosing cholecystitis, and retroperitoneal fibrosis, were evaluated on physical examination, CT, and US. Serum IgG4 levels were measured in 30 AIP patients and 2 PSC patients. Histological examination and immunostaining with anti-IgG4 antibody were performed on specimens of the extrahepatic bile duct (6 AIP patients and 1 PSC patient) and liver (3 AIP and 2 PSC patients).
Statistical analysis
Statistical differences between the two groups were analyzed first by the Kruskal-Wallis H-test, followed by Mann-Whitney’s U-test if significant. Other analyses were performed using Fisher’s exact test. In all tests, P < 0.05 was considered statistically significant.
RESULTS
Clinical features
Men were significantly more commonly affected by SC with AIP than by PSC. Patients’ age at diagnosis was significantly older in those with SC with AIP. Among the initial symptoms, obstructive jaundice was the most frequently observed in SC with AIP. Elevated serum IgG4 levels were frequent in SC patients with AIP, but not in the 2 PSC patients examined. Sclerosing diseases were frequently associated with SC with AIP. Ulcerative colitis was present in only 2 young PSC patients (Table 1). Thirty-two SC patients with AIP were treated with steroid therapy, and all of them showed a good response. All PSC patients were treated with ursodeoxycholic acid, and 1 patient underwent steroid therapy for associated ulcerative colitis. Cholangiographic findings progressed gradually in three PSC patients, and one patient ultimately required liver transplantation. All SC patients with AIP had a favorable outcome without liver failure.
Table 1.
Clinical differences between sclerosing cholangitis with autoimmune pancreatitis and primary sclerosing cholangitis
| SC with AIP | PSC | Pvalue | |
| Average age (yr) | 63.8 | 39.2 | < 0.01 |
| Male/Female | 29/5 | 1/3 | < 0.05 |
| Obstructive jaundice +/- | 30/4 | 0/4 | < 0.01 |
| Elevated serum IgG4 +/- | 26/30 | 0/2 | |
| Associated sclerosing disease +/- | 20/14 | 0/4 | < 0.05 |
| Associated ulcerative colitis +/- | 0/34 | 2/2 | < 0.01 |
SC with AIP: Sclerosing cholangitis with autoimmune pancreatitis; PSC: Primary sclerosing cholangitis.
Cholangiopancreatographic findings
On pancreatography, narrowing of the main pancreatic duct was detected in all SC patients with AIP, but no abnormal findings were detected in any of the PSC patients. On cholangiography, the intrahepatic bile duct was involved in all PSC patients, but was involved in only four SC patients with AIP (Figure 1). Segmental stenosis of the lower bile duct was observed in all SC patients with AIP, but was not detected in any of the PSC patients. Extensive involvement of the bile duct, showing widespread wall thickening of the middle and upper bile duct where stenosis was not obvious on cholangiography, was detected only in 14 SC patients with AIP, although there was no significant difference between the two groups. A diffusely distributed, beaded and pruned-tree appearance and diverticular formation were detected only in PSC patients (Figure 2 and Table 2). A long stricture was detected in the hepatic hilar region in all 4 SC patients with AIP involving the intrahepatic bile duct.
Figure 1.
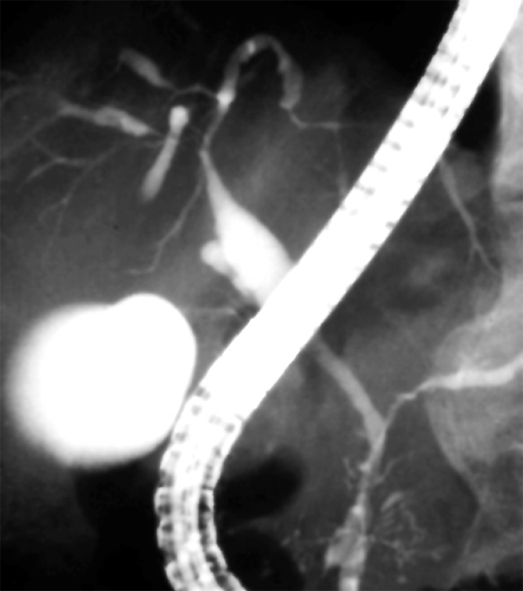
Endoscopic retrograde cholangiography of a patient with autoimmune pancreatitis showing a relatively long stricture of the hepatic hilar bile duct.
Figure 2.
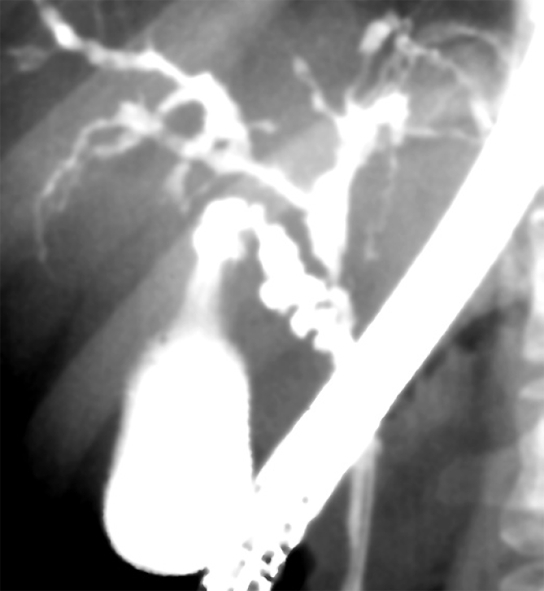
Endoscopic retrograde cholangiography of a patient with primary sclerosing cholangitis showing beaded and pruned-tree appearance.
Table 2.
Cholangiopancreatographic differences between sclerosing cholangitis with autoimmune pancreatitis and primary sclerosing cholangitis
| SC with AIP | PSC | Pvalue | |
| Narrowing of the main pancreatic duct +/- | 34/0 | 0/4 | < 0.01 |
| Stenosis of the intrahepatic bile duct +/- | 4/30 | 4/0 | < 0.01 |
| Stenosis of the lower bile duct +/- | 34/0 | 0/4 | < 0.01 |
| Extensive bile duct wall thickening | 14/20 | 0/4 | NS |
| Beaded appearance | 0/34 | 2/2 | < 0.01 |
| Pruned-tree appearance | 0/34 | 3/1 | < 0.01 |
| Diverticular formation | 0/34 | 2/2 | < 0.01 |
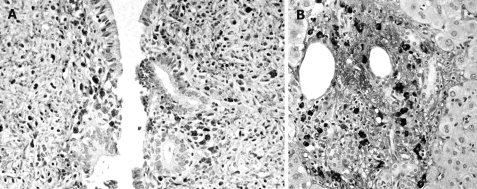
Histological and immunohistochemical findings
In PSC, the hilar bile duct displayed diffuse fibrosis with moderate lymphoplasmacytic infiltration. The liver of PSC patients showed features of biliary cirrhosis, and fibro-obliterative lesions characterized by onion skin-like periductal fibrosis with predominantly lymphocytic infiltration were observed around the intrahepatic bile duct. However, infiltration of IgG4-positive plasma cells was not detected in the bile duct or liver.
The histological findings of SC associated with AIP included transmural fibrosis and dense lymphoplasmacytic infiltration of the bile duct wall, along with lymphoplasmacytic infiltration and fibrosis in the periportal area of the liver. Compared with PSC, lymphoplasmacytic infiltration was denser, the degree of fibrosis was less severe, and the onion skin-like appearance was not observed. Dense infiltration of IgG4-positive plasma cells was detected in the bile duct wall (Figure 3A) and the periportal area (Figure 3B), as well as in the pancreas, of patients with AIP.
Figure 3.
IgG4-immunostaining of the bile duct (A) and liver (B) of a patient with autoimmune pancreatitis. Dense infiltration of IgG4-positive plasma cells was detected in the bile duct wall (A) and the periportal area of the liver (B).
DISCUSSION
SC is a heterogeneous disease that may be associated with choledocholithiasis, biliary tumor, or infection. SC of unknown origin is called PSC. PSC is progressive despite conservative therapy and involves the intra- and extrahepatic bile ducts, resulting in liver cirrhosis. The effect of steroid therapy is questionable, and liver transplantation currently provides the greatest hope for a possible cure. It occurs among patients in their 30 and 40 s and is frequently associated with inflammatory bowel disease[7,8]. Pancreatograms are not abnormal in most cases[9].
However, an analysis of 192 PSC patients in Japan found that their characteristics differed from those in Western counties, with regard to age distribution and the incidence of complications[10]. In that analysis, the patients were predominantly men, and two peaks in age distribution at diagnosis (20-30 years and 50-70 years) were identified. Compared to younger patients, those aged 40 years or older displayed a lower incidence of associated ulcerative colitis, whereas the incidence of chronic pancreatitis was higher.
SC is frequently associated with AIP, and occurs predominantly in elderly men. The major initial symptom of SC with AIP is obstructive jaundice, which differs from PSC. The most prominent feature on cholangiography for SC with AIP was stenosis of the lower bile duct. When stenosis is found in the intrahepatic or the hilar hepatic bile duct, the cholangiographic appearance is very similar to that of PSC[4,5]. However, a long stricture was detected in the hepatic hilar region in SC patients with AIP, instead of the beaded and pruned-tree appearance that is frequently observed in PSC. Widespread wall thickening of the middle and upper bile ducts was also detected only in SC patients with AIP.
SC patients with AIP responded dramatically well to steroid therapy and showed a favorable outcome[5,9,11]. Histologically, dense infiltration of IgG4-positive plasma cells was detected in the bile duct wall and the periportal area of SC patients with AIP, but it was not detected in PSC patients. SC with AIP is sometimes associated with sclerosing diseases such as sclerosing sialadenitis, sclerosing cholecystitis, or retroperitoneal fibrosis, and these salivary, gallbladder, and retroperitoneal lesions show similar histological findings to those in the bile duct and pancreas. Furthermore, abundant infiltration of IgG4-positive plasma cells is detected in various organs of AIP patients[12,13]. Therefore, we proposed a new clinicopathological entity, an IgG4-related sclerosing disease, which is histopathologically characterized by extensive IgG4-positive plasma cell and T lymphocyte infiltration of various organs. We also suspect that AIP and SC with AIP is a pancreatic and bile duct lesion of this systemic disease[13–15]. Based on the above findings, SC with AIP should be differentiated from PSC. In particular, since SC with AIP responds well to steroid therapy, discrimination between the two diseases is necessary before making therapeutic decisions. Clinically, serum IgG4 levels and cholangiopancreatographic findings are useful in differentiating between the two diseases.
Considering the predominance of elderly men, the infrequent association with inflammatory bowel disease, and the frequent association with chronic pancreatitis, many older patients diagnosed with PSC in Japan may actually have SC with AIP.
In conclusion, since SC with AIP is induced by different mechanisms to those in PSC, the condition should be differentiated from PSC. The two diseases can be discriminated based on their cholangiopancreatographic findings and serum IgG4 levels.
COMMENTS
Background
When patients with autoimmune pancreatitis (AIP) develop stenosis in the intrahepatic bile duct, the cholangiographic appearance is similar to that of primary sclerosing cholangitis (PSC). PSC is a progressive disease involving the intra- and extrahepatic bile ducts.
Innovations and breakthroughs
Sclerosing cholangitis with AIP is distinctly different from PSC. Only SC patients with AIP had elevated serum IgG4 levels and responded well to steroid therapy. Segmental stenosis of the lower bile duct was observed only in SC patients with AIP, but a beaded and pruned-tree appearance was detected only in PSC patients. Dense infiltration of IgG4-positive plasma cells was detected in the bile duct wall and the periportal area of SC patients with AIP.
Applications
Sclerosing cholangitis with AIP responds well to steroid therapy. The differential diagnosis between sclerosing cholangitis with AIP and PSC is important to ensure optimal patient treatment.
Peer review
The authors described the characteristic features of biliary lesions in autoimmune pancreatitis patients. The paper is well presented and the result are interesting.
Peer reviewer: Kiichi Tamada, MD, Department of Gastroenterology, Jichi Medical Shool, 3311-1 Yakushiji, Mina-mikawachi, Kawachigun, Tochigi 329-0498, Japan
S- Editor Li LF L- Editor Webster JR E- Editor Ma WH
References
- 1.Okazaki K, Uchida K, Chiba T. Recent concept of autoimmune-related pancreatitis. J Gastroenterol. 2001;36:293–302. doi: 10.1007/s005350170094. [DOI] [PubMed] [Google Scholar]
- 2.Kim KP, Kim MH, Song MH, Lee SS, Seo DW, Lee SK. Autoimmune chronic pancreatitis. Am J Gastroenterol. 2004;99:1605–1616. doi: 10.1111/j.1572-0241.2004.30336.x. [DOI] [PubMed] [Google Scholar]
- 3.Lara LP, Chari ST. Autoimmune pancreatitis. Curr Gastroenterol Rep. 2005;7:101–106. doi: 10.1007/s11894-005-0047-4. [DOI] [PubMed] [Google Scholar]
- 4.Nakazawa T, Ohara H, Yamada T, Ando H, Sano H, Kajino S, Hashimoto T, Nakamura S, Ando T, Nomura T, et al. Atypical primary sclerosing cholangitis cases associated with unusual pancreatitis. Hepatogastroenterology. 2001;48:625–630. [PubMed] [Google Scholar]
- 5.Kamisawa T, Egawa N, Tsuruta K, Okamoto A, Funata N. Primary sclerosing cholangitis may be overestimated in Japan. J Gastroenterol. 2005;40:318–319. doi: 10.1007/s00535-004-1543-2. [DOI] [PubMed] [Google Scholar]
- 6.Linder K, LaRusso NF. Primary sclerosing cholangitis. In: ER Schiff, MF Sorrell, WC Maddrey., editors. Disease of the liver. 9th ed. Philadelphia: JB Lippincott; 2003. pp. 673–684. [Google Scholar]
- 7.LaRusso NF, Wiesner RH, Ludwig J, MacCarty RL. Current concepts. Primary sclerosing cholangitis. N Engl J Med. 1984;310:899–903. doi: 10.1056/NEJM198404053101407. [DOI] [PubMed] [Google Scholar]
- 8.Wiesner RH, Grambsch PM, Dickson ER, Ludwig J, MacCarty RL, Hunter EB, Fleming TR, Fisher LD, Beaver SJ, LaRusso NF. Primary sclerosing cholangitis: natural history, prognostic factors and survival analysis. Hepatology. 1989;10:430–436. doi: 10.1002/hep.1840100406. [DOI] [PubMed] [Google Scholar]
- 9.Nakazawa T, Ohara H, Sano H, Ando T, Aoki S, Kobayashi S, Okamoto T, Nomura T, Joh T, Itoh M. Clinical differences between primary sclerosing cholangitis and sclerosing cholangitis with autoimmune pancreatitis. Pancreas. 2005;30:20–25. [PubMed] [Google Scholar]
- 10.Takikawa H, Manabe T. Primary sclerosing cholangitis in Japan--analysis of 192 cases. J Gastroenterol. 1997;32:134–137. doi: 10.1007/BF01213311. [DOI] [PubMed] [Google Scholar]
- 11.Kamisawa T, Egawa N, Nakajima H, Tsuruta K, Okamoto A. Morphological changes after steroid therapy in autoimmune pancreatitis. Scand J Gastroenterol. 2004;39:1154–1158. doi: 10.1080/00365520410008033. [DOI] [PubMed] [Google Scholar]
- 12.Kamisawa T, Funata N, Hayashi Y, Tsuruta K, Okamoto A, Amemiya K, Egawa N, Nakajima H. Close relationship between autoimmune pancreatitis and multifocal fibrosclerosis. Gut. 2003;52:683–687. doi: 10.1136/gut.52.5.683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kamisawa T, Funata N, Hayashi Y, Eishi Y, Koike M, Tsuruta K, Okamoto A, Egawa N, Nakajima H. A new clinicopathological entity of IgG4-related autoimmune disease. J Gastroenterol. 2003;38:982–984. doi: 10.1007/s00535-003-1175-y. [DOI] [PubMed] [Google Scholar]
- 14.Kamisawa T, Nakajima H, Egawa N, Funata N, Tsuruta K, Okamoto A. IgG4-related sclerosing disease incorporating sclerosing pancreatitis, cholangitis, sialadenitis and retroperitoneal fibrosis with lymphadenopathy. Pancreatology. 2006;6:132–137. doi: 10.1159/000090033. [DOI] [PubMed] [Google Scholar]
- 15.Kamisawa T, Okamoto A. Autoimmune pancreatitis: proposal of IgG4-related sclerosing disease. J Gastroenterol. 2006;41:613–625. doi: 10.1007/s00535-006-1862-6. [DOI] [PMC free article] [PubMed] [Google Scholar]