Abstract
Most heart failure (HF) patients are older adults. However, the association of functional status and outcomes in ambulatory older adults with chronic HF has not been well studied. Of the 7788 Digitalis Investigation Group (DIG) trial participants, 4036 were ≥65 years. Of these, 1369 (34%) had New York Heart Association (NYHA) class III–IV symptoms. We calculated propensity scores for NYHA III–IV symptoms for all 4036 patients using a non-parsimonious logistic regression model. We used propensity scores to match 1010 (74% of 1369) NYHA III–IV patients with 1010 of NYHA I–II patients. Kaplan-Meier and matched Cox proportion hazard analyses were used to estimate associations of NYHA class III–IV with mortality and hospitalizations. Patients had a mean age of 73 years, 31% were female, and 11% were nonwhites. All-cause mortality occurred in 394 (rate, 1385/10000 person-years) NYHA I–II and 452 (rate, 1654/10000 person-years) NYHA III–IV patients, respectively, during 2967 and 2733 years of follow up (hazard ratio {HR}, 1.28; 95% confidence interval {CI}, 1.09–1.50; P=0.002). NYHA III–IV class was associated with increased cardiovascular (HR, 1.25, 95% CI, 1.04–1.49, P=0.016) and HF mortality (HR, 1.51, 95% CI, 1.16–1.97, P=0.002). NYHA III–IV class was not significantly associated with hospitalizations due to all causes (HR, 1.10; 95% CI, 0.96–1.25; P=0.165), cardiovascular causes (HR, 1.11; 95% CI, 0.96–1.29; P=0.150), or worsening HF (HR, 1.09, 95% CI, 0.92–1.30; P=0.330). Baseline NYHA functional class was associated with mortality but not with hospitalization in ambulatory older adults with chronic HF.
Keywords: heart failure, geriatric, NYHA class, physical function, outcomes
1. Introduction
Aging and heart failure (HF) are both characterized by decline in physical function. However, the effect of functional status on outcomes in geriatric HF patients has not been well-studied. Functional status in HF is often assessed using the New York Heart Association (NYHA) functional classification (Hunt, et al., 2005; Radford, et al., 2005). According to NYHA classification, depending on the severity of HF symptoms and the degree of effort needed to elicit those symptoms, patients are classified into one of the four classes: class IV (symptoms of HF are present at rest), class III (symptom are present on less-than-ordinary activity), class II (symptoms on ordinary exertion), and class I (no symptoms at ordinary physical activity) (Radford, et al., 2005).
We have recently demonstrated in a propensity matched study that in ambulatory chronic HF patients, presence of NYHA III–IV symptoms was associated with a significant 23% increase in mortality (Ahmed, 2007). A subgroup analysis of that study suggested that the associations of NYHA class III–IV symptoms and mortality were significant in both younger (age <65 years) and older (age ≥65 years) patients. However, the association was significantly weaker among older adults (P for interaction=0.002) (Ahmed, 2007).
Evidence for elderly HF patients is frequently extrapolated from younger patients, as elderly HF patients are often excluded from randomized trials. Unlike in randomized trials, results of non-randomized studies can be more readily replicated in a cost-effective manner, obviating the need for such extrapolation. Therefore, the objective of this study was to determine the association between NYHA functional class and mortality and hospitalizations in a propensity score matched cohort of ambulatory older adults with chronic HF.
2. Subjects and methods
2.1. Data source and patients
A public use copy of the Digitalis Investigation Group (DIG) data sets was used for the current analysis. The DIG trial enrolled 7788 ambulatory chronic HF patients in normal sinus rhythm from 302 clinical centers in the U.S. (186 centers) and Canada (116 centers) between January 1991 and August 1993 (The Digitalis Investigation Group, 1996; The Digitalis Investigation Group, 1997). Of these patients, 4036 were 65 years and older, and 3405 (84%) had left ventricular ejection fraction (LVEF) ≤45%.
2.2. New York Heart Association functional (NYHA) class
Participants in the DIG trial were classified by DIG investigators into one of the four NYHA classes depending on the severity of HF symptoms and the degree of effort needed to elicit those symptoms: class I (n=516), class II (n=2151), class III (n=1276), and class IV (n=93). Because of functional similarity and convenience of propensity matching, we combined patients with NYHA class I and II symptoms as NYHA class I–II (n=2667), and those with class III and IV symptoms as NYHA class III–IV (n=1369).
2.3. Outcomes
For the purpose of this analysis, we studied the following outcomes: mortality and hospitalizations due to all causes, cardiovascular causes, and worsening HF. Data on vital status were 99% complete (Collins, et al., 2003).
2.4. Estimation of propensity scores
Because of significant imbalance in baseline covariates between patients with NYHA class I–II and III–IV symptoms (Table 1), we calculated propensity scores for NYHA III–IV symptoms for 4036 patients using a non-parsimonious multivariable logistic regression model, adjusting for all available baseline covariates, and incorporating significant two-way interaction terms in the model (Ahmed, et al., 2006b; Ahmed, et al., 2006c; Ahmed, et al., 2006d; Rosenbaum and Rubin, 1983; Rubin, 1997; Rubin, 2001). Covariates in the model included age, sex, race, body mass index, duration of HF, etiology of HF (ischemic versus other causes), prior myocardial infarction, current angina, hypertension, diabetes, diuretic, potassium-sparing diuretics, potassium supplement, angiotensin-converting enzyme (ACE) inhibitors, combined use of hydralazine and nitrates, and pre-trial use of digoxin, dyspnea at rest, dyspnea on exertion, third heart sound, elevated jugular venous pressure, pulmonary râles, lower extremity edema, pulmonary congestion, cardiothoracic ratio >0.5, serum creatinine and potassium levels, and LVEFE. The model calibrated (Hosmer-Lemeshow test: p = 0.329) and discriminated (area under the receiver operating characteristic curve; C = 0.79) well.
Table 1.
Baseline patient characteristics of geriatric heart failure patients, before and after propensity score matching
| Before matching | After matching | ||||
|---|---|---|---|---|---|
| N (%) or mean (±SD) | NYHA I–II (N=1010)* | P | NYHA III–IV (N=1010)** | P | NYHA I–II (N=1010) |
| Age (years) | 71.7 (±5.1) | <0.0001 | 72.5 (±5.6) | 0.879 | 72.5 (±5.5) |
| Age ≥75 years | 277 (27.4%) | 0.002 | 343 (34.0%) | 0.344 | 322 (31.9%) |
| Female | 238 (43.1%) | <0.0001 | 314 (31.1%) | 0.481 | 316 (31.3%) |
| Non-white | 114 (11.3%) | 1.00. | 113 (11.2%) | 1.000 | 113 (11.2%) |
| Body mass index, kg/square meter | 26 (±4) | 0.438 | 27 (±5) | 0.178 | 27 (±5) |
| Duration of HF (months) | 31 (±40) | 0.760 | 30 (±37) | 0.474 | 30 (±39) |
| Primary cause of HF | |||||
| Ischemic | 740 (73.3%) | 720 (71.9%) | 720 (71.3%) | ||
| Hypertensive | 121 (12.0%) | 109 (10.8%) | 109 (11.3%) | ||
| Idiopathic | 102 (10.1%) | 0.261 | 124 (12.3%) | 0.882 | 124 (11.9%) |
| Others | 47 (4.7%) | 50 (5.0%) | 57 (5.6%) | ||
| Comorbid conditions | |||||
| Prior myocardial infarction | 659 (65.2%) | 0.780 | 652 (64.6%) | 0.963 | 654 (64.8%) |
| Current anginapectoris | 245 (24.3%) | <0.0001 | 327 (32.4%) | 0.962 | 325 (32.2%) |
| Hypertension | 496 (49.1%) | 0.593 | 483 (47.8%) | 0.824 | 489 (48.4%) |
| Diabetes mellitus | 286 (26.2%) | 0.493 | 301 (29.8%) | 0.698 | 310 (30.7%) |
| Chronic kidney disease | 578 (57.2%) | 0.001 | 649 (64.3%) | 0.963 | 651 (64.5%) |
| Medications | |||||
| Pre-trial digoxin use | 428 (42.4%) | 0.964 | 426 (42.2%) | 0.653 | 437 (43.3%) |
| Trial use of digoxin | 486 (48.1%) | 0.306 | 510 (50.5%) | 0.593 | 497 (49.2%) |
| ACE inhibitors | 927 (91.8%) | 0.239 | 941 (93.2%) | 0.729 | 937 (92.8%) |
| Hydralazine & nitrates | 12 (1.2%) | 0.844 | 14 (1.4%) | 0.854 | 16 (1.6%) |
| Diuretics | 769 (76.1%) | <0.0001 | 870 (86.1%) | 0.898 | 867 (85.8%) |
| Potassium-sparing diuretics | 67 (6.6%) | 0.389 | 77 (7.6%) | 1.000 | 77 (7.6%) |
| Potassium supplement | 265 (26.2%) | 0.002 | 329 (32.6%) | 0.962 | 331 (32.8%) |
| Symptoms and signs of heart failure | |||||
| Dyspnea at rest | 131 (13.0%) | <0.0001 | 270 (26.7%) | 0.617 | 281 (27.8%) |
| Dyspnea on exertion | 678 (67.1%) | <0.0001 | 928 (91.9%) | 0.679 | 934 (92.5%) |
| Jugular venous distension | 91 (9.0%) | <0.0001 | 182 (18.0%) | 0.726 | 175 (17.3%) |
| Third heart sound | 188 (18.6%) | <0.0001 | 274 (50.2%) | 0.960 | 272 (26.9%) |
| Pulmonary râles | 135 (13.4%) | <0.0001 | 247 (24.5%) | 0.835 | 242 (24.0%) |
| Lower extremity edema | 172 (17.0%) | <0.0001 | 266 (26.3%) | 0.839 | 261 (25.8%) |
| Heart rate (/minute) | 76 (±12) | <0.0001 | 78 (±12) | 0.954 | 78 (±12) |
| Systolic blood pressure (mm Hg) | 131 (±20) | 0.001 | 128 (±22) | 0.109 | 128 (±19) |
| Diastolic blood pressure (mm Hg) | 74 (±11) | 0.013 | 73 (±12) | 0.800 | 73 (±11) |
| Serum creatinine (mg/dL) | 1.3 (±0.4) | <0.0001 | 1.4 (±0.4) | 0.808 | 1.4 (±0.4) |
| Chest radiograph findings | |||||
| Pulmonary congestion | 104 (10.3%) | <0.0001 | 189 (18.7%) | 0.774 | 183 (18.1%) |
| Cardiothoracic ratio >0.5 | 596 (59.0%) | <0.0001 | 690 (68.3%) | 0.962 | 688 (68.1%) |
| Ejection fraction (%) | 34 (±12.0) | <0.0001 | 32 (±13) | 0.603 | 32 (±13) |
| Ejection fraction >45% | 172 (17.0%) | 0.056 | 140(13.9%) | 0.795 | 135 (13.4%) |
Of the 2667 patients with NYHA I–II symptoms before matching, a sample of 1010 patients were randomly selected for comparison with 1010 NYHA III–IV patients from the matched cohort (middle column). This was done to avoid potential overestimation of significant p values from a larger per-match sample size.
Patients with NYHA I–II symptoms, both before matching (left column) and after matching (right column), were compared with NYHA III–IV patients who were matched (middle column); respective p values are displayed to the left and right side of this column.
2.5. Propensity score matching
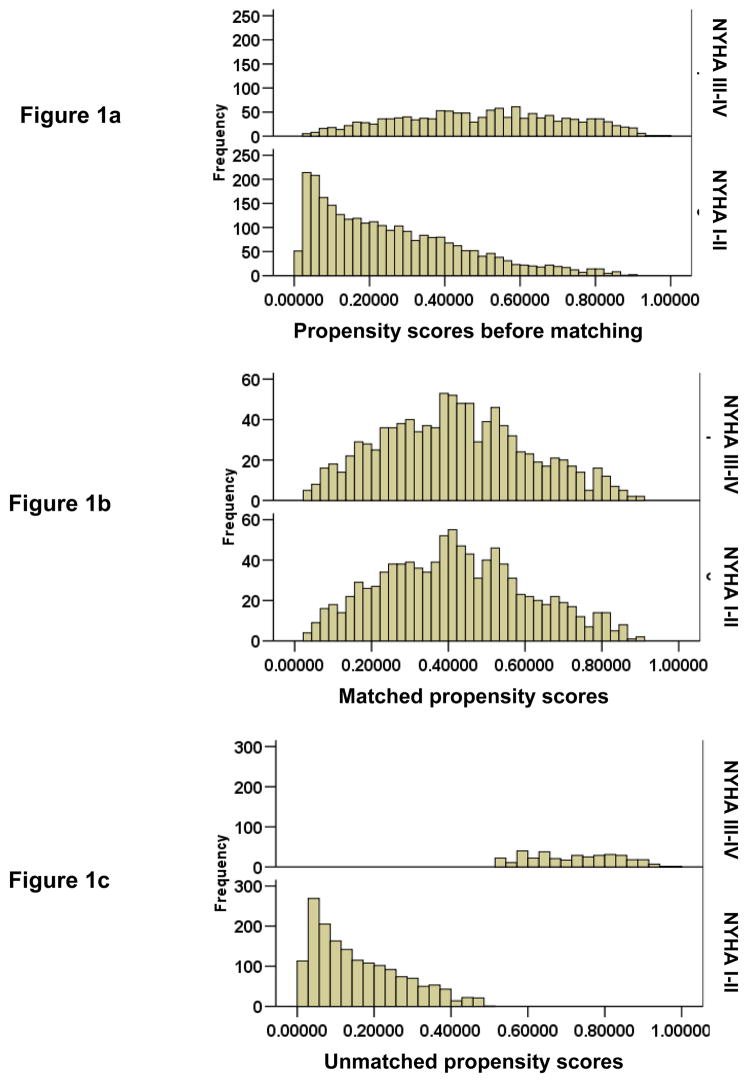
Using an SPSS macro, we matched each NYHA III–IV patient with another patient, who had NYHA class I–II symptoms, but had a similar propensity score for NYHA III–IV symptoms (Figure 1) (Ahmed, et al., 2006b; Ahmed, et al., 2006c; Ahmed, et al., 2006d; Levesque, 2005). Matching is considered the most conservative of the three commonly used propensity score methods. Overall, 74% (1010/1369) NYHA III–IV patients were matched with 1010 of NYHA I–II patients with similar propensity scores. To assemble a comparable sized pre-match cohort, we randomly selected 1010 NYHA I–II patients from the pre-match file and paired them with 1010 NYHA III–IV in the matched file.
Figure 1.
Distribution of propensity scores by New York Heart association (NYHA) functional class
2.6. Quantification of bias reduction: standardized differences
Absolute standardized difference in propensity scores between NYHA I–II and NYHA III–IV patients before and after matching were respectively 116% and 0.3%. Absolute standardized difference after matching between NYHA I–II versus III–IV patients in all measured covariates were <5% (Figure 2). An absolute standardized difference of <10% is considered acceptable reduction of bias (Ahmed, et al., 2006b; Ahmed, et al., 2006c; Ahmed, et al., 2006d; Austin, et al., 2006; Normand, et al., 2001).
Figure 2.
Absolute standardized differences before and after propensity score matching comparing covariate values for patients with New York Heart Association class I–II versus III–IV
2.7. Statistical analysis
Baseline characteristics of HF patients with NYHA I–II versus III–IV symptoms were compared using Pearson chi-square and Wilcoxon rank-sum tests. Kaplan-Meier analysis and matched Cox proportional hazards analyses were used to determine association of NYHA III-IV (relative to class I–II) and various outcomes. Proportional hazards assumptions were checked using log-minus-log scale survival plots for patients in the two treatment groups. To determine if there was any heterogeneity in the association between NYHA class and mortality, we conducted subgroup analyses, and tested for interactions. All statistical tests were done using SPSS for Windows (Release 14) (SPSS, 2006), and two-tailed 95% confidence levels; a p <0.05 was required to reject the null hypothesis.
3. Results
3.1. Patient characteristics
Overall, patients had a mean age of 73 years, 31% were female, and 11% were nonwhites. Balance in baseline characteristics and quantitative measures of biases in patients with NYHA I–II and III–IV symptoms, before and after matching are displayed in Table 1 and Figure 2. Values of absolute standardized differences for all covariates were <5%, suggesting considerable reduction of bias (Ahmed, et al., 2006b; Ahmed, et al., 2006c; Ahmed, et al., 2006d; Austin, et al., 2006; Normand, et al., 2001).
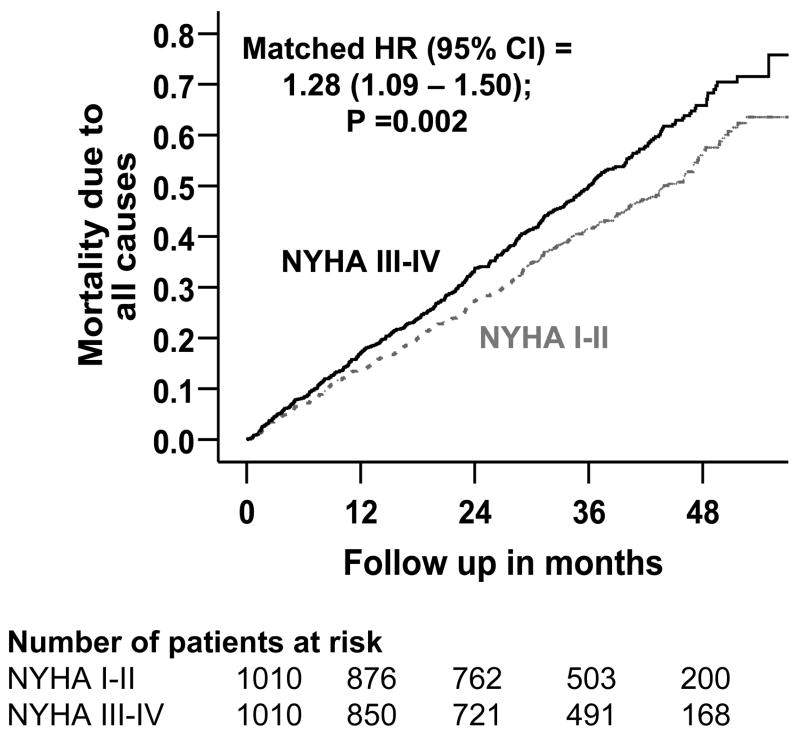
3.2. Function and mortality
Overall, 846 (42%) died from all causes, including 652 (32%) due to cardiovascular causes and 330(16%) due to HF during the median follow up of 35.6 months. Kaplan-Meier plots for deaths due to all causes are displayed in Figure 3. Compared with 394 deaths from all causes in NYHA I–II patients during 2967 years of follow up (mortality rate, 1385 per 10000 person-years), 452 NYHA III–IV patients died during 2733 years of follow up (mortality rate, 1654 deaths per 10000 person-year; Table 2). Presence of NYHA III–IV symptoms at baseline was associated with a significant 28% increase in all-cause mortality (hazard ratio, 1.28, 95% confidence interval, 1.09– 1.50; p =0.002). Association of NYHA III–IV and mortality due to cardiovascular causes and HF are displayed in Table 2. Unadjusted associations of NYHA III–IV class symptoms and various mortalities before matching are also displayed in Table 2.
Figure 3.
Kaplan-Meier plots for mortality due to all-causes by New York Heart Association (NYHA) functional class
Table 2.
Mortality by causes in geriatric heart failure patients before and after matching by propensity scores for NYHA class III–IV
| NYHA I–II (N=1010)
|
NYHA III–IV (N=1010)
|
Absolute rate difference* (per 10000 person-years of follow up) | Hazard ratio (95% confidence interval)† | P value | |
|---|---|---|---|---|---|
| Mortality Events/total follow-up years (Rate per 10000 person-years of follow up) | |||||
| Before matching | |||||
| All-cause | 355/2967 (1196) | 452/2733 (1654) | + 458 | 1.39 (1.21–1.60) | <0.0001 |
| Cardiovascular | 258/2967 (870) | 348/2733 (1273) | + 403 | 1.47 (1.25–1.73) | <0.0001 |
| Worsening heart failure | 109/2967 (367) | 189/2733 (691) | + 324 | 1.91 (1.51–2.42) | <0.0001 |
| After matching | |||||
| All-cause | 394/2967 (1385) | 452/2733 (1654) | + 269 | 1.28 (1.09–1.50) | 0.002 |
| Cardiovascular | 304/2967 (1196) | 348/2733 (1654) | + 304 | 1.25 (1.04–1.49) | 0.016 |
| Worsening heart failure | 141/2967 (496) | 189/2733 (692) | + 196 | 1.51 (1.16–1.97) | 0.002 |
Absolute differences in rates of mortality per 10000 person-year of follow up were calculated by subtracting the death rates in the NYHA I–II group from those in the NYHA III–IV group (before values were rounded)
Hazard ratios and confidence intervals were estimated from the matched cox proportional-hazards models
3.3. Function and hospitalization
Overall, 1459 (72%) patients had hospitalizations due to all causes, including 1145 (57%) due to cardiovascular causes and 744 (37%) due to worsening HF. Compared with 723 hospitalizations from all causes in patients with NYHA I–II symptom during 1553 years of follow up (rate, 4656 hospitalizations per 10000 person-years), 736 NYHA III–IV patients were hospitalized during 1418 years of follow up (rate, 5190 deaths per 10000 person-years; Table 3). Baseline NYHA III–IV symptoms were not associated with hospitalizations (Table 3). Association of NYHA III–IV and hospitalizations due to cardiovascular causes and HF are displayed in Table 3. Unadjusted associations of NYHA III–IV class symptoms and various hospitalizations before matching are also displayed in Table 3.
Table 3.
Hospitalizations by causes in geriatric heart failure patients before and after matching by propensity scores for NYHA class III–IV
| Cause for hospitalization* | NYHA I–II (N=1010)
|
NYHA III–IV (N=1010)
|
Absolute difference† (per 10,000 person-year of follow up) | Hazard ratio (95% confidence interval)‡ | P value |
|---|---|---|---|---|---|
| Hospitalization Events/total follow-up years (Rate per 10,000 person-years of follow up) | |||||
| Before matching | |||||
| All-cause | 682/1763 (3868) | 736/1418 (5190) | + 1322 | 1.30 (1.17–1.44) | <0.0001 |
| Cardiovascular | 501/2113 (2371) | 588/1753 (3354) | + 983 | 1.37 (1.21–1.54) | <0.0001 |
| Worsening heart failure | 263/2609 (1008) | 381/2176 (1751) | + 743 | 1.68 (1.43–1.96) | <0.0001 |
| Number of total hospitalizations | 10533 | 16262 | + 5729 | ||
| After matching | |||||
| All-cause | 723/1553 (4656) | 736/1418 (5190) | + 534 | 1.10 (0.96–1.25) | 0.165 |
| Cardiovascular | 557/1899 (2933) | 588/1753 (3354) | + 421 | 1.11 (0.96–1.29) | 0.150 |
| Worsening heart failure | 363/303 (1576) | 381/2176 (1751) | + 175 | 1.09 (0.92–1.30) | 0.330 |
| Number of total hospitalizations | 13799 | 16262 | + 2463 | ||
Data shown include the first hospitalization of each patient due to each cause.
Absolute differences were calculated by subtracting the percentage of patients hospitalized in the placebo group from the percentage of patients hospitalized in the digoxin group (before values were rounded).
Hazard ratios and confidence intervals (CI) were estimated from a Cox proportional-hazards models that used the first hospitalization of each patient for each reason
4. Discussion
4.1. Key study findings
The findings of the current study suggest that the presence of NYHA class III–IV (versus class I–II) symptoms was associated with increased mortality in older adults with HF. However, in contrast with relatively younger HF patients (Ahmed, 2007), the presence of NYHA class III–IV symptoms was not significantly associated with hospitalization. These findings are important as most HF patients are older adults and with the aging of the population, the prevalence of HF is projected to increase in the coming decades.
4.2. Possible explanation of study findings
The findings of our study are intriguing as after matching, patients with NYHA class I–II and III–IV had similar symptom and comorbidity burden, yet those with higher NYHA class were at increased risk of death. The relatively weaker association of functional limitation and mortality in elderly HF patients compared with younger HF patients (Ahmed, 2007) is likely due to the fact that in older adults functional decline can be due to causes other than HF symptoms. It is possible that in older adults with HF, presence of functional limitation may be a marker of disease progression, and not just a marker of temporary symptomatic exacerbation.
This notion is also supported by our finding that presence of higher NYHA class symptoms was not associated with increased hospitalization in this cohort of elderly HF patients. This finding is also consistent with clinical observation that older adults with HF often attribute their HF symptoms to aging, thus delaying diagnosis, clinical evaluation, and hospitalization. Other factors such as difficulty with transportation, and disliking for long delays in busy emergency departments and non-familiar hospital environment may also explain why geriatric HF patients may not seek and receive timely care. Because older adults are in general a heterogeneous group and are more likely to restrict their physical activity due to aging, deconditioning, and other comorbidities, NYHA functional class may not be a good marker of HF symptom burden in these patients.
4.3. Comparison with other studies in the literature
To the best of our knowledge, this is the first study of association of NYHA class and long-term outcomes in a propensity score matched cohort of geriatric HF patients. Our finding of an increased mortality associated with higher NYHA class is consistent with those of prior studies, which were mainly based on relatively young patients with advanced systolic HF awaiting cardiac transplants (Campana, et al., 1993; Horwich, et al., 2002). Other studies are smaller and based on short-term outcomes (Bouvy, et al., 2003; Jiang, et al., 2001; Madsen, et al., 1994; Muntwyler, et al., 2002; Scrutinio, et al., 1994). Matching by propensity scores is a particular strength of the current study.
4.4. Clinical implications
Geriatric HF patients with higher NYHA class symptoms should be assessed for potential reasons for their higher symptom burden. They should also be treated with life-saving neurohormonal antagonists following recommendations of a major HF guideline. If they are volume overloaded, euvolemia should be achieved with careful use of diuretics. Other interventions such as salt and fluid restriction, adherence with medications, physical therapy, and palliative care should also be considered as appropriate.
4.5. Strengths and limitations
While propensity score technique can account for imbalances in all measured covariates, it may or may not balance unmeasured covariates. However, for such an unmeasured confounder to explain away our finding it must be strongly associated with NYHA class and outcomes, and be not strongly associated with any of the many baseline covariates in the DIG trial (Ahmed, et al., 2006a; The Digitalis Investigation Group, 1997). It is possible that some patients with NYHA class I–II became III–IV due to disease progression or noncompliance with therapy, and vice-versa. However, such misclassification is likely to be random and could only have underestimated the association observed in our analysis. Finally, the results of our study are based on HF patients who were in normal sinus rhythm from a pre-beta-blocker era. Thus, their generalizability to contemporary elderly HF patients is uncertain.
4.6. Conclusions
In geriatric HF patients, the presence of dyspnea and fatigue at rest or on less-than-ordinary physical activity (NYHA class III–IV) at baseline was associated with increased mortality but had no effect on hospitalizations, including those due to worsening HF.
Acknowledgments
“The Digitalis Investigation Group (DIG) study was conducted and supported by the NHLBI in collaboration with the DIG Investigators. This Manuscript was prepared using a limited access dataset obtained by the NHLBI and does not necessarily reflect the opinions or views of the DIG Study or the NHLBI.”
Funding/Support: Dr. Ahmed is supported by the National Institutes of Health through grants from the National Institute on Aging (1-K23-AG19211-04) and the National Heart, Lung, and Blood Institute (1-R01-HL085561-01 and P50-HL077100).
Footnotes
Author Contributions: Dr. Ahmed conceived the study hypothesis and design, wrote the first and subsequent drafts of the manuscript. Dr. Ahmed conducted statistical analyses and Dr. Aronow participated in the interpretation of the data and critical revision of the paper and approved the final version of the article. Dr. Ahmed had full access to the data
Contributor Information
Ali Ahmed, University of Alabama at Birmingham and Veterans Affairs Medical Center, Birmingham, AL.
Wilbert S. Aronow, New York Medical College, Valhalla, NY.
References
- Ahmed A. A propensity matched study of New York Heart Association class and natural history endpoints in heart failure. Am J Cardiol. 2007;99:549–553. doi: 10.1016/j.amjcard.2006.08.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed A, Aronow WS, Fleg JL. Higher New York Heart Association classes and increased mortality and hospitalization in patients with heart failure and preserved left ventricular function. Am Heart J. 2006a;151:444–50. doi: 10.1016/j.ahj.2005.03.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed A, Husain A, Love TE, Gambassi G, Dell’italia LJ, Francis GS, Gheorghiade M, Allman RM, Meleth S, Bourge RC. Heart failure, chronic diuretic use, and increase in mortality and hospitalization: an observational study using propensity score methods. Eur Heart J. 2006b;27:1431–1439. doi: 10.1093/eurheartj/ehi890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed A, Perry GJ, Fleg JL, Love TE, Goff DC, Jr, Kitzman DW. Outcomes in ambulatory chronic systolic and diastolic heart failure: A propensity score analysis. Am Heart J. 2006c;152:956–66. doi: 10.1016/j.ahj.2006.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed A, Rich MW, Love TE, Lloyd-Jones DM, Aban IB, Colucci WS, Adams KF, Gheorghiade M. Digoxin and reduction in mortality and hospitalization in heart failure: a comprehensive post hoc analysis of the DIG trial. Eur Heart J. 2006d;27:178–86. doi: 10.1093/eurheartj/ehi687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin PC, Grootendorst P, Anderson GM. A comparison of the ability of different propensity score models to balance measured variables between treated and untreated subjects: a Monte Carlo study. Stat Med. 2006 doi: 10.1002/sim.2580. [DOI] [PubMed] [Google Scholar]
- Bouvy ML, Heerdink ER, Leufkens HG, Hoes AW. Predicting mortality in patients with heart failure: a pragmatic approach. Heart. 2003;89:605–9. doi: 10.1136/heart.89.6.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campana C, Gavazzi A, Berzuini C, Larizza C, Marioni R, D’Armini A, Pederzolli N, Martinelli L, Vigano M. Predictors of prognosis in patients awaiting heart transplantation. J Heart Lung Transplant. 1993;12:756–65. [PubMed] [Google Scholar]
- Collins JF, Howell CL, Horney RA. Determination of vital status at the end of the DIG trial. Control Clin Trials. 2003;24:726–30. doi: 10.1016/j.cct.2003.08.011. [DOI] [PubMed] [Google Scholar]
- Horwich TB, Fonarow GC, Hamilton MA, MacLellan WR, Borenstein J. Anemia is associated with worse symptoms, greater impairment in functional capacity and a significant increase in mortality in patients with advanced heart failure. J Am Coll Cardiol. 2002;39:1780–6. doi: 10.1016/s0735-1097(02)01854-5. [DOI] [PubMed] [Google Scholar]
- Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup ML, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation. 2005;112:e154–235. doi: 10.1161/CIRCULATIONAHA.105.167586. [DOI] [PubMed] [Google Scholar]
- Jiang W, Alexander J, Christopher E, Kuchibhatla M, Gaulden LH, Cuffe MS, Blazing MA, Davenport C, Califf RM, Krishnan RR, O’Connor CM. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med. 2001;161:1849–56. doi: 10.1001/archinte.161.15.1849. [DOI] [PubMed] [Google Scholar]
- Levesque R. Macro. In: Levesque R, editor. SPSS® Programming and Data Management, 2nd Edition. A Guide for SPSS® and SAS® Users. 2. Chicago, IL: SPSS Inc; [Last access date: June 4, 2005]. 2005. Available online at: http://www.spss.com/spss/data_management_book.htm. [Google Scholar]
- Madsen BK, Hansen JF, Stokholm KH, Brons J, Husum D, Mortensen LS. Chronic congestive heart failure. Description and survival of 190 consecutive patients with a diagnosis of chronic congestive heart failure based on clinical signs and symptoms. Eur Heart J. 1994;15:303–10. doi: 10.1093/oxfordjournals.eurheartj.a060495. [DOI] [PubMed] [Google Scholar]
- Muntwyler J, Abetel G, Gruner C, Follath F. One-year mortality among unselected outpatients with heart failure. Eur Heart J. 2002;23:1861–6. doi: 10.1053/euhj.2002.3282. [DOI] [PubMed] [Google Scholar]
- Normand ST, Landrum MB, Guadagnoli E, Ayanian JZ, Ryan TJ, Cleary PD, McNeil BJ. Validating recommendations for coronary angiography following acute myocardial infarction in the elderly: a matched analysis using propensity scores. J Clin Epidemiol. 2001;54:387–98. doi: 10.1016/s0895-4356(00)00321-8. [DOI] [PubMed] [Google Scholar]
- Radford MJ, Arnold JM, Bennett SJ, Cinquegrani MP, Cleland JG, Havranek EP, Heidenreich PA, Rutherford JD, Spertus JA, Stevenson LW, Goff DC, Grover FL, Malenka DJ, Peterson ED, Redberg RF. ACC/AHA key data elements and definitions for measuring the clinical management and outcomes of patients with chronic heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Data Standards (Writing Committee to Develop Heart Failure Clinical Data Standards): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Failure Society of America. Circulation. 2005;112:1888–916. doi: 10.1161/CIRCULATIONAHA.105.170073. [DOI] [PubMed] [Google Scholar]
- Rosenbaum PR, Rubin DB. The central role of propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997;127:757–63. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Using propensity score to help design observational studies: Application to the tobacco litigation. Health Services and Outcomes Research Methodology. 2001;2:169–188. [Google Scholar]
- Scrutinio D, Lagioia R, Ricci A, Clemente M, Boni L, Rizzon P. Prediction of mortality in mild to moderately symptomatic patients with left ventricular dysfunction. The role of the New York Heart Association classification, cardiopulmonary exercise testing, two-dimensional echocardiography and Holter monitoring. Eur Heart J. 1994;15:1089–95. doi: 10.1093/oxfordjournals.eurheartj.a060633. [DOI] [PubMed] [Google Scholar]
- SPSS. SPSS for Windows, Rel. 14. Chicago, IL: SPSS Inc., Chicago, IL; 2006. [Google Scholar]
- The Digitalis Investigation Group. Rationale, design, implementation, and baseline characteristics of patients in the DIG trial: a large, simple, long-term trial to evaluate the effect of digitalis on mortality in heart failure. Control Clin Trials. 1996;17:77–97. doi: 10.1016/0197-2456(95)00065-8. [DOI] [PubMed] [Google Scholar]
- The Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med. 1997;336:525–33. doi: 10.1056/NEJM199702203360801. [DOI] [PubMed] [Google Scholar]