Abstract
Introduction
The diagnosis and subsequent treatment for early stage breast cancer is stressful for partners. Little is known about the role of cognitive and social processes predicting the longitudinal course of partners’ psychosocial adaptation. This study evaluated the role of cognitive and social processing in partner psychological adaptation to early stage breast cancer, evaluating both main and moderator effect models. Moderating effects for meaning-making, acceptance, and positive reappraisal on the predictive association of searching for meaning, emotional processing, and emotional expression on partner psychological distress were examined.
Materials and Methods
Partners of women diagnosed with early stage breast cancer were evaluated shortly after the ill partner’s diagnosis (n= 253), nine (n = 167), and 18 months (n = 149) later. Partners completed measures of emotional expression, emotional processing, acceptance, meaning-making, and general and cancer-specific distress at all time points.
Results
Lower satisfaction with partner support predicted greater global distress, and greater use of positive reappraisal was associated with greater distress. The predicted moderator effects for found meaning on the associations between the search for meaning and cancer-specific distress were found and similar moderating effects for positive reappraisal on the associations between emotional expression and global distress and for acceptance on the association between emotional processing and cancer-specific distress were found.
Conclusions
Results indicate several cognitive-social processes directly predict partner distress. However, moderator effect models in which the effects of partners’ processing depends upon whether these efforts result changes in perceptions of the cancer experience may add to the understanding of partners’ adaptation to cancer.
Keywords: Spouses, breast cancer, psychological adaptation
The diagnosis and subsequent treatment of early stage breast cancer impacts not only the woman but her partner as well. Indeed, studies have indicated that husbands of women diagnosed with early stage breast cancer report significantly higher levels of distress and significantly lower emotional role functioning than community comparison groups (Wagner, Bigatt, & Storniolo, 2006) and significantly higher levels of distress than husbands of women diagnosed with benign breast disease (Maguire, 1985). Research has also indicated that between 20 and 24% of male partners report clinically-significant levels of depression shortly after diagnosis (Given et al., 1993). Findings regarding the course of distress have been inconsistent with some studies indicating that husbands’ distress remains stable over time (Omne-Ponten, Holmberg, Bergstrom, Sjoden, & Burns, 1993) and other studies suggesting levels of clinically-significant distress decline over time (Keitel, Zevon, Rounds, Petreliia, & Karakousis, 1990).
Compared with what is known about demographic, medical, and psychosocial factors contributing to the long-term course of psychological distress among women diagnosed with early stage breast cancer (Engel et al. 2003; Helgeson, Snyder, & Seltman, 2004), there is relatively little known about factors influencing the course of partners’ psychological adaptation. In an attempt to fill this void, there has been increasing attention paid to this topic over in the last decade. These studies have pointed to a number of personal and social factors contributing to partner adaptation. Greater pre-surgical appraisals of stress (Keitel et al., 1990), more hopelessness and uncertainty (Northouse, Templin, & Mood, 2001), less social support (Northouse, 1988; Wagner et al., 2006), more social conflict (Makabe & Nomizu, 2006), and lower marital satisfaction (Northouse et al., 2001) have been associated with partner distress in prior cross-sectional and longitudinal studies.
Unfortunately, conclusions regarding factors contributing to psychological adaptation among partners are limited because many studies have employed cross-sectional methodologies, have had sample sizes of less than 100, and have included partners of women with benign breast disease. In addition, with one exception (Northouse et al., 2001), these studies have not examined responses across the continuum from active treatment to survivorship. Thus, little is known about the trajectories of distress among partners and what distinguishes partners who are persistently distressed from those who are not persistently distressed. The present study attempts to fill this gap by examining patterns of psychological adaptation among partners of women with early stage breast cancer over a one and a half year period spanning the active treatment to survivorship phases.
When considering factors predicting partner long-term adaptation, it is important to select factors based upon a theoretical perspective. In our work, we have adopted the cognitive-social processing theory which suggests that difficult life experiences challenge people’s beliefs themselves and their environment and cause people to question these core beliefs (Janoff-Bulman, 1999). According to this theory, emotional distress arises from the discrepancy between people’s beliefs about themselves and their environment and the meaning that is inherent in the trauma (Epstein, 1991). A reduction in emotional distress can be achieved by confronting, contemplating, and reevaluating the experience with the goal of adjusting one’s beliefs (Keitel et al., 1990). This integration is called “cognitive processing” (Horowitz, 1986). Research has consistently supported the adaptive role of a number of cognitive processes among individuals coping with cancer. For example, efforts to reframe the cancer experience in positive terms such as utilizing positive reappraisal, finding benefit and meaning in the event, and increasing acceptance have been associated with less concurrent and long-term distress (Carver et al., 1993; Sears, Stanton & Danoff-Burg, 2003).
One common way that people process events is by sharing their thoughts and feelings about the experience with others. However, although individuals report the desire to share with others (Coates, Wortman, & Abbey, 1979), there is little evidence that talking alone assists adaptation e.g., (Rime, Philippot, Boca, & Mesquita, 1992). Indeed, how others respond to these disclosures can either aid or interfere with effective cognitive processing (Rime, Mesquita, Philippot, & Boca, 1991). This process has been labeled social modulation of cognitive processing (Lepore, 2001). If the individual perceives that others respond to him or her in a supportive manner, then sharing is more likely to have beneficial effects because supportive responses to disclosures may facilitate successful cognitive processing. Supportive responses help the person learn to tolerate and control negative feelings and intrusive thoughts, support effective coping (Pennebaker, 1989), assist in reestablishing a coherent world view, and facilitate benefit-finding. These responses are typically labeled “social support”. If others do not respond in a manner that is perceived of as supportive, then sharing may not have beneficial effects. Unsupportive responses might impede cognitive processing by inhibiting the person from sharing emotional reactions to the experience, and ultimately lead to cognitive and behavioral avoidance (e.g., Manne, Alfieri, Taylor & Dougherty, 1999).
There has been relatively little attention paid to the role of cognitive processing and social modulation of cognitive processing in partners’ adaptation to cancer. In terms of cognitive processing, Eton and colleagues (2005) evaluated the association between searching for meaning, found meaning, positive reappraisal, and acceptance among wives of men with early stage prostate cancer and found that greater searching for meaning, less found meaning, greater positive reappraisal, and greater acceptance were associated with lower partner distress. In terms of social modulation of cognitive processing, results of several studies support the role of responses of the social network in psychological adaptation to cancer. Cross-sectional studies have suggested that less social support, more social conflict, and lower marital satisfaction are associated with greater partner distress (Given et al., 1993). Eton and colleagues (2005) found that higher marital quality, spouse support, and fewer perceived spouse unsupportive behaviors were associated with less distress among wives of men diagnosed with early stage prostate cancer. In sum, the few cross-sectional studies that have been done support the role of cognitive processing and social modulation of cognitive processing in partner outcomes.
When considering the role of cognitive processing and social modulation of cognitive processing in partners’ adaptation to cancer, it is important to consider that the outcome of cognitive processes such as the searching for meaning and delving into one’s emotions may depend on the success of these attempts in assisting the individual to gain a new perspective on the cancer experience. A search for meaning that is not successful will lead to more distress, whereas a search for meaning that results in found meaning should lead to less distress (Tomich & Helgeson, 2004). However, attempts to understand one’s emotional reactions that result in a new way of thinking about the cancer experience in terms of acceptance or positive reappraisal are likely to lead to less distress, whereas attempts to understand one’s emotional reactions that do not lead to changes in one’s view about the experience are not likely to result in less distress. Similarly, the benefits of sharing emotional reactions to members of one’s social network may not be realized if this sharing does not facilitate a new perspective on the cancer experience in terms of acceptance and/or positive reappraisal (Manne et al., 2007).
The goal of this study was to evaluate the role of cognitive processing and social modulation of cognitive processing in predicting partners’ distress responses to early stage breast cancer. We examined direct influences of these processes as well as moderating influences of specific processes on partner psychological distress. We examined the role of five cognitive processes: searching for meaning, found meaning, acceptance, positive reappraisal, and emotional processing. We examined emotional expression about cancer as well as perceived social modulation of cognitive processing. Perceived satisfaction with support provided by the spouse, family, and friends was assessed as an evaluation of the perceived receptivity and supportiveness of the social network. Our first set of hypotheses involved the direct influences of cognitive processing and social modulation of these processes on partner distress (“main effect models”). We had three predictions. First, we predicted that partners who engaged in greater positive reappraisal would report less global and cancer-specific distress over time. Second, we hypothesized that partners who engaged in greater acceptance would report less global and cancer-specific distress over time. Third, we predicted that partners who reported higher levels of satisfaction with support provided by the patient and other family and friends would report less global and cancer-specific distress over time.
Our second set of hypotheses concerned moderator effects for processes in predicting partner psychosocial outcomes (“moderator effect models”). Specifically, we hypothesized that the effect of some processes on partner distress would depend upon whether these efforts succeeded in altering the partner’s views and appraisals of the patient’s cancer. We had five moderator effect model predictions. First, we predicted that the search for meaning in the patient’s cancer would be associated with less global and cancer-specific distress for those partners who claimed to have found meaning in the patient’s cancer whereas the search for meaning would be associated with more distress for those who claim not to have found meaning. Second, we proposed that attempts to understand one’s emotions (emotional processing) would be associated with less global and cancer-specific distress among partners when these attempts resulted in more acceptance and that emotional processing would predict more global and cancer-specific distress when this processing was associated with lower acceptance. Third, we proposed that emotional processing would be associated with less global and cancer-specific distress among partners when these attempts resulted in a more positive reappraisal of the cancer by the partner and that emotional processing would predict more global and cancer-specific distress when this processing was associated with less positive reappraisal. Fourth, we proposed that emotional expression would be associated with less distress when this expression resulted in greater acceptance of the cancer experience. Fifth, we proposed that emotional expression would be associated with less distress when this expression resulted in greater positive reappraisal of the cancer experience. We studied a large sample of partners and followed them with three assessments over an 18 month period of time.
Methods
Participants and Procedure
This investigation uses data from participants in a larger study of couples’ communication and breast cancer (Manne et al., 2004a; Manne et al., 2004b; Manne et al. 2004c; Manne, Ostroff, Winkel, Grana, & Fox, 2005; Manne et al., 2006; Manne et al., 2007). Participants were 253 partners of women diagnosed with early stage breast cancer undergoing medical treatment for the disease. The eligibility criteria were; a) the ill partner had a primary diagnosis of breast cancer (DCIS or invasive cancer of the breast-Stages I-IIIa); b) the ill partner had completed surgery for breast cancer and was currently enrolled in chemotherapy, radiation, or hormone therapy; c) both partners were 18 years of age or older; d) both partners had no significant neurological deficit; e) both partners were English speaking; f) both partners had no hearing impairment; g) currently married or living with the significant other; h) the partner had no chronic, disabling medical condition. Partners were approached for study participation from outpatient oncology clinics. 690 partners were approached. Participants were given a written informed consent and the study questionnaire to complete and return. 277 partners consented and, among these partners, 253 completed the Time 1 survey (37% acceptance). The most common reasons for refusal were that the participant felt s/he would not receive benefit from participating (39%) and that the survey would take too much time (18.4%). Comparisons were made between participants and refusers with regard to available patient data (patient age, patient stage of disease, patient ethnicity) Results indicated that partner participants were in relationships with younger patients than refusers (M participants = 49.9, M refusers = 53.3, t (688) = 4.3). We could not compare partner refusers with partner participants because we were not able to collect information on partner refusers.
Partners were given surveys immediately upon consenting (Time 1), nine months (Time 2), and 18 months (Time 3) after they consented. Surveys were returned by mail. The nine month time frame was selected because we were interested in assessing partners after the patient had completed active treatment and had entered the survivorship phase.
Measures administered: Outcome variables (all time points)
General Psychological Distress
The distress subscale of the Mental Health Inventory-18 (Ware, Manning, Duan, Wells, & Newhouse, 1984) was administered (9 items, scale rang e =9-53). Participants rated their feelings in the past month. This scale has been used in previous studies assessing partners of cancer patients (Manne & Schnoll, 2001). In the present study, Cronbach’s alphas for the distress scale were .87, .83, and .86 at Time 1, 2, and 3, respectively. Higher scores indicated more distress.
Cancer-specific distress
The 15-item Impact of Events Scale (IES; Horowitz, Wilner, & Alvarez, 1979) was administered. Partners rated their feelings and thoughts about their partner’s breast cancer in the past week on a 4-point Likert scale (0 = “Not at all”, 5 = “Often”)(scale range = 0-75). Cronbach’s alphas were .87, .89, and .90, at Time 1, 2 and 3, respectively.
Measures Administered: Predictor Variables (all time points)
Acceptance, positive reappraisal, emotional processing, and emotional expression
Acceptance and positive reappraisal were assessed by the COPE (Carver et al., 1993). Both scales contain four items with Likert scale ratings from 1 (Did not do this) to 4 (Did this a lot)(scale range = 4-16). Stanton and colleagues’ emotional approach scale (2000) contained two items assessing acknowledgment of and contemplation of the meaning of emotions (emotional processing) and two items assessing expression of emotions (emotional expression) rated from 1 (Did not do this) to 4 (Did this a lot). Participants rated how they dealt with their partner’s cancer in the past month. Internal consistencies for Time 1, 2, and 3 respectively were: Positive reappraisal = .77, .68, .78, Acceptance = .78, .77, .83, Emotional expression = .67, .74, .75; Emotional processing = .70, .69, .66.
Searching for and Finding Meaning
Partners were asked whether they tried to find meaning in the patient’s cancer experience (one item) (1 = not at all, 5 = a great deal) and to what degree they felt they had found meaning in the patient’s cancer experience (one item) (1 = not at all, 5 = a great deal). Similar items were used by Eton and colleagues (2005) and others (Wu et al., in press; Markarian et al., 2006. Items were rated with an instruction to report searching for and finding meaning in the past month.
Satisfaction with Support Provided
A scale was composed specifically for this study to assess how satisfied the partner was with support they received from the patient and from other family and friends. Items assessed the four main functions of social support (Gottlieb, 1978): tangible, emotional, advice or guidance, and reassurance. There were separate and equivalent Likert scales for partner (4 items) and friends and family (4 items) (1 = very satisfied, 6 = very dissatisfied) (scale range = 4-24). No time frame instruction was provided for ratings. Cronbach’s alphas were .91, .93 and .93 for satisfaction with support from the patient at Time 1, 2, and 3, respectively, and Cronbach’s alphas were .88, .94, and .95 for satisfaction with support from other family and friends at Time 1, 2, and 3, respectively. Higher scores indicated greater dissatisfaction with support and were reverse coded for the subsequent analyses. In addition, the satisfaction with support scale was kurtotic. Both a square root and a log transformation were applied to reduce the kurtosis. The log transformation was most effective and subsequently used.
Receipt of psychosocial care
At each time point, participants were asked whether they were_currently seeing a religious counselor, a professional counselor, attended a support group, took psychotropic medication in the past month, or sought another type of psychosocial care (e.g., complementary therapy) (yes/no). The five items were summed (scale range= 0-5). The resulting scale was kurtotic. Both a square root and a log transformation were applied to reduce the kurtosis. The square root transformation was most effective and subsequently used.
Patient Medical Variables
Data regarding the patient’s disease stage, medical treatment, type of surgery, date of diagnosis, and physician-rated Eastern Cooperative Oncology Group scores (ECOG) of the patient’s physical functioning were obtained from the patient’s chart at each time point. Physical impairment ratings from the 26-item CARES (Manne et al. 2006) were completed by patients at each time point and included in the analyses.
Results
Sample Characteristics
In terms of education, 3% of the partners had some high school education, 11% of the partners completed high school, 17% of the partners completed between one to three years of college, 19% of partners completed college, 12% of partners completed trade or business school, 8% completed some graduate level education, and 30% completed a graduate degree. The median household income level was $84,000. Most partners (91%) were Caucasian. Most partners were married (95%) and (97%) were male. The average age was 51.2 years (SD = 11.2 years, range =26-80 years). The average relationship length was 22 years (range= 2-57 years).
Patient cancer stages included ductal carcinoma in-situ (DCIS)(9.7%), stage 1 (36.4%), stage 2 (50.6%), and stage 3A (3.2%) breast cancer. 27.2% of patients underwent mastectomy and the remaining 72.7% underwent breast-conserving surgery. The average time from the patient’s diagnosis and the partner completion of the Time 1 survey was 5 months (range = 1-12 months). After surgery, the majority of the patients had chemotherapy (87%). The average time between Time 1 and 2 surveys was 10 months, and the average time between the Time 2 and Time 3 surveys was 10 months.
Psychological distress and psychosocial care utilization
Means, standard deviations, and ranges for partners’ global (MHI distress) and cancer-specific distress (IES) scores at the three time points are shown in Table 1. The MHI-18 distress scale does not have an established cutoff score. Therefore, partners’ MHI distress scores were compared with normative data provided by the authors of this scale (Stewart, Sherbourne, & Hays, 1992). The means of the present sample at all time points were lower than the normative mean for the MHI distress scale (M = 23.0, SD = 19.2). There are no published data on MHI-18 distress scale scores derived from a sample of partners of women diagnosed with early stage breast cancer to provide a comparison for the present sample with other studies that have examined partner distress.
Table l.
Descriptive Information Regarding Partner Psychological Variables Included in the Analyses
| Variable | Time 1 | Time 2 | Time 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| M | (SD) | Range | M | (SD) | Range | M | (SD) | Range | |
| Global MHI distress | 20.21 | (6.69) | 10-58 | 19.22 | (6.31) | 10-40 | 18.47 | (5.79) | 10-44 |
| Cancer-specific distress | 18.40 | (13.00) | 0-53 | 14.36 | (12.35) | 0-51 | 12.73 | (12.15) | 0-49 |
| Psychosocial care use | 0.22 | (0.55) | 0-3 | 0.24 | (0.64) | 0-4 | 0.34 | (.95) | 0 -5 |
| Searching for meaning | 2.60 | (1.31) | 1-5 | 2.41 | (1.27) | 1-5 | 2.14 | (1.17) | 1-5 |
| Finding meaning | 2.39 | (1.27) | 1-5 | 2.39 | (1.33) | 1-5 | 2.45 | (1.25) | 1-5 |
| Acceptance | 12.24 | (2.96) | 4-16 | 11.82 | (2.96) | 4-16 | 11.93 | (3.02) | 4-16 |
| Positive reappraisal | 10.31 | (3.00) | 4-16 | 9.85 | (2.67) | 4-16 | 9.62 | (2.93) | 4-16 |
| Emotional expression | 4.05 | (1.43) | 2-8 | 3.97 | (1.27) | 2-8 | 3.78 | (1.33) | 2-8 |
| Emotional processing | 4.62 | (1.53) | 2-8 | 4.47 | (1.43) | 2-8 | 4.34 | (1.58) | 2-8 |
| Satisfaction with support from patient | 6.34 | (4.02) | 4-24 | 6.25 | (3.50) | 4-24 | 6.83 | (4.53) | 4-24 |
| Satisfaction with support from family and friends | 7.30 | (4.15) | 4-24 | 8.39 | (4.94) | 4-24 | 8.74 | (5.02) | 4-24 |
Note. MHI = Mental Health Inventory.
Scores at or above 20 on at least one of the IES subscales indicate a significant stress response that may warrant a PTSD diagnosis (Horowitz, 1982). At Time 1, 12.5% of partners scored at or above 20 on the IES intrusion subscale, 7.5% of partners scored at or above the same cutoff on the avoidance subscale, and 12.6% of the sample scored in this range on at least one of the subscales. At Time 2, 6% of partners scored at or above 20 on the IES intrusion subscale, 5.4% of partners scored at or above the same cutoff on the avoidance subscale, and 10.1% of the sample scored at or above this cutoff on one of the scales. At Time 3, 3.8% of partners scored at or above 20 on Intrusions, and 6.1% of the sample scored in this range on at least one of the subscales. We conducted comparisons of IES scores from the present study with a study using the IES in a sample of male spouses of cancer patients (Baider, Walach, Perry, & Kaplan De-Nour, 1998). Comparisons indicated that IES scores in the present sample were significantly lower at Time 1 than in the comparison sample (t (291) = 4.94, p < .05). However, it should be noted that the comparison sample was comprised of partners of patients with tumors with a poorer prognosis (e.g., stomach and colorectal cancers), which may have resulted in higher IES scores. Utilization of psychosocial care was low (see Table 1). Between 83% and 85% of partners did not seek any kind of psychosocial care at Time 1, 2, and 3.
Missing data
One hundred sixty seven partners completed the Time 2 survey (66%) and 149 partners completed the Time 3 survey (59%). Logistic regression was used from available Time 1 partner demographic, medical, and psychological data to predict missing data at Time 2. Results indicated that missing data at Time 2 were related to partner education (Wald chi square = 5.76; p = 0.0164). Less educated partners were more likely to have missing data at Time 2 (odds ratio = 0.840; C.I. 0.729, 0.969). There were no significant demographic, medical, or psychological variables that predicted missing data at Time 3.
Statistical Plan
The present study involved repeated measurements for both outcomes of interest (MHI distress and cancer-specific distress) as well as the predictors of these outcomes. Because of the repeated measures, the data in the present study possess a nested structure. The repeated measures represent what are called the Level 1 model and the repeated measures are nested under the research participants (the Level 2 model) and can be analyzed as a hierarchic linear or multilevel model (Raudenbush & Bryk, 2002).
In addition to the assessment of the average change in an outcome over time, multilevel or hierarchic models also provide for the possibility that, in addition to average change over time, there may be significant and potentially theoretically interesting individual differences around the average change trajectory (a growth curve model). This possibility was examined using the mixed linear model procedure implemented in the SAS procedure, MIXED.
There are two advantages associated with the use of a multilevel model for change. Aside from the ability to examine individual differences in trajectories of change over time, multilevel models employ maximum likelihood estimation of the parameters meaning that they can readily accommodate missing data in most situations (Singer & Willett, 2003). Thus, partners who did not complete one or both of the follow-ups were included if they completed the Time 1 survey.
If there is no evidence of individual differences in change trajectories over time, the data may be analyzed as a mixed linear repeated measures model. In addition to being able to accommodate missing data on the outcomes, another of the advantages of the mixed linear model approach to repeated measures is that it offers a wider choice of error variance/covariance possibilities than does the traditional repeated measures procedure (Singer & Willet, 2003).
Since this was an observational study, participants were recruited at varying times after the patients’ initial diagnosis. As a consequence, the Time 1 variable was the time since diagnosis, the Time 2 variable was time since diagnosis plus 9 months, and the Time 3 variable was time since diagnosis plus 18 months.
We adopted a growth curve models approach to the data since we were interested in individual differences in the outcomes of interest as a function of time as a random variable. In the first step of the analyses, time was the only explanatory variable included in the models. In the second step, partner demographic, psychosocial care use, and patient medical variables were introduced. In the third step, the main effects for the hypothesized predictors were entered along with any significant demographic, psychosocial care use, and patient medical variables identified in the second step. All hypothesized predictors were added at Steps 2 and 3 and only those predictor effects that attained significance were retained. In the fourth step, the hypothesized moderator effects were entered into the equation and only those interactions that attained significance were retained. Since there were two outcomes of interest, the p-values were Sidak adjusted for the two correlated outcomes. For a two-tailed test, the critical t-value is 2.13 for a p value of 0.034.
We will organize the report of results around the hypotheses from the two models (main and moderator effects models). Analyses were conducted separately for each outcome variable. In our description of the results for the main effect models, we will initially present the first two steps of model building for each of the two outcomes (the effects for time and demographic and medical variables). This information will not be repeated when reporting the other main effects. Similarly, moderator effect model results will present only the interaction effects as the first three steps (effects for time, demographic and medical variables, and the predicted main effects) were already reported. In addition, the results for the moderators will be reported in a univariate format for each of the two outcomes. For example, in the model for cancer-specific distress, it was hypothesized that there would be an interaction between searching for and finding meaning. This model would contain the time main effect, any significant demographic/medical predictors, the main effects of searching for and finding meaning, and the interaction involving these two main effects. Table 3 summarizes the results for global MHI distress in a model that contained all the significant main effects and all the significant univariate moderator effects. Table 4 similarly presents the results for cancer-specific distress. Only significant effects are reported.
Table 3.
Growth Curve Model Results for Social and Cognitive Processes Predicting Partner Global MHI Distress
| Effect | Parameter Estimate | Confidence Interval | df | t-value | Probability |
|---|---|---|---|---|---|
| Intercept | 22.62 | 20.02 - 25.21 | 203 | 17.20 | <0.01 |
| Time | -0.05 | -0.10 - 0.01 | 195 | -1.51 | 0.13 |
| Partner age | -0.13 | -0.20 - -0.07 | 203 | -4.19 | <0.01 |
| Patient self-reported physical impairment | 0.06 | 0.02 - 0.10 | 195 | 3.25 | <0.01 |
| Psychosocial Care Use | 3.44 | 1.82 - 5.06 | 195 | 4.18 | <0.01 |
| Satisfaction with support from the patient | -0.13 | -0.25 - 0.01 | 195 | -1.89 | 0.06 |
| Searching for meaning | 0.62 | 0.16 - 1.07 | 195 | 2.68 | <0.01 |
| Finding meaning | -0.61 | -1.03 - -0.18 | 195 | -2.82 | <0.01 |
| Emotional expression | 0.11 | -0.29 - 0.50 | 195 | 0.54 | 0.59 |
| Positive reappraisal | -0.14 | -0.34 - 0.06 | 195 | -1.34 | 0.18 |
| Emotional expression X Positive reappraisal | -0.15 | -0.25 - -0.06 | 195 | -3.12 | 0.01 |
Table 4.
Growth Curve Model Results of Cognitive and Social Processes Predicting Cancer-specific Distress
| Effect | Parameter Estimate | Confidence Interval | df | t-value | Probability |
|---|---|---|---|---|---|
| Intercept | 18.80 | 16.66 - 20.94 | 207 | 17.31 | <0.01 |
| Time | -0.16 | -0.29 - -0.04 | 206 | -2.51 | 0.01 |
| Partner age | -0.12 | -0.25 - 0.02 | 207 | -1.75 | 0.08 |
| Patient self-reported physical impairment | 0.10 | 0.02 - 0.17 | 206 | 2.43 | 0.02 |
| Psychosocial Care Use | 4.57 | 1.81 - 7.34 | 206 | 3.26 | <0.01 |
| Searching for Meaning | 2.28 | 1.27 - 3.29 | 206 | 4.43 | <0.01 |
| Finding Meaning | -0.35 | -1.29 - 0.60 | 206 | -0.73 | 0.47 |
| Acceptance | -0.14 | -0.56 - 0.27 | 206 | -0.68 | 0.50 |
| Emotional Processing | 1.28 | 0.56 - 1.99 | 206 | 3.52 | <0.01 |
| Acceptance X Emotional Processing | -0.36 | -0.53 - -0.18 | 206 | -4.06 | <0.001 |
| Search for Meaning X Finding Meaning | -0.69 | -1.25 - -0.12 | 206 | 1.84 | 0.02 |
Table 2 summarizes correlations among the predictor variables at Time 1.
Table 2.
Correlations between Predictor Variables included in the Model at Time 1
| Predictor | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. Searching for meaning | .51*** | -.08 | .38*** | .22** | .32*** | .08 | .09 | |
| 2. Finding meaning | .03 | .38*** | .05 | .16* | .08 | -.04 | ||
| 3. Acceptance | .35*** | .14 | .25** | .05 | -.02 | |||
| 4. Positive reappraisal | .36*** | .47*** | -.02 | -.06 | ||||
| 5. Emotional expression | .47*** | .05 | .07 | |||||
| 6. Emotional processing | .09 | .01 | ||||||
| 7. Satisfaction with support from patient | .74*** | |||||||
| 8. Satisfaction with support from family and friends |
p < .05
p < .01
p < .001
Main Effects Models
Positive reappraisal
In the initial model predicting MHI distress, there were no indications of individual differences in the slopes relating time to MHI distress. As a consequence, a mixed linear model repeated measures analysis of variance was conducted in which the focus was on the fixed effects of the predictor variables. The Akaike Information Criterion (AIC) indicated that a heterogenous compound symmetric error variance/covariance matrix fit the data best. In the first step evaluating the effect of time, there was a significant (t (263) = -3.35; p = 0.0009) decline in partner distress over the assessment period. In the second step evaluating the effects of demographic, psychosocial care use, and patient medical variables, partner age was a significant predictor of distress (t (211) = -4.77; p < 0.0001) as was the patient’s self-reported functional impairment (CARES) (t (219) = 3.64; p = 0.0003) and the partner’s use of psychosocial services (t (219) = 3.96; p = 0.0001). Younger partners were significantly more distressed. Increases in patient self-reported physical impairment averaged over time was associated with greater partner distress as was the greater use of psychosocial services by the partners. In the third step evaluating the proposed psychological variables, after controlling for time, demographic, psychosocial care, and patient medical variables, positive reappraisal was not a significant predictor of MHI distress.
In the initial model predicting cancer-specific distress, there were again no individual differences in the rates of change in IES over time. Thus, a mixed linear models repeated measures analysis of variance with a compound symmetric error variance/covariance matrix fit the data best using the AIC criterion and the results focus on the fixed effects of the predictors. In the first step evaluating the effects of time, there was a significant decrease in partner cancer-specific distress over time (t (265) = -5.51; p = < 0.0001). In the second step evaluating the effects of demographic, psychosocial care use, and medical variables, results indicated effects for age, use of psychosocial care, and patient physical functioning. Younger partners reported significantly higher cancer-specific distress (t (212) = -2.83; p = 0.0052). Increases in the patient’s average physical functioning (CARES) were associated with higher average cancer-specific distress (t (220) = 3.02; p = 0.0028) as was greater partner use of psychosocial care (t (220) = 3.16; p = 0.0018). In the third step, positive reappraisal was a significant predictor of cancer-specific distress but in a direction opposite to prediction (t (215) = 2.76; p = 0.0063.
Acceptance
Acceptance was not a significant predictor of either MHI distress or cancer-specific distress.
Satisfaction with partner and family and friend support
Greater satisfaction with partner support was a significant predictor of decreased partner MHI distress (t (204) = -2.38; p = 0.0183) while satisfaction with support from family and friends was not a significant predictor of distress. Neither satisfaction with support from the partner nor from friends was a significant predictor of cancer-specific distress.
Moderator Effects Models: Univariate Results
Finding meaning and searching for meaning
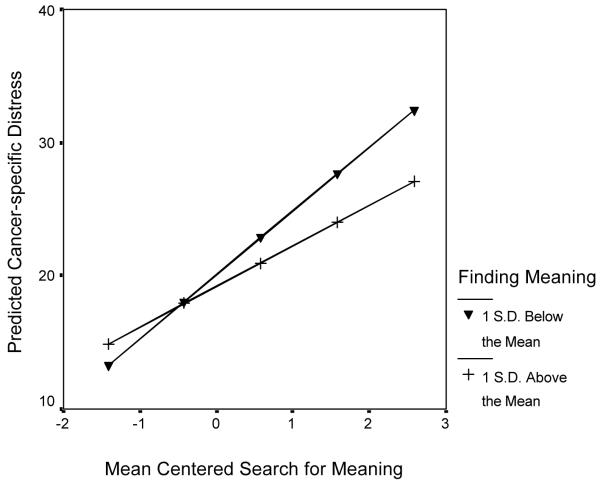
There were no univariate moderator effects for found meaning on the association between searching for meaning and partner global MHI distress. In the univariate model predicting cancer-specific distress, there was a marginally significant moderator effect of finding meaning by searching for meaning on cancer-specific distress (t (214) = -2.06; p = 0.04). As can be seen in Figure 1, following procedures described by Aiken and West (1991), at one standard deviation (S.D.) above the mean on finding meaning, increased reports of searching for meaning were significantly (b = 3.05; t (214) = 4.79; p < 0.001) associated with increased cancer-specific distress. At one S.D. below the mean, increased reports of searching for meaning were also associated with increased cancer-specific distress (b = 4.80; t (214) = 3.91; p < 0.0001), but the slope was significantly more positive.
Figure 1.
Graph depicting the interaction between searching for meaning and finding meaning predicting partner’s cancer-specific distress
Moderator effects for emotional processing
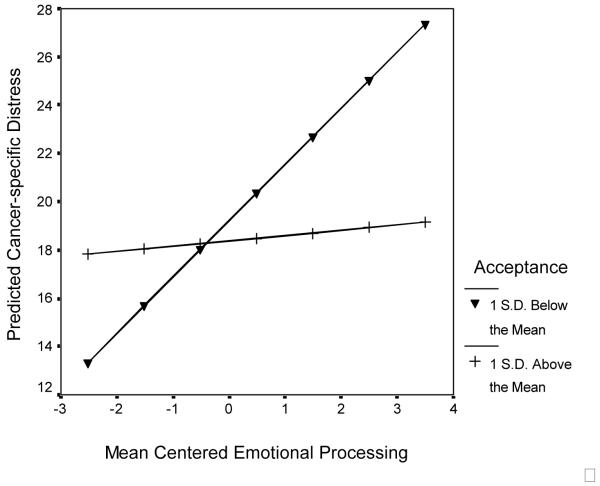
In the univariate model for cancer-specific distress, there was a significant (t (212) = -3.93; p = 0.0001) interaction between emotional processing and acceptance. Following procedures described by Aiken and West (1991), at 1 S.D. above the mean on acceptance, emotional processing was associated with a non-significant (t (212) 1.14; p = 0.2574) increase in cancer specific distress as can be seen in Figure 2. Essentially, emotional processing had no effect on cancer-specific distress. At 1 S.D. below the mean on acceptance, however, emotional processing was associated with a significant (t (212) = 6.30; p <0.0001) increase in cancer-specific distress (Figure 2).
Figure 2.
Graph depicting the interaction between emotional processing and acceptance predicting partner cancer-specific distress
The interaction between emotional processing and acceptance was not a significant predictor of global MHI distress. In addition, the moderating effect of positive reappraisal on emotional processing was not found for either global MHI distress or cancer-specific distress.
Moderator effects for emotional expression
In the univariate model predicting cancer-specific distress, acceptance moderated the effects of emotional expression (t (212) = -2.52; p = 0.0125). In the analysis of this interaction, at 1 S.D. above the mean on acceptance, changes in emotional expression were not a significant predictor of cancer-specific distress (t (212) = 0.21; p = 0.8311). At 1 S.D. below the mean on acceptance, increased emotional expression was associated with a significant increase in cancer-specific distress (t (212) = 3.79; p = 0.0002). The interaction of emotional expression by acceptance was not a significant predictor of MHI distress.
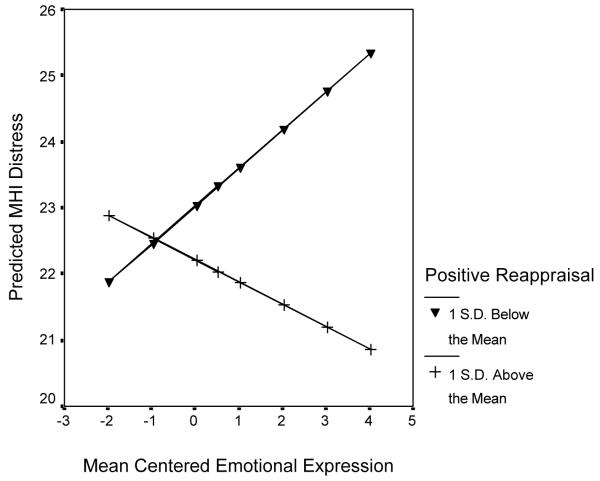
There was a significant univariate moderator effect of emotional expression by positive reappraisal on global MHI distress (t (195) = -3.12; p = 0.0010). As can be seen in Figure 3, at 1 S.D. above the mean on positive reappraisal, increased emotional expression was associated with lower MHI distress but the slope was not significantly different from zero (t (195) = -1.62; p = 0.1067). At 1 S.D. below the mean on positive reappraisal, higher scores on emotional expression were associated with significantly greater MHI distress (t (195) = 1.99; p = 0.0478). The interaction of emotional expression by positive reappraisal was not a significant predictor of cancer-specific distress.
Figure 3.
Graph depicting the interaction between emotional expression and positive reappraisal predicting partner global distress
Moderator Effects Combined Models
Table 3 summarizes the results for the combined moderator model predicting global MHI distress. The interaction between emotional expression and positive reappraisal described above was the only moderator variable that continued to be a significant predictor. Table 4 summarizes the results for the combined model predicting cancer-specific distress. The interaction of emotional processing and acceptance continued to be significant. However, the interaction of emotional expression by acceptance found in the univariate analysis was no longer significant. In addition, the marginally significant interaction between finding and searching for meaning described earlier was now clearly significant (t (206) = -2.38, p = .0182) in the context of the interaction between acceptance and emotional processing.
Discussion
This study explored the role of cognitive processing and social modulation of cognitive processing in predicting the 18-month course of psychological distress among partners of women diagnosed with early stage breast cancer. We proposed that four processing variables would have direct influences on partner psychological distress and that the predictive associations of three processing variables on partner outcomes would depend upon their success in altering partner appraisals of the cancer experience. Our findings were largely not consistent with the direct effect predictions. The only direct association between these processes and partner outcomes that was consistent with our hypotheses was that greater satisfaction with social support provided by the patient was predictive of less partner global distress over time. With regard to moderating effects, our results were somewhat consistent with the hypothesis that the effects of cognitive processing and social modulation of cognitive processing would depend upon their success in altering partners’ perspectives about the cancer experience.
With regard to main effect models, our finding that partners who reported higher levels of satisfaction with support provided by the patient reported less global distress is consistent with prior research on partners of patients with breast cancer (Manne et al., 2007) and partners of patients diagnosed with other types of cancer (Banthia et al., 2003), as well as research on the role of support from the ill partner in the healthy partner’s adaptation (Kuijer, Buunk, DeJong, Ybema, & Sanderman, 2004). These results suggest that the quality of the marital relationship is important to spouses. Satisfaction with support from family and friends was not predictive of partner distress which suggested that support provided by the marital relationship may play a more important role in partner distress during and following cancer diagnosis than support from family and friends. However, it should be noted that the correlation between satisfaction with support from the partner and satisfaction with support from family and friends were highly correlated (r =.60) and thus multicollinearity may have reduced the impact of support from family and friends.
Our results suggesting that positive reappraisal and acceptance were not predictive of less partner global distress or cancer-specific distress were surprising, as these findings contrast with cross-sectional associations reported in previous studies (Eton, 2005) as well as studies examining the role of cognitive processes in patients’ adjustment to cancer (e.g., Carver, Lehman, & Antoni, 2003). In fact, greater use of positive reappraisal was associated with greater cancer-specific distress, rather than less distress. There are at least two potential explanations for these findings. First, it is possible that, when considered longitudinally rather than cross-sectionally, reappraisal and acceptance do not have the same associations. Second, acceptance and positive reappraisal are related to the constructs of benefit-finding and post-traumatic growth (PTG)(Helgeson, Reynolds & Tomich, 2006). Recent findings have suggested that benefit-finding (Tomich & Helgeson, 2004) and PTG (Hobfoll et al., 2007) can lead to higher levels of cancer-related distress among patients. Recent meta-analyses of the effects of benefit-finding and psychological outcomes have suggested that benefit-finding has different associations with different psychosocial outcomes (Helgeson, Reynolds, & Tomich, 2006). The associations between reappraisal and acceptance and psychological outcomes among partners may be similarly complex.
One of the basic tenets of cognitive-social processing theory is that the success of cognitive processing depends on whether these efforts result in a shift in the person’s perspective on the cancer experience. We evaluated this hypothesis by evaluating whether attempts at processing (searching for meaning, emotional processing, and emotional expression) resulted in meaning making, positive reappraisal, and acceptance. The pattern of results was partially supportive of this prediction. First, the positive association between searching for meaning and cancer-specific distress was marginally stronger among partners who did not report finding as much meaning in the patient’s cancer compared with partners who reported that their search for meaning resulted in found meaning (although the association became statistically significant when the interaction between acceptance and emotional processing was entered into the equation). Second, at high levels of acceptance, partners’ attempts to understand their emotions were not related to changes in cancer-specific distress, while at low levels of acceptance, partner attempts to understand their emotions were associated with a significant increase in cancer-specific distress. Third, at low levels of acceptance, increased emotional expression was associated with an increase in cancer-specific distress, whereas at high levels of acceptance, changes in emotional expression were not a significant predictor of cancer-specific distress. Fourth, at high levels of positive reappraisal, increases in emotional expression were associated with lower global distress (the change was not significant), but at low levels of positive reappraisal, high levels of emotional expression were associated with significantly greater global distress. These moderator effects suggest that main effect models may not fully capture the complexity of cognitive processing and social modulation of cognitive processing. A successful resolution of searching for meaning, expressing feelings, and delving into the meaning of emotional reactions in terms of changing views and appraisals of the cancer experience may be important. Future research should evaluate other social modulation mechanisms that may account for these associations. For example, emotional processing and expression may be more likely to result in positive reappraisal and/or acceptance if the members of the social network respond in facilitative ways (i.e., encouraging the adoption of different perspectives).
Despite our findings supporting the moderator effect models, it is important to note that only four of the ten proposed interactions (five interactions and two dependent variables) were significant. The interactions between searching for and finding meaning did not predict global distress, the interaction between emotional processing and positive reappraisal did not predict either outcome, the interaction between emotional processing and acceptance did not predict global distress, the interaction between emotional expression and acceptance did not predict global distress, and the interaction between emotional expression and positive reappraisal did not predict cancer-specific distress. One finding (the interaction between emotional processing and acceptance predicting global distress) was no longer significant when all moderator effects were included in the final model. In summary, although our findings were partially consistent with the moderator effects model, our findings were not completely consistent across all psychological outcomes.
There are a number of limitations of this study. The 37% participation rate is lower than figures reported in other research focusing on spouses of cancer patients e.g., (Northouse, Dorris, & Charron-Moore, 1995). It is important to point out that the participation rate was reasonable given the requirement that both partners to participate and complete three surveys over a one and a half year time period. Nevertheless, this participation rate may have resulted in a non-representative sample of partners and limit generalizability of the findings. Indeed, partner participants were married to patients who were younger and therefore our findings may not generalize to older partners. We do not know in what other ways our sample of partners was biased because we were not able to collect data on the characteristics of partners who refused. Second, the study retention rate at the two follow-up time points was relatively low (68% at Time 2, 59% at Time 3). Although the statistical techniques that were used can address missing dependent variable data, they could not handle missing data on the predictor variables. Therefore, the study retention rate may have biased the results of this study. Third, the minority representation was low and it is unclear how our findings would generalize to minority partners. Fourth, there were several measurement issues. We used single-item measures of searching for and finding meaning, and the emotional processing and emotional expression scales were comprised of only two items. The support satisfaction scale was composed specifically for the present study and therefore has unknown validity. These issues may limit the conclusions made about these constructs. Fifth, the vast majority of partners were male. It is possible that female partners may process cancer differently particularly with regard to emotional expression and emotional processing.
The present findings have theoretical, research, and clinical implications. Our findings did not provide overwhelming support for the cognitive processing model. It is possible that other theoretical models may be more appropriate for understanding spousal adaptation to cancer. For example, among partners, the relationship with the ill partner, particularly how the couple communicates about the illness, may play a stronger role in partner adaptation than cognitive processing. Therefore, it may be important for future research on partners to include on relationship process models (Manne & Badr, in press). In terms of future research, it would be interesting to better understand the interplay between spouse support, emotional expression, and emotional processing and changes in appraisals of the ill partner’s cancer. Why does expressing and delving into feelings result in changes in views for some partners but not for others? How do the responses of friends and family influence whether partners’ emotional expression and efforts to understand the cancer experience result in positive reappraisal or acceptance? Future research would benefit from understanding the interplay of different cognitive adaptation processes. In terms of clinical implications, our results indicate that levels of psychological distress are relatively low among partners, with global distress levels lower than the general population and cancer-specific distress levels lower than samples of partners of women with other types of cancer. Moreover, distress declined for partners over time, and few partners sought out psychosocial care on their own. These findings suggest that the majority of partners of early stage breast cancer survivors are not at risk for adverse psychological outcomes. However, a small subset of partners report persistent and significant cancer-related distress over time which suggests that some partners may require professional assistance. Our results suggest that it may be beneficial to facilitate adaptive cognitive processing, particularly among partners whose attempts to find meaning in the cancer experience do not result in meaning-making or attempts to express and understand their emotional reactions do not result in changed perspectives on the cancer experience. Overall, these results underscore the complex interplay between cognitive processes and suggest that moderator effect models may be a valuable supplement to main effect approaches in understanding the role of these processes in adaptation to cancer.
Acknowledgments
This work was supported by grant # 78084 from the National Institutes of Health.
Contributor Information
Sharon Manne, Psycho-Oncology Program, Fox Chase Cancer Center, Philadelphia, PA.
Jamie Ostroff, Department of Psychiatry and Behavioral Sciences, Memorial Sloan-Kettering Cancer Center, New York, NY.
Kevin Fox, Department of Hematology-Oncology, Hospital of the University of Pennsylvania, Philadelphia, PA.
Generosa Grana, Breast Cancer Program, Cooper Hospital, Voorhees, New Jersey.
Gary Winkel, Department of Psychology, City University of New York, New York, NY.
REFERENCES
- Aiken LD, West SG. Multiple Regression: Testing and interpreting interactions. Sage Publications; Newbury Park, CA: 1991. [Google Scholar]
- Baider L, Walach N, Perry S, Kaplan De-Nour A. Cancer in married couples: Higher or lower distress? Journal of Psychosomatic Research. 1998;45(3):239–248. doi: 10.1016/s0022-3999(98)00016-6. [DOI] [PubMed] [Google Scholar]
- Banthia R, Malcarne VL, Varni JW, Ko CM, Sadler GR, Greenbergs HL. The effects of dyadic strength and coping styles on psychological distress in couples faced with prostate cancer. Journal of Behavioral Medicine. 2003;26(1):31–52. doi: 10.1023/a:1021743005541. [DOI] [PubMed] [Google Scholar]
- Caplan G. Support Systems and Community Mental Health: Lectures on Concept Development. Behavioral Publications; New York: 1974. [Google Scholar]
- Carver CS, Lehman JM, Antoni MH. Dispositional pessimism predicts illness-related disruption of social and recreational activities among breast cancer patients. Journal of Personality and Social Psychology. 2003;84(4):813–821. doi: 10.1037/0022-3514.84.4.813. [DOI] [PubMed] [Google Scholar]
- Carver CS, Pozo C, Harris SD, Noriega V, Scheier MF, Robinson D, et al. How Coping Mediates the Effect of Optimism on Distress: A Study of Women With Early Stage Breast Cancer. Journal of Personality and Social Psychology. 1993;65(2):375–390. doi: 10.1037//0022-3514.65.2.375. [DOI] [PubMed] [Google Scholar]
- Coates D, Wortman CB, Abbey A. Reactions to victims. In: Frieze IH, Bar-Tal D, Carroll JS, editors. New approaches to Social Problems. Jossey-Bass; San Francisco, CA: 1979. pp. 21–52. [Google Scholar]
- Epstein S. The self-concept, the traumatic neurosis and the structure of personality. In: Ozer D, Healy JN, Stewart AJ, editors. Perspectives on Personality. JAI press; Greenwich, CT: 1991. [Google Scholar]
- Eton DT. Psychological distress in spouses of men treated for early-stage prostate carcinoma. Cancer. 2005;103(11):2412–2418. doi: 10.1002/cncr.21092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Given CW, Given B, Osuch J, Stommel M, Kurtz ME, Kurtz JC. The Influence of Cancer Patients’ Symptoms and Functional States on Patients’ Depression and Family Caregivers’ Reaction and Depression. Health Psychology. 1993;12(4):277–285. doi: 10.1037//0278-6133.12.4.277. [DOI] [PubMed] [Google Scholar]
- Gottlieb BH. The development and application of a classification scheme of informal helping behaviors. Canadian Journal of Behavioral Science. 1978;10:105–115. [Google Scholar]
- Helgeson VS, Reynolds KA, Tomich PL. A meta-analytic review of benefit finding and growth. Journal of Consulting and Clinical Psychology. 2006;74(5):797–816. doi: 10.1037/0022-006X.74.5.797. [DOI] [PubMed] [Google Scholar]
- Helgeson V, Snyder P, Seltman H. Psychological and physical adjustment to breast cancer over 4 years: identifying distinct trajectories of change. Health Psychology. 2004;23(1):3–15. doi: 10.1037/0278-6133.23.1.3. [DOI] [PubMed] [Google Scholar]
- Hobfall S, Hall B, Nisim D, Galea S, Johnson R, Palmieri P. Refining our understanding of traumatic growth in the face of terrorism: Moving from meaning cognitions to doing what is meaningful. Applied Psychology: An international review. 2007;56:345–366. [Google Scholar]
- Horowitz MJ. Stress Response Syndromes. 2nd ed Jason Aronson Press; Northvale, NJ: 1986. [Google Scholar]
- Horowitz MJ. Stress response syndromes and their treatment. In: Goldberger L, Breznitz S, editors. Handbook of Stress: Theoretical and Clinical Aspects. Free Press; New York: 1982. pp. 711–732. [Google Scholar]
- Horowitz M, Wilner N, Alvarez W. Impact of event scale: A measure of subjective stress. Psychosomatic Medicine. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Janoff-Bulman R. Rebuilding shattered assumptions after traumatic events: Coping processes and outcomes. In: Snyder CR, editor. Coping: The Psychology of What Works. Oxford University Press; NY: 1999. [Google Scholar]
- Keitel MA, Zevon MA, Rounds JB, Petrelli NJ, Karakousis C. Spouse adjustment to cancer surgery: Distress and coping responses. Journal of Surgical Oncology. 1990;43:148–153. doi: 10.1002/jso.2930430305. [DOI] [PubMed] [Google Scholar]
- Kuijer RG, Buunk BP, DeJong GM, Ybema JF, Sanderman R. Effects of a brief intervention program for patients with cancer and their partners on feelings of inequity, relationship quality and psychological distress. Psycho-Oncology. 2004;13:321–334. doi: 10.1002/pon.749. [DOI] [PubMed] [Google Scholar]
- Lepore SJ. A social-cognitive processing model of emotional adjustment to cancer. In: Baum A, editor. Psychosocial interventions for cancer. APA; Washington, D.C.: 2001. pp. 99–118. A. B. [Google Scholar]
- Maguire P. The psychological impact of cancer. British Journal of Hospital Medicine. 1985;34:100–103. [PubMed] [Google Scholar]
- Makabe R, Nomizu T. Social support and psychological and physical states among Japanese patients with breast cancer and their spouses prior to surgery. Oncology Nursing Forum. 2006;33(3):651–655. doi: 10.1188/06.ONF.651-655. [DOI] [PubMed] [Google Scholar]
- Manne S, Alfieri T, Taylor K, Dougherty J. Spousal negative responses to cancer patients: The role of social restriction, spouse mood and relationship satisfaction. Journal of Consulting and Clinical Psychology. 1999;67(3):352–361. doi: 10.1037//0022-006x.67.3.352. [DOI] [PubMed] [Google Scholar]
- Manne S, Badr H. Intimacy and Relationship Processes in Couples’ Psychosocial Adaptation. Cancer. doi: 10.1002/cncr.23450. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne S, Norton T, Ostroff J, Winkel G, Fox K, Grana G. Protective buffering and psychological distress among couples coping with breast cancer; The moderating role or relationship satisfaction. Journal of Family Psychology. 2007;21:380–388. doi: 10.1037/0893-3200.21.3.380. [DOI] [PubMed] [Google Scholar]
- Manne S, Ostroff J, Norton T, Fox K, Goldstein L, Grana G. Cancer-related relationship communication in couples coping with early stage breast cancer. Psycho-Oncology. 2006;13(3):234–247. doi: 10.1002/pon.941. [DOI] [PubMed] [Google Scholar]
- Manne S, Ostroff J, Rini C, Fox K, Goldstein L, Grana G. The interpersonal process model of intimacy: The role of self-disclosure, partner disclosure and partner responsiveness in interactions between breast cancer patients and their partners. Journal of Family Psychology. 2004;18:589–599. doi: 10.1037/0893-3200.18.4.589. [DOI] [PubMed] [Google Scholar]
- Manne S, Ostroff J, Sherman M, Heyman R, Ross S, Fox K. Couples’ support-related communication, psychological distress and relationship satisfaction among women with early stage breast cancer. Journal of Consulting and Clinical Psychology. 2004;72(4):660–670. doi: 10.1037/0022-006X.72.4.660. [DOI] [PubMed] [Google Scholar]
- Manne S, Ostroff J, Winkel G, Goldstein L, Fox K, Grana G. Posttraumatic growth after breast cancer: Patient, partner, and couple perspectives. Psychosomatic Medicine. 2004;66:442–454. doi: 10.1097/01.psy.0000127689.38525.7d. [DOI] [PubMed] [Google Scholar]
- Manne S, Ostroff J, Winkel G, Grana G, Fox K. Partner Unsupportive Responses, Avoidance and Distress among Women with Early Stage Breast Cancer: Patient and Partner Perspectives. Health Psychology. 2005;24(6):635–641. doi: 10.1037/0278-6133.24.6.635. [DOI] [PubMed] [Google Scholar]
- Manne S, Schnoll R. Measuring cancer patients’ psychological distress and well-being: A factor analytic assessment of the Mental Health Inventory (MHI) Psychological Assessment. 2001;13(1):99–109. [PubMed] [Google Scholar]
- Markarian Y, Rini C, Manne S, DuHamel KN, Austin J, Ostroff J, Boulad F, Parsons S, Martini R, Williams S, Mee L, Sexson S, Redd WH. Making Sense of Trauma: The Search for Meaning after Pediatric Bone Marrow Transplantation and Its Impact on Maternal Adjustment; Poster presented at the American Psychological Society’s 18th Annual Meeting; New York, NY. March, 2006. [Google Scholar]
- Northouse LL. Social support in patients’ and husbands’ adjustment to breast cancer. Nursing Research. 1988;37(2):91–95. [PubMed] [Google Scholar]
- Northouse LL, Dorris G, Charron-Moore C. Factors affecting couples’ adjustment to recurrent breast cancer. Social Science and Medicine. 1995;41(1):69–76. doi: 10.1016/0277-9536(94)00302-a. [DOI] [PubMed] [Google Scholar]
- Northouse L, Templin T, Mood D. Couples’ adjustment to breast disease during the first year following diagnosis. Journal of Behavioral Medicine. 2001;24(2):115–136. doi: 10.1023/a:1010772913717. [DOI] [PubMed] [Google Scholar]
- Omne-Ponten M, Holmberg L, Bergstrom R, Sjoden PO, Burns T. Psychosocial adjustment among husbands of women treated for breast cancer; mastectomy vs. breast-conserving surgery. European Journal of Cancer. 1993;29A(10):1393–1397. doi: 10.1016/0959-8049(93)90009-5. [DOI] [PubMed] [Google Scholar]
- Pennebaker JW. Confession, inhibition, and disease. In: Berkowitz L, editor. Advances in Experimental Social Psychology. Vol. 22. Academic Press; Orlando, FL: 1989. pp. 211–244. [Google Scholar]
- Raudenbush R, Bryk A. Hierarchical linear models: Applications and data analysis methods. 2nd ed Sage publications; Thousand Oaks, Ca: 2002. [Google Scholar]
- Rime B, Mesquita B, Philippot P, Boca S. Beyond the emotional event: Six studies on the social sharing of emotion. Cognition and Emotion. 1991;5:435–465. [Google Scholar]
- Rime B, Philippot T, Boca S, Mesquita B. Long-lasting cognitive and social consequences of emotion: Social sharing and rumination. European Review of Social Psychology. 1992;3:225–258. [Google Scholar]
- Sears SR, Stanton AL, Danoff-Burg S. The yellow brick road and the emerald city: Benefit finding, positive reappraisal coping, and posttraumatic growth in women with early-stage breast cancer. Health Psychology. 2003;22(5):487–497. doi: 10.1037/0278-6133.22.5.487. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. Oxford; New York: 2003. [Google Scholar]
- Stanton A, Danoff-Burg S, Cameron C, Bishop D, Collins C, Kirk S, et al. Emotionally expressive coping predicts psychological and physical adjustment to breast cancer. Journal of Consulting & Clinical Psychology. 2000;68(5):875–882. [PubMed] [Google Scholar]
- Stewart A, Sherbourne D, Hays R. Summary and discussion of MOS measures. In: Stewart AL, Ware JE, editors. Measuring Function and Well-Being: The Medical Outcome Studies Approach. Duke University Press; Durham, NC: 1992. pp. 345–371. [Google Scholar]
- Tomich P, Helgeson V. Is finding something good in the bad always good? Benefit finding among women with breast cancer. Health Psychology. 2004;23:16–23. doi: 10.1037/0278-6133.23.1.16. [DOI] [PubMed] [Google Scholar]
- Wagner CD, Bigatt SM, Storniolo AM. Quality of life of husbands of women with breast cancer. Psycho-Oncology. 2006;15:109–120. doi: 10.1002/pon.928. [DOI] [PubMed] [Google Scholar]
- Ware JE, Manning WG, Duan N, Wells KB, Newhouse JP. Health status and the use of outpatient mental health services. American Psychologist. 1984;39(10):1090–1100. doi: 10.1037//0003-066x.39.10.1090. [DOI] [PubMed] [Google Scholar]
- Wu L, Bonnano G, Duhamel K, Redd WH, Rini C, Austin J, Nereo N, Ostroff J, Parsons S, Martini S, Williams S, Mee L, Sexson S, Manne S. Pre- Bereavement Meaning and Post-bereavement Distress in Mothers of children who underwent hematopoetic stem cell transplantation. British Journal of Health Psychology. doi: 10.1348/135910707X204236. in press. [DOI] [PubMed] [Google Scholar]