Abstract
Objective
The outcome evaluation for the revascularization of intracranial vascular stenoses has not been fully described due to the highly technical nature of the procedure. We report here on the early and late clinical outcomes of angioplasty and/or stenting of symptomatic severe intracranial vascular stenoses at a single institute.
Materials and Methods
Since 1995, we have treated 35 patients with symptomatic intracranial vascular stenosis (more than 70% stenosis, mean stenosis: 78.6% ± 6.2%). Angioplasty (n = 19) was performed for the horizontal segment of the middle cerebral artery (M1) (n = 16) and the basilar artery (BA) (n = 1), the intradural vertebral artery (VA) (n = 1), and the cavernous internal carotid artery (ICA) (n = 1). Stenting (n = 16) was performed for the cavernous or petrous ICAs (n = 9), the intradural VA (n = 3), BA (n = 2), and M1 (n = 2) artery. We assessed the angiographic success (defined as residual stenosis < 50%) rate, the periprocedural complications during the 30-day periprocedural period, the symptomatic recurrence and restenosis during a mean 22-month follow-up (FU) period. The Kaplan-Meier estimate of the cumulative event-free rate of the major cerebrovascular events, i.e. death, stroke or restenosis, was also done.
Results
Angiographic success was achieved in 97% of our patients (34/35). There were four procedure-related complications (11%) including a death and a minor stroke. During the mean 22-month FU, the asymptomatic restenosis rate was 9% and the symptomatic restenosis rate was 6% in the target lesion and 9% in all the vascular territories. The Kaplan-Meier estimate was 70.6% (95% confidence interval = 46.5-94.7) after 33 months of FU.
Conclusion
In addition to a high angiographic success rate and an acceptable periprocedural complication rate, intracranial angioplasty and/or stenting revealed a relatively low symptomatic recurrence rate. Hemorrhage is a rare, but the physician must aware that potentially fatal periprocedural complications can occur.
Keywords: Cerebral blood vessels, transluminal angioplasty; Stents and prostheses
Intracranial atherosclerosis is a major cause of ischemic stroke, and depending on the studied population, it accounts for 8-15% of all strokes that are due to cerebral atherosclerosis (1-5). In a retrospective, nonrandomized review of 151 patients in the United States, the annual rate of stroke for patients with symptomatic severe intracranial stenosis was 10.7% in the aspirin-treated group (6). Annual stroke rates reach 15.0% for patients with basilar artery stenosis and 13.7% for patients with vertebral artery stenosis (7). Thijs et al. (8) have reported that those patients with symptomatic intracranial atherosclerosis who failed at antithrombotic therapy, they revealed a very high rate of cerebral ischemic events (55.8%), e.g., 29 of the 52 study patients.
Extracranial-intracranial anastomosis has not been proven to be effective for preventing cerebral ischemia in those patients with atherosclerotic arterial disease in the carotid and middle cerebral arteries (9). In the report by the EC/IC Bypass Study Group (9), non-fatal and fatal strokes occurred earlier and more often in patients who underwent bypass surgery and the patients with severe middle cerebral artery stenosis had the worst outcomes. Bypass surgery also resulted in an 8% mortality rate and a 13% morbidity rate for 83 patients having symptomatic vertebrobasilar insufficiency who underwent 85 bypass procedures (10).
Although endovascular revascularization for symptomatic intracranial stenoses remains at the investigational stage and much of the pertinent information is anecdotal, intracranial angioplasty and stenting are being increasingly performed to treat stenotic lesions (11). The complication rates range from 0-50% (12-23). The possible reasons why the outcomes of angioplasty and stenting procedures vary greatly from center to center have not yet been identified. In addition, any direct comparison of the relevant literature results is difficult because there is no uniformity of the procedures' protocols and of the methods for evaluating the results, and there are also ethnic differences in the incidence of intracranial stenosis. For Koreans, severe atherosclerotic stenoses tend to be more intracranial stenoses than extracranial stenoses (3).
We report here on our results for angioplasty/stenting of the intracranial arteries in 35 consecutive patients. We have included the early and late clinical outcomes, and we compared our results to the results that have been reported in the literature.
MATERIALS AND METHODS
Since 1995, we have treated 35 consecutive patients with severe (more than 70%) symptomatic intracranial stenosis. Nine patients from the authors' previous reports (14, 24) were included along with their full follow-up (FU) data. The patients' ages ranged from 31 to 73 years (mean age: 53), and the male to female ratio was 3.4:1. Angioplasty (n = 19) was done in the M1 segment of the middle cerebral artery (M1) (n = 16) (Figs. 1, 2), the basilar artery (BA) (n = 1), the intradural vertebral artery (VA) (n = 1), and the cavernous internal carotid artery (ICA) (n = 1). Stenting (n = 16) was done in the cavernous (n = 8) or petrous (n = 1) ICA (Fig. 3), the intradural VA (n = 3), the basiler artery (BA) (n = 2), and the M1 segment of the middle cerebral artery (M1) (n = 2). This report did not include any patients who were treated as part of emergency protocols or those patients with intracranial occlusion. For each patient, a complete history taking and a neurological examination were performed by an independent neurologist who was not involved in the interventional procedure. Our data revealed that types of procedure were different among the lesion sites; angioplasty was performed more often in the M1 segment in contrast to stenting being performed in the posterior circulation and in the cavernous segment of the ICA (p < 0.001).
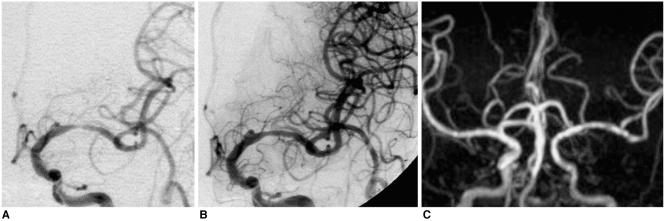
Fig. 1.
A 60-year-old female patient presented with dysarthria and right arm weakness of 20 days duration.
A. The anterioposterior view of the left internal carotid arteriogram shows a severe stenosis of the horizontal segment of the left middle cerebral artery.
B. The flow improves after angioplasty.
C. MR angiogram obtained 68 months later reveals good patency of the horizontal segment of the left middle cerebral artery. She had no symptom recurrence and no residual symptoms.
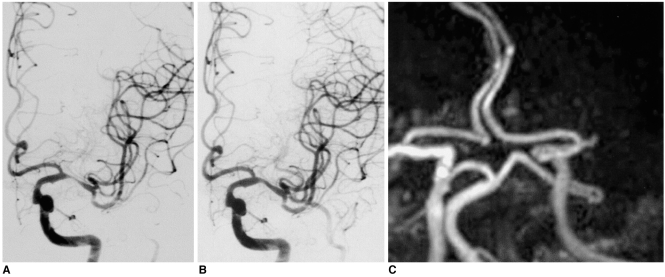
Fig. 2.
A 62-year-old male presented with right side weakness and global aphasia.
A. Angiogram of the left internal carotid artery shows a severe stenosis in the horizontal segment of the left middle cerebral artery.
B. The angiogram obtained after angioplasty shows the relieved stenosis and improved flow. The patient's symptoms slowly improved except for some mild weakness and expressive aphasia that remained after there was symptom aggravation two years later.
C. MR angiography obtained at the time of the symptom aggravation reveals complete occlusion of the left horizontal segment of the left middle cerebral artery.
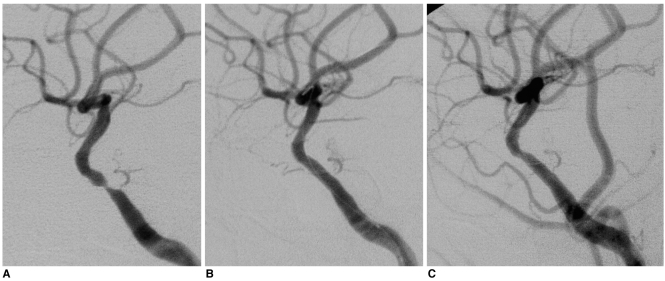
Fig. 3.
A 49-year-old male presented with the left arm weakness.
A. Lateral view of the right internal carotid arteriogram shows a severe stenosis of the cavernous segment of the internal carotid artery.
B. Post-stenting angiogram shows no residual stenosis.
C. One-year follow-up angiogram shows good patency of the stented segment of the internal carotid artery with a 20% stenosis at the distal stent margin. Note a patent side branch of the cavernous segment of the internal carotid artery. The patient recovered completely and had no symptom recurrence during the one-year follow-up period.
Angio-interventional Procedures
Most patients were premedicated with 100 mg of acetylsalicylic acid (ASA) and either 75 mg of clopidogrel (Plavix, Sanofi, Inc) or 250 mg of ticlopidine (Ticlid, Roche, Inc) for at least four days before the procedure. One hundred milligrams of ASA (low dose regimen) once daily was continued as a permanent medication. Additionally, 75 mg of clopidogrel were given once daily for more than six months following the procedures. All the procedures were performed under local anesthesia, and during the procedures, each patient received 5,000-8,000 IU of intravenous heparin to attain an activated clotting time (ACT) of more than 250 seconds. Prior to treatment, diagnostic cerebral angiography was performed via the transfemoral approach. The procedure started with a common carotid artery injection, and this was followed by selective angiography of both the internal carotid and vertebral arteries.
A 6F sheath was introduced and it was then positioned in either the internal carotid artery or the vertebral artery. The sidearm of the guiding catheter was continuously flushed with pressurized, heparinized normal saline, and this catheter was used for angiography treatment steps. After crossing the lesion with a 0.010-0.014-inch outer diameter microguidewire, the balloon catheter was placed over the microguidewire and next directed across the lesion. We used balloon catheters with diameters ranging from 2 to 3 mm and with lengths of 10 or 20 mm according to the target vessel size, and we were careful not to allow any over-dilatation. Balloon inflation was performed slowly and maintained for 10 to 20 seconds with a disposable inflation device that allowed for exact pressure control.
In the 16 stenting procedures, the stenotic lesion was predilated with a balloon catheter 2 mm in diameter and 10-20 mm in length in all cases. A stent 2-4 mm in diameter and 8-18 mm in length was passed over the guidewire and positioned across the stenosis. Each stent was selected according to the size of the target vessel. The residual stenosis of the treated intracranial artery was measured via post-procedural angiography. As the more flexible and lower profile stents have become available, our approach has changed from performing angioplasty alone to performing angioplasty followed by stenting at the same session: this has been done on a more routine basis than was previously done before 2002.
Measurement of Stenosis
The percentage of the diameter of the stenosis was calculated by dividing the narrowest linear diameter at the stenotic segment by the distal diameter at the segment of the same vessel that had a normal appearance (25). Lesion length and eccentricity were measured and categorized according to Mori's classification (13) and these parameters were analyzed for comparison of treatment outcome. An eccentric lesion was defined as when the residual lumen was asymmetrically shifted to one wall of the vessel due to the eccentrically located plaque. Restenosis was evaluated by using transcranial Doppler and/or cerebral angiography.
FU Evaluation
We obtained the clinical data, with the exception of the data for one patient who died, during a mean 22-month FU period (FU range: 3-86 months, median FU: 13). In addition to the clinical FU, MR angiography (MRA) was obtained in 11 patients (Figs. 1, 2), conventional angiography was done for 10 patients (Fig. 3), CT angiography was done for one patient, and transcranial Doppler (TCD) was done for only five patients. The mean imaging study FU period including the TCD was 21 months (range: 3-74, median: 11). Only the clinical FU without the imaging studies was available for seven patients. Two of these seven patients were followed for less than six months (three and four months) and other five patients did not undergo angiographic FU.
Evaluation of Outcome and Statistical Methods
We evaluated angiographic success rate, the periprocedural complications during the 30 days periprocedural period, and the symptomatic recurrence and restenosis during a mean 22-month FU period. The angiographic success, as calculated on a per-vessel basis, was defined as any residual stenosis < 50%. Angiographic restenosis on conventional cerebral angiography was defined as a stenosis > 50% of the luminal diameter. MR angiography FU was mainly used for those patients who only received angioplasty and the degree of stenosis on MRA was based on the interpretations by the staff neuroradiologists. Doppler ultrasonic restenosis was defined as an increased peak systolic velocity threshold of 220 cm/sec for the intracranial internal carotid artery and the proximal middle cerebral artery; the corresponding thresholds were 140 cm/sec for the basilar artery and 120 cm/sec for the vertebral artery (26). Minor stroke was defined as a new non-disabling neurological deficit or an increase of 3 on the National Institutes of Health Stroke Scale (27), or a non-fatal hemorrhage that completely resolved within 30 days. Major stroke was defined as a new neurologic deficit that persisted beyond 30 days and an increase of 4 according to the National Institutes of Health Stroke Scale.
The cumulative event-free rate of major adverse cerebrovascular events (MACEs), i.e. death, stroke or restenosis was analyzed by the Kaplan-Meier method. MACEs included stroke, death and restenosis with or without a symptomatic recurrence during the FU. The log-rank test was used to compare MACEs between the M1 segment of middle cerebral artery and the other sites in the intracranial arteries. We used χ2 or Fisher's exact tests to compare the differences of MACEs between angioplasty and stenting procedures and for the lesion length, lesion eccentricity and the location of the lesions. All the calculations were performed with SPSS for Windows (version 10.0, SPSS Inc).
Repeated angioplasty or repeated stenting during the FU period was not attempted for our patients. We compared our results with the relevant long-term outcomes in the currently available literature (Table 1).
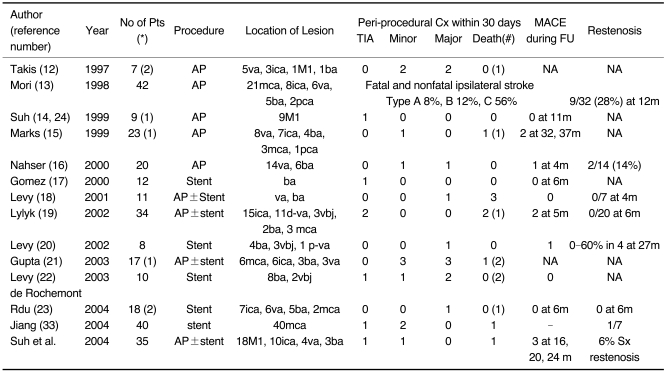
Table 1.
Comparison of Complication Rates in the Literature
Note.-(*) = number of patients not attempted, (#) = death from other causes during follow-up, Cx = complication, AP = angioplasty, ica = internal carotid artery, d-va = distal vertebral artery, p-va = proximal vertebral artery, vbj = vertebrobasilar junction, ba = basilar artery, mca = middle cerebral artery, s = stroke, MACE = major adverse cerebrovascular event (nonfatal cerebral infarct or hemorrhage, revascularization), FU = follow-up, m = month(s), NA = not available, Sx restenosis = symptomatic restenosis related to the target vessel, Mori type A ≤ 5 mm; type B = 5 to 10 mm; type C ≥ 10 mm in lesion length
RESULTS
The mean degree of stenosis in the symptomatic intracranial artery was 78.6% ± 6.2%. After the procedure, the mean residual stenosis was 20.7% ± 14.4%. Angiographic success (less than 50% residual stenosis) was achieved in 97% of the patients, and the only exception was one patient who had an asymptomatic dissection (34/35).
Periprocedural complications within the first 30 days were noted in four patients (11%), and this included an aymptomatic dissection at M1 and a transient ischemic attack at M1. There was a minor stroke in one patient (3%) who experienced a subarachnoid hemorrhage that was due to a guidewire-related arterial perforation, but it resulted in only a transient headache. There was one death due to hemorrhage during a BA stenting (3%).
There was no recurrence of symptoms within one year period (Figs. 1, 3). During the mean 22-month total FU period, symptomatic restenosis/occlusion related to the target lesion was noted in two patients (symptomatic restenosis, 6%). One patient had an ischemic stroke that was not related to the treated vessel. Asymptomatic restenosis was detected in three patients (9%) during the FU period.
Among the three symptomatic patients we observed during FU, one patient experienced aggravation of a neurologic deficit that was related to an occlusion at the M1 segment 24 months after the angioplasty procedure (Fig. 2). Another patient had an intracerebral hematoma and intraventricular hemorrhage that was associated with M1 occlusion 16 months after the angioplasty procedure, but this patient experienced a full recovery by the time of the 33-month FU examination. The other patient revealed an ipsilateral internal carotid artery occlusion on MRA at the time of a pontine infarction 20 months after the procedure; this led to some mild weakness of the patient's extremities.
The Kaplan-Meier curves predicted that the cumulative event-free rate of MACEs, i.e. death, stroke or restenosis, was 70.6% (95% confidence interval = 46.5-94.7) at 33 months. The log rank test for the difference in the cumulative event-free rate of MACEs according to the lesion site showed no statistical significance. There were also no significant differences in MACEs among the types of procedures, the lesion lengths and the lesion eccentricities.
DISCUSSION
Our experience in this study indicated that 97% of our study patients achieved angiographic success (34/35). The incidence of symptomatic restenosis was very low after angioplasty and/or stenting of intracranial stenoses, i.e. 6%, during a mean 22 months of FU. The symptomatic recurrence rate in any vascular territory was 9% during the same FU period. However, intracranial angioplasty and stenting had a 3% fatal complication rate, although our fatality rate was less than those fatality rates reported in the literature (Table 1).
Because the symptomatic recurrence rate was as high as 9% and it seemed to go higher with further long term FU, the physician is required to make a therapeutic decision for those patients with asymptomatic restenosis. Our policy has been to observe these patients closely while they are under medication because symptomatic restenosis is regarded as the only indication for a revascularization procedure including repeated angioplasty and/or stenting.
The recent advent of new generation stents that have low profiles and high flexibility has encouraged the consideration of performing stent-assisted angioplasty as an alternative approach to angioplasty alone for intracranial stenosis (17-23). Presently, the primary limitation of angioplasty appears to be restenosis (defined as more than 50% diameter stenosis on FU angiography), and this is seen in as many as 30% to 40% of the patients who are treated by coronary angioplasty (28).
The complication rates of intracranial angioplasty and stenting are known to be very high, i.e. from 0 to 50% (12-23). The mortality rate was 3% in our study. The periprocedural mortality and morbidity rate also seem to be higher after stenting than for an angioplasty procedure alone (21, 22). Bleeding is a serious complication for intracranial stenting as was seen in one of our study patients. The causes of bleeding include a bleeding tendency caused by aggressive antiplatelet and anticoagulation therapy, hyperperfusion syndrome, vessel rupture or dissection due to ballooning and/or stenting, and guidewire injury. The subarachnoid hemorrhage due to a guidewire injury in a patient of our study had a relatively benign clinical course without further symptomatic problems at four months clinical FU. In addition to the hemorrhagic complications, infarctions related to thromboemboli or to side-branch occlusion due to the presence of the deployed stent also contribute to the fatal peri-procedural complications. We only experienced one transient ischenic attack in a patient after angioplasty of the M1 segment.
One of the major concerns in intracranial stenting is the side branch occlusion that can be caused by the stent struts, although we did not experience any problem related to the perforator or side branch occlusion. The possible mechanism for side branch occlusion after stenting in the coronary artery is the 'snow plow' effect where the atheroma from the parent vessels is shifted into the ostium of a side branch (29, 30). Other mechanisms for side branch occlusion may include side branch spasm, embolization of the atherosclerotic material, thrombus formation and the stent material itself. The presence of ostial narrowing arising from within or just beyond the diseased portion of the parent vessel was the most powerful predictor of side branch occlusion in the coronary artery immediately after stenting (30). The plaque volume of the parent vessel and the side branches is a major determinant for the fate of the side branches.
Perforaters in M1 and BA are different from the side branches in the coronary vessels in that the perforators are terminal branches supplying the deep nuclei of the basal ganglia and brainstem. Experimental evidence from canine vertebral arteries suggests that the cervical muscular branches, which are comparable to human perforators, tend to remain patent if less than 50% of the ostial diameter is covered by the stent strut (31). A size comparison between the stents and the perforators should be made in order to avoid any compromised flow in the perforators (32).
In conclusion angioplasty and/or stenting of the intracranial arteries are relatively safe procedures having a high angiographic success rate (97%), an acceptable rate of periprocedural complication (11%), which included a minor stroke and a death within 30 days, and a low symptomatic restenosis rate for the target lesion (6%) and for all the vascular territories (9%) during the mean 22-month FU. Replacement of intracranial revascularization by stenting needs to be further studied in conjunction with the advent and arrival of new stent devices that have high flexibility and low profiles.
Footnotes
This study was supported by a grant of the Korea Health 21 R&D Project, Ministry of Health & Welfare, Korea. (03-PJ1-PG1-CH06-0001).
References
- 1.Sacco RL, Kargman DE, Gu Q, Zamanillo MC. Race-ethnicity and determinants of intracranial atherosclerotic cerebral infarction. The Northern Manhattan Stroke Study. Stroke. 1995;26:14–20. doi: 10.1161/01.str.26.1.14. [DOI] [PubMed] [Google Scholar]
- 2.Wityk RJ, Lehman D, Klag M, Coresh J, Ahn H, Litt B. Race and sex differences in the distribution of cerebral atherosclerosis. Stroke. 1996;27:1974–1980. doi: 10.1161/01.str.27.11.1974. [DOI] [PubMed] [Google Scholar]
- 3.Suh DC, Lee SH, Kim KR, Park ST, Lim SM, Kim SJ, et al. Pattern of atherosclerotic carotid stenosis in Korean patients with stroke: different involvement of intracranial versus extracranial vessels. AJNR Am J Neuroradiol. 2003;24:239–244. [PMC free article] [PubMed] [Google Scholar]
- 4.Lee SJ, Cho SJ, Moon HS, Shon YM, Lee KH, Kim DI, et al. Combined extracranial and intracranial atherosclerosis in Korean patients. Arch Neurol. 2003;60:1561–1564. doi: 10.1001/archneur.60.11.1561. [DOI] [PubMed] [Google Scholar]
- 5.Warfarin-Aspirin Symptomatic Intracranial Disease (WASID) Trial Investigators. Design, progress and challenges of a double-blind trial of warfarin versus aspirin for symptomatic intracranial arterial stenosis. Neuroepidemiology. 2003;22:106–117. doi: 10.1159/000068744. [DOI] [PubMed] [Google Scholar]
- 6.Chimowitz MI, Kokkinos J, Strong J, Brown MB, Levine SR, Silliman S, et al. The Warfarin-Aspirin Symptomatic Intracranial Disease Study. Neurology. 1995;45:1488–1493. doi: 10.1212/wnl.45.8.1488. [DOI] [PubMed] [Google Scholar]
- 7.The Warfarin-Aspirin Symptomatic Intracranial Disease (WASID) Study Group. Prognosis of patients with symptomatic vertebral or basilar artery stenosis. Stroke. 1998;29:1389–1392. doi: 10.1161/01.str.29.7.1389. [DOI] [PubMed] [Google Scholar]
- 8.Thijs VN, Albers GW. Symptomatic intracranial atherosclerosis: outcome of patients who fail antithrombotic therapy. Neurology. 2000;55:490–497. doi: 10.1212/wnl.55.4.490. [DOI] [PubMed] [Google Scholar]
- 9.The EC/IC Bypass Study Group. Failure of extracranial-intracranial arterial bypass to reduce the risk of ischemic stroke. Results of an international randomized trial. N Engl J Med. 1985;313:1191–1200. doi: 10.1056/NEJM198511073131904. [DOI] [PubMed] [Google Scholar]
- 10.Ausman JI, Diaz FG, Vacca DF, Sadasivan B. Superficial temporal and occipital artery bypass pedicles to superior, anterior inferior, and posterior inferior cerebellar arteries for vertebrobasilar insufficiency. J Neurosurg. 1990;72:554–558. doi: 10.3171/jns.1990.72.4.0554. [DOI] [PubMed] [Google Scholar]
- 11.Chaturvedi S, St Pierre ME, Bertasio B. Cerebral angioplasty practice at major medical centers in the United States. Neuroradiology. 2000;42:218–220. doi: 10.1007/s002340050051. [DOI] [PubMed] [Google Scholar]
- 12.Takis C, Kwan ES, Pessin MS, Jacobs DH, Caplan LR. Intracranial angioplasty: experience and complications. AJNR Am J Neuroradiol. 1997;18:1661–1668. [PMC free article] [PubMed] [Google Scholar]
- 13.Mori T, Fukuoka M, Kazita K, Mori K. Follow-up study after intracranial percutaneous transluminal cerebral balloon angioplasty. AJNR Am J Neuroradiol. 1998;19:1525–1533. [PMC free article] [PubMed] [Google Scholar]
- 14.Suh DC, Sung KB, Cho YS, Choi CG, Lee HK, Lee JH, et al. Transluminal angioplasty for middle cerebral artery stenosis in patients with acute ischemic stroke. AJNR Am J Neuroradiol. 1999;20:553–558. [PMC free article] [PubMed] [Google Scholar]
- 15.Marks MP, Marcellus M, Norbash AM, Steinberg GK, Tong D, Albers GW. Outcome of angioplasty for atherosclerotic intracranial stenosis. Stroke. 1999;30:1065–1069. doi: 10.1161/01.str.30.5.1065. [DOI] [PubMed] [Google Scholar]
- 16.Nahser HC, Henkes H, Weber W, Berg-Dammer E, Yousry TA, Kuhne D. Intracranial vertebrobasilar stenosis: angioplasty and follow-up. AJNR Am J Neuroradiol. 2000;21:1293–1301. [PMC free article] [PubMed] [Google Scholar]
- 17.Gomez CR, Misra VK, Liu MW, Wadlington VR, Terry JB, Tulyapronchote R, et al. Elective stenting of symptomatic basilar artery stenosis. Stroke. 2000;31:95–99. doi: 10.1161/01.str.31.1.95. [DOI] [PubMed] [Google Scholar]
- 18.Levy EI, Horowitz MB, Koebbe CJ, Jungreis CC, Pride GL, Dutton K, et al. Transluminal stent-assisted angiplasty of the intracranial vertebrobasilar system for medically refractory, posterior circulation ischemia: early results. Neurosurgery. 2001;48:1215–1221. doi: 10.1097/00006123-200106000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Lylyk P, Cohen JE, Ceratto R, Ferrario A, Miranda C. Angioplasty and stent placement in intracranial atherosclerotic stenoses and dissections. AJNR Am J Neuroradiol. 2002;23:430–436. [PMC free article] [PubMed] [Google Scholar]
- 20.Levy EI, Hanel RA, Bendok BR, Boulos AS, Hartney ML, Guterman LR, et al. Staged stent-assisted angioplasty for symptomatic intracranial vertebrobasilar artery stenosis. J Neurosurg. 2002;97:1294–1301. doi: 10.3171/jns.2002.97.6.1294. [DOI] [PubMed] [Google Scholar]
- 21.Gupta R, Schumacher HC, Mangla S, Meyers PM, Duong H, Khandji AG, et al. Urgent endovascular revascularization for symptomatic intracranial atherosclerotic stenosis. Neurology. 2003;61:1729–1735. doi: 10.1212/01.wnl.0000103900.65021.5b. [DOI] [PubMed] [Google Scholar]
- 22.Levy EI, Hanel RA, Boulos AS, Bendok BR, Kim SH, Gibbons KJ, et al. Comparison of periprocedure complications resulting from direct stent placement compared with those due to conventional and staged stent placement in the basilar artery. J Neurosurg. 2003;99:653–660. doi: 10.3171/jns.2003.99.4.0653. [DOI] [PubMed] [Google Scholar]
- 23.de Rochemont Rdu M, Turowski B, Buchkremer M, Sitzer M, Zanella FE, Berkefeld J. Recurrent symptomatic high-grade intracranial stenoses: safety and efficacy of undersized stents--initial experience. Radiology. 2004;231:45–49. doi: 10.1148/radiol.2311030183. [DOI] [PubMed] [Google Scholar]
- 24.Lee JH, Kwon SU, Suh DC, Kim JS. Percutaneous transluminal angioplasty for symptomatic middle cerebral artery stenosis: long-term follow-up. Cerebrovasc Dis. 2003;15:90–97. doi: 10.1159/000067135. [DOI] [PubMed] [Google Scholar]
- 25.Barnett HJ, Taylor DW, Eliasziw M, Fox AJ, Ferguson GG, Haynes RB, et al. Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. North American Symptomatic Carotid Endarterectomy Trial Collaborators. N Engl J Med. 1998;339:1415–1425. doi: 10.1056/NEJM199811123392002. [DOI] [PubMed] [Google Scholar]
- 26.Baumgartner RW, Mattle HP, Schroth G. Assessment of >/=50% and < 50% intracranial stenoses by transcranial color-coded duplex sonography. Stroke. 1999;30:87–92. doi: 10.1161/01.str.30.1.87. [DOI] [PubMed] [Google Scholar]
- 27.Goldstein LB, Samsa GP. Reliability of the National Institutes of Health Stroke Scale. Extension to non-neurologists in the context of a clinical trial. Stroke. 1997;28:307–310. doi: 10.1161/01.str.28.2.307. [DOI] [PubMed] [Google Scholar]
- 28.Dangas G, Fuster V. Management of restenosis after coronary intervention. Am Heart J. 1996;132:428–436. doi: 10.1016/s0002-8703(96)90442-1. [DOI] [PubMed] [Google Scholar]
- 29.Aliabadi D, Tilli FV, Bowers TR, Benzuly KH, Safian RD, Goldstein JA, et al. Incidence and angiographic predictors of side branch occlusion following high-pressure intracoronary stenting. Am J Cardiol. 1997;80:994–997. doi: 10.1016/s0002-9149(97)00591-2. [DOI] [PubMed] [Google Scholar]
- 30.Cho GY, Lee CW, Hong MK, Kim JJ, Park SW, Park SJ. Effects of stent design on side branch occlusion after coronary stent placement. Catheter Cardiovasc Interv. 2001;52:18–23. doi: 10.1002/1522-726x(200101)52:1<18::aid-ccd1006>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 31.Wakhloo AK, Tio FO, Lieber BB, Schellhammer F, Graf M, Hopkins LN. Self-expanding nitinol stents in canine vertebral arteries: hemodynamics and tissue response. AJNR Am J Neuroradiol. 1995;16:1043–1051. [PMC free article] [PubMed] [Google Scholar]
- 32.Lopes DK, Ringer AJ, Boulos AS, Qureshi AI, Lieber BB, Guterman LR, et al. Fate of branch arteries after intracranial stenting. Neurosurgery. 2003;52:1275–1278. doi: 10.1227/01.neu.0000064567.15270.27. discussion 1278-1279. [DOI] [PubMed] [Google Scholar]
- 33.Jiang WJ, Wang YJ, Du B, Wang SX, Wang GH, Jin M, et al. Stenting of symptomatic M1 stenosis of middle cerebral artery: an initial experience of 40 patients. Stroke. 2004;35:1375–1380. doi: 10.1161/01.STR.0000128018.57526.3a. [DOI] [PubMed] [Google Scholar]