Abstract
Objective
To describe the technical feasibility and usefulness of extrahepatic biliary stone removal by balloon sphincteroplasty and occlusion balloon pushing.
Materials and Methods
Fifteen patients with extrahepatic bile duct stones were included in this study. Endoscopic stone removal was not successful in 13 patients, and two patients refused the procedure due to endoscopy phobia. At first, all patients underwent percutaneous transhepatic biliary drainage (PTBD). A few days later, through the PTBD route, balloon assisted dilatation for common bile duct (CBD) sphincter was performed, and then the stones were pushed into the duodenum using an 11.5 mm occlusion balloon. Success rate, reason for failure, and complications associated with the procedure were evaluated.
Results
Eight patients had one stone, five patients had two stones, and two patients had more than five stones. The procedure was successful in 13 patients (13/15). In 12 of the patients, all stones were removed in the first trial. In one patient, residual stones were discovered on follow-up cholangiography, and were subsequently removed in the second trial. Technical failure occurred in two patients. Both of these patients had severely dilated CBD and multiple stones with various sizes. Ten patients complained of pain in the right upper quadrant and epigastrium of the abdomen immediately following the procedure, but there were no significant procedure-related complications such as bleeding or pancreatitis.
Conclusion
Percutaneous extrahepatic biliary stone removal by balloon sphincteroplasty and subsequent stone pushing with occlusion balloon is an effective, safe, and technically feasible procedure which can be used as an alternative method in patients when endoscopic extrahepatic biliary stone removal was not successful.
Keywords: Extrahepatic bile duct, calculi; Extrahepatic bile duct, stone extraction
Bile duct stones may be related to various clinical manifestations such as biliary colic, obstructive jaundice, cholangitis, and biliary sepsis. Medication is needed to relieve clinical symptoms and improve patients' clinical condition, although stone removal is necessary to completely remedy the condition. Various methods including surgical and non-surgical techniques have been used to remove bile duct stones. Among them, endoscopic sphincterotomy has been recognized as the primary modality to remove extrahepatic duct stones based on its effectiveness and overall comfort of the patients. Its usefulness has been confirmed in numerous studies (1, 2), and it is being adopted as the main modality in most centers.
Development of devices and techniques used in endoscopic sphincterotomy has improved the success rate of stone removal. However, the use endoscopic sphincterotomy may be difficult or impossible in some clinical situations, including previous operation of upper gastrointestinal (GI) tract, patients' intolerance or phobia for endoscopy, and anomaly of GI tract among others, which require alternative therapeutic modalities. As a surgical modality, peritoneoscopic biliary surgery has been widely used. It is very effective and relatively safe compared with conventional open surgery. However, general anesthesia is necessary to perform the surgery and the cost of the procedure is high. Another alternative, transhepatic stone removal using a Dormia basket has also been used. It is has been shown to be helpful, but a 12 to 16 F large diameter tract through the liver parenchyma is needed, and should be reserved until the tract is completely matured.
Gil et al. reported the effectiveness of balloon dilatation of the papilla and clearing CBD stones using occlusion balloon pushing (1). The study emphasized the procedure was safe as well as simple, and it could be used as an alternative to endoscopic sphincterotomy. Despite a relatively large number of patients in the study, indication of the procedure was not definitely described in the report. It seems that competition with endoscophic sphicterotomy is time-consuming and not reasonable. We believe the technique outlined by Gil is valuable in patients who cannot undergo endoscopic sphincterotomy.
In this study, we present our experience for applying balloon sphincteroplasty and occlusion balloon pushing to remove extrahepatic bile duct stones in patients who refused endoscopic sphicterotomy or when endoscopic sphicterotomy was not successful, and discuss its technical feasibility and usefulness.
MATERIALS AND METHODS
From 2002 to 2004, fifteen patients (10 male, 5 female, 54-89 years old, mean age: 69 years) who had refused endoscopic sphicterotomy or when endoscopic sphicterotomy was not successful, were referred from endoscopists. There were several reasons the endoscopic sphicterotomy was not successful. In six patients it was due to anatomical change caused by a previous operation, poor compliance in three patients, intolerance due to poor general condition in four patients, and two patients refused the procedure due to endoscopy phobia. All of the patients received prophylactic broad-spectrum antibiotics upon arrival at the hospital and following the procedure to prevent and manage cholangitis.
At first, PTBD was performed in all patients to relieve clinical symptoms and ensure hepatic tract for the procedure. For the convenience of the procedure, segment 6 intrahepatic duct (IHD) was primarily punctured in PTBD. However, the segment 3 duct in the left lobe was punctured in three patients with a normal diameter IHD in segment 6.
The procedure was performed 3-4 days after PTBD to ensure at least minimal tract maturation and subsidence of the present cholangitis. Prior to the procedure, cholangiography with diluted contrast material was performed to define the anatomy of the biliary tree and number, size, and location of the stones. Various analgesics were administered depending on the needs of each individual patient. The procedure started by exchanging the catheter over a 150 cm, 0.035 inch diameter guide wire (Radifocus Guide wire M; Terumo, Tokyo, Japan) with the tip located in the duodenum. Next, 8-9 French vascular introducer sheath (Radifocus; Terumo, Tokyo, Japan) with their distal tips were inserted in to the biliary tree. A 65 cm 5 F angled taper angiographic catheter (Radifocus Glidecath; Terumo, Tokyo, Japan) was introduced through the introducer sheath. Stiff type 0.035 inch guidewire with 260 cm of length (Radifocus Guide wire M; Terumo, Tokyo, Japan) was passed through the angiographic catheter and the catheter was then pulled out. A dilatation balloon catheter (Ultra-Thin Diamond; Boston Scientific, Medi-Tech, MA) was inserted over the stiff type guidewire and positioned across the papilla. The balloon was then inflated with diluted contrast material until the waist by papillary sphincter disappeared. Inflation was maintained for 30-60 sec and repeated two or three times in each patient. The diameter of the balloon ranged from 8 mm to 14 mm. The size of the dilatation balloon was determined by estimating the size of the largest extrahepatic bile duct stone, and did not exceed 14 mm in order to avoid possible rupture of the common bile duct.
After dilation, the balloon was carefully removed to avoid pulling the stones proximally into the intrahepatic tree, and exchanged for an 11.5 mm standard occlusion balloon catheter (Standard Occlusion Balloon Catheter; Boston Scientific, Medi-Tech, MA). The balloon was inflated with diluted contrast material proximal to the stones and advanced over the guidewire through the papilla and into the duodenum. This maneuver was repeated until the stone was evacuated completely from the extrahepatic bile duct. By controlling the volume of the balloon with the syringe, it was possible to modulate its size in the duct. If the patient suffered from pain during the procedure, it was helpful to administer about 10 cc of 2% lidocaine into the bile duct via the introducer sheath.
The evacuation of the bile duct stone was confirmed by observing filling defects in the contrast agent-filled duodenum. The procedures described above are illustrated in Fig. 1. The balloon and the introducer were then removed, and a 10 F drainage catheter was placed in the common bile duct. This catheter remained in place for 3-7 days to allow external drainage. Pancreatic enzyme study was performed routinely to evaluate the onset of acute pancreatitis. Before removing this catheter, cholangiography was obtained to determine if the biliary tree was free of stones and easy flow of contrast material into the duodenum was shown. We evaluated the success rate, reason for failure, and complications associated with the procedure.
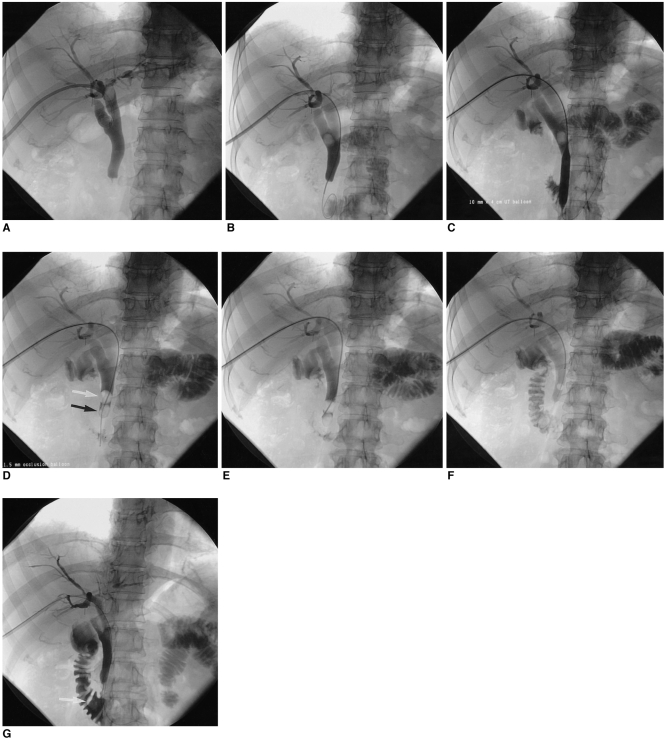
Fig. 1.
Fourty-three year-old female patient with a common bile duct stone and related right upper quadrant pain. This patient refused endoscopy, due to a terrible experience during a previous endoscopy (A) percutaneous transhepatic biliary drainage is performed, showing a stone in the common bile duct.
B. The stone is pushed more distally using a 5 F catheter, and 0.035 inch stiff wire is passed to the duodenum.
C. Using a 10 mm dilatation balloon, the ampullary sphincter is dilated.
D. 11.5 mm occlusion balloon (white arrow) is inserted into the common bile duct, just proximal to the stone (black arrow).
E. Using the occlusion balloon, the stone is pushed into the duodenum.
F. The stone is completely pushed into the duodenum.
G. The stone is shown in the duodenum (arrow).
RESULTS
Eight patients had one stone, five patients had two stones, and two patients had more than five stones. The procedure was successful in 13 patients (13/15). The size of the CBD in these patients was less than 15 mm and the size of the stones were 5-10 mm. In 12 patients, all stones were removed in the first trial. In one of the patients with one extrahepatic bile duct stone, another stone was not observed on cholangiography which was performed prior to and immediately after the the procedure. The hidden stone was completely removed in the second trial. Technical failure occurred in two patients. Both of them had severely dilated CBD measuring over 15 mm and multiple stones with the largest stone measuring less than 10 mm (Fig. 2). In two patients, additional stones other than the extrahepatic bile duct stones were located in the cystic duct and primary intrahepatic duct, which were pulled down to the extrahepatic bile duct using angle tapered angiographic catheter.
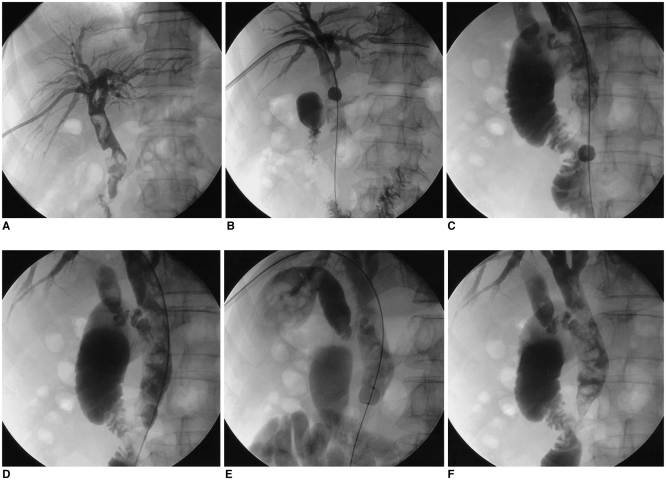
Fig. 2.
Fifty-six year-old male complaining of fever and right upper quadrant pain.
A. Multiple filling defects are seen in Common bile duct, indicating multiple stones. Common bile duct is severely dilated, measuring 16-17 mm in diameter.
B-D. Stone evacuation with occlusion balloon failed. The occlusion balloon passed over the stone, unable to push the stones effectively.
E. Even a larger sized balloon (13 mm), that is used for endoscopic common bile duct stone removal, fails in pushing the stones.
F. Multiple stones still remain in common bile duct.
All patients complained of sharp pain in the right upper abdomen during balloon dilatation of the sphincter. However, it subsided relatively quickly following balloon decompression. Ten patients complained of mild to moderate dull pain in the right upper abdomen following the procedure. This pain was controlled with analgesic agents and subsided within one or two days. There were no significant procedure-related complications such as bleeding, perforation or acute pancreatitis.
DISCUSSION
Endoscopic sphincterotomy has become the first line of treatment for patients with extrahepatic bile duct stones. However, this technique may not be successful due to difficult anatomy, previous surgery, periampullary diverticula, the presence of a large stone (3), or this technique may not be performed due to refusal by patients with endoscopy phobia. A comparison of endoscopic sphincterotomy and balloon sphincteroplasty has been reported in previous studies (4, 5). These studies indicated that endoscopic sphincterotomy was superior to endoscopic papillary balloon dilation based on stone removal, duration of the procedure, and complication rates. On the other hand, some studies have mentioned the advantages of percutaneous or endoscopic balloon sphincterotomy (2, 6, 7). These studies noted endoscopic balloon sphincterotomy was very safe, effective, and advantageous for the preservation of the papillary function. Generally, endoscopists believe that there is a higher risk for acute pancreatitis associated with balloon sphinteroplasty than endoscopic sphincterotomy. However, according to the results of the study by Gil et al. (1), acute pancreatitis was extremely rare, which is consistent with the results from this study. We did not experience any serious complications such as acute pancreatitis, hemobilia, or infection. Patients only complained of discomfort during the sphincteroplasty and following the procedure. However, it was well controlled by 2% lidocaine infusion into the bile duct and analgesics medications with non-steroid antiinflammatory drugs. No patient complained of pain for more than two days.
The technique described in this study also has advantages over percutenous extrahepatic biliary stone removal technique using a Dormia basket. As Burhenne et al. reported, Dormia baskets have high success rates and low complication rates (8). The success rate has been shown to be 95%, and complication rates have been reported to be around 4% (8-11). However, the Dormia basket method requires a larger tract diameter, and it should be reserved for at least 4-6 weeks for maturation of the transhepatic tract (8, 9, 12-15). Our technique requires only 3-4 days after PTBD, which can reduce hospitalization period. For the tract diameter, our technique needed only an 8-9 F sheath passing to perform the procedure.
In the present study the success rate in initial trial was very high. Only one patient underwent two sessions of the procedure to eliminate all the extrahepatic bile duct stones. Technical failure occurred in two patients due to multiple stones and severely dilated common bile duct measuring approximately 15 mm. An 11.5 mm occlusion balloon could not fully cover the diameter of the dilated common bile duct to push the stones and it slipped over the stones without effective stone pushing. We repeatedly tried pushing the stones with a larger 13 mm balloon used in endoscopic extraction of CBD stones, although it was still not successful after more than ten attempts during the trial.
A limitation of this study was that all the subjects had extrahepatic biliary stones measuring less than 10 mm. Consequently, the successful results demonstrated in this study may not always be duplicated, especially in patients with larger extrahepatic biliary stones. We only used 11.5-13 mm occlusion balloons for stone extraction because we dilated the papilla with dilatation balloon from 8 mm to 14 mm. We did not attempt stone extraction with larger sized occlusion balloons in the two patients with extremely dilated common bile ducts, and in which the procedure was not successful that reason. A more aggressive approach may have lead to successful stone extraction in these cases.
Even though endoscopic sphincterotomy is preferred in extrahepatic duct stone removal in most centers, alternative methods are necessary in various clinical situations. The results of this study show that balloon sphincteroplasty with occlusion balloon pushing is a very safe and effective treatment modality to remove extrahepatic duct stones, and it can be used in patients with anatomical or clinical difficulties for endoscopic sphincterotomy as an excellent alternative modality.
References
- 1.Gil S, de la Iglesia P, Verdu JF, de Espana F, Arenas J, Irurzun J. Effectiveness and safety of balloon dilation of the papilla and the use of an occlusion balloon for clearance of bile duct calculi. AJR Am J Roentgenol. 2000;174:1455–1460. doi: 10.2214/ajr.174.5.1741455. [DOI] [PubMed] [Google Scholar]
- 2.Garcia-Vila JH, Redondo-Ibanez M, Diaz-Ramon C. Balloon sphincteroplasty and transpapillary elimination of bile duct stones: 10 years' experience. AJR Am J Roentgenol. 2004;182:1451–1458. doi: 10.2214/ajr.182.6.1821451. [DOI] [PubMed] [Google Scholar]
- 3.Lauri A, Horton RC, Davidson BR, Burroughs AK, Dooley JS. Endoscopic extraction of bile duct stones: management related to stone size. Gut. 1993;34:1718–1721. doi: 10.1136/gut.34.12.1718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Binmoeller KF, Schafer TW. Endoscopic management of bile duct stones. J Clin Gastroenterol. 2001;32:106–118. doi: 10.1097/00004836-200102000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Arnold JC, Benz C, Martin WR, Adamek HE, Riemann JF. Endoscopic papillary balloon dilation vs. sphincterotomy for removal of common bile duct stones: a prospective randomized pilot study. Endoscopy. 2001;33:563–567. doi: 10.1055/s-2001-15307. [DOI] [PubMed] [Google Scholar]
- 6.Garcia-Garcia L, Lanciego C. Percutaneous treatment of biliary stones: sphincteroplasty and occlusion balloon for the clearance of bile duct calculi. AJR Am J Roentgenol. 2004;182:663–670. doi: 10.2214/ajr.182.3.1820663. [DOI] [PubMed] [Google Scholar]
- 7.Lin CK, Lai KH, Chan HH, Tsai WL, Wang EM, Wei MC, et al. Endoscopic balloon dilatation is a safe method in the management of common bile duct stones. Dig Liver Dis. 2004;36:68–72. doi: 10.1016/j.dld.2003.09.014. [DOI] [PubMed] [Google Scholar]
- 8.Burhenne HJ. Garland lecture: percutaneous extraction of retained biliary tract stones - 661 patients. AJR Am J Roentgenol. 1980;134:889–898. doi: 10.2214/ajr.134.5.889. [DOI] [PubMed] [Google Scholar]
- 9.Garrow DG. The removal of retained biliary tract stones: report of 105 cases. Br J Radiol. 1977;50:777–781. doi: 10.1259/0007-1285-50-599-777. [DOI] [PubMed] [Google Scholar]
- 10.Burhenne HJ. Complications of non-operative extraction of retained common duct stones. Am J Surg. 1976;131:260–265. doi: 10.1016/0002-9610(76)90111-2. [DOI] [PubMed] [Google Scholar]
- 11.Stokes KR, Clouse ME. Biliary duct stones: percutaneous transhepatic removal. Cardiovasc Intervent Radiol. 1990;13:240–244. doi: 10.1007/BF02578025. [DOI] [PubMed] [Google Scholar]
- 12.Clouse ME, Stokes KR, Lee RGL, Falchuk KR. Bile duct stones: percutaneous transhepatic removal. Radiology. 1986;160:525–529. doi: 10.1148/radiology.160.2.3726136. [DOI] [PubMed] [Google Scholar]
- 13.Stokes KR, Falchuk KR, Clouse ME. Biliary duct stones: update on 54 cases after percutaneous transhepatic removal. Radiology. 1989;170:999–1001. doi: 10.1148/radiology.170.3.2916070. [DOI] [PubMed] [Google Scholar]
- 14.Park JH, Choi BI, Han MC, Sung KB, Choo IW, Kim CW. Percutaneous removal of residual intrahepatic stones. Radiology. 1987;163:619–623. doi: 10.1148/radiology.163.3.3575704. [DOI] [PubMed] [Google Scholar]
- 15.Harris VJ, Sherman S, Trerotola SO, Snidow JJ, Johnson MS, Lehman GA. Complex biliary stones: treatment with a small choledochoscope and laser lithotripsy. Radiology. 1996;199:71–77. doi: 10.1148/radiology.199.1.8633175. [DOI] [PubMed] [Google Scholar]